



Diet and Chronic Fatigue Syndrome (ME/CFS)
Even a short scan of the published medical literature on the impact of diet, specifically food allergies and intolerances on chronic fatigue syndrome (CFS) would lead you to conclude dietary modifications have no impact on either the onset of or a recovery from the illness.
Back in 1996 researchers in the Journal of the American Dietetic Association found no specific nutrient deficiencies in ME/CFS and concluded diet did not play a role. Dietary guidelines for CFS remain as those recommended by the CDC in the US and abroad; CFS patients should simply follow the official government “balanced diet” guidelines which promotes high levels of starchy carbohydrates like gluten-containing breads and cereals.
Could they be missing something? I propose that two disorders associated with sensitivity to the gluten products in grains, Celiac Disease (CD) and Non-Celiac Gluten Sensitivity (NCGS) are vastly underdiagnosed both in the general and CFS population. In fact, studies suggest in undiagnosed gluten sensitivity is contributes to early mortality.
Definitions of CD and NCGS:
“CD is a much greater problem than has previously been appreciated” Archives of Internal Medicine February 2003
- Celiac Disease – refers to people with total villous atrophy in the gut as a result of immune sensitivity to gluten (gliadin) which has resulted in autoimmune antibodies to the gut lining
- Non-Celiac Gluten Sensitivity – includes broadly two classes of people, first those with only partial villous atrophy or inflammation in the gut (which the current test for CD misses) induced by sensitivity to gluten, and second, people with no gut imbalances at all but autoimmunity to other organs and systems (e.g. thyroid) induced by sensitivity to gluten
Autoimmunity and Celiac Disease
“Gluten sensitivity is a systemic autoimmune disease with diverse manifestations…Lancet Neurology March 2010
As you will read below, both untreated Celiac and NCGS appear to significantly increase mortality rates and CD is being implicated in almost all autoimmune disorders. .
Autoimmune disorders are now cumulatively the third leading cause of death in the industrialized world.
While many individual autoimmune diseases are rare, collectively they are thought to affect approximately 8 percent of the United States population – 24 million persons. To provide a context to evaluate the impact of autoimmune diseases, cancer affected approximately 9 million people and heart disease affected approximately 22 million people in the United States
NIH. Autoimmune Diseases Coordinating Comm.Autoimmune Diseases Rearch Plan, 2006
With diagnostic rates at about 1 out of 3 people, some form of autoimmunity is probably present in at least 72 million people in the US.
You are 10 times more likely to develop an autoimmune disorder if you have CD.
More than 19,000 papers on CD and the new entity NCGS have been published in PubMed. Despite (or maybe because of) the voluminous data, no one has worked connecting the dots and synthesizing the results in a way that both patients and busy practitioners can get… Enter Dr Tom O’Bryan, formerly busy physician himself and a functional medicine specialist.
Dr. O’Bryan specialized in the treatment of Celiac and NCGS before giving it up to train other Doctors and practitioners around the world full-time on the subject. This man Dr. Bryan, you might say, is on a mission.
In this article I aim to summarize key information from trainings Dr O’Bryan gave in the UK in 2011 to nutritional therapists and doctors.
I can almost guarantee your doctor or gastroenterologist or specialist ME/CFS doctor doesn’t know much of this information and probably doesn’t grasp its potential significance in ME/CFS.
A list of resources for further education with Dr O’Bryan can be found at the end of these series of articles as this article only covers a partial amount of the information.
|
“Dear Niki
|
Surprised Diet Could Play a Significant Role in Such a Serious Disease as Chronic Fatigue Syndrome?
Patients and practitioners alike may be surprised that diet can play a critical role in serious chronic complex illnesses such as ME/CFS. Some may even feel downcast that “just diet” and not a virulent bug that is the cause or a major contributor their ME/CFS.
Misconception and Misdiagnosis
Misperceptions regarding the nature of food ‘allergy’ that still permeate much of the medical world are at the root of this misunderstanding. “Classical” approaches to understanding food allergies assume reactions to food can only be IgE mediated. IgE produces classic allergic reactions such as sneezing, sniffling, rashes and difficulty breathing. We know from the research that IgE food allergies are likely to play only a small role in CFS patients.
Celiac disease (CD) and non-celiac gluten sensitivity (NCGS), however, are IgG and IgA mediated immune responses that can cause chronic gut inflammation, and very likely chronic inflammatory and autoimmune processes elsewhere in the body.
