

Researchers used a broad brush when they focused on the most easily understood aspect of the disorder – fatigue. Now, in this bold and provocative blog, the first part of a four-part series called “A Neuroinflammatory Model of ME/CFS”, guest blogger Marco proposes that other symptoms, none of which are in the Fukuda definition of CFS, may provide more insights into the causes of Chronic ‘Fatigue’ Syndrome than the fatigue its been so firmly linked with. Only time will tell if Marco’s theory is correct but it’s good to get a fresh perspective on this disorder.
Voices Rising! – Many talented people with ME/CFS who do not have medical degrees have spent considerable time and effort trying to understand this disorder – sometimes with very fresh perspectives. Marco’s essays are the first to appear in the ‘Voices Rising’ series of rigorous research and treatment reviews, advocacy essays and others from members of the ME/CFS community. Health Rising will provide each author with 40% of Paypal donations through its first six months on the site. Each author will retain full copyright of their material and will be able to post it on other sites. Thanks to Marco for kicking off the Health Rising Series:)

Marco’s personal investigations lead him to conclude chronic fatigue syndrome was likely a ‘neuro-inflammatory’ disorder
A Neuroinflammatory Model of ME/CFS
This document is the first in a series of four in which I hope to set out a hypothesis for a single neuroinflammatory process as the core pathophysiology underpinning ME/CFS as well as a range of other conditions.
I have written this in ‘blog’ format rather than in the more traditional format of a scientific paper for two reasons. Firstly, it was always my intention to put together a ‘short’ paper that I could open up for discussion amongst ourselves. Every hypothesis must be critically tested and who better to do this than those who live with ME/CFS on a daily basis.
Secondly, this material has evolved over the course of just over a year. The initial impetus came from several threads on Phoenix Rising where I and others were discussing several ‘atypical’ symptoms we experienced including various types of ‘sensory defensiveness’ or ADHD or ASD like behaviours or symptoms that are rarely if ever mentioned in the ME/CFS literature and which seemed more appropriate to an alternative ‘diagnosis’.
Comparing conditions in which various forms of ‘sensory overload’ featured brought up some startling commonalities and led to neuroinflammation as a potential common pathophysiology.
I hope to present this under the following headings :
- Part I – Sensory Gating
- Part II – Glutamate – One More Piece in the Puzzle?
- Part III – Glutamate/GABA Imbalance – Stiff Person Syndrome
- Part IV – Symptoms, heterogeneity and onset
My many thanks to Cort Johnson who has worked with me on this over a period of many months in the capacity of ‘contributing editor’ and who has now kindly agreed to host this material here as one of what will hopefully become a growing list of ‘guest bloggers’.
I hope this ‘hypothesis’ resonates with at least some of you.
- Learn more about Marco’s background and his experiences with ME/CFS here.
‘Sensory Gating’ – A Key to Chronic Fatigue Syndrome (ME/CFS)?
First a short questionnaire….. Would you agree or disagree with below statements?
- My hearing is so sensitive that ordinary sounds become uncomfortable
- There have been times when it seems that sounds and sights are coming in too fast
- It’s not bad when just one person is speaking but if others join in, then I can’t pick it up at all. I just can’t get into tune with that conversation
- There are days when indoor lights seem so bright that they bother my eyes.
- I have more trouble concentrating than others seem to have
- I seem to hear the smallest details of sound
- When I’m tired sounds seem amplified
These statements are taken from a questionnaire developed to assess problems with something called ‘sensory gating’. If you answered yes to several of these or other similar questions you could have problems with sensory gating. (Other possible sensory gating problems include over-sensitization to such things as touch (allodynia), smell (environmental sensitivities) and taste.)
Breaking out of the bunker. Systemic diseases and vague non-specific symptoms
Why focus on these kind of odd sensory issues when the medical community overwhelmingly associates chronic fatigue syndrome with fatigue? Because there is a tendency in science and medicine to use ‘cardinal symptoms’ (the most obvious and pressing symptoms’ found in a disorder) to pigeon-hole it. Once a diagnosis is made and a condition named both researchers and physicians tend to focus on these symptoms, largely ignoring minor symptoms or those that tend to overlap with other conditions. This ‘bunker mentality’ approach may be appropriate for single organ, single pathogen diseases but increasingly research points to multi-pathogen (or stressor) systemic diseases or physiological pathologies that may underlie a whole range of illnesses.
The problem is that cardinal symptoms such as fatigue or pain that are almost ubiquitous in chronic illnesses may offer little insight into a disorder’s underlying pathology. Minor and overlap symptoms, that are downplayed or often ignored, may in fact offer greater insights. It’s possible that neurological symptoms, in particular a condition called ‘sensory overload’ could provide a better ‘key’ to ME/CFS than fatigue and pain.
Sensory overload, of course, is a well-known feature of chronic fatigue syndrome that is described in the Canadian Consensus Criteria for ME/CFS as :
“cognitive, sensory- e.g., photophobia an hypersensitivity to noise – and/or emotional overload, which may lead to crash periods and/or anxiety.”
Cognitive Issues
The Canadian Consensus Criteria Manual also mentions many cognitive problems such as confusion, impairment of concentration and short-term memory consolidation, disorientation, difficulty with information processing, categorizing and word retrieval, and perceptual and sensory disturbances. e.g., spatial instability and disorientation and inability to focus vision.
Note that many cognitive problems in ME/CFS could be impacted, if not caused, by high levels of ‘sensory overload’ interfering with the ability to effectively process ‘outside information’ (i.e. understanding conversations, understanding reading materials, navigating through physical space etc) as well as difficulty processing bodily sensations, which brings us to the question ….. could sensory overload contribute to many of the symptoms found in ME/CFS? The marked reduction in the speed of decision making, frequently noted in ME/CFS, for instance, might be expected if people with ME/CFS are being constantly being bombarded with sensory ‘noise’.
Too much information? – What is sensory gating and what does a deficit imply?
“Sensory gating describes neurological processes of filtering out redundant or unnecessary stimuli in the brain from all possible environmental stimuli. Also referred to as filtering, or sensorimotor gating, sensory gating prevents an overload of irrelevant information in the higher cortical centres of the brain”
Wikipedia
Sensory gating is a basic physiological/neurological mechanism (present in all, at least, vertebrate species) that allows an organism to attend to salient stimuli (from all the senses) important to survival while filtering out routine, on-going and irrelevant signals.
Cocktail Party Syndrome, Seat of the Pants Phenomenon and the Startle Reflex
Three common phenomena that may be disturbed if there is a problem with sensory gating are ‘the Cocktail Party Syndrome’, the ‘Seat of the Pants’ phenomenon and the ‘Startle Reflex.’ Perhaps they apply to you?
In the ‘cocktail party syndrome’ it’s difficult to carry on a conversation with in a room because we have difficulty filtering out the noise of others. In the ‘seat of the pants’ phenomenon we have difficulty attending to the outside world because nerve impulses signalling the body is in contact with a surface don’t get filtered out as they should.
If we hear a loud bang we jump but if the noise is repeated several times and nothing untoward happens then eventually we learn to ignore it through a process of habituation and it becomes just so much more background noise. However, if our brains keep attending to the jackhammer or the door shutting or banging or whatever, again we don’t have much room left to attend to what’s in from of us.
It’s easy to imagine the ‘information overload’ if all these signals and others, reached the conscious mind on an on-going basis.
An important point to note though is that these mechanisms operate at the pre-conscious level. For example a sudden loud noise will elicit a startle response regardless of whether or not we had previously identified the noise as dangerous or harmless. It also appears that the strength of the startle response varies between individuals.
Measures of sensory gating
Two commonly used and related measures of sensory gatingare PPI (pre-pulse inhibition)in which a weaker prestimulus (prepulse) inhibits the reaction of an organism to a subsequent strong startling stimulus (pulse) and determines the strength of the startle response and the ERP (event-related potential) which reflects the habituation of repeated stimuli. Both measures involve recording the brain’s electrical response to auditory, visual or tactile signals.
Sensory Gating Deficits
It may be hypothesised that ME/CFS patients, if tested, would show a deficit in neurological sensory gatingand that this gating deficit may give an insight into many of our common and not so common symptoms.
It doesn’t take very long to identify a fairly long list of neurological/psychiatric conditions in which a gating deficit has been identified. They include Autism; Asperger’s; Bipolar disorder; Post Traumatic Stress Disorder; Alzheimer’s Disease; Obsessive Compulsive Disorder; Huntington’s Disease; Parkinson’s Disease; Fibromyalgia; IBS; Interstitial Cystitis/Painful Bladder Syndrome, Schizophrenia and Treatment Resistant Depression.
Sensory gating problems are also present in Attention Deficit Hyperactivity Disorder (ADHD). High rates of ADHD have been found in Fibromyalgia and just recently in ME/CFS and sensory gating questionnaires were recently proposed as easy diagnostic tools for ADHD. A recent study found a drug, methylphenidate used in ME/CFS can ameliorate sensory gating problems to some extent in ADHD. Methylphenidate (Ritalin, Concerta) is a psychostimulant that increases the levels of dopamine and norepinephrine in the brain. Another psychostimulant study involving Vyvanse found improved cognition and, interestingly enough, fatigue and pain levels in ME/CFS patients (Young, 2012).
Gating issues may produce different kinds of ‘overload phenomena’ in different disorders. Gating problems appear to cause or contribute to pain issues in Fibromyalgia and Interstitial Cystitis, fullness and urgency feelings in Irritable Bowel Syndrome, sensory integration problems in Autism; auditory hallucinations in Schizophrenia; the manic phase of Bipolar Disorder; and cognitive/memory/multi-tasking difficulties (Alzheimers); or ataxia (Huntington’s).
Evidence of Sensory Gating Problems in ME/CFS
in his 1996 book ‘Betrayal by the Brain’ Dr J A Goldstein proposed that a sensory gating deficit played a key role in ME/CFS and set out (in numbing detail) how it could account for many of the symptoms and physiological findings in ME/CFS. Unfortunately, it doesn’t appear that Dr Goldstein has published any research which investigated whether a gating deficit really is associated with ME/CFS.
