



NEUROINFLAMMATORY MODEL OF ME/CFS Part IV – SYMPTOMS, HETEROGENEITY AND ONSET -PULLING IT ALL TOGETHER?
B – CAN THE NEUROINFLAMMATORY STATE EXPLAIN THE CARDINAL SYMPTOMS OF ME/CFS? – SYMPTOMS – FROM MOOD DISORDERS TO TINNITUS
Firstly, it must be acknowledged that this line of inquiry started with the observation that overlooked and minor symptoms rather than the cardinal symptoms could hold the key to uncovering the underlying pathology of ME/CFS. However the proposal is that a single neuroinflammatory condition underlies ME/CFS and related conditions and therefore this proposed mechanism must also explain the cardinal symptoms of the condition. So let’s take see if it can.
Mood
In the interests of brevity (at last!!) several common symptoms can be easily and directly explained by glutamate/GABA dysregulation resulting in a neuroinflammatory ‘vicious cycle’. With glutamate dysregulation strongly implicated in Major Depressive Disorder (MDD) and bipolar disorder (Machado-Vieira et al 2012), anxiety (Cortese, Phan, 2005) and Obsessive Compulsive Disorder (OCD) (Pittenger et al, 2011) for example, the symptoms associated with ‘mood’ can be directly attributed to this mechanism.
Pain
Similarly glutamate transmission is closely associated with pain transmission generally (Zhen et al, 2012) and appears to play a key role in specific conditions such as fibromyalgia (Valdés et al, 2010) where pain predominates (a RCT is currently planned to assess the effects of the glutamate blocking drug memantine in fibromyalgia to include magnetic resonance measurement of glutamate levels during treatment – Olivan-Blázquez, 2012).
Cognition

Problems with filtering out stimiuli (sensory gating) could contribute to the cognitive problems seen in chronic fatigue syndrome
It goes without saying that the disruptions in neural signalling caused neuroinflammatory issues that result in sensory gating deficits can lead to a wide range of cognitive problems involving memory, executive functioning and ‘disperceptions’ (from hallucinations to hypersensitivity to sensory inputs).
- Dig Deeper –Not Fatigue After All? New Model Suggests Other Symptoms Better Explain Chronic Fatigue Syndrome (ME/CFS) – Marco explores whether symptoms associated with sensory gating disorders provide better clues to ME/CFS.
Somatic symptoms
Nociception and Multiple Chemical Sensitivity (MCS)
As previously noted glutamate receptors are not restricted to the brain but are also concentrated in peripheral tissues including the heart, adrenal glands and the gastrointestinal tract. Glutamate mediated nociception (the detection and processing of noxious stimuli) may account for many somatic symptoms (Lin et al, 2011) including food and chemical sensitivities or indeed may directly affect the functioning of these peripheral tissues.
Given the evolutionary importance of the primary senses in survival, plus the anatomically small distance between the sinuses and amygdala (that amongst other things mediates emotional responses to stimuli and associated learning) it is perhaps not surprising that ‘noxious’ odours may trigger the release of glutamate (which potentiates memory which is how through experience we learn to avoid noxious stimuli) in the amydala (Hegoburu et al, 2009) which may then trigger the neuroinflammatory cycle.
Similarly, Martin Pall (Pall, 2002) proposed a model for MCS whereby ‘organic solvents’ trigger glutamate release leading to ‘long-term potentiation’ of glutamate receptors sparking a ‘vicious cycle’ involving glutamate and nitric oxide/pyroxinitrate ;
“Accordingly, if organic solvent exposure acts to induce excessive NMDA” (glutamate receptor) “stimulation, the subsequent nitric oxide increase may produce inappropriately high glutamate release, leading to inappropriately high NMDA and non-NMDA (AMPA, kainate, and metabotropic) receptor activity.”