The Inflammatory Disease ‘Epidemic’
Inflammatory disorders have been increasing rapidly over the past thirty years. Chronic inflammation and autoimmune processes are implicated in ALL of the major chronic complex illnesses that blight humans today. The studies covered in this blog suggest a ‘fire in the gut’; i.e., untreated gut inflammation may increase the risk of early mortality in all major chronic illnesses
For a variety reasons covered later, including the intriguing evidence that at least a subgroup of the ME/CFS population has an autoimmune disorder , the facts about CD and NCGS need to be fully understood.
This article will show why most research studies on dietary modification in ME/CFS have find no improvement, while studies using nutritional approaches in clinics like I co-founded are showing statistically significant improvement in CFS patients.
Read my full bio HERE
At the end of this series of articles is a special discussion section for CFS/ME patients, covers the implications of the CD and NGSC research for ME/CFS, plus steps concerned ME/CFS patients can take next.
10 FACTS YOUR DOCTOR OR GASTEROENTEROLOGIST PROBABLY DOESN’T KNOW ABOUT CELIAC DISEASE AND NON GLUTEN CELIAD SENSITIVITY (NCGS)
“…for every symptomatic patient with celiac disease there are eight patients with celiac diseaseand no gastrointestinal symptoms.”Gastroenterology February 2001
 FACT 1 – Due to a Historical Misconception that Celiac Disease (CD) MUST Present with Gastrointestinal Symptoms, CD is Vastly Underdiagnosed.
FACT 1 – Due to a Historical Misconception that Celiac Disease (CD) MUST Present with Gastrointestinal Symptoms, CD is Vastly Underdiagnosed.
“We found a high-prevalence of CD between CD FMs, and most of them were asymptomatic.” European review for medical and pharmacological sciences.
The chances are if you have few or no GI symptoms, your Doctor won’t have tested you for CD. Nor is CD part of the differential diagnosis for ME/CFS. Unfortunately, doctors don’t realise that neurological symptoms and a wide range of other non-GI symptoms, most of which are found in ME/CFS, should trigger the test for CD.
The current guidelines for celiac disease suggest testing for it in “chronic fatigue, short stature, delayed puberty, dental enamel defects, elevated liver transaminase levels, dermatitis herpetiformis, and nutritional anemias…
The brain seems to be particularly vulnerable… Pediatrics August 2001
CD was originally believed found in people with diarrhea, cramping, bloating, constipation and other gastrointestinal issues, stool problems, anemia and weight loss. Further research revealed CD and its offshoots commonly cause fatigue, weakness, osteoporosis, joint and bone pain, migraines, numbness and tingling, depression, etc.
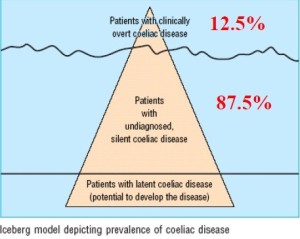
“The iceberg is a common model used to explain the epidemiology of coeliac disease. The majority of patients have what is termed silent coeliac disease, which may remain undiagnosed because the condition has no (GI) symptoms.”British Medical Journal July 1999
Although celiac disease has been known for over thirty years to cause both gastrointestinal and neurological symptoms, it took until 2000 that celiac disease was shown, in some individuals, to cause only neurological symptoms. As late as 2010, a review article in Lancet, no less, noted that ‘only recently’ has it been accepted that celiac disease can present with only neurological symptoms. In fact, it appears that most people with CD who have neurological symptoms don’t have gastrointestinal symptoms.
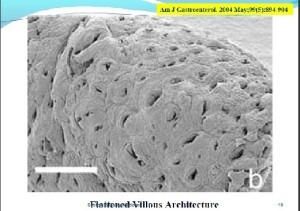
 FACT 2 – A Diagnosis of Celiac Disease Refers to the End Stage of the Disease and Requires Total Villous Atrophy
FACT 2 – A Diagnosis of Celiac Disease Refers to the End Stage of the Disease and Requires Total Villous Atrophy
CD takes YEARS to manifest and is preceded by GUT INFLAMMATION. These earlier stages may be described as part of Non-Celiac Gluten Sensitivity (NCGS) but, like, celiac disease, also still mostly go undiagnosed and untreated.
If you had a negative test for CD that means you didn’t have total villous atrophy. You could, however, have partial villous atrophy or increased lymphocyte activity in the gut lining which standard testing for CD misses.
