Gut bacteria are a hot topic in medical circles right now, but few studies have assessed their impact on chronic fatigue syndrome (ME/CFS). This Irish and Swiss study asked if inflammation was present in ME/CFS, and if it was, if a single gut bacteria (Bifidobacteriun infantis 35624) could reduce it. The answers were yes, and yes.
The answers, with some proviso’s, were yes, and yes.
Inflammation
The inflammation/sickness behavior theory suggesting increased levels of cytokines and other immune factors cause fatigue and pain, etc. in ME/CFS makes sense given the disorders infectious onset and symptoms, but inconsistent study results have given some researchers pause.
This study, however, suggests that three of the big pro-inflammatory actors, all of which could send your symptoms soaring, are increased in ME/CFS, and the authors placed ME/CFS in the same class of ‘chronic inflammatory disorders’ as ulcerative colitis and psoriasis. (One proviso – the ME/CFS patients were not age, sex and BMI matched to the healthy controls (many of whom were probably from a University.) Age, sex and BMI can affect cytokine levels)
Let’s take a quick look at these markers.
- C-reactive protein (CRP) – Produced in response to increased levels of pro-inflammatory cytokines such as TNF-a and IL-6, CRP levels reflect systemic inflammation. Increased CRP levels in a CDC study were associated with reduced physical functioning (SF-36) and depressed mood in ME/CFS. Increased CRP levels in a MERUK study that were associated with markers of cardiovascular risk suggested a low-grade inflammatory state is present in ME/CFS.
- Tumor necrosis factor – TNF-a plays a major role in producing inflammation. Several ME/CFS studies have found increased TNF-a levels and others have not. One study proposed that a TNF-a network (IL-2:IFN-γ:TNF-α network) played a key role in ME/CFS.
- IL- 6 – a pain producer extraordinaire, one study found increased levels of IL-6 in ME/CFS,and a gene expression study suggested increased IL-6 levels after exercise could contribute to the increased pain after exercise seen in this disorder.
A Bacterial Boost
With B. infantis significantly reducing the levels of all three pro-inflammatory markers, it appeared that eight weeks of B. infantis supplementation did reduce the inflammation present in this disorder.
A look at the charts provided suggested that a subgroup of ME/CFS patients had particularly large reductions in inflammatory markers while most had moderate to mild reductions. Enormous reductions in CRP levels, for instance, found in three or four patients, for instance,contrasted with more moderate reductions in others (and some increases in others).
One question that had to be asked, given the lack of information on symptom improvement, was whether the intervention actually showed up in the patients lives.
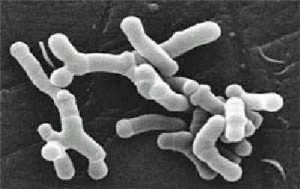
Focus on Bifidobacterium infantis
Bifidobacterium infantis 35624 is a commercial probiotic formula produced by Procter and Gamble. One of the few probiotic strains to undergo testing at the research level, numerous studies have examined B infantis effectiveness in irritable bowel syndrome and other disorders.
According to a probiotics website B. infantis strains produce much higher rates of thiamine, nicotinic acid and folic acid that other Bifidobacterium species. ( A number of different B. infantis strains exist.)
B infantis administration for 8 weeks did not significantly alter gut microbiota in infants but did so in IBS patients (although symptoms did not improve). A large 2006 placebo controlled, double-blinded study, however, found that B. infantis was significantly more effective than placebo at improving gastrointestinal symptoms in IBS. A recent meta-analysis of probiotic studies in IBS suggest that probiotics can assist with symptoms in that disorder.
A quick drop in B. infantis levels after the supplementation stopped, however, suggested probiotic administration probably needs to be permanent. B. infantis improved gastrointestinal symptoms and reduced antibodies in celiac patients but did not affect intestinal permeability.
Conclusion
A small placebo-controlled, double-blinded study suggested that a commercial probiotic (Bifidobacterium infantis 35624) can reduce inflammatory markers that may contribute to fatigue and pain in some ME/CFS patients. A chart review indicated a subset of patients had remarkable drops in inflammatory marker, and most had mild to moderate reductions. Past studies suggest ongoing B. infantis supplementation is needed to to confer results.