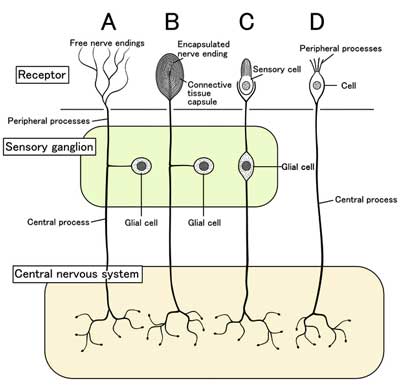
One study (Geisser et al, 2008) found that ME/CFS patient’s brains have trouble turning off their attention to innocuous stimuli. Dr. Baraniuk reported he believes the sensory filtering processes are broken down in this disorder. The Lights propose that sensory ganglia that transmit sensory data to the spinal cord may be dysfunctional in ME/CFS.
A dissertation “Sensory Gating in Adolescents with Chronic Fatigue Syndrome” by EM Van de Putte et al found that adolescent CFS (Fukuda) patients showed a sensory gating deficit using the P50 ERP (sensory) paradigm but not on the PPI ‘Startle reflex (sensorimotor). The deficit only reached borderline significance once they controlled for confounding variables such as age; gender; depression and anxiety. They suggested, however, that co-morbid symptoms of anxiety and depression may mask a gating deficit in CFS.
Another point to note is that in the study that found a gating deficit in Fibromyalgia patients, the researchers used both an auditory and somatosensory stimulus (painless pressure) and significant results were found only for the somatosensory stimulus. It is entirely possible that, while some of us report increased sensitivity to sounds, an increased sensitivity to internal body signals may be a more important test in disorders like fibromyalgia and ME/CFS. Indeed, several studies suggest that an area of the brain called the insula which regulates awareness of one’s body, pain and perception may not be working properly in ME/CFS and fibromyalgia.
Causes
Causes I: Chemotherapy toxicity –A Model for a breakdown in Gating?
ME/CFS patients obviously aren’t typically exposed to chemotherapy drugs but they may arrive at the same endpoints as cancer patients. Chemotherapy is known to often lead to long term fatigue and cognitive problems in a significant number of patients. Studies suggest that up to 50% of cancer survivors exhibit signs of ‘Cancer-Related Fatigue’ and 12% have severe CRF two years after their cancer treatment. Cognitive issues are so prevalent that the term ‘chemo-fog’ (similar to ‘brain-fog’ in ME/CFS and ‘fibro-fog’ in Fibromyalgia) has entered the cancer lexicon.
One assumption has been that the psychological trauma of dealing with a life threatening illness is causal but some evidence suggests the drugs could spark sensory gating and cognitive problems.
Gandal et al, 2008, demonstrated that administering a common breast cancer chemotherapy drug to mice results in significantly impaired ERP gating with reduced sensory habituation, reflected in behavioural changes such as increased pain sensitivity and reduced habituation to novel objects. To quote their discussion:
“In the present situation, gating deficits may underlie the qualitative observations of neurocognitive dysfunction reported in the clinical literature. An inability to filter out extraneous sensory stimuli in the pre-attentive stages of sensory processing could overwhelm an individual with a flood of incoming stimuli and interfere with the ability to mount a selective attentive response to the most salient information”
“Future studies should employ this animal model to probe underlying mechanisms of chemotherapy induced cognitive impairments. While definitive mechanisms for these cognitive changes have yet to be established, there are several potential hypotheses. Leading candidates include disruption of the blood brain barrier, cytokine upregulation and neuroinflammation, DNA damage, oxidative stress, and dysfunction of the neurohormonal axis”
Many of the causes suggested for ‘Cancer related fatigue’ are under discussion in ME/CFS as well; they include inflammatory cytokines, HPA axis problems, alterations in central nervous system serotonergic systems, problems with melatonin secretion, genetic predispositions, problems with energy metabolism and problems with muscular activation.
ME/CFS research also increasingly points to evidence of systemic inflammation/oxidative stress; immune dysfunction and, perhaps to a lesser degree (on the basis of the volume of published evidence), mitochondrial dysfunction.
Causes II: Psychological Stress
Thankfully (for us if not the mice) sensory gating can be readily studied in animal models and the effects of various stressors and their physiological effects elucidated.
It does indeed appear that, in animal models, a sensory gating deficit (PPI) can be induced, by stress induced by Social Isolation Rearing (SIR). The isolation results in increased levels of oxidative stress including increased superoxide dismutase activity, decreased oxidized: reduced glutathione ratio and increased lipid peroxidation in brain regions.
Causes III: Oxidative Stress/Mitochondrial dysfunction
Another study shows that systemic administration of the mitochondrial toxin 3-nitropropionic acid (3NP) induces a similar gating deficit (PPI) to that seen in Huntington’s Disease.
Schizophrenics may provide another clue. A very high proportion of schizophrenics smoke tobacco as a form of self medication as nicotine can help ameliorate a sensory gating deficit and the resulting psychotic episodes. Peroxisome proliferator-activated receptors (PPARs) are important regulators of mitochondrial function and may provide neuroprotection. Watt et al (2004) demonstrated that nicotinic acid could induce the production of mitochondrial regulating PPARs as effectively as exercise.
Further support for oxidative stress and mitochondrial dysfunction playing a role in sensory gating may come from the finding that the antioxidant and glutathione precursor (and glutamate antagonist) N-acteylcysteine can ameliorate sensory gating deficits (PPI) in knockout mice (Chen et al, 2010). While this study was primarily concerned with glutamate metabolism other studies have noted reduced glutathione levels in schizophrenia and that administration of NAC reduced symptoms in schizophrenia (Berk et al, 2008) and bipolar disorder (Magalhães et al, 2012).
Causes IV: Genetic Risk
Many now consider Bipolar Disorder and Schizophrenia to be the same or similar conditions and both show an associated sensory gating deficit. Dopamine is believed to play a key role in these conditions. In a large study of dopamine metabolism associated genes , Ancin et al, 2011 found that a particular polymorphism of the COMT gene was associated with Bipolar Disorder and the associated gating deficit (P50 ERP).
The 2011 Wyller study linked COMT gene alterations (rs4680) in adolescents with increased sympathetic nervous system (‘fight or flight’) activity and both Light studies have shown increased expression of the COMT genes after exercise.
Although it now appears that attempts to link a single genetic polymorphism to a particular disease were overoptimistic, it does appear that individuals who carry the COMT val to met mutation and in particular the low COMT activity met/met genotype may be predisposed to greater pain sensitivity and a loss of higher cognitive function when put under stress. It may be that ME/CFS patients carrying the met allele (particularly met/met) are more likely to experience higher levels of pain and/or cognitive fatiguability and may represent a sub-set with greater overlap with Fibromyalgia symptomology. The same genotype also appears to represent a risk factor for developing ADHD in males only.
Note that the loss of cognitive functions and increased pain sensitivity are to be expected when sensory overload is present.
Focus on Immune Dysfunction, Oxidative Stress and Mitochondrial Dysfunction
Returning to those conditions already associated with a sensory gating deficit, a quick search (Pubmed and similar sources) finds that immune dysfunction, oxidative stress and mitochondrial dysfunction are often found in these disorders. (Only those terms were used rather than specific markers such as TNF-alpha or terms such as glutathione so papers may easily have been missed).
An asterisk indicates that a positive association has been reported.
| Immune dysfunction | Oxidative stress | Mitochondrial dysfunction | |
| Schizophrenia | * | * | * |
| Autism/Asperger’s | * | * | * |
| Bipolar Disorder | * | * | * |
| PTSD | ? | * | * |
| Alzheimer’s | * | * | * |
| OCD | * | * | * |
| Huntington’s | * | * | * |
| Fibromyalgia | ? | * | * |
| IBS | * | ? | Under research |
| Interstitial Cystitis | * | * | ? |
| TR Depression | * | * | Suspected |
| Parkinson’s | * | * | * |
| ADHD | Suspected | Suspected | Suspected |
Psychiatric Disorders or Neuroinflammatory Ones?
It appears that many of the illnesses previously regarded as ‘psychiatric’ are increasingly explained by underlying neuroinflammatory pathologies that may be amenable to treatment with no need to resort to ‘theories of the mind’.
A recent paper reviewing trends in Autism Spectrum Disorder research over the past 40 years concluded that there had been a move away from traditional areas such as neuropathology and ‘theory of mind’ and a rapid increase in papers on immune dysfunction/inflammation; oxidative stress; mitochondrial dysfunction and environmental toxin exposure; that a high proportion of papers confirmed a link and were of increasingly high quality.
They also noted similar associations for other psychiatric/neurological disorders :
“Immune dysregulation and inflammation has been implicated in several psychiatric disorders”. For example, “neuroinflammation, which generally refers to CNS-specific, chronic glial reactions…. has been implicated in several psychiatric disorders,including Alzheimer’s disease,schizophrenia, bipolar disorder,and depressionas well as ASD.”
These are not isolated observations. A further review (Bitanihirwe and Woo, 2010) discusses the rationale for and effects of treating Schizophrenia with antioxidants :
“Currently available evidence points towards an alteration in the activities of enzymatic and nonenzymatic antioxidant systems in schizophrenia. In fact, experimental models have demonstrated that oxidative stress induces behavioral and molecular anomalies strikingly similar to those observed in schizophrenia. Recent clinical studies have shown antioxidant treatment to be effective in ameliorating schizophrenic symptoms. Hence, identifying viable therapeutic strategies to tackle oxidative stress and the resulting physiological disturbances provide an exciting opportunity for the treatment and ultimately prevention of schizophrenia.”
Dantzer et al (2009) reports on recommendations from a multidisciplinary conference held in 2007 to consider how best to identify and treat medically ill patients with a range of conditions in which inflammation played a key role in the symptomology.
“The most harmful and costly health problems in the Western World are originating from a few diseases that include coronary heart disease, cancer, obesity, type II diabetes, physical disability and neurodegenerative disorders associated with ageing. In addition to the specific symptoms that are characteristic of each of these conditions, most patients experience non-specific symptoms that are similar in all these conditions and include depressed mood, altered cognition, fatigue, and sleep disorders.”