Pall further suggests that “elevated levels of nitric oxide, peroxynitrite, and other associated biochemical changes” can produce all the symptoms found in MCS and those of other ‘overlapping conditions’ such as ME/CFS, Post-traumatic stress disorder (PTSD) and fibromyalgia which he proposes share the same underlying pathophysiology.
If such ‘long-term potentiation’ can take place in response to odors it must be at least plausible that a similar ‘overlearning’ process can affect other sensory inputs. For example, it’s long been recognized that chronic pain conditions can lead to more generalized pain hypersensitivity (Curatolo et al, 2006). In fact, recent research at McGill University suggests that peripheral injuries that result in chronic pain (where the pain is not initially due to central over-sensitivity) may leave a (potentially reversible) ‘trace’ in the pre-frontal cortex and amygdala regions of the brain due to epigenetic changes involving DNA methylation (McGill University Newsroom, 2013) suggesting that experiences as well as biochemical changes can influence gene functioning.
Fatigue and Exercise intolerance
Other somatic symptoms including the key symptoms of fatigue, exercise intolerance and PEM or NMH/POTS may appear on the face of it to be more difficult to explain on the basis of neurotransmitters alone.
Heart Rate Variability and Vagal Tone
A GABA/Glutamate imbalance could cause or contribute to the high heart rate and other cardiovascular issues seen in ME/CFS
Reduced heart rate variability and alterations in vagal tone have been reported in ME/CFS (Beaumont et al, 2012) and also in MDD (Licht et al, 2008) and anxiety states (Miu et al, 2009) both of which are associated with glutamate dysregulation. In the latter conditions it’s unclear if reduced heart rate variability results from antidepressant use although a recent study found the same problem in un-medicated patients (Kemp et al, 2012). These alterations have been ‘correlated’ with slow cognitive processing (Beaumont et al, 2012) and poor sleep quality (Burton et al, 2010) in ME/CFS patients. As discussed below, reduced heart rate variability is also a sign of autonomic dysfunction.
Breathing difficulties/dyspnea
Many ME/CFS patients experience breathing difficulties including shortness of breath/’air hunger’, shallow breathing, laboured of painful breathing etc associated with feelings of lightheadedness.
One recent large study comparing two cohorts of ME/CFS patients and controls found that subjective reports of breathing difficulties in patients were not associated with objective findings of obstructed breathing (Ravindran et al, 2012). The authors propose that sensory hypersensitivity, perhaps reflecting conflicting sensory inputs, without “airflow limitation” contributed to the experienced breathing difficulties in ME/CFS patients :
“Dyspnea is a sensation that requires intact afferent and efferent neural pathways, and may represent an imbalance between competing sensory input systems that gauge the musculoskeletal work of breathing, and the respiratory consequences of those efforts.”
Fatigue and exercise intolerance
Central
Once again ‘fatigue’ needs some teasing out. ME/CFS patients experience both mental and physical fatigue and either physical or mental stressors can result in PEM. To recap Rönnbäck and Hansson’s description of ‘mental fatigue’ discussed in Part II :
“Intense mental activity with high glutamate signalling can lead to astrocytes swelling, especially if their glutamate uptake capacity is impaired. This state, which is locked, may resemble the feeling of cramp in a muscle and the signalling takes a long time to be restored”
It may be that the physical fatigue experienced results from a similar process of ‘overload’ and a resulting ‘locked’ state or perhaps exercise induced pain and fatigue is due to a similar but less severe state of muscle spasm as seen in stiff person syndrome.
Physical exercise or mental exertion would also both increase oxidative stress and additional demands on mitochondria as well as producing a much increased influx of sensory information that is likely to ramp up the neuroinflammatory vicious cycle.
