(Marco’s first two Neuroinflammatory blogs lead us into sensory gating and glutatmate excitoxoicity and now he dives into a rare neurological disorder called Stiff Person Syndrome (SPS) (sometimes misdiagnosed as Fibromyalgia) with factors (high glutamate levels, increased sensitivity to stimulation, autoimmune manifestations, possibly infectious onset) that makes it an intriguing, if unusual, possible cousin of ME/CFS/FM
Let’s see what we can learn from another disorder with a funny name and a decided unfunny outcome. For myself overexertion is a call for increased sensitivity to stimulation, a high ‘startle reflex’, stiff, painful muscles and a decided downturn in coordination; a stiff person indeed. Cort )
Glutamate/GABA Imbalance and Stiff Person Syndrome
In Parts I and II, I proposed that the same neuroinflammatory vicious cycle underlies a range of neurological, psychiatric and neurodegenerative conditions that may result in a variety of symptoms and hence different diagnostic labels. I have suggested that ME/CFS may be one of these neuroinflammatory conditions.
Could Stiff Person Syndrome tells us something about Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia?
Intuitively, it is relatively easy to accept that neuroinflammation can result in a wide range of sensory processing problems, ‘mood’ disorders and cognitive symptoms however for many, if not most of us, ME/CFS is a profoundly ‘physical’ condition characterised by muscular pain, exercise intolerance and post-exertional malaise.
It may not be quite so easy to accept that an imbalance in the neurotransmitters glutamate and GABA could cause many of the symptoms found in ME/CFS but the disorder below demonstrates that they’re clearly capable of causing those symptoms and more.
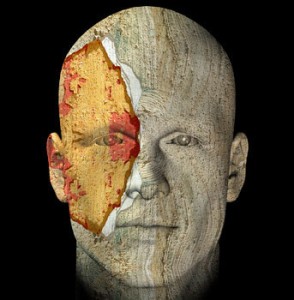
Stiff Person Syndrome
An extreme example of the potential impact a glutamate/GABA imbalance can have is the unfortunately named stiff person syndrome (SPS). This relatively benign name belies the true nature of a debilitating and at times fatal progressive illness (Duddy, Baker, 2009). Stiff person syndrome (SPS) is rare, affecting only one in one million of the population (Wikipedia) and as a consequence is often misdiagnosed but it shares some interesting characteristics with ME/CFS/FM type disorders.
This disorder is characterised by the sudden onset of muscle rigidity severe enough to cause muscle and joint damage and even spontaneous bone fractures. In the course of an attack the muscles of SPS sufferers can become so contracted and rigid that they’ll fall over suddenly and are unable to protect themselves from injury. Consequently they frequently end up at hospital for treatment of cuts, bruises and fractures. These seizure-like episodes are impossible to predict and often leave SPS sufferers confined to their homes.
The National Institutes of Health, National Institute of Neurological Disorders and Stroke (NINDS) provide a concise summary of the disease (paragraph breaks and bolding added):
“What is Stiff-Person Syndrome?
Stiff-person syndrome (SPS) is a rare neurological disorder with features of an autoimmune disease. SPS is characterized by fluctuating muscle rigidity in the trunk and limbs and a heightened sensitivity to stimuli such as noise, touch, and emotional distress, which can set off muscle spasms. Abnormal postures, often hunched over and stiffened, are characteristic of the disorder.
People with SPS can be too disabled to walk or move, or they are afraid to leave the house because street noises, such as the sound of a horn, can trigger spasms and falls. SPS affects twice as many women as men.
It is frequently associated with other autoimmune diseases such as diabetes, thyroiditis, vitiligo, and pernicious anemia. Scientists don’t yet understand what causes SPS, but research indicates that it is the result of an autoimmune response gone awry in the brain and spinal cord.
The disorder is often misdiagnosed as Parkinson’s disease, multiple sclerosis, fibromyalgia, psychosomatic illness, or anxiety and phobia. A definitive diagnosis can be made with a blood test that measures the level of glutamic acid decarboxylase (GAD) antibodies in the blood.
People with SPS have elevated levels of GAD, an antibody that works against an enzyme involved in the synthesis of an important neurotransmitter in the brain (GABA).