Conclusions and….Treatments (?)
Concentrating almost exclusively on fatigue and/or pain whilst ignoring minor and overlap symptoms may only serve to ‘ring-fence’ ME/CFS research in a way that is artificial and unproductive.
There are tentative findings that a sensory gating deficit is also associated with ME/CFS. This is a testable hypothesis that, if confirmed, might suggest common physiological aberrations and understanding the pathology of these other conditions may help unearth the core pathology of ME/CFS.
Research is increasingly implicating oxidative stress in a wide range of neuroinflammatory conditions as it is with ME/CFS. These conditions are all associated with a neurological sensory gating deficit which may be induced by oxidative stress.
Interventions to attenuate oxidative stress have shown promise in a number of conditions. Additionally, it’s not uncommon for drugs to find uses well outside of their originally intended use.
Trazodone, a commonly used sleep drug in ME/CFS is also used, for instance in central nervous system degenerative diseases (behavioral disorders in dementia and other organic disorders), schizophrenia, chronic pain disease and diabetic neuropathy and sexual dysfunction.
An anti-psychotic, Quetiapine, used in the treatment of schizophrenia can enhance sleep in healthy people and is suggested as a sleep aid and pain reducer in fibromyalgia and ME/CFS. Clozapine (an antipsychotic agent used in the treatment of Schizophrenia and off-label for Bipolar Disorder) reverses the gating deficit produced in rats.
As a final example, it appears that a number of antidepressants also have the effect of reducing inflammatory cytokines and the reduction in depressive symptoms may be due to this anti-inflammatory action.
More importantly, given their vastly greater levels of funding, a major breakthrough is more likely to come from research into one or more of these other neuroinflammatory conditions. One promising candidate is the gene RORA which is involved in several key processes including brain cell differentiation; protection of neurons against chemical stress; suppression of inflammation and regulation of circadian rhythms.
RORA has already been implicated in bipolar disorder, ADHD, depression and autism and lately variants of the RORA gene have been shown to be a risk factor for developing post-traumatic stress disorder. Of particular interest is the RORA gene’s responsiveness to sex hormones which has been proposed as the explanation for gender prevalence differences in ASD.
Please Support This Author and Health Rising!
Forty Percent of Paypal Donations Go to the Author of this Blog








I have had sensory issues all of my life. They have continued to worsen the older I get and I have often wondered if they were not the underlying cause of my near complete physical collapse from CFS/ME several years ago. Or if not the cause, then a huge piece of the puzzle. I have explored the possibility of Asperger Syndrome (soon to be subsumed under Autism in the new DSM-5) as so many people on the spectrum have co-morbid Sensory Processing Disorder. I haven’t come to any conclusions. But it is clear to me that the my fatigue and sensory issues are inextricably linked.
Thank you for your article. I look forward to further installments.
I think there’s got to be something to this. Studies, after all, show that the brains of people with ME/CFS have difficulty releasing themselves from tracking ‘innocuous stimuli such as background noices. That in itself- that need to try and track numerous streams of input is fatiguing… Dr. Lights research suggests our sensory systems may be flooding the brain with stimuli. If he’s right then attending to normal, everyday matters in the face of that would be draining and difficult. I expect it could even account for coordination problems since studies have now shown that cognitive issues can effect such things as coordination. Sensory processing disorder looks interesting – I’ll have to check that out.
Interesting “Blog”. I think it’s essential to approach this horrible illness from any angle keeping in mind that they are all integrated somehow. I’m not sure I would call fatigue an “easily understood aspect” of any disorder. I don’t believe that even since polio there has been adequate understanding of “fatigue.” Certainly I don’t believe that even 99+% of the best CFS/ME Physicians really understand what we are going through when we talk about fatigue. Other than adrenaline type medications, which will often just lead to post-exertional malaise in most, it is the hardest aspect of the disease to treat.
Any way to make use of other studies and other findings to help our cause is a godsend!
Thanks,
Marco
I had trouble with that sentence; I meant to say that it was the most easy part of the disorder for the scientific community to hang a handle on- hence the name chronic fatigue syndrome. It took them years and many are still trying to get ‘post-exertional malaise’ into their understanding – which is the key aspect of fatigue that differentiates ME/CFS from many other disorders. So even while trying to grab hold of the disorder at its most approachable characteristic it still slipped away.
Acquired mitochondrial myopathy (and a bunch of other acquired stuff) due to methylation issues would be a better description.
Mitochondrial dysfunction definitely features in the neuroinflammatory ‘vicious cycle’ which should become clear in the sections to follow.
Whether or not mitochondrial dysfunction is the driver of neuroinflammation or a result is the question!
Forgetting the title of the article…migraine headaches tend to leave people EXHAUSTED. Also, in common with CFS/ME is nausea and dizziness, even at times when a person is not having a headache…and a host of other things I’m sure I am not thinking of.
I can also relate to feeling sensorily overwhelmed – to touch, sound, light and smells all my life. No matter how unwelcome the link is in discussions of CFS, it is undeniable that many, though not all with CFS, have been exposed to some form of trauma in early life. The association of CFS “with trauma or reported high levels of co-morbidity between PTSD and CFS (Dansie et al, 2012)” may be partly a result of underestimating the impact of trauma and its escalation into chronic PTSD. There is evidence that a “range of neurobiological abnormalities are beginning to be identified in [traumatised children]” (van der Kolk, 1994).
I was a witness to domestic violence for my first 17 years. My CFS is not “all in my head” and I do not see myself as victim of abuse. It is simply a reality that my developmental years were spent in the highly neurologically aroused state that was necessary for my survival. Your hypothesis may help to elucidate the intuitively obvious body-mind link, though your emphasis, so far, is on medications and social isolation rearing as triggers for a sensory gating deficit.
It makes sense that any trauma, be it physical, mental or emotional could lead to a hypervigilant neurological response: it would be a protective response in the short term. It has been shown that trauma causes “lasting changes in neuronal excitability and enduring behavioural changes in the direction of either fight or flight.” (van der Kolk, 1994).
Behaviour is a response to environment, be it external or internal – neurological, endocrine, and so on: physiological.
CFS and chronic PTSD are strongly related. Kolb (1987) proposed that trauma may result in neuronal changes that undermine stimulus discrimination. Sounds like a sensory gating issue to me.
Interestingly, Yehuda et al (1991) described HPA axis dysfunction in PTSD.
Thanks Maree…
Early life trauma is controversial as many do not experience it; I’m happy to say that I didn’t have that burden to deal with but I was surprised at a Chronic Pain Workshop to see early life trauma, in whatever form, is being studied in FM, IBS….it seemed like all the disorders that are typically allied with ME/CFS. It is possible, as you note, that for other that short-live trauma’s whether they be infection (CFS, FM, IBS) or accidents (FM) or whatever somehow set off this disorder in others…and if the stress response is a key player as the disorder evolved it would make perfect sense that a system that was turned on initially was the one that got whacked seemingly permanently. In Dr. Klimas’ CDC talk she noted that the autonomic nervous system – one of the two major branches of the stress response – was the first system to go haywire when people exercise and that it was the ANS that trigger the immune cascade that triggers the inflammation.
hi Marie,
I’m sorry for your difficult childhood.
Trauma is associated with a higher incidence of disease in general. There is no particular link between ME/CFS and childhood trauma–some people like to publish about this but they don’t generally use other disease control groups. When they do, ME/CFS is no more likely than any other disease to be associated with childhood adversity.
Taylor RR, Jason LA. Sexual abuse, physical abuse, chronic fatigue, and chronic fatigue syndrome: a community-based study. J Nerv Ment Dis. 2001 Oct;189(10):709-15.
“Compared with healthy controls, childhood sexual abuse was significantly more likely to be associated with outcomes of idiopathic chronic fatigue, chronic fatigue explained by a psychiatric condition, and chronic fatigue explained by a medical condition.
“None of the abuse history types were significant predictors of chronic fatigue syndrome.
“A closer examination of individuals in the chronic fatigue syndrome group revealed that significantly fewer individuals with CFS reported abuse as compared with those who did not.” [i.e. it is not “many” or a large percentage of us; it is relatively few of our number–though any amount who have been through this is of course too many]
http://www.ncbi.nlm.nih.gov/pubmed/11708672
This study is from Dr. Jason’s work group, and it is the best study on ME/CFS and abuse because Jason knows how to perform differential diagnosis (i.e. differentiate ME/CFS from idiopathic chronic fatigue, Lupus, MDD, MS, celiac disease, etc.) and use control groups (both typical failings of many CFS studies).
Of course, correlation doesn’t prove causation. The fact that childhood trauma is associated with increase in disease doesn’t necessarily show that it contributes directly; it could be emotional trauma as suggested (Marco mentioned a possible pathway for this and Martin Pall also has one), or there could be shared risk factors (homes with abuse may tend to be dysfunctional in other ways, and it could be some of the other ways, such as poor nutrition or disrupted sleep) rather than emotional trauma itself, which produce the increased health risk. We don’t have an ethical and elegant way to test this, so we don’t really know.
What we do know is that not all people who suffered abuse go on to develop the same or even any health condition. We also know that most people with ME/CFS and many other health conditions did not experience these types of adversity.
This doesn’t make your experience unimportant. Certainly it may have impacted you a lot and perhaps you can help others who have been through similar.
all the best.
Thanks for your thorough response JW – fascinating reading. I didn’t know about Taylor and Johnson’s important work. I will look further at Martin Pall’s stuff with great interest 🙂
Hi Maree
The links with PTSD I feel are very suggestive but like Cort I can’t point to any particular trauma and in fact had a fairly happy childhood environment. What I have had is a lifelong high level of anxiety even prior to the onset of physical illness.
Apparently there is also a high rate of ‘co-morbid’ PTSD in fibro patients.
The onset of PTSD in chemo patients may give a clue. While it can be shown that chemotherapy can cause a gating deficit not all chemo patients develop the symptoms of PTSD and only a minority develop full blown PTSD.