It may be plausible that the release of high levels of glutamate in response to the increased sensory input associated with physical exertion could temporarily overload glutamate receptors blocking further sensory transmission and resulting in a physical and mental ‘shut-down’. Speculatively, ‘sudden collapse’ following mental or physical exertion may in fact be protective, acting like a ‘trip switch’ to prevent lasting neurological damage due to glutamate excitotoxicity
Cort recently blogged on how Nancy Klimas has described her patients’ response to exercise
“Dr. Klimas noted that time sensitive gene expression studies have revealed the fascinating and possibly absolutely pivotal finding that during exercise the autonomic nervous system tanks first in ME/CFS and then it takes down the immune system. That ANS ‘tank point’ occurs when the body changes over from aerobic to anaerobic metabolism, a switch that occurs all too early for many people with ME/CFS.”
As will be seen below, glutamate and GABA play a critical role in the autonomic response to stressors and both fatigue and exercise intolerance are again associated with autonomic dysfunction.
‘Peripheral’ Fatigue
Of course, the ‘vicious cycle’ of glutamate excitotoxicity, oxidative stress, and mitochondrial dynamics, if also occurring in peripheral tissues could also result in ‘easy fatigueability’ that is not restricted to central mechanisms. Some research suggests a key factor protecting our cells against glutamate excitoxicity and oxidative stress may be impaired in ME/CFS.
Heat Shock Proteins
One further intriguing possibility involves the usually protective role heat shock proteins (HSPs) play in protecting the whole body against oxidative stress induced by a wide range of physiological and psychological stressors associated with daily living
Important role players in reducing the effects of glutamate excitoxicity, some studies suggest heat shock proteins are impaired in ME/CFS
Heat shock proteins are ‘molecular chaperones’ that maintain the physiological and functional integrity of organisms by helping to collect and recycle cells damaged by oxidative stress induced by environmental stressors. Aging may be considered the gradual malfunctioning of cellular repair mechanisms with HSP expression increasingly impaired with age. The findings of heat shock proteins at the site of neural ‘aggregations’ in neurodegenerative diseases such as Alzheimer’s, Parkinson’s and Huntington’s disease might suggest they provide a protective response against neurodegeneration (Peter Csermely and Ichiro Yahara, 2003)
Two groups of researchers however have independently found a defective (attenuated) HSP response to oxidative stress induced by exercise in ME/CFS patients (Thambirajah et al, 2008, Jammes et al 2009, 2011). In the 2011 Jammes study it should be noted that this dysfunction was most strongly associated with those reporting a prior viral illness or previously engaging in high intensity exercise
Intriguingly (in normal subjects) HSP production typically peaks at 48 hours post exercise (Morton et al, 2006) which accords with the description of post-exertional malaise/PENE in response to exercise in the International Consensus Primer (Carruthers, van de Sande, 2012)
“prolonged recovery period: usually 24 hours, often 48 but can last days, weeks or cause a relapse”
If the peak production of HSP’s normally occurs 48 hours after exercise (which suggests this may coincide with peak levels of oxidative stress) and this response is impaired, the delayed recovery (or exacerbation of symptoms) in ME/CFS is to be expected.
Furthermore, heat shock proteins also protect the brain against glutamate excitotoxicity (Mokrushin et al, 2005) and play a role in the immune response to viral infection (Santoro, 1994). A deficit in the induction of HSPs in response to stressors may again have both peripheral and central effect
The Autonomic Nervous System (ANS) – Autonomic dysfunction (NMH/POTS etc)
I won’t say too much about this as, while I have some of these symptoms, I haven’t looked into autonomic dysfunction in detail and I’m sure many are much more knowledgeable than me
However, it has long been suggested that both ‘CFS’ and fibromyalgia (plus overlap conditions such as irritable bowel syndrome, chronic headaches, irritable bladder syndrome, and temporomandibular disorders) all belong to a ‘spectrum of stress-related illnesses’ due to the role of the Hypothalamic-Pituitary-adrenal (HPA) Axis in the physiological response to physical or emotional stress (Crofford, 1998). As previously discussed, the rapid onset or increase in symptoms in response to ‘stressors’ is a key aspect of ME/CFS symptomology (as it is also with many autoimmune conditions including stiff person syndrome and potentially multiple sclerosis – Heeson et al 2007).