Is there any treatment?
People with SPS respond to high doses of diazepam and several anti-convulsants, gabapentin and tiagabine. A recent study funded by the NINDS demonstrated the effectiveness of intravenous immunoglobulin (IVIg) treatment in reducing stiffness and lowering sensitivity to noise, touch, and stress in people with SPS.
What is the prognosis?
Treatment with IVIG, anti-anxiety drugs, muscle relaxants, anti-convulsants, and pain relievers will improve the symptoms of SPS, but will not cure the disorder. Most individuals with SPS have frequent falls and because they lack the normal defensive reflexes; injuries can be severe. With appropriate treatment, the symptoms are usually well controlled.
What research is being done?
The National Institute of Neurological Disorders and Stroke (NINDS) conducts research related to SPS in its laboratories at the National Institutes of Health (NIH), and also supports additional research through grants to major medical institutions across the country. A study using the drug Rituximab proved ineffective in treating individuals with the disorder. Current research is focused on understanding the cause of the disease and the role of the anti-GAD antibodies.”
Key Points
In the context of the previous discussion, it is worth re-emphasizing some similarities between Stiff Person Syndrome/ME/CFS, Fibromyalgia and other ‘neuro-inflammatory’ conditions :
- SPS misdiagnoses include Parkinson’s, fibromyalgia and a range of anxiety disorders including phobia and psychogenic movement disorders;
- SPS is considered to be an autoimmune disease involving raised levels of glutamic acid decarboxylase (GAD) antibodies – which effectively lowers levels of GABA, taking the brakes off the excitatory neurotransmitter glutamate
- like many autoimmune diseases SPS affects twice as many women as men;
- Like ME/CFS, SPS patients are reported to respond to Rituximab: (in a series of case studies inc Bates et al, 2005, Fekete and Jankovic, 2012) although these results have yet to be replicated in clinical trials;
- Current treatments contain several drugs used in ME/CFS such as anticonvulsants, gabapentin, tiageine, IVIG and some that might work such as Baclofen (Whelan, 1980 etc) and diazepam;
- Given reports of metabolic syndrome and one doctor’s report of increased rates of diabetes in his practice, it’s intriguing that SPS effects diabetics at a much higher rate than the general population;
- most intriguingly, SPS attacks (exacerbation of symptoms) can be triggered by sensory input including loud noises, emotions or stress or exercise (Rodgers-Neame); ie, it appears to have a sensory gating component. There appears to be no literature investigating a sensory gating deficit (as described in Part I) in SPS. SPS patients, however, have been shown to have an exaggerated acoustic startle response. (Matsumoto et al, 1994)
Conclusions
An imbalance in the excitatory and inhibitory neurotransmitters glutamate and GABA is implicated in a wide range of neuropsychiatric (ASD, schizophrenia, bipolar disorder, major depressive disorder, OCD etc) and in pain (fibromyalgia, interstitial cystitis, IBS) and movement disorders (Parkinson’s, Huntington’s) and perhaps chronic fatigue syndrome (ME/CFS).
Current research provides hints that a similar etiology may underlie a range of ‘neuroinflammatory’ conditions including ME/CFS.
- Get the References here
- Part II of Stiff Person Syndrome examining at anxiety, autoimmunity and infection in SPS will be up soon.
The Neuroinflammation Series from Marco
- Part I: Not Fatigue After All? New Model Suggests Other Symptoms Better Explain Chronic Fatigue Syndrome (ME/CFS)
- Part II: Glutamate – One More Piece in the Chronic Fatigue Syndrome (ME/CFS) Puzzle? The Neuroinflammatory Series







Hi Marco,
In trying to find more information on the drug you mentioned called Tiageine, I find it is Tiagabine. Thank you for bringing in this associated illness. It seems highly associated to me. I have had extra stiff muscles since my twenties, extra sensitivity to noise and light, which I react emotionally against, and of course, ME/CFS. I hope researchers are reading this site!
Thanks,
Cecelia
Oops!
Sorry about the misspelling Cecelia. Something must have gone amiss between drafts.