Likewise not all survivors of traumatic events develop PTSD.
Which suggests to me that developing PTSD and related conditions depends on both exposure to a stressor and a predisposition to this neuroinflammatory state.
Thanks Marco, I am looking forward to the next instalments!
I had been having peculiar symptoms of balance problems with nausea and dizziness for quite some time (years) and worsening in the last few years, and I have recently been diagnosed with migraine headaches. I have never suffered from migraines prior to being diagnosed with me/cfs and fms. It seems as though our systems are over reactive, as certain odors and scents or lights and sunlight will cause me to feel as though I will pass out, give me the shakes, palpitations and nausea. As someone stated, if speaking with one person, it is easier to follow the conversation, but when in a room full of people, I tend to tune out.When there are too many people I tend to hear a lot of buzzing, and all that conversation really exhausts me so that I don’t understand one word that is spoken, but as my hearing is almost at 100% it is a cognitive problem not a hearing problem.
I’ve been sick for over 15 years and battling insurances and the government all this time and have just now managed to get approved for disability. These are horribly complicated illnesses to get.Your life is changed forever overnight and no doctor or friend/relative believes that you’re ill because you look healthy. It’s up to us, the patients, to keep informing ourselves and to keep fighting. Thank you, Cort, for all the information I got from your writings, it gave me lots of information and ammunition and courage to keep fighting for my rights.
Thanks Annie and thanks to Marco for illuminating such an interesting subject that I knew little about. I imagine there may be a really large number of people who are getting thrown into one kind of disorder or another depending on the kind of doctor they see but the essential conditions…some sort of stimulus overload…. some central nervous system problem that goes bananas in the face of some kinds of stimuli – is common.
The migraine connection is really intriguing given how many symptoms (I just found out from the past comment) are similar. That connection was proposed years ago by two UK neurologists whose names escape me, but who failed to get more funding to pursue it…
Hang in there Annie!
When reading this post, I’m reminded of the importance of subgrouping ME/CFS. For me, sensory issues are a problem, but I see them as secondary to my flu-like, PEM dominated ME/CFS. I’m a typical post-infectional ME/CFS patient, feeling like I always have an infection in my body. “Fatigue” or energy deficiency is one of my core symptoms.
I read in Marco’s profile that “General ‘fatigue’ has never been a major problem for me”. Very different from my experience! I really wish ME/CFS researchers begin to get the hang of subgrouping soon, so that we can get studies going on the different types of disease within this umbrella. (Marco, do you fit the CDC Fukuda and Canadian criteria for ME/CFS?)
I feel that “my ME/CFS” is more related to chronic infection, or to autoimmune diseases like Sjogren’s syndrome or SLE – and not at all to for example autism or Aspberger’s.
My conclusion: We’re all so different – maybe my disease is a different animal compared to yours, Marco!
Hi Emma
Yes I fit CCC to a T – but sporadically!
Plus my symptoms have also ‘morphed’ over time. For many years I had that feeling of ‘something’ in my bloodstream but can’t point to an infectious onset. Now it feels like constant inflammation that increases as the day goes on.
Why I stated that fatigue didn’t apply to me is that most of the time I just feel ill and inflamed and have severely limited mental endurance but as long as I don’t overdo it for most of the time I’m pretty much physically functional.
If I do overdo things physically or mentally I can end up pretty much bed bound within minutes. It hits me like a seizure. One minute I can walk, talk etc just fine and the next I can’t stand, walk, think or talk.
Perhaps its just a matter of terminology but this doesn’t sound like fatigue to me.
Emma,
I, too, am often struck by the heterogeneity of the group of illnesses labelled as CFS/ME and see them “clustering”. I had an acute onset of an illness, following a viral illness and for many years, that was how I would describe how I felt. If I were trying to give a healthy person some idea of “what it was like to be me”, I’d say something like, imagine having a really bad flu, ALL the TIME. It gets better, it gets worse, but it never completely goes away. And no matter how much sleep you get…you wake up…achey, exhausted and as sick as ever. I would say I am always exhausted.
I also wonder how long you have been sick. Many people use the word “morph” or something similar, to describe how their symptoms evolve over time. Whether this is a function of the disease’s process affecting our various systems, I don’t know. I first got sick in the latter part of 1983. I was VERY sick, I thought. But through dogged determination, I was able to complete a psychiatric residency and fellowship, get married, have a baby, go into private practice. It was not easy! I felt like everything was harder for me than “healthy” people and early on I knew no one that had what I did.
But, my symptoms have evolved and I wonder if other people’s have. I have more trouble processing information, more cognitive difficulties, concentration issues…and have become much more “sensitized” to, well all the “senses”. While I had some of these issues, I now cannot walk through a grocery aisle with laundry detergent without becoming nauseated, people’s perfume makes me sick, I have to wear sunglasses a LOT. I went to a movie theatre for the first time in awhile and when a trailer came on, everyone else calmly ate their popcorn and I jumped out of my seat repeatedly. I was SHOCKED at the volume and my reaction was involuntary. I think I always had normal hearing, now when I try to go to sleep, I hear the hum of a television that has been turned off, my son’s computer (that he is not using, but has power to it) way down the hall.
A flash of light coming off glass or water (we live near the ocean) can cause a stabbing pain in my eyes even if it does not precipitate a full blown migraine. I have developed ANS changes, dysregulation if you will and also things that seem to be brainstem issues, such as balance problems…other neurologic problems such as parasthesias in extremities.
So, I guess I am hypothesisizing, that I was a “typical post infectional ME/CFS patient” that now has a lot of other, mostly CNS related problems. But I also have characteristics in common with Eehlers danlos syndrome, a connective tissue disorder that is probably autoimmune. So, over nearly three decades, this “syndrome” has changed, at times, I feel like an acute viral picture is the most pressing problem, at others, my cognitive problems are, at others, pain is.
And YET, I agree with you that there seem to be some people who seem to have a cluster of symptoms that predominate and seem to be an overlapping but somewhat different symptom cluster. I guess I think IT’s COMPLICATED and possibly the clinical picture, like with most chronic illnesses, changes over time. Ours is just even more hard to find the “underlying unifying feature!”
Thanks for an interesting article, Marco. I think it’s important to remember, though, that a lot of people with ME don’t have these sensory overload symptoms. I read your list of questions and answered ‘no’ to all of them and yet I have acute viral-onset ME, and fit all the tightest diagnostic criteria including the CCC and ICC. I think you’re talking about a subset here. Is there any data on what percentage of PWME have these sensory overload symptoms?
Hi Sasha
I hear what you’re saying. Those questions were taking from questionnaire dealing with sensory issues in schizophrenia where visual and auditory sensory inputs are problematic. Apart from the issue with dealing with hearing in crowded environments I don’t have much of a problem with noise or lights either. What I do have is a sensitivity to tactile stimuli.
But sensory overload also includes cognitive processing, somatic sensations, pain etc so there is the possibility that these are examples of sensations not being filtered out but not recognised as such.
You may be right of course that we are talking about a ‘sub-set’ distinct and different from those with a post-viral onset and we’ve all just been lumped together under the generic title of ‘fatigued’. As stated elsewhere I prefer to think about individuals rather than sub-groups but this is more a matter of personal philosophy.
I do hope later to try to make a case that the same core pathology underlies ME/CFs and other conditions regardless of onset – I lay be unsuccessful.
But if there is indeed a discrete subset as I described then that at least is a step forward for what may well be a substantial minority of those currently lumped in as ME/CFS. Also better for the remainder if this model doesn’t apply.
As regards percentages who may have these ‘sensory’ issues it hasn’t been studied as yet as far as I’m aware.
Hi Marco, and thanks for the considered response.
I’m not suggesting that some people with acute viral onset don’t have symptoms of sensory overload – I was really trying to say that I seem to be what would originally have been a ‘classic’ case of ME, including the viral onset, and yet didn’t have these symptoms of sensory sensitivity.
I think it would be controversial to categorise cognitive processing, somatic sensations and pain as ‘sensory overload’. If you broaden out your definition that far then I think you will include most ME patients but I don’t think that would be a widely accepted definition of sensory overload.
The cardinal symptom of ME used to be not ‘fatigue’ but ‘post-exertional malaise’, defined as a worsening of symptoms caused by trivial effort which appeared with a delay of up to 48 hours after the inciting event. The Drs Light have demonstrated this very nicely with an exercise-provocation test. ‘CFS’ bundles a lot of people together in a very ill-defined way who probably have a lot of different diseases.
So I still think you’re talking about a subset but that’s not to say that it’s not important to talk about subsets. If you can clearly identify a subset and get to the bottom of their problem that’s a huge achievement.
I think you’re right that post-exertional malaise is currently the best signateur (if that’s a word :)) of ME/CFS Sasha…Even there, though, we run into some difficulties with some people who experience it not demonstrating metabolic abnormalities on the 2-day VO2 max exercise test – so its sound like there will be subsets within that..
My problems with external sensory overload are present but I wonder more about internal sensory overload; overload coming from bodily signals. I’m very much taken with Dr. Lights work and the idea that pain and other signals interfere with cognitive processing; ie I’m not as clear as I could be because my brain is constantly attending to and trying to figure out what to do with all these internal signals.
It’ll be interesting to see how it all fits together and I’m glad Marco is keeping an eye on the sensory gating field..
Cort, I like the word signateur a lot but I think maybe you are trying to say “signifier.”
Personally I can’t decide whether my aphasia or dysphasia is worse.
By the way, Dr. Russell Blaylock writes a lot on excitotoxins in our diets. Such as MSG and aspartame.
Hi again Sasha
Perhaps sensory ‘overload’ was the wrong term to use in the context but cognitive processing, somatic sensations and pain are very much what I would propose are affected by a breakdown in sensory gating and the ability to distinguish ‘signal from noise’ and are probably of more relevance to ME/CFS than some external sensory input. As I said in the piece, fibro patients show impaired gating in response to skin pressure but not to an auditory signal so gating deficits can manifest themselves through different sensory modalities in different conditions.