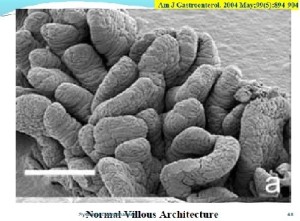
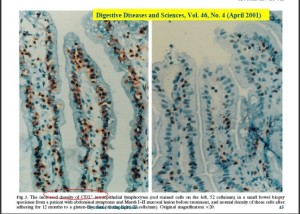
The villi, with their finger-like projections, appear like shag carpets in the gut. The villi, with their high surface area, maximise nutrient absorption from the gut.
If you have partial villous atrophy, or no villous atrophy at all; your CD test will be NEGATIVE.
A large amount of inflammation in the gut can still occur in people not testing positive for CD. In fact, it’s clear that the processes that result in total atrophy of the villi begin much, much earlier and are often evident if they are looked for. In fact, some researchers believe the search for the roots of celiac disease should begin early in life, perhaps even in utero .
Normal Vs Atrophied Villi
Normal looking villi appear like the below:
Below is total villus atrophy (required for coeliac disease diagnosis):
Total villous atrophy doesn’t occur overnight. The gut inflammation (mucosal intraepithelial lymphocytosis) that usually precedes the war zone-like structures occurring in total villus atrophy, can be identified. The lymphocytes shown in brown, below, are producing the cytokines that will eventually destroy the intestinal villi, leading to “total villous atrophy” or “CD.”
Indeed, studies suggest that the degree of lymphocyte invasion present is a more effective and certainly earlier test for gluten sensitivity than charting the degree of atrophy of the villi. Inflammation (lymphocyte invasion) comes first, followed by damage to the villi, followed by destruction (atrophy) of the villi.
The presence of gluten induced autoantibodies is another early test which, if the person keeps consuming gluten, appears to be able to predict the ultimate demise of their villi – (and their ultimate diagnosis as celiacs.)
If we include now not only all CD, but also all those with NCGS, how many people suffer from some form of gluten sensitivity?
312 family members (FMs) of CD disease patients were tested for all types of gluten sensitivity ie: CD, subclinical and silent forms. 1 out of 5 FM tested positive – suggesting 20% of the population have some form of gluten sensitivity.
 FACT 3 – Untreated Celiac Disease (CD) and Non Celiac Gluten Sensitivity (NCGS) Is Associated with Increased Mortality Rates Than Celiac Disease
FACT 3 – Untreated Celiac Disease (CD) and Non Celiac Gluten Sensitivity (NCGS) Is Associated with Increased Mortality Rates Than Celiac Disease
Your mortality rate is HIGHER with NCGS AND CD and does not require the end-stage of total villous atrophy
“The elevated mortality risk for all causes of death combined, reflected, for the most part, disorders characterized by immune dysfunction” Archives of Internal Medicine July 2003
A large Swedish Inpatient Registry study investigating mortality risks in more than 10,000 CD patients over 30 years found having CD increased the risk of death from a plethora of major disease. The study examined standardized mortality ratio (SMR) which charts the increased likelihood of death if you have both CD and another disease. The SMR of 11.4, for instance, in non-Hodgkins Lymphoma (NHL), for instance, indicates a person with CD and NHL is 11.4 times more likely to die earlier from Non-Hodgkins lymphoma than someone with that disease and no CD.
Note that most of these disorders are associated with immune dysfunction.
- “Non-Hodgkins Lymphoma (SMR 11.4)
- Cancer of SI (SMR 17.3)
- Inflammatory Bowel Diseases (SMR 70.9)
- Autoimmune Diseases (including RA) (SMR 7.3)
- Diffuse disease of Connective Tissue (SMR 17.0
- Allergic Disorders (ie.asthma) (SMR 2.8) Diabetes (SMR3.0)
- Disorders of Immune Deficiency (SMR(20.9) Tuberulosis (SMR 5.9)
- Pneumonia (SMR 2.9)
- Nephritis (SMR 5.4)”
The largest ever study of mortality rates found celiac disease in almost 10% of 350,000 plus biopsys collected over 40 years, ‘latent’ CD (normal mucosa but positive blood work) in about 1% (3.7K), and inflammation but still partially intact villi in about 5% (13K) of the biopsies
Results showed increased mortality rates in all three cohort groups; startlingly, mortality rates were highest in the inflammation (Non-Celiac Gluten Sensitive) group.