Sending all of this info to my Environmental Dr. Some of these drugs have already been rec. However. Not what to take when and what together. From ME/CFS Dr.This really hit a nerve with me on this disease. A lot of my symptoms. At least there is a definitive test.
Thank you Cort!!!
Interesting, though a bit far from my symptoms. I am not clear about the relationship, if any, between your report that a study under the NIH umbrella reported that Rituximab was not effective, and reported cases that it was–any explanation? Chris
Hi Chris
Two possibilities.
(a) Positive case study, anecdotal or small scale study reports often fail to be replicated when subject to the ‘gold standard’ of well powered randomly controlled trials (RCTs).
(b) To deliver the required scientific rigor required, RCTs need to reduce the number of variables to the bare minimum and in doing so often result in an artificial laboratory context that may bear little relationship to what happens ‘in the field’.
You take your choices etc!
PS – I’m not suggesting what we have is stiff person syndrome. Its an example of how a glutamate/GABA imbalance can have both ‘mental’ and very physical effects.
Is this doctor going to publish his results?
This is very interesting. I wondered about this myself, years ago as I read on Stiff Person Syndrome. My medical texts (I was a physical therapist) noted that sometimes it manifests in young babies then disappears for a while only to resurface in adulthood. A niece looked like she had this as an infant; I have been disabled by ME/CFS characterized by a non FM type abnormal stiffness (as well as PEM) after normal activity. So it did make me wonder if we had this in our family.
I am glad to see others are looking into this. Thanks.
I was diagnosed with fibromyalgia 24 years ago. I have had pain stiffness and muscle cramps all my life. I really believe I was misdiagnosed with the fibromyalgia and think it is stiff person syndrome. I have muscle cramps so severe they’ve broken a rib and I catch them all over my body from head to toe. I have insomnia lack of concentration brain fog, depression anxiety hypothyroid fatty liver ulcers sciatic nerve bulging disc rectocele migraines hypothyroid restless leg syndrome irritable bowel syndrome Raynaud’s disease, sensitivity to smells sounds, soreness all over nausea. I went to the neurologist the other day and she wanted to start with blood work and said that fibromyalgia is a diagnosis but it’s usually an underlying and condition of a more severe problem. She Drew 15 miles of blood to send the California for blood work it’s going to take two months for the blood work to come back. I sure do hope that figure something out because I am really scared. Thank you
The only similarities I see between SPS and ME are the comparisons you made. This is a very rare disorder, with old research. I understand the desire for ME to be studied in a similar manner as this illness, but there is no mental causes of ME, only distress resulting from lack of recognition or treatment. I understand the similarity concerning glutamate. Yet how can you compare ME to any disease when it is still lacking a diagnostic code (of its’ own) to be studied at the appropriate federal level? There has to be a process, scientifically, to further research to help sufferers of ME. It starts by recognition and a classifcation of the CFS that follows the slash. While I am interested in reading research of neurological background, if an illness only affects 1 in a million, it is not similar to ME at all. Patients with fibromyalgia, such as myself do have incidents of stiffness that usually resolve on their own or with medication. Once again, I saw the FDA recognizes ME/CFS as a serious, life threatening illness, yet blocks the most effective treatment for many patients. Repetitious? Absolutely. I will continue to repeat myself and try to bring in medical clarity for readers who are patients. If an analogy will help, you don’t study a cucumber by studying the whole vegetable produce department in a grocery store. I must see more research that is M.E. specific for those who are so ill and easily confused. Yet, I still enjoy reading research of neurological nature, it began in training as such a mysterious subject…our brains are amazing organs, yet like other organs they ‘get sick’. Chemical imbalances, neuronal disturbances and unlimited aspects of both nervous systems.Since it is explained that M.E. causes dysfunction of the autonomic nervous system, one must recognize that the central nervous system is disturbed as well, as they also work in tandem. Having sensitivity to noise and light is typical of a patient with M.E. due to widespread inflammation. Oh! And figure this out, someone! I had a CAT scan following a series of serious headaches, both pressure and migraine quality that read: Macroplasia (overgrowth) of the mesenteric membrane around the brain. No one had any explanation, and a following scan later did not demonstrate this finding, it was at a different hospital. I have dropped the subject, as if it no longer exists, then I must have recovered from a growth spurt of the brain!! Or am I creating my own new blood brain barrier? LOL
Also- it was after understanding GWS that I understood my own illness, caused by ‘everything’. Elementary sounding but oh, so true. I am interested in these studies at Georgetown University.