But I would also expect that these unfiltered sensory inputs do also contribute to a state of ‘overload’.
Re cognitive processing this will be covered more in Part II including ‘mental fatigue’.
Here’s a little excerpt :
mental fatigue :
“a decreased ability to intake and process information over time. Mental exhaustion becomes pronounced when cognitive tasks have to be performed for longer time periods with no breaks (cognitive loading).”
and :
“In addition to the fatigue itself, the patient with mental fatigue often suffers from loudness and light sensitivity, irritability, affect lability, stress intolerance, and headaches”
Hi Marco – thanks for that, I’ll look forward to reading your next articles!
A quick thank you to Marco (and Cort) before slowly taking in. It is so refreshing to see (with all the well known pathologies) this article putting the pieces together.
Thank you all for the comments so far (and thanks to Cort for ‘fielding questions’ in my absence).
What’s clear is that we all experience our illness(es) differently. Some can point to traumatic events, some can identify ‘prodromal’ symptoms and some can point to a clear post-viral onset.
This I find very reassuring. Some may have guessed by now that I’m not a great fan of diagnostic ‘labels’.
What I hope to set out in the sections to follow is that a single neuroinflammatory mechanism underlies ME/CFS and a number of other ‘neuroinflammatory’ conditions.
This mechanism is overlaid on top of a range of individual differences in genetic predisposition, developmental stage, environmental ‘stressors’ and perhaps even gender and the range of symptoms we then develop – as individuals – determines what diagnosis we end up with.
Even amongst those who meet strict criteria for ‘ME/CFS’ I’d expect that our experiences differ widely and I’d also expect many to have symptoms that would be considered ‘atypical’ of ME/CFS.
If this makes sense?
I’m very interested in this topic as my daughter has been ill for 14 years and presently lives in a partially soundproofed room to enable her to function. She is not on any medication but has managed in this environment to make some improvements. She remains very sensitive to , I think, certain tones and repetitive sounds. For example, last night I pulled a Velcro fastner apart on a hot water bottle cover and her back jerked with after waves of jerking following for a few seconds. The sensory problems are what prevents her from functioning. I will read with great interest the next sections of the presentation. Thanks.
Fascinating Linda – and very distressing for your daughter. My sympathies to you both.
Have you ever looked into ‘stiff person syndrome’?
I’ll be covering this in Part III but the key feature is sudden muscle spasms – usually in response to sharp noises.
I haven’t heard of stiff person syndrome but she does talk about feeling ‘tight’ and as if the jerks release this. I will investigate it further thanks.
Linda
I should mention that this is an extremely rare disorder (one in a million) but it may give some insight into what is going on with your daughter.
Just thought I’d mention Dr.Chaudhuri’s findings on autopsy of people with ME. He found the presence of dorsal root ganglionitis, which I was very interested in as a possible explanation of my daughters symptoms. Linda
Aha! Thanks for that Chaudhuri and Behan were the two neurologists who postulated that ME/CFS had connections to migraines in the early 2,000’s because of their similar symptoms and what they believed were the relapsing/remitting nature of both disorders. Thanks 🙂
Very interesting Marco – yes to your questionnaire and rider but suspect in my case smell and taste abnormalities were related to deep infection (sinuses perhaps). A great believer in the Canadian Consensus (having experienced most – presenting and/or persisting at different times) a “cardinal” is indeed difficult – fatigue in common parlance a misnomer to my mind, might accept clinical fatigue as the inertia is so profound as to be barely functioning at all physically and cognitively. I see your Neuroinflammatory Model as very exciting. Sensory overload (gating problems) especially. Though this has eased for me I note an inability to source the origin of sounds suggesting some permanent damage. At the moment PEM appears if I move out of an “envelope”. Your model could encompass all things “neurological” as I suspect in my case this was where the whole problem began – an infection – with the ability to cross the BBB and wreak havoc in the controlling systems in the (brainstem ?). Looking forward your next thoughts in our hunt to unravel.
Thanks Enid
Glad you got something out of it.
‘Fatigue’ is definitely a misnomer as far as I’m concerned also.
Funny you should mention not being able to ‘source’ sounds.
It appears that people with sensory processing problems can be either hyper or hypo sensitive.
This checklist is aimed at children but you can get the gist of it :
“Hyposensitivity To Sounds (Under-Registers):
– appears confused about where a sound is coming from”
http://www.sensory-processing-disorder.com/sensory-processing-disorder-checklist.html
I’m also glad that you’re sticking with the blog. Personally I find the next bit more interesting where it gets into what may be causing these sensory issues.
Yes. At last. I am so weary of physicians telling me that they are ‘tired, too’. This disease is not about being tired. Neuroinflammatory is right on from where I sit and suffer. Thanks.
Hi there yes it all resonates positively!!!
I have spoken to Dr. Don Staines (see ME Invest’s London conference 2012) on a number of occasions about his theory it explains the inflammatory response and the symptoms that ME sufferers have!!! Don and Sonya Marshall have the theory that explains it all – malfunction of the vascoactive peptides———- they just need funding to test it!!!!
So frustrating that the world seems to be focussing on one or two symptoms when a theory that explains it all is not being tested/investigated!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
Once you use a strict diagnostic criteria like the International Consensus Criteria 2011 – you have a group of patients with incredibly similar symptoms!!!!!!!!!!!!! Weird and wacky symptoms!!!!! When such a diverse range of people with such a wide range of different events triggering the disease all have a similar range of symptoms there must be ONE KEY malfunction somewhere in the body. Is it as Don thinks the vascoactive peptides (not taught at medical school – so go bio-chem).
I really hope they get the opportunity to prove their theory. Vasoactive peptides would effect the blood vessels which play a key role in autonomic nervous system functioning. It could be that blood vessel problems (inflammation) in different parts of the brain trigger different kinds of symptoms (leading to different diagnoses)…Baraniuks brain proteome paper of 7 years or so ago postulated blood vessel breakdown associated, I think with increased oxidative stress and amyloid particles played a role…I’ve got to think the blood vessels play a key role somehow…
Ritchie Shoemaker the mold guy has been working on that hypothesis for some time. He calls it chronic inflammatory response syndrome and believes a driving factor is low VIP. He has been prescribing VIP to his patients for several years. He claims great success but it’s very hard to find people who have been helped.
Dr. Delgado of Spain has done a lot of research in this area:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2730848/
Thanks very much, Marco, for putting all this research together. My experience having fibromyalgia and ME/CFS for nearly a decade now definitely supports your hypothesis. It’s incredibly debilitating not to be able to screen out unwanted sounds, light and smells. They actually feel like they hurt. For me, thank God, it’s not 24/7, but frequently I’m overwhelmed by things like the hum of my husband’s car in idle mode or the smell of a mildewed rag on the back porch, rooms away from me. My response is very much like a startle response. I find myself putting my fingers in my ears and yelling out, “Put the car in gear, please put the car in gear now!” Many times a single candle in a dark room is too much light. And, perhaps oddly, I am often comforted in an out-sized way by a wonderful smell–like the tea olives by the front door, or by blocking out all light with my eye mask, or by getting away from noise. Living with this disease has definitely made me a pilgrim in a strange land. I’m simple now and entertained by simple things. I laugh easily, and cry easily, and feel that I live in a world of geniuses and amazing athletes.
Cort mentions blood vessel involvement and I do recall a period when the nurses were trying to take blood samples “complaining” they couldn’t find a vein – it was as they had “shrunk” and I finished up black and blue. At the same time my heart would slow or suddenly take off at the rate of knots for no particular reason – so yes Cort a definite vascular problem I agree.
Fantastic article. I may not agree 100% but it does not matter.
What matters is that sometimes things need turning upside down, shaking and looked at from the other side.
Cognitive problems, and their severity do vary, but as a carer who has attended social events where many M.E patients are often together in one room so to speak, it can actually be quite disturbing to see how the cognitive problems come to the foreground. If you were a fresh faced medical student and you had to guess what united the people in the room, you would firstly think some nuerodegenerative process must be going on, and that this is affecting ‘minds’ as much as bodies. You would think, my god, what is happening to these people?, everything is slowed down, the normal hubbub of social intercourse is measured and wound down in some way.
Anyway, as a general point, sometimes research into M.E has to take a step back sometimes since in many ways it can find itself bogged down in the minute details of universal disease processes that apply to nearly all immune responses – cytokine pathways, immunoglobulins etc. Not that this is not useful of course, but ocassionally it is like people pondering to much on why peoples bodies ache with the flu, while having entirely missed the virus in the throat.
Not a brilliant analogy I know – but you see what I am getting at – we need to keep and eye on everything, and keep looking again at all of the main symptoms in broad strokes, until we see what patterns the constellation spells out, and keep reminding ourselves of the basic presentation.
Good stuff.
Many thanks for your kind comments David.
I’m glad you don’t agree with everything I’ve said. The reason for putting this out to the community was to test if it resonated with others or was just viewing ME/CFS through my own personal lens.
I also agree that we can get bogged down in minutiae and sometimes need to take a step back (in time as well as perspective) and I’m the first to admit that I don’t have the background to get deeply into the biology/neuropsychopharmocology of all this.
I do hope others chip in to support or refute my suggestions.
What I will say is that sensory processing problems, while important, have turned out to be really a vehicle to link ME/CFS to other neuroinflammatory conditions which have turned up a potentially common pathology underlying many psychiatric/neurological conditions. I think (or hope) you’ll find part II of interest where I’ll get to what I feel is the core problem.
All of which is hypothetical of course. if only I could interest some researcher to test it!
Regards
Marco
Marco – a few uneducated thoughts not wanting to detract from your “overarching” model with vascular – amongst many other – problems which Wikipedia well describes under the autonomic nervous system (situated in the brain stem). I was diagnosed (MRI brain scan) with patchy “high signal changes – whatever that is. So a neuro modelling sits happily with me.
Hi Enid
A very timely comment as I’m currently tidying up the final part of the ‘series’ – trying to tie everything together including dysautonomia/POTs etc.
Our HPA problems can certainly potentially stem from the model outlined as glutamate and GABA (next up in Part II – Cort permitting) are the ‘yin and yang’ of the HPA response to stressors.