Studies suggest that both axes of the stress response, the autonomic nervous system and the HPA axis, are affected in ME/CFS.
Needless to say, several researchers have noted HPA alterations in ME/CFS and have correlated impaired negative feedback (required to terminate the stress response) and blunted HPA axis responsiveness with inactivity, depression and early life events (Papadopolous, Cleare, 2011). A similar alteration in HPA regulation has also been found in post traumatic stress disorder (PTSD), following chronic stress and also in depression, panic disorder, OCD, generalized anxiety disorder and bipolar disorder (summarized in Levy, Tasker, 2012).
When faced with a stressor it is essential that an organism can mount an appropriate physiological response. Glutamate release directly activates the HPA axis and the sympathetic nervous system and it has been shown that stress induced glutamate release ‘primes’ the HPA axis to respond to future stressors with the possibility that an extremely traumatic event (as in PTSD) may over-sensitize the HPA axis (Kuzmiski et al, 2010).
The balance between GABA and glutamate may cause autonomic dysfunction via their direct effects on the paraventricular nucleus (PVN) of the hypothalamus with GABA and glutamate inhibiting or stimulating respectively the PVN and therefore the HPA (Herman et al, 2006).
The balance between GABA and glutamate in the PVN also impacts on sympathetic nervous system outflow with glutamate increasing sympathetic outflow and GABA having a tonic effect to reduce this. Glutamatergic receptors within the PVN appear to have a particular impact on cardiovascular response and thus cardiovascular function including raising heart rate and blood pressure. Conversely GABA agonists decrease arterial blood pressure (BP), heart rate (HR), and peripheral sympathetic nerve activity (Herman et al, 2006)
It appears that both glutamate and GABA contribute to long term alterations in HPA function and response to stressors through neuroplasticity (Levy, Tasker, 2012). It has also been suggested that PTSD is essentially a hyperglutamatergic state (Ravindran, Stein, 2010)
Therefore the proposed vicious cycle which involves a hyperglutamatergic state can directly impact on HPA axis function with all the subsequent downstream effects associated with dysregulation. Autonomic dysfunction, with the sympathetic (fight/flight) to parasympathetic (rest/digest) ratio altered in favor of a chronic ‘sympathetic dominant’ state, has been reported a number of ME/CFS studies (Freeman and Komaroff, 1997; Newton et al, 2007; Beaumont et al, 2012)
It may be that chronic prolonged HPA stimulation by glutamate results in reduced receptor sensitivity and that the HPA eventually becomes hypo-responsive to normal stressors.
Peripheral and Autonomic Neuropathy
In Part II it was noted that (potentially glutamate induced) peripheral neuropathies were common in diabetes and metabolic syndrome, as a result of chronic alcohol consumption, following chemotherapy and had been found in a high percentage of fibromyalgia patients (this latter finding has recently been confirmed independently by a German research team – Üçeyler et al, 2013)
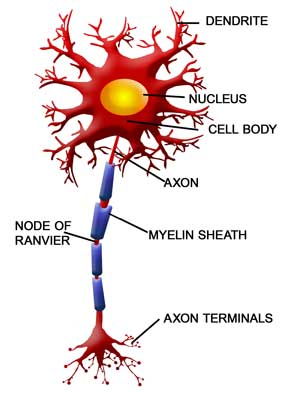
Damage to the autonomic nerves produces symptoms very much like those found in chronic fatigue syndrome
Autonomic neuropathy is also common in these conditions (and others including autoimmune diseases), affecting the sympathetic and parasympathetic nervous systems which “carry information from the brain and spinal cord to the heart, bladder, intestines, sweat glands, pupils, and blood vessels” (Pubmed Health, 2012). However, while autonomic dysfunction has been frequently noted in fibromyalgia, autonomic neuropathy has not (to my knowledge) been investigated in that condition
Common effects of autonomic neuropathy include various cardiovascular symptoms such as orthostatic or postural hypotension; reduced heart rate variability and tachycardia; absence of or increased sweating; loss of temperature regulation; facial pallor; bladder and bowel dysregulation; various vision problems; tinnitus etc (summarised at Patient.Co.UK). The most common early symptoms are urinary problems and orthostatic hypotension and cardiovascular symptoms can manifest as fatigue and exercise intolerance (Karayannis et al, 20
Historically, neuropathies have been associated with diseases such as beriberi (in its various forms including Wernicke’s encephalopathy) that result from a vitamin B1 (thiamine) deficiency (Lonsdale, 2006).