Mary Silvey,RN
BARANIUK COMES THROUGH!
This is important research on Gulf War Illness just out, on the brain. Could be very relevant to CFS too.
I’ve been harping on about the brain for a while. So has the sadly much sniggered at (in the CFS community) Andrew Lloyd.
http://www.plosone.org/article/info:doi/10.1371/journal.pone.0058493
The question I have is: are these kind of brain problems potentially reversible with some form of treatment, or irreversble (but potentially treatable)???
Hi Matthias
The reason Gulf War Illness hasn’t been discussed in this series is that to my knowledge no research has be carried out on sensory gating issues in GWI – which is the first commonality that started to tie all these conditions together.
That’s not to say we can’t learn something from GWI. In fact one prominent GWI researcher suggest that GWI is ideal for getting to the bottom on ‘Chronic Multisymptom Conditions’ including ME/CFS and FM.
Well worth a read (free full text) :
Oxidative Stress and Mitochondrial Injury in Chronic Multisymptom Conditions: From Gulf War Illness to Autism Spectrum Disorder
Beatrice A. Golomb
http://precedings.nature.com/documents/6847/version/1
Has anyone tested ME/CFS patients for glutamic acid decarboxylase antibodies?
Nope but look at this:
http://www.ncbi.nlm.nih.gov/pubmed/20847504
This woman suffered fatigue, weight loss and palpitation after interferon treatment.
The IFM treatment may have lead to her coming down with Type I Diabetes and high GAD antibodies.This is intriguing because IFN therapy has long been thought to be a possible model for ME/CFS and a recent hepatitis study implicated the RNase L pathway in IFN problems….
So here we have a woman being given a drug that is possibly a model for ME/CFS and not only does she come down with diabetes (which has connections to glutamate excitotoxicity issues, as I remember) but her GAD antibodies erupts….
Intern Med. 2010;49(18):1987-90. Epub 2010 Sep 15.
A case of type 1 diabetes onset and recurrence of Graves’ disease during pegylated interferon-α plus ribavirin treatment for chronic hepatitis C.
Fujioka T, Honda M, Yoshizaki T, Ogawa M, Matsuno H, Shimokawa K, Koyama K.
Source
Department of Internal Medicine, Mishuku Hospital, Tokyo.
We report a case of type 1 diabetes onset and recurrence of Graves’ disease during pegylated interferon (PEG-IFN)-alpha plus ribavirin treatment for chronic hepatitis C. The patient was a 55-year-old woman diagnosed with chronic hepatitis at age 46 years. She was treated for Graves’ disease at 50 years of age. Because Graves’ disease remitted, PEG-IFN-alpha plus ribavirin treatment was started for chronic hepatitis C. She was examined because of complaints of general fatigue, weight loss, and palpitations after 24 weeks of the treatment. She was diagnosed with a recurrence of Graves’ disease, and methimazole treatment was started. However, she complained of malaise, thirst, polyuria, and loss of body weight. Her fasting blood glucose level was 292 mg/dL and HbA1c was 9.3%.
Serum anti-GAD (glutamic acid decarboxylase) antibodies were 2.2 U/mL. She was diagnosed with type 1 diabetes with ketosis, and insulin treatment was started. Serum anti-GAD antibodies gradually increased to 15.1 U/mL. Graves’ disease and type 1 diabetes are often complicated, and the coincidental occurrence of these 2 diseases is known as autoimmune polyglandular syndrome type III. However, only a few cases have shown that these diseases occur after IFN treatment.
Good find.
“This woman suffered fatigue, weight loss and palpitation after interferon treatment”
All of which could be attributed to the reactivation of Graves’ disease but IFN inducing anti-GAD antibodies (and potentially diabetes) does make you wonder about the mechanism underlying post IFN treatment fatigue as a model for ME/CFS.