- HRs in Coeliac disease (HR, 1.39; 95%) (i.e. 39% more likely to die earlier)
- HRs in latent Coeliac disease (HR, 1.35; 95%) (35% more likely to die earlier)
- HRs in patients with inflammation (HR, 1.72; 95%) (72% more likely to die earlier)
When Ignorance is Not Bliss
“Individuals with Coeliac disease are treated with a gluten-free diet, while very few with inflammation are. Those with inflammation may have an overall worse prognosis than those with villous atrophy, since institution of a gluten-free diet often leads to normalisation of the mucosa.”Journal of the American Medical Association Sept 2009
What could account for such a large increase in mortality in what appeared to be the least severely affected group? Proper diagnosis. The study authors suggested that people with celiac disease tend to get diagnosed and heal their gut. People with NCGS, however, often don’t get diagnosed. In their case it’s not the celiac disease that gets them but the long-term inflammatory state that increases their risk of dying from another disorder.
Focus on Children
“Children diagnosed with Coeliac disease had a threefold increased risk of long-term mortality. This is in marked contrast to the experience of adult Coeliac disease where the long-term increase of mortality was modest. The increased mortality in children from external causes may reflect behavioral change associated with coping with a chronic disease and its treatment.” American Journal of Gastroenterology April 2007
 FACT 4 – Having CD/NCGS and Not Ahering to a Gluten Free Diet Can Increase Your Risk of Death 6-fold. The Equivalent of 1/90th of a Slice of Bread Can Cause Severe Symptoms in the Most Sensitive. CD/NCGS is Permanent
FACT 4 – Having CD/NCGS and Not Ahering to a Gluten Free Diet Can Increase Your Risk of Death 6-fold. The Equivalent of 1/90th of a Slice of Bread Can Cause Severe Symptoms in the Most Sensitive. CD/NCGS is Permanent
“Death was most significantly affected by diagnostic delay, pattern of presentation, and adherence to the GFD…Non-adherence to the GFD, defined as eating gluten once-per-month increased the relative risk of death 6-fold…Our results emphasize the need for prompt diagnosis and treatment also in those patients with a minor or symptomless form of coeliac disease”
A Lancet study following up 1072 adult Celiacs and 3384 first-degree relatives after 20 years found the SMR of 2.0 (200%) i.e. if you have CD you are twice as likely to die early than someone without it. Remarkably, eating even small amounts of gluten, placed celiacs at increased risk of death.
Gluten Intolerance is Permanent
“Coeliac Disease is a permanent intolerance to gluten that results in immunologically mediated inflammatory damage to the small intestine mucosa” American Journal of Clinical Nutrition March 1999
Gluten-related disorders are permanent; while your gut may heal, your gluten intolerance remains and adding gluten back into your diet will eventually cause the inflammation to rear up again.
Studies have found that even after five years on a gluten free diet, the gut will eventually flare up if you return to eating gluten products.
In some cases even very small amounts of gluten can cause system-wide problems.
|
Nutrition Review in Sept 2004
A frustrated 34 woman went to a Celiac specialist to find out why, after following a gluten-free diet for a year she was still not better. Testing revealed her antibodies were still sky high and she had total villus atrophy and osteoporosis. She was suffering from hair loss, poor skin and chronic fatigue, but had a good attitude. The specialist asked how strict her gluten-free diet was. After being told she was still eating the odd amount every month, she was told to cut out gluten completely. A year later her energy was a bit better and her antibody results were high normal instead of sky-high, but her endoscopy results were still bad and she still had hair loss and osteoporosis. The specialist agreed she was indeed on a gluten free diet but then discovered the lady was a Nun, and she was eating a small piece of host (sacramental bread) daily. The specialist met the priest and asked for a sample of the host. The specialist measured it and found that a 30 mg fragment of wafer contains approximately 0.5mg of gliadin (1 mg of gluten). The woman refused to give up her daily sacrament until her priest prevailed on her to do so. Eighteen months later the woman came back radiant with a full head of hair, a healthy small intestine and no chronic fatigue. The fragment of the wafer was half a thumb size.
|
Read the Next Two Parts:
Resources
- Find out more about Niki here
- Dr. O’ Bryan’s 1 day Doctors training on Gluten on DVD for US Practitioner
- Dr O’Bryan’s 1 Day Training on Gluten for Practitioners in the UK
- Dr O’Bryan’s DVD on Gluten for patients in the US
- Dr. O’Bryan’s 1 day seminar on Autoimmunity












Diet is probably the key to us regaining our health. It’s the one thing we have complete control over —yet, it’s the one thing people refuse to change. No changes = NO CHANGE.