No information was provided on symptom improvement; we don’t know if B. infantis improved symptoms or not. Dr. Klimas’ research, however, suggests inflammation after exercise causes much symptomatic distress in ME/CFS.
- Check out our ME/CFS/FM Gut Resource Center for more information on the Gut and Chronic Fatigue Syndrome
- Check out Ken Lassesen’s blogs for his take on gut manipulation in ME/CFS






Another great help is Symbiotics brand of Immune Colosturm. Very soothing, calming and effective.
And just because it applies, I’m going to repeat myself with talking about GastroCrom – it helps to regulate mast cells but also plays a big role in helping with the immune system at the gut level. Many of us POTS people are on it and it has been of great benefit to many of us.
Probiotics are great if you get the right strains and populate the intestines with good bacteria vs. bad.
Good review Cort. Keep the info coming. You give us something to think about and then to implement. Change for the better!
Issie
Thanks Issie, I always learn alot from your posts….Onto colostrum – something new to learn about 🙂
I get that some strains of probiotics work for some people and others don’t. It’s going to take awhile to figure all this out.
Along with colostrum – a lot of research has been done on lactoferrin (an active substance within colostrum) and possibly more useful. An example of the many papers: http://www.ncbi.nlm.nih.gov/pubmed/19083463
It also acts as a prebiotic which should work well in conjunction with most probiotics.
Maury
caution is required with probiotics. I have tried some probiotics and got worse on them. A number of probiotics boost the wrong cytokines for CFS people!
this is interesting research. Might be worth emailing the researcher and finding out if there was any anecdotal evidence of symptom improvement
I think I may have a similar experience; not sure because so much else was going on at the time…but I’m going slow.
This is very intetresting in light of the differences between individual strains of B. infantis. If a mix of strains are used, the results suffer. There’s something about B. infantis 35624. Might be interested to know it was isolated from gut tissue removed during resection surgery of an otherwise healthy donor. Doesn’t guarantee results, of course, but strongly suggests this is one of the positive ones.
There is another article (at least it appears to be a different citation) published in the current issue of Gut Microbes:
“Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut”; Groeger D, O’Mahony L, Murphy EF, Bourke JF, Dinan TG, Kiely B, Shanahan F, Quigley EM; Gut Microbes 2013; 4:325 – 339; PMID: 23842110; DOI: 10.4161/gmic.25487
Hi Cort and Issie, I find your mention of mast cells interesting. After seeing a dermatologist over a year ago, and having suffered with what I believe is mast cell disease from too much histamine being released into the blood through the cerebral spinal fluid’s substance P, I figured it out for myself that it is indeed the mast cell issue. for years I have dealt with the tiny pinhead itchy rash all over my body, increasing at times, decreasing others but no rhyme or reason as to why.
I’ve had chronic sinusitis for years. I’ve just gone off of gluten and dairy at the suggestion of a holistic np who said she’s already determined I have leaky gut as my folate showed elevated in bloodwork. Do you know anything about the elevated folate? I am 60 and well past menopause. Just wondering if getting mega high doses of Vit D is the best thing to do and/or b12 injections, that she’s talking about doing……
A little curious about this before starting one or both of these regimens….any advice is appreciated….
Thanx…..Brenda
Cort- Know this is off subject somewhat of Probiotic. However wanted to ck something else out with your members and bloggers. I have recently had a sleep study done by a specialist. This has probably been the worst year I have had in 10. Anyway- he rec I go on a Cpac machine and mask. I did 3-4 weeks ago. The reason he wanted me on it as I quit breathing as the study confirmed 25-30 times per night. I would wake up startled and with Palpitations. We went with the Palpitations and Cardiologist never mentioned sleep study. I have been on machine 3-4 weeks as I said and I cannot tell you the difference in my energy level, dizziness, even Gut problem. I also changed Probiotics to VSL#3 -2-3 times a day. Then increased my Mothers Earth Humic Acid formula
from 1/4 tsp to almost 2 tablespoon. However all of the other came after a week on CPAAC machine and mask. If many of you as I was are told you have serious heart issues – please consider seeing a sleep specialist. There are many types of sleep Apnea.