Hi Beatrice I was tested for SPS in 2010 with GAD blood test. It takes 6 wks for results, and test was repeated and I was also sent for nerve conduction and muscle testing. All came back clear – GAD test result 0.6 but normal range 0-0.5, as EMG normal confirmed not SPS. I have dx of Cfs/ME for 10+ years and get very stiff in hips and spine and neck and hand joints affecting my mobility.
Very interesting.
Clearly you don’t have SPS and I’m not suggesting that ME/CFS patients do either but I do wonder just how far outside normal range GAD antibodies need to be before low GABA levels start causing problems?
I was diagnosed with FM 23 years ago. I was also eventually diagnosed with late onset diabetes (LADA) on the basis of the presence of anti-GAD in my blood. I often wonder if these antibodies could also play a role in my chronic muscle contractions. To my knowledge there is only one published case study showing the presence of anti-GAD in a female patient with FM like symptoms. Any thoughts on the interest (or lack of) testing FM patients for anti-GaD?
With due respect to all opinions involved, I was asked by Rich via PM a few years ago to ask Dr. Klimas about his glutamate/methylation theories. (May Rich rest in peace.)
Her response was very fast and also respectful to Rich as a person. ( Very respectful to Rich as a person), But her ‘quick’ comment on the ‘glutamate/methylation theory’ was quick, to the point and very clear.
(Which I greatly appreciate, as my conversations with her were on my dime, and she did not waste time on this issue.)
She explained, in no more than two sentences that the methylation pathway theory is not valuable to CFS research because (this is from my memory, although I have her precise words on tape).
She was quick to say that there are over 40,000 genes in the body and thus over 40,000 methylation pathways, so ‘a single methylation pathway isn’t relevant to CFS. And how could it be?’
She was able to parse this subject down to less than one minute of my time, and it was me who asked her! It would not, (NOT) have come up otherwise.
Her response was more than enough for me. We moved on.
Dr. K is brillant and in my view is a genius, (as is Dr. Cheney, who was my doctor for well over a decade, and as I understood it from Rich, he too had zero interest in this theory.)
So while I know people are pursuing this theory, it’s not relevent to me as a CFS patient. The opinion from Dr. K on this was very valuable to me as I ceased to be interested or willing to ‘chase’ this train of thinking, (ever, and forever.) Am grateful for that.
Best,
Questus
Interesting response from Dr Klimas Questus.
I’m not that familiar (in depth) with Rich’s methylation hypothesis and I don’t know what he said about a relationship between methylation and glutamate?
I’m a little perplexed though.
I haven’t mentioned and won’t be mentioning methylation or methylation blocks. This is not a methylation centred hypothesis.
Perhaps but I have yet to see Dr. Klimas make much of an attempt to publicly get at the root cause herself – so I applaud people like Rich Vank for trying to tie everything together. Moreover, Rich Vank’s protocol does seem to help people improve function, which is the best that many people can hope for. For the most part Klimas’ general treatment plan is not a whole different: a few supplements and for those willing an “exercise plan”.
I think Rich’s protocol has been effective in some people and that speaks for itself. Some practitioners (Dr. Myhill, Dr. Nathan..) do use it and some do not….
My understanding is that Dr. Klimas uses just about every treatment in the book though; from immune modulators (immunovir) to antivirals to beta blockers to yes, her ‘exercise’ plan…
I actually think Dr. Klimas is getting closer and there’s a good reason to have some hope in the next year or so that something major is going to come out of her clinic/lab. We’ll see!
Yeah, there was probably too much snark. But the point is that Rich attempted to lay out a model that explains the condition. Granted it is more difficult for Dr. Klimas to do that (based on politics of treating patients and needing funding) but as far I know has yet to do it. So what I was trying to say is that it is unfair and way too easy to be an arm chair critic without coming up with or advocating another model that can explain the condition.
Interesting info in the link below on the link between neuroinflammatory disorders like MS (and ME/CFS?) and white brain matter disease. Is neuroinflammation in CFS causing the white brain matter problems in CFS???
http://www.neurosciencecampus-amsterdam.nl/en/research/research-activities/brain-disease-mechanisms/white-matter-disease/index.asp
Thanks for the link Matthias.
Neuroinflammation causing white matter damage in ME/CFS is certainly a plausible possibility.