The symptoms of Wernicke’s encephalopathy include eye movement disorders, gait ataxia, confusion, confabulation (inaccurate describing of past or current events) and short-term memory loss (Wikipedia). In the context of the present discussion, it has been noted that brain lesions in an experimental rat model of Wernicke’s encephalopathy are exactly the same as those associated with glutamate excitotoxicity (Zhang et al, 1995).
In Wernicke’s encephalopathy, thiamine deficiency and glutamate promote excitotoxicity with thiamine deficiency resulting in a downregulation of the GLAST glutamate transporter thus impairing glutamate clearance from astrocytes (Hazell et al, 2003).
The results are “lactic acidosis, brain edema, oxidative stress, inflammation, and white matter damage” (Wikipedia)
It is highly likely that any thiamine deficiency would exacerbate an existing neuroinflammatory state.
Intriguingly, back in 1997, objective evidence of autonomic dysfunction in ME/CFS patients was presented and it was proposed that this was “consistent with a postviral, idiopathic autonomic neuropathy” (Freeman, Komaroff, 1997)
Lately, ongoing research at the UK’s Newcastle University has suggested that autonomic dysfunctional plays a central role in ME/CFS and can explain both physical and mental symptoms although the researchers propose that the problems arise peripherally as a result of skeletal muscle cellular membrane function rather than centrally (He et al, 2013).
Autonomic neuropathy therefore provides a direct link between glutamate excitotoxicity and the autonomic dysfunction evident in ME/CFS patients
Sleep Disturbance
You may recall from part II that a CDC study identified differences in polymorphisms and gene expression of two genes in ME/CFS patients involved in glutamate transmission and circadian rhythms which govern the wake/sleep cycle.
Additionally HPA axis dysregulation can also directly impact on sleep (and vice versa)
As seen earlier, ME/CFS patients show alterations in vagal tone and heart variability and these alterations have been correlated with poor sleep quality.
With a predominantly hyperglutamatergic state and a sensory gating deficit, it is highly likely that the continuous sensory input (plus ‘internally generated’ thoughts and anxieties) would make sleep difficult to enter and ‘unrefreshing’
Tinnitus
Tinnitus is a common symptom in ME/CFS. Although the percentages affected are difficult to obtain, the Ramsey definition of ME lists tinnitus as a symptom occurring at least as frequently as sleep disturbances. Tinnitus is usually preceded by hearing loss (due to exposure to loud noises, injury or infection for example) yet only approximately one third of people with hearing loss develop tinnitus (NIH – National Institute on Deafness and other Communication Disorders).
One novel theory (Leaver et al, 2011) suggests that damage to the limbic system (involved in emotion, behaviour, and long-term memory) and a significant loss of volume in the medial prefrontal cortex (an area of the brain that may modulate sensory information) results in the impaired ability of the limbic system to ‘gate out’ tinnitus signals from reaching the conscious cortex.
Depression is twice as common in tinnitus sufferers compared to the general population leading researchers to propose that similar mechanisms may underlie both tinnitus and depression and suggest that antidepressant medications may also help with tinnitus by impacting serotonin
As we have already seen, the ‘serotonin hypothesis’ of depression is rapidly giving way to a ‘glutamate hypothesis’.