This has changed my life as of 3-4 weeks ago. Not easy to get used to-but the longer I use it the better I feel..
I was told by one of the top CFIDS Dr. I was in Heart Failure. BULL MANURE!!!!! He keeps people coming back to him by telling them they are so sick-no one else can help them.
This may be old news to many of your more educated bloggers. I feel it has saved my life.
San Diego #1
Cort forgot to mention. The improvement in Neuro is astounding. I am able to concentrate, think clearly for a change and mental fatigue is much improved. OXYgen, Oxygen. OXYgen.
TO BE CONTIUNUED The machine I use also has a humifier in it.
SAN DIEGO #1
Wow – San Diego – that’s fantastic..
Keep it coming….Any one who has an experience like this PLEASE ‘hijack’ a post to get the word out.
It does make a huge difference. I have apnea too. There are two kinds – one is obstructive and occurs in the throat when the muscles relax and cut off the airways, the other is due to the CNS (central nervous system). For us with dysautonomia (POTS, OI, etc) there can be issues with both kinds and some of us have found this to be a problem. Oxygen does make a difference and if your brain doesn’t remind you to breathe having a machine force you to – is for sure a good thing. When the autonomic nervous system is mess up – we need all the assistance we can get.
Issie
Hi Cort,
Great article, thanks so much. I have just ordered the Natren life start, the brand of this probiotic in Aus, and am starting it tomorrow. I hope that I see some improvement in IBS and inflammation, I will be sure to post if I do. I have been disappointed with other probiotics, they have all been the type that add to neuro excitotoxicity. Thanks for the comment about Mast Cells Issie, I have POTS and have been to an immunologist but he wasn’t keen in testing for MCAD, I’d be interested in hearing how you get tested for this and by whom. Weirdly I used to take Gastrocom in the form of Intal when I was a child for asthma.
I hope it works out. I think we have a huge amount to learn about probiotics but studies do suggest that this one can help the symptoms of some people. Good luck with it!
There are several specialist here in the USA that are testing for MCAS. There are different things that they do. They will have you do a urine test after a flare occurs to check for different markers and they also need to do a blood draw within an hour of a major flare to check your tryptase levels. Dr. Afrin is doing tissue samples via a special stain and using esophagram testing – with tissue taken during the test.
They will also rule out allergies with traditional allergy testing. You may find that you have those also. I had immune testing done in checking IGG, IGM, and IGE levels. I have hypogammaglobulinemia – low IGG levels on subset 1 and therefore low autoimmunity. (Despite this – I have an overactive immune system. My body is attacking itself. Faulty signaling and recognition at play.)
I also had a very scary ER visit which was mast cell related that affected my heart called Kounis Syndrome. The treatment for that is massive antihistamines, nitroglycerin and IV’s. I had this reaction to sugar free gum that had aspartame in it which created an imbalance in my glutamate levels and caused a mast cell degranulation and a very expensive overnight stay at the hospital. With the doctors thinking I was having a heart attack – but, no heart damage – thankfully.
My doctor at Mayo, AZ (who is a neurologist) is trialing GastroCrom with some of us that have EDS (Ehlers Danlos) and HyperPOTS and have symptoms (yet possibly not caught with science) of MCAS. I think of all the ones that I’ve talked to only one did not stay with the GastroCrom. All the others found that it made a big difference for them in how they felt and in their reactions and responses to stimuli (exercise, excitement, foods, sex, crowds, stress, emotions —etc.) It is a very expensive medicine and one I would not be able to be on without insurance. For some, they are finding that ketotifen is of benefit. That is not available here in the US but some are obtaining it from Canada. I have not tried that – as the GastroCrom is working for me and I can get it with my insurance making it affordable.
Interesting that you have had it before. Would you be able to obtain it again and see if it makes a difference for you?