Here’s a small excerpt from part IV of this series which will be coming up in due course ; Wernicke’s encephalopathy due to thiamine deficiency is associated with autonomic neuropathy :
“In the context of the present discussion, it has been noted that brain lesions in an experimental rat model of Wernicke’s encephalopathy are exactly the same as those associated with glutamate excitotoxicity (Zhang et al, 1995).
It appears that in the same experimental model of Wernicke’s encephalopathy, thiamine deficiency and glutamate interact leading to excitotoxicity with thiamine deficiency resulting in a downregulation of the GLAST glutamate transporter impairing glutamate clearance from astrocytes (Hazell et al, 2003).
The results are “lactic acidosis, brain edema, oxidative stress, inflammation, and white matter damage” (Wikipedia).
This series is really interesting to me because it addresses some of my worst symptoms and I think that at this point, ANY research is good, especially when it addresses neuro symptoms that are often ignored. Why NOT look at other conditions which have some similarities, or at least for those of us with myoclonus or who are seriously affected by stimulation of any kind. For instance, years ago we were traveling somewhere and my husband had to slam on the brakes – not serious, but it startled me. Being startled shouldn’t turn a person into a zombie, unable to speak, move etc. for hours. Shouldn’t do the opposite either, setting off bone-rattling myoclonus. Same thing has happened with odors or even after great times like after a concert. Can’t write much more – fighting a cold/bronchitis so although I’m trying to think of something more intelligent to write, I really can’t. (Probably couldn’t do that on a GOOD day, but it sounds like a good excuse 😉 I just hate to see research limited to areas that are already being pursued. I don’t have a scientific background, am just a pragmatic person who thinks it worthwhile to look at other conditions, physical or mental, that involve problems with sensory gating. Thank you!
Thanks for the comments Nan and also for sticking with this.
Not quite as dramatic as your own experiences but even pleasurable stimuli can trigger a crash in my experience also.
Not long after being medically retired, I used to infrequently (three times a year or so) have spells where I felt quite well for a brief period. On one of these occasions my wife and I decided to bite the bullet and go for a rare outing to the cinema (a matinee showing where the only thing worth watching was the kids’ animation Finding Nemo – and very good it was too).
Still feeling OK we then decided to follow up with an even rarer meal out which was also very enjoyable.
Unfortunately I then spent the night eyes wide staring at the ceiling with all of the days’ ‘events’ going round and round in my brain. I was knocked off my feet for days after that.
‘Finding Nemo’ and a nice meal were too much of a ‘stressor’ for my system to handle : )
Bizarre eh?
Not bizarre to me at all, unfortunately. I’m lucky that I can tolerate more than when I was sickest but if we go out at night I have a terrible time shutting my brain down and sleeping.
Cort, am quoting your response from above.
My understanding is that Dr. Klimas uses just about every treatment in the book though; from immune modulators (immunovir) to antivirals to beta blockers to yes, her ‘exercise’ plan…
I actually think Dr. Klimas is getting closer and there’s a good reason to have some hope in the next year or so that something major is going to come out of her clinic/lab. We’ll see!
Cort, well said. I couldn’t agree more on all of the above. I believe Dr. Klimas will be the one to ‘crack’ this. I say that with all due respect to all those researching as well.
As to her approach, she models it on the patient. She has used all of the above, and more, (some of which are very interesting and not well known.) She has quite a few tricks up her sleeve and doesn’t always just use the well known immune modulators to shift Th2 to Th1.
It depends on the patient and how they present. She does not use a cookie cutter approach.
In my opinion her exercise plan is sound, and even more important for people with CFS and POTS.
I start cardio rehab next week, hope for good results.
Best,
Questus
Ha! Questus I hope your quest for better health takes a good turn with your rehab. Please check in along the way…
From Facebook
Mary Mullan – 6:21pm Mar 23
This disorder is autoimmune, so does this mean cfs could well have an autoimmune causation, considering symptom overlap with this disorder and so many other autoimmune diseases like multiple sclerosis and lupus. I believe we as patients of a disease with no real treatment should b offered some of the treatments offered to other autoimmune disorders like steroids or biologics.