I’m told I have ME, I don’t have any sensory symptoms. I do have severe headaches if I try to undetake much physical activity (like going up more than one flight of stairs). I’m quite sure there are subgroups of ME patients!
Having said that I suspect that neuroinflammation is behind at least some of my problems.
Hi tatt
Headaches of a new type are certainly one symptom of ME/CFS. However; and this is my own personal view and I’m not sure what others would think, from my own experience I would resist any diagnosis of ME/CFS as (in the UK at least) this equates to no further investigations and no effective treatment.
I’m sure there are many potential causes of headaches following (minimal) exertion, some of which may not be quite a benign as ‘benign myalgic encephalomyelitis’.
If this diagnosis is being made by a doctor I’d personally insist on excluding every other possibility before even considering ME/CFS.
FWIW – in the context of this model, glutamate is also implicated in migraine :
http://www.achenet.org/decreasing_brain_excitability_with_migraine_therapy_targeting_glutamate/
Thank you for this. At last! Sensory overload given the place it deserves. My story started 43 years ago and the first symptoms were those of sensory overload and balance/ co-ordination problems, the latter accentuated according to the level of background stimulation. In those days the fatigue was less of an issue though it has become much more prominent since then, but never ever the worse symptom of my long illness history. In fact the fatigue is always been the least worrying symptom I’d argue, for me at least!
As time has gone on the level of sensory overload has dominated, and depsite not generally having a great deal of pain associated with my ME (2 solid years of very bad IC were horrible but ‘doable’ and continued IC is just part of life as is IBS etc), in the last 12 months I have devolped very severe allodynia pain from head to foot. It * seems* to have been triggered by a severe cat allergy (I may be wrong there..but cause and effect seemed to tally) and I’d be incredibly interested about any links this author might have connecting his theory to allergy. I have become steadily more allergic or sensitive to all sorts of things as the disease has progressed. If this theory could take us nearer to decent pain relief for neuropathic pain (treatment which didn’t result in the side effeect profile of the present alternatives) then that would make a huge contribution to the illness.
I hope others will continue to research this aspect of the illness. I’m inclined to agree that’s it’s presence is the defining element of authentic ME: the ‘fatigue stuff’ is the red herring which takes people off message and enables others to misdiagnose on a mammoth scale.
Hi Rosie – thank you for the comments.
43 years is a very long time indeed!
Your story sounds very like mine. Fatigue as such has been pretty much a non-issue and whatever pain I’ve had (joints, limbs) has been manageable and IBS is just a constant way of life now.
Neuropathic pain inc allodynia has been a recent development for me too. Mostly affecting my eyes and hands but I had an acute attack of allodynia a few weeks ago when I awoke, put on a cotton shirt and immediately felt as if my back was covered in barbed wire. A first for me and I thought the shirt might have picked up something around the garden Of course a clean shirt made no difference and this sensation gradually declined but lasted two days in total.
Regarding allergies – at the moment I’m tending to lump it in with the general hypersensitivity to sensory input. I’m very sensitive to certain smells (gloss paint etc) and meds. I could suggest that our reported ‘exquisite sensitivity’ to meds may be that even relatively minor physiological changes related to meds are not screened out like they should which just stokes up the inflammatory cycle.
I have to admit its not something I’ve looked deeply into as the scope of this enquiry is already very broad.
I can think of a few alternatives.
Given the close interconnections between the brain and immune system I’d be very surprised if there isn’t some interaction between mast cells and neurotransmitters.
Another possibility was suggested by someone else (on another forum) – the gist of which is that the sinuses are anatomically very close to the amygdala and given the evolutionary importance of the sense of smell it is likely that there are pretty direct connections between the sinuses and the sub-cortical brain structures that are involved in ‘fight or flight’. They suggested that any inflammation in the sinuses might stimulate glutamate release from the amygdala, again stoking up the neuroinflammatory state and hence could lead to an exacerbation of other symptoms.
Sounds plausible to me but not something I’ve yet worked into the model.
Re neuropathic pain – some people swear by alpha-lipoic acid and I also feel that glutamate also plays a key role in neuropathic pain (which I hope to introduce in Part II).
Thanks Marco, you might find this archive interesting: http://phoenixrising.me/archives/13083 The ‘sinus/amydala’ theory is interesting too. I don’t have respiratory allergic symptoms but I’m conscious that what I breathe in (in terms of residual cat allergen in my case) is the trigger for additional pain. If there were a way to reset the gating mechanism I feel many with this illness would be given a much better quality of life, whilst not necessarily being fully well.
I can concur that your sensation with the shirt is allodynia. Sadly I have it from top to toe 24/7 . I cannot wear cotton, I have to wear silk and this has lasted for over a year now. The self help measures you mentioned have been tried and spectacularly failed: they made the pain even worse. I use pregabalin and low dose amtritp which takes the edge off and reduces the level of pain from suicidal to liveable with but every day is pretty grim really.
Like you I am exquisitely sensitive to meds and supplements which limits possible routes to improvement.
Thank you for your reply..and I look forward to more of your musings.
Hello again Rosie
I can only sympathise. Two days of partial allodynia was plenty for me!
I’d forgotten that Cort had written that article on MCAD. I’d previously posted on another thread that I felt that my symptoms were more akin to mastocytosis than ‘CFS’ :
http://forums.phoenixrising.me/index.php?threads/doctor-suggested-mastocytosis-anyone.5181/#post-113310
Interesting that they found increased mast cells in fibro patients as recent findings also suggest a high level of peripheral polyneuropathy (which I’ll mention in the next part) in fibro patients.
Neuropeptide y not only induces mast cell degranulation but also antagonises glutamate release :
http://www.ncbi.nlm.nih.gov/pubmed/16026936
Raised levels of neuropeptide y in ME/CFS (and Alzheimer’s and Huntington’s) might not be a disease marker as such but a neuroprotective mechanism ;
http://www.ncbi.nlm.nih.gov/pubmed/20673761
Pregabalin and related compounds will also feature next and in that context the ‘antidepressant’ effects of amitriptyline may also be due to its impact on glutamate :
http://www.ncbi.nlm.nih.gov/pubmed/19405995
Plenty of possibilities. MCAD is very much a viable theory that might better explain or even complement what I’m suggesting but for the meantime I’ll leave that particular avenue to others.
PS – Sorry the ALA didn’t work (to say the least). I haven’t tried it myself for neuropathy. It was on a short list of things to try but I may not bother now.
I think one other thing to consider in this context are the cases where patients with M.E refuse food or water.
It is this kind of behaviour that makes psychiatrists of a certain bent think of conditions like hysterical blindness, or eating disorders and other somatic or dismorphic conditons – it seams to much to believe that any condition of the nervous system could result in such a ‘real’ hypersensitivity, it must be some kind of learned helplessness.
Yet of course you just have to look at severe allergies to realise that such oversensitisatoin is in fact commonplace, and of course refusing food and water in some cases is a deep down instinct triggered as part of a generalised repertoire of illness behaviour.
More research and observation on these patients from a completely none psychiatric or suspicious point of view is sorely needed to get away from this condescending idea that M.E patients are somehow just being ‘weak’ in response to their environment.
Hi David
Its hard to know what’s going on in severe cases such as those but really the last conclusion to jump to should be that its ‘psychogenic’ or that its a ‘refusal’ to take food or water and not an inability.
They may be rare disorders but people with mitochondrial disease can often have problems with swallowing and in the case of certain types of autoimmune encephalitis they may either not be able to swallow or may refuse food and water as part and parcel of the associated encephalitis ‘psychosis’.
There’s a certain failure in logic that states that we don’t know what causes ME/CFS but then to state with any certainty that any particular symptom ‘must be’ psychological.
Thank you so much for your interesting blog post, Marco.
Have you ever read the books or seen the lecture by Dr. Ritchie Shoemaker? He really understands chronic neuroinflammation. Even if you don’t agree with his theory that the inflammation in ME/CFS is caused by external and/or internal biological toxins, you could get a lot out of what he has figured out. You don’t have to re-invent the whole wheel.
Forebearance
Thanks for the ‘heads up’.
No I haven’t read his book but I’m not really in the business of trying to develop a new model of neuroinflammation.
What I’m attempting to do is reference recent peer reviewed research into neuroinflammation in those conditions that have been shown to have sensory gating problems and then apply that to ME/CFS to see if it fits.
So I’m not trying to ‘reinvent the wheel’ more finding a novel application for it.
Thank you so much for the extremely interesting article, Marco. When you wrote, “If I do overdo things physically or mentally I can end up pretty much bed bound within minutes. It hits me like a seizure. One minute I can walk, talk etc just fine and the next I can’t stand, walk, think or talk,” it really struck a chord. I always called it getting zapped out. The wrong odor, cross-conversations, a sudden adrenaline rush or just overdoing are just a few things that can cause it. I’ve had so many episodes after new meds that I shudder when a doctor even mentions trying a new one, and if a drug doesn’t knock me half unconscious, it does the opposite, although there are a handful I can tolerate and are helpful. I have a lot of problems with myoclonus and ended up in the ER after taking Amantadine for a couple of weeks, appearing as if I was having a grand mal seizure. Luckily, these episodes are not as severe or as commonplace as they were several years ago but its still a struggle. I never had a problem with myoclonus until after exercise ergometry testing and still can’t believe that’s all it took to make it a permanent problem, but I obviously have an extremely sensitive system. My symptoms have morphed over the years, too, as others have mentioned. I’ll stop before I write a book but thank you again and I look forward to reading the next 3 installments.
Hi Nan
Many thanks for your comments.
Either you and I are pretty unrepresentative or else there is a serious disconnect between what the researchers believe we are experiencing and the reality.
Even ‘easy fatigueability’ doesn’t cover it. ‘Fatigue’ usually comes on gradually and even when exhausted ordinary people can make their way home and crash out feeling better the next day. That a far cry from a sudden collapse where you are incapable of carrying out the most rudimentary of physical or mental functions.