Issie
I’ve been studying methylation pathways and mutations that can happen in the genes that causes the dysfunction of this pathway. It has to do with folic acid (MTHFR), B12, sulfur/sulfa and other things. If there is a mutation in your pathways it means that you may not be utilizing the vitamins that you take – they could potentially show up as high – but, not be used at the cellular level and you getting benefit from it. Depending on what your mutations are and where the break in the pathways are —would determine whether or not the B12 injections would be of benefit to you. Many of us are finding that we can only tolerate the methyl form of B12 and/or methyl folate. There are actually other things that you may need to work on before these things would be assimilated and unless you work on those first —it may be a waste of your time and money. My suggestion is to do a 23&me genetic test and when you get your results download your raw data into Genetic Genie and see where your mutations are. From there you start to learn what the mutations mean and where you need to start to get this up and running. For some of us that have CBS mutations and issues with sulfur/sulfa we have to address that with diet first and then some supplements and then we add in the methyl form of B12 and possibly methyl folic acid (if needed). One thing I learned is that some need a very small amount of lithium orotate (homeopathic amounts) that will help the B12 to be uptaken by the cells. This also helps with brain function and neurotransmission. (This is a very tiny amount – not amounts used for bipolar people). This is a very complex and deep subject – but, I think will prove to be very valuable. It is controversial and is in it’s infancy of understanding. I can say that my addressing my mutations and using some of the things suggested and a change in diet – has been a big benefit to me. Hope this helped!
As for MCAS – there probably is an autoimmune component to this. GastroCrom has been one of my greatest helps as has been my low-fat, vegan, whole foods diet. That also addresses the immune system. I can’t stress strongly enough DIET. Something we all have control over – yet few address. Some are also using ketotifen if GastroCrom isn’t available or unaffordable. Along with that I nightly use Allegra and 1/2 of a Zantac. This is necessary to block H1 and H2’s. I was told not to ever take an H2 without an H1 because if you block the H2 and not the H1 it will convert into an H1 and make the allergy reaction worse. I find this combination great for me and the key was the GastroCrom.
Cort, let me know how the colostrum works for you. You may find that it really calms down your sympathetic reactions and completely relaxes you. It’s one natural way to add immunoglobulin without doing IVIG. It may help your immune system to balance out and helps to calm down and heal the gut. (That’s what it’s done for me.) 🙂 Glad you are learning from me. Makes me feel good when someone benefits from what I’ve learned.
Issie
(I asked Cort if it was okay to list these links. I didn’t want to take away from his great article or hi-jack his post. He said to go ahead – so here they are. Hope it helps some of you.)
There is info on the Inspire forum. There is info on EDS and MCAS on this site. There are some threads that can’t be accessed unless you are a member – but, there are many that can be accessed with you not signing up.
http://www.inspire.com/
For MCAS there is a girl in the UK that has it very badly and has a site with lots of information that she has put together.
http://www.iamast.com/
There are also several MCAS sites that predominately talk about MCAS – these both require membership.
http://mastcelldisorders.wallack.us/yabb/YaBB.pl
http://uk.groups.yahoo.com/group/theelephantproject/
Lots of ways to find information. You can read forever and still not learn it all.
I was telling someone earlier tonight – when you start to research into these things, you realize there is such a close connection between them all. It’s like the blind men and the elephant in the room and depending on the angle that you look at the animal is what you perceive as it’s view – but in the end it’s all the same animal.
https://en.wikipedia.org/wiki/Blind_men_and_an_elephant
Of course, I have my theories of what the final results will be with the connections between them all. I’m trying to work on that for myself —we will see if I’m right. 🙂
Issie
Great stuff Issie, I’m really interested MCAS and I heard Dr. Klimas is as well. 🙂
I love that there are connections between these disorders that have not been made explicit yet. Maybe we can help to do that. 🙂
Cort, where did you hear that Dr. Klimas is interested in MCAS?
During some talk recently I remember her saying the mast cell connection was really interesting. It was brief comment.