The Exercise plan (N. klimas) does not work for most patients. It is a misunderstanding that exercise is good. We do not know what causes this desease. When the immunesystem is active you never can rehab. I think Klimas is wrong. If oxidatieve stress is a problem exercise is the last thing you must do.
It’s long past time to group patients. Despite waht Beth Unger/Bill Reeves say we are not all the same and should be treated differently.
But then we need objective data to support ‘your’ (N. klimas) statement. Which patiënts etc…POTS is a different and objective group. This group must be verry carefull with exercise. When you have tachycardia exercise can be verry harmfull at the long term. N. klimas is a wonderfull researcher but she is wrong. We must know the cause. And i never see the Vo2max turning to be normal or better after exercise.
What “your” statement are talking about? I thought I was agreeing with you.
Even the tachycardia and dysautonomia issue is not so simple. I have tachycardia but it is not necessarily driven by exercise – for me it’s more a body temp issue. It can be more complex than just “exercise” is bad.
Oke, The statement of N. Klimas that exercise is ‘good’. Tachycardia by POTS is not due to deconditionering. Therefore it is a verry dangerous ‘symptome’, in the long term it will lead to heart failure and sudden death. Patients with this problem will not get old. I think scientist are not aware of this point.
I’d agree I think. It’s some kind of brain damage affecting blood flow, HR, etc.
I think you are right. I would like to know why some patients have little white lesions in there brain. Just like MS but they are little and spread over the brain. Nobody knows. I wonder if this group have POTS.
Interesting article Cort. I’m no scientist but my experience with Gabapentin (allowed low dose for pain – it did not touch) was very positive. I believe it stabilises brain activity by the reduction of glutamate if understood correctly. I’m completely of the opinion “brain” not “mind”, it is after all a functioning organ like any other. With some trepidation I raised Gabapentin to Epilepsy levels and over a period of about a month slept mostly day and night (at last), and vivid dreams disappeared. Coming off at the end gradually I felt considerably better (not cured because sudden wired bouts still appeared).Since my brain MRI scans showed “high intense spots” not understood by my Neurologist I do very much endorse current thinking about Immune dysfunction caused poss in our case by infection/overload/undiagnosed infection initially.
Hi Enid
‘Stabilising brain activity’ could be exactly what at least a sub-set of us need in my opinion.
Hi Marco, apologies for not seeing it was your article – put it down to a period of lay-off please. Apart from the Gabapentin session the next step forward was Amoxycillan (following tooth extraction) which eased GI problems enormously.
No worries Enid
Its a joint effort with Cort trying to make my turgid prose a little more digestible – or to give him his official title – contributing editor.
Antibiotics are interesting drugs – lots of effects beyond their expected mode of action.
If you don’t mind me asking – how are you doing? It sounds as if there has been some improvement of late?
Hi Marco, Thanks for asking, I’m over hopefully the worst ME throws at one but complications building up over the years have now firmly set in. What my Neurologist described as “reactive” arthritis in my early days (I believe there is a viral one) is now disabling Osteoarthritis and Osteoporosis. I have a feeling there are so many “chemical” cycles disrupted and had I known about Rik’s methylation and supplement support earlier on things might have been different. I do recall excreting high potassium levels in my urine at one stage and high heavy metals when everything tasted metallic for quite a spell. I’m certainly of the opinion it’s Neurological in origin though and suspect a virus in the Herpes family went/goes undiagnosed. The muscle function tests were terribly painful as the electrical currents passed through my spine, so damaged nerves (demyelisation suspected). But quite what and why remains a mystery here – there is no testing here for those appearing amongst PR members. Again I endorse Immune system failure as the primary pathology to be addressed (I had what are called latent viruses expressing – eg Polio like, Chicken pox like etc). On the good side thinking, memory etc. are much improved now, as long as I keep within an envelope.
Good and not so good Enid.
Sorry to hear about the additional problems. Its long been a concern of mine that I’d pick up other health problems (including those associated with normal aging) well before anyone got to the bottom of the ME/CFS puzzle. Time’s wearing on though and things seem to be rapidly going to pot (deteriorating eyesight, neuropathies etc).
But on the positive side there’s nothing worse than not being able to enjoy a simple pleasure like reading so I’m very glad to hear that your cognitive issues have improved.
Keep sticking within the envelope!