A recent review (Smith et al, 2012) of the use of the GABA-B agonist Baclofen (as seen in Parts II and III Baclofen has been used for the treatment of alcohol withdrawal and stiff person syndrome) for the treatment of tinnitus concludes that methodological issues may have contributed to previous negative findings and that the use of Baclofen for the condition should not be ‘written off’ in Tinnitus
The preliminary findings that the injection of a glutamate antagonist directly into the eardrum has been found to be effective in treating tinnitus may provide further ‘proof of concept’ (Muehlmeier et al, 2011).
If tinnitus in ME/CFS is another manifestation of a glutamate/GABA imbalance then it may provide a non-invasive objective measure of the efficacy of treatments.
- Next up – Neuroinflammation, glutamate/GABA and the immune System in ME/CFS.
- Find the references to this blog here.
A Neuroinflammatory View of ME/CFS
- Not Fatigue After All? New Model Suggests Other Symptoms Better Explain Chronic Fatigue Syndrome (ME/CFS)
- Glutamate – One More Piece in the Chronic Fatigue Syndrome (ME/CFS) Puzzle? The Neuroinflammatory Series Pt. II
- Does A Rare Neurological Disorder Provide Clues to ME/CFS and FM? The Neuroinflammation Series Pt 3
- Scared Stiff? Exploring Anxiety, Autoimmunity and Infection in Stiff Person Syndrome – A Possible Model For Chronic Fatigue Syndrome
- When Definitions Obscure: A Neuroinflammatory View of ME/CFS
- Find the entire series here.
Support Health Rising!








Cort, I am looking at neuroinflammation as a result of an infectious assault on the brain, not the cause. Serotonin and glutathione insufficiencies are also happening as the continuous assault on neurological function. Yet, it is hard, once again, to say for sure, what happens in what order, and I seem to stay with the original models of this illness, and personal experience. Research can be interpreted in different ways, so if this is what you are seeing, then that is your opinion. Natural enhancements for the production of serotonin are preferable to taking antidepressants, if one is not depressed. I only found one drug responsible for increasing glutathion, appeared to be a psychiatric drug. When reading about the multiple effects of this illness on the brain, one can be overwhelmed. Yes, there were epidemics responsible for so many taking ill, yet tinnitus can occur in a perfectly healthy person. (failed to connect here…) I watched my father deal with tinnitus and other hearing issues until he had a synthetic stapes (stirrup formation in inner ear) implanted, and I was amazed at a young age. (He has been visiting an aircraft carrier and was not given headphones, thus the stapes shattered.) I must have been misunderstanding, as I thought tinnitus could be the result of hearing bloodflow through the area, and took an aspirin one time for it and it worked. (Placebo effect!) So sorry if this is appearing disconnected, bad day….
I am back to torture you again! I am surprised you don’t bring up neurotoxicity in your discussion of neuroinflammation. It seems quite possible that the neuroinflammation is coming from toxins that have either passed into the brain or have affected the brain through inflammation. The neurotoxicity could be caused by an onslaught of mold, chemicals, etc.
Not surprisingly excess glutamate is also associated with mold exposure. Dr. Shoemaker performs (or used to anyway) a special MRI that looks for excess glutamate of which I have.
It’s also worth looking at the genetic possibilities concerning certain halotypes. Many alternative docs find that a much higher percentage of their patients than would normally be expected have particular genetic profiles.
🙂 I am sincerely sorry floydguy, in the light of our recent discussions (especially as I’d stated that ‘mood disorders wouldn’t be mentioned much again) that this blog started with the aforementioned.
I can only say that these blogs were written months ago and that’s just the order they came up in – whereby I felt these symptoms could be dispensed with fairly quickly.
Not torture at all – a constructive discussion which is what I was hoping for; after all, any theory has to be tested to destruction.
Re neurotoxins – it is very plausible that they are one of the triggers. Just because mold exposure doesn’t figure in my background doesn’t mean it isn’t a factor for other people. I currently live in a approx 130 year old French farmhouse where the exterior walls are black from the fungus that feeds off the fumes from the Cognac distilling process. I don’t feel any better or worse than when I lived in a modern bungalow back in the UK.