Oh, forgot to add . . . .with the colostrum —-take it early in the day as it gives you energy. (Sounds like something really good for ME/CFS – doesn’t it.) If you take it too late in the day it may keep you alert, awake and full of energy.
I hope that we maybe help some with what we learn. The more I learn the more I realize how little I know and how much more there is to learn. I’ve always tried to share my “light bulb moments with others”. You never know, what one thing, may make a difference. If we, personally, don’t put something together – maybe, someone else will be able to from what we share. The information is out there — it’s just compiling it, connecting it, and somewhat looking at it from a different angle. Todays theories and ideas are tomorrows facts. It all started with someone looking at and thinking about something from a different angle. Then that idea is researched and either proven or dis-proven. It takes a brave person to put that idea out there —risking criticism. I think there’s a few of us willing to take that leap —who knows what we will discover.
Issie
Are you talking about Bofidiflora here, I had use Intestiflora and Bofidiflora and I feel great!relocate, don’t know where to find it now.
Keep in mind that there a many many studies on the health benefits of probiotics, and this is just one study amongst many.
And keep in mind that Proctor and Gamble have the resources and motivation to research and promote their favoured probiotic, and good reasons to ignore other potentially beneficial probiotics.
This study doesn’t mean that this specific probiotic is necessarily better for health than many of the other zillions of bacteria found in our gut.
And also keep in mind that lowering levels of certain immune activity markers doesn’t necessarily mean that these probiotics are particularly helpful.
There are many different claims made for many different probiotics, prebiotics, fungi, and other supplements.
I have come across many different claims for probiotics over the years, and I personally think some may be helpful, for some health issues, in certain situations, for some people, but maybe of very limited help in many situations.
(Some strains have helped me personally for occassional short-term IBS, for example when I had a thyroid problem, and after I’ve had a stomach bug.)
Keeping all of that in mind, I just did a search for this specific probiotic, and have found it for sale on Amazon, sold under the brand name ‘Align’…
UK:
http://www.amazon.co.uk/Align-Infantis-35624-Probiotic-Supplement/dp/B000W4PNDS/ref=sr_1_1?ie=UTF8&qid=1373986457&sr=8-1&keywords=Align
USA:
http://www.amazon.com/Align-Infantis-35624-Probiotic-Supplement/dp/B0031RGL66/ref=sr_1_1?ie=UTF8&qid=1373986765&sr=8-1&keywords=align
Well said Bob! Thanks…
The Align probiotic labels now say b. longum.
http://www.nowfoods.com/Supplements/Products-by-Category/Digestive-Support/Probiotics/Probiotic-10-50-Billion-50-Veg-Capsules.htm#.UeVyeOHn_IU
This is the one I’ve been using. It’s hard to get, it gets sold out very fast. Has a lot of strains of different bacteria and seems to make the most difference for me. However, it does not have that particular strain of bifido. This brand can be ordered on-line from many places at half off the normal retail price.
Issie
I have CFS/Fibro and Ulcerative Colitis and have been using “align” probiotic ( B. infantis 35624) for about 9 months. I can’t say that I’ve noticed much difference in my pain and fatigue levels however, I have noticed a big improvement in my UC symptoms. It might be too soon to tell but if my condition is helped to this level it will be worth the premium price of the “align” brand. And yes that is the only brand on the market to contain that strain of probiotic. The large grocery clubs and Amazon seem seem to have the best prices for this. Thank you Cort !
Another two probiotics with a lot of research supporting immune and gut enhancement in humans are Bifidobacterium animalis and Lactobacillus rhamnosus. I know there is a Clinicians product with both of these in it (Multiflora Digest) and possibly others.
My son has been taking both of these for nearly 2 months (apparently should take 2-4 weeks before any improvement is noticeable) and has been improving slowly but steadily (but these are not the only things we are trying, so I can’t guarantee a link).
Read the review on the US Amazon page (above) about the potentially toxic fillers, stabilizers, colors etc.in the Align product. I don’t know if P&G has any experience in making healthfoods but this is a big disappointment, especially considering the cost of the product. I wonder how much it really differs from regular Bifidus Infantum, which is available from other manufacturers?