That’s a major plus for me of having the opportunity to write this blog. The opportunity to talk about the illness as I experience it rather than what symptoms I’m told I’m supposed to experience.
Your experience with Amantadine is actually a little contrary to what I would have expected (on the basis of this hypothesis). Had you recently discontinued it or were taking it irregularly?
PS – ‘Zapping’ will feature a lot in the remainder of the blog!
Thanks so much for your reply. I had been taking Amantadine regularly for about 2 weeks. At first I thought it was my miracle drug. I probably looked like a maniac, outside raking leaves in December, but I finally had the energy to do so. When the myoclonus began, I didn’t even connect that to the Amantadine. I had two other severe episodes when my husband would drive me to the hospital but I’d wait it out in the parking lot, not wanting to go in since I was already experiencing some pretty major white coat syndrome. The last time, when I went inside, I finally connected the dots. The doctor kept yelling at me, asking what drugs I was on and I yelled back “Amantadine!” Naturally, he looked at me as if I had two heads and possibly horns. I was so disappointed since it had given me an energy boost, but the severe myoclonus stopped once I discontinued the med. I tested my theory by starting the Amantadine again about a month later and sure enough, the myoclonus returned. I still have minor jerking most days, especially by evening or all day on a bad day, but nothing like those severe episodes. I wondered for awhile if perhaps the extra activity caused the myoclonus rather than the Amantadine, but I’ve pushed myself to overdo many times since but it never caused the severe seizure-like myoclonus. Exercise only induced such an attack after the exercise ergometry testing. l-carnitine caused similar problems. Most drugs do the opposite except for Wellbutrin and Pamelor, which caused extreme nervousness. I know my case is extremely weird. I was DX in ’78 with FMS but didn’t believe that rheumatologist since he was an idiot, then a couple years later I was DX with MCS by Dr. Kroker, an allergist/clinical ecologist, and then Dr. Lapp DX me with CFS and FMS in ’93 but he suspected I had an undiagnosed neurological disorder as well. I went to a very good neurologist; however, and she said that it was all ME/CFS and Fibro. I hope this helped and didn’t muddy the waters further. By the way, Dr. Lapp found an extremely high level of alpha interferon in my system. He said my number was off the chart, and I’ve never heard this from others with ME either. What a puzzle. Thanks again!
Wow Nan
You’ve been through the wars.
I did notice, when trying to figure out the problem with Amantadine, that in rare cases (approx 1%) it can lead to seizures – particularly when there is a prior history of ‘epilepsy or other seizures’.
You may have been one of the unlucky 1%
Regards
Marco
Yes, that could explain it. I think we’ve all been through a war of one kind or another. I could write a book.
All the best, Nan
Great article 🙂 marco, Ive never read one anything like this one before and everything I managed to read so fits what ive experience. Thank you for writing it.
“In the ‘cocktail party syndrome’ it’s difficult to carry on a conversation with in a room because we have difficulty filtering out the noise of others. ”
Due to that I have been also given a diagnoses of CAPD (central auditory processing disorder). It used to be impossible for me to be able to focus on a voice throu all the “noise” of other voices.
….
To the poster in the comments with the daughter who gets the jerking on noise (sorry forgot your name). I used to be like that too fortunately Im less sensitive in this way so okay now with that and no longer getting the jerking and tremors I used to get. I hope your daughter recovers from this symptom soon. (I was like that for 2-3 years) . Any kind of sensory stimulation could send me into those jerks… one time I was in a car and someone opened the window.. just the sudden air hitting my face sent me into jerks for several minutes. Severe neuro reactions to stimuli.
…………………….
Cort Im wondering if this article can be broken down more for people. Ive only managed to read half of it ? before Ive had to stop and are going to struggle to find where Im up to next when I come back to try to read the rest. eg wondering if it can be broken down to eg Part 1a Sensory Gating and 1b Senory Gating seeing its so long, with a link part for each of the two parts of the article?
I know seeing I cant manage to get throu it.. so many others arent going to be able to either.and its sooo very interesting.
Many thanks for your comments Tania.
I’m glad it resonates so strongly for you.
Very interesting that you were diagnosed with central auditory processing disorder as its another condition that appears to be associated with ASD and ADHD.
Sorry that its hard to read in one go. I’m covering a lot of ground (and more to come) and I can fully appreciate that its a lot of text to take in in one go. A major stressor for me when working was the ‘paperless office’ policy where I often had to digest 100 page documents from the screen only. I find that I can’t even determine the overall structure of a document unless I have a paper copy.
I’m not sure if Cort would be able to split this or the coming parts and keep all the references and comments in sync? We may be able to sort something out.
In the meantime, if you can, I’d recommend printing a hard copy that you can work through in easier to digest chunks and mark where you’ve got to etc.
That’s what works for me.
I’ve certainly struggled with sensory issues, sound, light, smell, heat, during my 9.5 years w/ ME/CFS. I got a huge reduction in sensitivity after adding hypothalamus glandular. And pituitary glandular has been very effective for sleeping, allowing me to completely terminate the Rx I used periodically. I’m also using adrenal glandular, and when I recently had to decrease from 2/day to 1 while awaiting my next supply, I felt much more on edge. I’ve been using these things about 1.5 years. I also had a tremendous reduction in all symptoms when I eliminated grains and dairy. Thanks for this work, on to the next article after resting my brain, so tomorrow or next. 🙂
Thanks ahmo.
You may need a rested brain for Part two but part three (coming soon) should be a lighter read.
Interesting results from the glandulars. What prompted you to try them?
I’m pretty sure I would also benefit from eliminating grains and dairy – unfortunately I like my food and have eggs benedict on toast lined up for lunch today.
Probably not worth the increased symptoms but as someone who used to have a ‘cast iron’ digestive system I hate having to tip toe around food sensitivities.
I’ve no doubts that ME/CFS is essentially a chronic stress response, whether you called this trauma or PTSD or whatever.
The answer isn’t in drugs, nutrition or anything like that just finding ways of breaking this cycle or loop….hypothalamus and Amygdala are over reacting to the environment around them and this leads to muscle constriction and, elevated stress hormones and sub optimum brain chemistry.
I developed it back in 1995, fairly early on I came to the conclusion that orthodox medicine offered nothing by way of a cure and so I devoted my existence to recovering, it’s taken a long time but I lead a pretty normal life now, still a little way to go.
I would suggest to anyone suffering from it to look into Trauma Release Exercises, whether you think you have been traumatised or not, learning these exercises is inexpesnive and then you can do them at no cost in your home and over time there is every chance that you will notice a difference in your symptoms.
Good luck.
Thanks for the comments Matt
Although I do discuss ‘drug re-purposing’ and will do so again in later articles I do share your concerns about relying on drugs long term (particularly those affecting the central nervous system) as there are just too many feedback loops and adaptions that might take place that could lead to issues of tolerance or even unwanted ‘paradoxical’ worsening of the condition.
I also agree that there are certain ‘non-pharmaceutical’ approaches that may be beneficial – I’ve tried mindfulness meditation, EMDR and EFT myself but being the wired and tired type I’m just not very good at it or at sustaining it.
However, certain drugs may be helpful in either speeding up the recovery process or in breaking the cycle – plus I’ve reasons for proposing that this is not a ‘benign’ condition at all with the neuroinflammatory state carrying a risk for a wide range of conditions to develop – not all of which are likely to be reversible.
But in the current absence of a magic bullet ‘stress reduction’ of whatever form is certainly one of the best approaches we can take in my view.
BTW – congratulations on your progress to date.
Thank you Matt!! I’ve had CFS since 1994. I had every medical test known to man to try to discover a physical cause. It’s become completely clear to me now that it was caused by trauma. I’ve been wanting to shout this from the rooftops!
I recently had a trigger to childhood that made me realize I have PTSD. I knew I had it bad as a kid and I had, had severe depression and panic disorder as an adult, but PTSD wasn’t my diagnosis.
Something that opened my eyes was learning about the freeze response to trauma. While we all know about Flight or Fight, I had never read before about the Freeze response. Dr. Peter Levine has written about this as seen in animals and it is exactly how I coped in childhood.
Animals who freeze and then manage to survive a predator (impalas, opossums) can recover physiologially (they run away, muscles shake and twitch, hormones regulate, etc.). But many of us humans had no outlets for our fears – no one to tell, no place to scream, no where to recover emotionally and physiologically. Our emotions had to be stuffed to survive, which is what I did from age 0-14. I basically froze in terror, living in a state of constant anticipatory anxiety.
I’ve had the ACTH test and while the result was in range, it was on the low end. Still, I think my whole HPA axis is totally off and my system does not know how to re-regulate after stress. Unfortunately I still have a lot to learn about how to better deal with stress on a day to day basis in addition to recovering from childhood.
I will definitely look into trauma release exercises. I think the only hope for my CFS lies in recovering from past trauma (possible? don’t know) and dealing with daily triggers.
If Marco reads this, I’ve looked through some of the info here but it’s pretty over my head. I noticed however that you mentioned something about GABA so this may be of interest to you.
I had severe depression for a few years before getting CFS – not the kind where you retreat to bed. I was miserable, angry and suicidal but still forced myself to push myself physically. I still went to work, aerobic classes, everything until I broke emotionally at the thought of having to do one more thing and checked into a depression clinic. A few months later I developed the CFS symptoms. I’m pretty sure I had CFS prior to the depression. I just lived in a severe state of denial about how I felt physically. Denial is my forte (childhood training).
Anyway, I still battled panic attacks and depression for several years and tried numerous antidepressants. Most worked for a few months and then quit. Eventually I was put on Paxil, which thankfully has virtually cured my panic attacks (been on it almost 15 years). The depression lingered until I was finally put on Gabapentin and after being on it a while, it was like the heavens parted. I remember saying, “So this is how normal people feel!”
I haven’t the foggiest idea if that helps you. And I’m more than happy to answer any questions you have. Thanks.
Thanks Kira
That’s very helpful indeed.
It seems to be that anxiety,depression, PTSD and the symptoms of ME/CFS are all facets of the same underlying state and your experiences with Gabapentin is very suggestive.
I like the thought of “so this is how normal people feel”.