I just don’t feel its the one answer – which I’ll get on to subsequently. On this issue I recommend the writings of the Gulf War illness researcher Beatrice Golomb who lays out a model for how the various putative exposures could result in the same pathology (in GWI and other ‘overlap’ conditions such as ME/CFS :
http://precedings.nature.com/documents/6847/version/1
I should note that I create the titles; the reason, believe it or not, that I put mood disorders in there is that it went well with MCS – a bit of alliteration – that was catchy. There’s also an issue of space…I put MCS in there because it was just three letters 🙂
Ha. I think you just wanted to torture ME!!
The mood disorders make me do it 🙂
So do you propose any triggers aside from mold exposure and pestide exposure? I think it is highly likely there are multiple roads leading to Dublin. For example, I’ve been told that at a cellular level I am close match to the Gulf War vets yet I’ve never served in the military and have not had unusual exposures – however there are few things that I am suspicious of like high exposure to Roundup.
Most definitely multiple routes either singly or in combination as I’ll discuss next. A similar model to that proposed by Mady Hornig who’ll be leading the pathogen study.
Aside from organic solvent exposure, mercury is also potentially causative. Mercury inhibits glutamate uptake and stimulates the release of glutamate in brain cells at micromolar concentrations. It is also linked to many of the biochemical abnormalities mentioned in this article and known to persist for decades in the human brain after oxidation to Hg++.
Mercury is another one of those interesting factors that MD with alternative bents test for and devise therapies to reduce it but which gets absolutely no play in the research world (that I can see). What a disconnect there is between physicians and research priorities in this area.
What about people who take L-glutamine supplements? I’ve been taking them for years and they seem to have positive effects rather than negative ones. And, could we draw any conclusions from this hypothesis about natural supplements to try? Should we all be taking GABA in supplement form, for example?
Sorry I missed you post yesterday.
In a healthy body and brain glutamine is necessary and supplementation is proposed to help with mental alertness (presumably why you take it?).
Given that, in the brain, glutamine is a substrate for both glutamate and GABA (and glutamate converts to GABA) I’m not sure if the problem is glutamate levels per se or extracellular glutamate (either not being cleared via glut transporters or converted to GABA).
If you’re finding benefits by all means carry on – this is a hypothetical model.
As regards GABA supplementation it may be worth trying but many patients use GABAergic drugs and supplements.
Long term changes in the brain due to neuroplasticity may take a prolonged period of treatment to resolve.
Thanks! I’ve been taking L-Glutamine for years as general digestive and immune system support.
Interesting, I think neuroinflammation could explain a huge part of what is going on. I’ve taken LSD 3 times since being ill with CFS/ME (been ill for 2 and a half years now, I am virtually housebound) and each time my symptoms have gone away COMPLETELY for 3 days afterwards. LSD is a powerful anti-inflammatory and I did feel very much like i had received a deep massage from the inside of my body out-wards, like cooling balm being rubbed on a hyperactive frazzled nervous system. I was able to walk a few miles and play the guitar and sing for hours with strong fingers and a strong voice (can’t usually do that at all!) as well as read much more during the 3 days post-tripping. My symptoms returned quickly however and a week later (on all 3 occasions) I was just as ill as before I took it, so it’s positive effects are short.
This has led me to the theory that neuroinflammation is causing a lot of my CFS symptoms. Sadly one cannot take LSD regularly as the profound spiritual and emotional experience it induced need integrating in to daily life and it’s just not convenient. But I am curious about BROMO-LSD, a non-hallicinogenic form of LSD being developed for cluster headaches. Perhaps that would have the same effect and could be taken regularly enough to be beneficial long term for CFS/ME sufferers? I wonder if you have come across anyone else with similar experience, as I seem to be one of the only CFS sufferers to have tried LSD while ill…
Really interesting, John. I hope you can dig into this more and figure out what LSD did that worked so well…Never heard of Bromo-LSD – sounds really interesting as well.
Quite a story John!
I didn’t know that LSD was anti-inflammatory but did turn this up (in relation to schizophrenia :
“Serotonin (5-HT) and Schizophrenia
The idea that serotonergic alterations might have a role in the pathophysiology of schizophrenia initially developed from several indirect findings. Firstly the observation that Lysergic Acid Diethylamide (LSD), a psychedelic agent which shares structural similarities with 5-HT, can cause schizophrenia-like symptoms such as hallucination and perceptual abnormalities. This led to the hypothesis that psychosis may be caused by brain serotonergic dysfunction
However the findings from the LSD studies were later found to be more complex to interpret, not least because some of the effects of LSD on 5-HT receptors result in enhanced glutamate transmission”.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3662992/
The last sentence might seem to be the opposite of what I’m suggesting (high glutamate) but as the above paper discusses in relation to dopamine, negative effects are seen with too high or too low dopamine. The same U shape response also seems to apply to glutamate.
Plus the model I suggested relates to the neuroinflammatory effects of high ‘extracellular’ glutamate. ‘Enhanced glutamate transmission’ may mean just that. Glutamate is being transported, used and taken up again efficiently rather than building up in the extracellular spaces where it causes neuroinflammation.
Interesting stuff.
It’s the mercury. Google “Andrew Cutler, PhD” for accurate info on how to safely chelate it out of the body. Takes 2-4 years, but people have actually recovered.
Wow! Great article, though I must admit, as sick as I am it took me a week to read through it + a lot of re-reading.
I found this article b/c I was trying to find a correlation b/w neuroinflammation and severe fatigue. I’ve been diagnosed with CFS (took 10 yrs) but there are so many unanswered questions and no CFS doctor has been able to help at all. Then I was diagnosed with PANDAS syndrome – suggesting neuro-inflammation.
For me the first symptoms were overactive bladder at age 7. Now the bladder is one of my worst symptoms. At 15 I was injured but the pain never went away, this has repeatedly happened so I just have severe pain where there was once an injury. At 18 sudden onset of anorexia nervosa, depression, and fatigue though by CFS standards I would be considered “high functioning” though could not sleep, onset of insomnia that no doctor has been able to treat (even trialed xyrem).
I went through every AD and psych med out there then did ECT without any benefit from any of them. 2008, sudden onset of adrenaline and anxiety 24/7, 6 months of no sleep. Antipsychotics and xanax would get me a couple hours of sleep. 2009 – bedridden + new onset of severe mental fatigue and headaches. 2010 sudden onset of ocd, worsening of fatigue, excessive daytime sleepiness, inability to sleep though extremely tired and sleepy, to present: mostly stuck in bed or on couch, ocd all the time, no quality of life.
Just typing this to see if anyone has any ideas. I had major violent reactions to tiny doses of the stupid immunomodulators……….. CFS docs unable to treat symptoms. Have severe OI. Neurologist bailed on me after diagnosing PANDAS. I have been referred to Dr. Souhel Najjar who specializes in treating neuro-inflammation connected to psychiatric ailments, but not sure if I’ll be accepted.
Excellent article though. I can see how this would explain a lot of “CFS” symptoms. BUT BIGGEST QUESTION – what is the treatment? Steroids seem risky b/c of all the infections we have, insurance won’t cover IVIG……. ETC. etc.
It was a toughie but goodie :)….
Thanks Christiana
Until researchers investigate ME/CFS as a neuroinflammator disorder we can only speculate on how to treat it. Re PANDAS perhaps the Lipkin/Hornig and Rituximab research will turn up something valuable.
Something you could try (as its cheap and safe) is high dose thiamine (B1) as Cort discusses here :
http://www.cortjohnson.org/blog/2013/07/05/is-simple-relief-from-fibromyalgia-mecfs-found-early-reports-spark-interest/
As discussed above B1 deficiency is neurotoxic and would exacerbate existing neuroinflammation. Some anecdotal reports are very positive.