I’ve never felt that I was experiencing ‘life’ in the same way as others.
One question is – did Gabapentin help with any other symptoms?
PS – you really do need to get help for PTSD if that may be the root problem either via specialist help or using some of the techniques Matt suggested.
Hi Marco,
Actually the gabapentin did not help with my other symptoms. When I have a bad relapse with CFS (always stress induced) I can also get awful fibromyalgia symptoms – muscles aches so bad they’re painful and I have to take lots of Tylenol. I believe some people take gabapentin for fibro but it doesn’t seem to do any good in that respect for me. (And I take 1500mg/day). When the fibro hits, exercise just makes it worse. I generally have to rest a lot and wait it out.
Yes – believe it or not I’ve been in one type of therapy or another for 25 years. (I am a 50 y.o. woman). PTSD was never considered in all that time since I wasn’t raped or beaten or in combat. Still for various reasons, I did live in constant state of fear thoughout childhood – as I said, I did the freeze response. I’ve recently started mindfulness medititation and EFT though I fear a long road ahead. I think we need better PTSD treatments.
Thanks – have a good day!
Pity the gabapentin didn’t help with the other symptoms. Strange how it helps some with pain and sleep issues and not others.
Re PTSD treatments – something that might be worth trying is n-acetylcysteine (NAC) given that its well tolerated and with a good safety record.
It appears to be one antioxidant (and glutamate antagonist) that has some evidence for effectiveness in treating conditions linked with neuroinflammation :
” N-acetylcysteine shows the most promising results to-date, with several randomized placebo-controlled trials demonstrating its efficacy in MDD, BPD and schizophrenia”
with a trial planned for treatment of PTSD :
http://clinicaltrials.gov/ct2/show/NCT01664260
Might be worth keeping an eye on this?
Good luck and thanks for the feed-back.
Thanks for the tip. I’ll check NAC out. Good luck!
hi cort, i hope i’m at the right place. can you explain WHY i can’t react to things such as loud BANGS, the neuro scraping the bottom of my foot and it does nothing when it should jump? sort of NO reflexes since M.E. hit! thanx cort
Hi Dee
I’ll try and answer that as it my piece.
This was written from the perspective of how I (and others) experience ‘my’ ME/CFS which is the ‘wired and tired’ type.
In a later blog I make the suggestion that ME/CFS may resemble ADHD with subgroups. In ADHD there are hyperactive, inattentive and mixed types. ME/CFS may be similar.
Another possibility is the neuroinflammatory state I outlined in part II of these blogs leads to progressive deterioration and the nervous system becomes under-reactive (like the boy that cried wolf).
I do know personally that when my symptoms worsened several years ago I completely lost that feeling of an adrenalin surge despite the fact that stress does now knock me off my feet.
I’ll hope to be blogging soon on a piece of research that supports the idea of patients with either a hyper or hypo reactive nervous system in a single ‘CFS’ cohort.
Speculation of course.
Re – your foot – is it a lack of reflexes or a total lack of feeling?
This is great stuff. As scientist and patient I found your research and ideas quite compelling.
When this all began for me, or I should say when it finally became disabling, I explained it to my “long suffering MD” as follows:
“Seriously, Jim, it’s like I can feel my very mitochondria–buzzing–or sizzling or something. Whatever this is it’s on the cellular level, and I don’t care that my sed rate is normal, it’s inflammatory because I can FEEL it!”
Needless to say (but I will say it anyway) I feel validated and vindicated by your work and that of other forward thinking people. Thank you so much!
I would only add that I think we need to look to our food chain and environment, not just heredity and medication exposure, when discussing world cause/effect. This has very real-world implications in the case of people exposed to toxins like PCBs, such as Fort McClellan veterans currently fighting for court-ordered care from the VA–care the VA is denying them (us) because they claim no cause/effect has been proved between PCB exposure and autoimmune disease. As you know, that is simply not true.
Clearly this “syndrome”, whatever we call it (and I DESPISE the label CF-anything! …Canada is wayyy ahead of the US on that one!) is also going to continue to grow as humans are exposed to stronger and stronger toxins in the food chain. Weeds become resistant, so they have to make the herbicides stronger and it all stays ‘alive’ in the environment for generations. They have to genetically alter the food crop seeds because the herbicides are so deadly…and the cycle becomes more vicious and deadly generation after generation. This planet has a real problem when the only country with the common sense to outlaw genetically modified foods is Ireland. Monsanto “owns” the rest of the agriculture of the WORLD! …and a past Monsanto vice president is the current head, as I write this in 2013, of the United States Food and Drug Administration.
I hope future research includes environmental and food chain toxin exposure when considering cause/effect of all autoimmune disease, because I strongly believe they are all related. While the research will likely come too late to help me, I hope it will not come too late to help my children who had the bad luck to be born to an unwitting military lab rat.
While stationed at Fort McClellan, Alabama I (and countless thousands of others like me) was exposed to excessively high levels of the components of Agent Orange, as well as chemicals like Dioxin and PCBs due to spillage/illegal dumping at the Anniston, Alabama Monsanto factory located near ‘Fort Mac’. The civilian population served by the same water supply as the base won several hundreds of millions of dollars in a mass action lawsuit against Monsanto for this illegal activity which went on from 1939-1996, and internal memos, now a matter of public/judicial record prove that not only were the powers that be at Monsanto aware that the spilling and open pit storage of their chemicals taking place, but they knew by the 1940’s that many of the chemicals they were dumping into Anniston and Fort McClellan’s water were lethal to humans in very small amounts.
The rate of autoimmune diseases like diabetes, MS, Fibromyalgia, cancers, arthritis and what we call ME/CFS are sky high in that area, as are rates of miscarriage, reproductive failure and early life hysterectomy, heart and pulmonary disease. Environmental factors wreak havoc at the cellular and genetic level, and this damage has indeed been passed on genetically.
The reason I bring this up is because they, Monsanto, indulged in a massive cover-up and CONTINUED TO DUMP TOXINS INTO THE WATER IN THE ANNISTON AREA FOR DECADES AND COVER UP THEIR ACTIONS, even with so many thousands of lives known to be at risk, so there is absolutely no reason to believe they will behave in a more responsible manner in the future as long as there is money to be made. Monsanto’s reach and influence extends worldwide.
Fort McClellan was also the location of the Army’s Chemical Warfare Headquarters, MP School and a major Basic Training Center. It is in the former capacity that basic trainees like myself were exposed to Sarin Nerve Gas, Oxidized Uranium and Mustard gas, as well as unknowable experimental bio-chemical weaponized toxins. We unwitting lab rats were never informed of our exposure; in fact the military and VA have done their best to deny it, and I do not overstate the case when I say we were directly experimented upon in addition to our ‘accidental’ exposure. It is all a matter of public record, yet with a 24-hour “news” cycle no one seems to find the time to report on the issue with possibly millions of people affected.
I do not mean to step on your important blog, but I think a large percentage of “us” with this disease have also at some point been exposed to high levels of toxins. I really think you were on to something there. My advice to anyone reading this who has been in the military or who knows anyone who has been in the military or lived near a base is to check the internet for news about environmental hazards at or near your duty stations. Check information about Superfund sites, which are often near military installations. Our government, unfortunately, cannot be trusted to inform or care for us, no matter who is in charge, even when they are responsible for making us sick. ***This is NOT a political issue, nor is it intended in any way to be one. It has continued over many administrations, from 1939 to the present day and with no president since the court case stepping forward to issue an executive order that would force the VA to follow the court’s order in Anniston v Monsanto.
Thanks very much for the kind comments Michelle. Glad you liked it.
I don’t propose any specific trigger for this neuroinflammatory state. I’m pretty sure many ‘stressors’ could be the trigger and once started the neuroinflammatory cycle can be self sustaining.
As regards the food chain you may have a point although I’m not sure whether the problem lies with what’s being put in it as opposed to what’s been taken out through modern farming and processing practices. I”d be surprised for example if even raw foods nowadays contain the same nutrients including antioxidants as they used to. I know I feel less ill if I avoid processed foods which I pretty much do now.
Toxins are another highly possible trigger.
I don’t know if you’ve come across her work but the Gulf War researcher Beatrice Golomb proposes a pathological mechanism whereby all the putatative exposures (whether vaccinations, pesticides, radioactive or other chemical toxins) eventually lead to the same pathological state which includes an increased tendency to autoimmunity. She uses Gulf War Illness as a model (because the circumstances around disease onset are more easily identified for this group of people) but suggests the model also applies to other ‘overlapping multisymptom’ illnesses including ME/CFS.
Might be worth a read if you haven’t already :
Oxidative Stress and Mitochondrial Injury in Chronic Multisymptom Conditions: From Gulf War Illness to Autism Spectrum Disorder
Beatrice A. Golomb
http://precedings.nature.com/documents/6847/version/1
Is this blog/study still active and/or updated somewhere? I find much of this might relate to my own situation, though not typical and a long story.
Overstimulation or overwhelming, multiple stress factors hitting at one time seems to have led to, or at least was followed by autoimmune disorder, fatigue, diagnosis of depression years before I experienced a true depression: and now 10 years later, I’m left with intermittent but fast hitting fatigue, sleep issues and a kind of stress avoidant behavior that is so frustrating after being a strong and healthy person until that year of overwhelming physical, mental and emotional stress.
I received TMS treatments that worked enough to make some difference.
One thing I noticed in particular, Vyvanse of all things, seems to help more than any of the antidepressants given me over the years. SSRIs pretty much do nothing for me. Clonazepam helps and Vyvanse, as well as remarkable vitamin D. I was just put in Pristiq (my doctor demands I stay in something to prevent a relapse but which I have ceased to take due to so MANY terrible side-effects. It’s poison to me despite my genetic profile showing otherwise.
Also, I had an aunt with schizophrenia and a cousin with bipolar- and others with either anxiety or depression.
If anti-oxidants are indeed as this article suspects, then my entire family needs to know of it.
Interesting. Check out a blog on Vyvanse in chronic fatigue syndrome – https://www.healthrising.org/blog/2012/12/28/26/