If one is sensitive to something even a small amount is like eating poison. Would you take even one drop of poison into your mouth and not expect bad consequences? When a person has a sensitivity to something this is how your body reacts to it.
My doc feels that many people are reacting to the arginine in wheat bread. It’s an interesting thought and I’ve found that high arginine foods seem to bother me. He feels that this helps to feed and make happy a protozoa and co-infection spread by mosquitoes and ticks that is similar to malaria and associated with Lyme disease – that I was found positive for.
My husband is not a true celiac but strongly reacts to gluten and has Crohn’s of the esophagus. A very small amount of wheat and he has reflux and inflammation of his esophagus and a cough. He has to take allergy meds for this if he gets exposed to it. This does help him, he has to use both an H1 and H2 for this.
I’m looking forward to reading your future articles. Job well done. I’m on board with you here. I think DIET is the key to our regaining our health.
Issie
Check this out from the New York times (http://www.nytimes.com/2013/08/01/booming/answers-about-rheumatoid-arthritis-part-3.html?pagewanted=all)
. I caught a video on celiac disease. I had all the symptoms and then some. I changed my diet: no wheat or gluten. Within three days my joint pain was at least half what it was. No swollen hands and fingers, back pain was gone and neck pain too. I have a ruptured disc in my neck, but no more sleeping on heating pads to reduce the spasms in my neck and low back, for a few restful hours of sleep. No more antidepressants, no more pain pills. Three weeks now, and I feel like I’m getting my life back. I’ve been saying, I feel like 18 again, but I don’t look it at 56 years old. I want to tell everyone, gefore drugs, change your diet and cut out all wheat and gluten. The drugs are a deadly Band-Aid and if I only knew I would have never taken the drugs. Best of Luck, Barry W. — Bear8357, America
The Doctors response was interesting….She kind of mildly pans it – pointing out where it doesn’t work, how expensive it is (why is it more expensive???), how difficult it is, how it doesn’t work for everyone…and then refers to classical celiac; she obviously has just sketched the surface. She does tie it with autoimmune disorders….In the end you feel kind of deflated 🙂 instead of inspired by this persons experience. Hey, if it only happens in 5% of patients – that’s still 5%
In my experience many try eliminating various foods or supplementing with others, but this doesn’t always seem work in the long term. It is difficult and expensive to be on a gluten-free diet. I have great respect for those who can maintain it. Of note, people with celiac disease ( who truly cannot tolerate gluten) can have joint symptoms, so this may explain the response to this approach in a few. Also both R.A. and celiac disease are autoimmune diseases and can occur together. If you have abnormal bowel habits, weight loss, unexplained low bone density you should ask your doctor if you have celiac disease. It occurs in 1 percent of the population, mostly in those of northern European descent. R.A. also is present in about 1 percent of the population.
OHHHHHH, this could get me on a rant. What????? I’m using Dr. McDougall, Forks over Knives and Engine 2 diets as my vegan lifestyle choice. This is what has helped me in the last 7 months get onto the road to recovery. These diets advocate a low-fat, whole food, vegan lifestyle. There are scientific reasons for this choice. People who decide to go this route, don’t just wake up one day and decide I’m going to stop eating any animal products and eat no oil or processed foods —just because. We have to educate ourselves as to why this may be a healthier choice and then how to do it for it to be a healthy lifestyle choice. Anyone who is a vegan and knows about nutrition and vitamins – realizes that we need to take B12 and maybe iron and iodine. These are the three things my doc keeps monitored – along with Vit D.
But, for someone to need empirical evidence and peer reviewed journals – is ridiculous. For one thing – lots of the papers are slanted to convey the opinion of the writer and even though it is peer reviewed – that opinion doesn’t lose translation if the basic idea can be supported with science. But, if you have a bunch of people saying something is making a difference and it continues to over time. My ears are going to perk up. If it has helped them, then maybe it will help me. If it’s a placebo effect —yayyyy! If it gets the results you want. Then don’t question where the gift came from. Lots of things will not get the money/grants behind them to show empirical evidence. But, if you have people reversing heart disease, arthritis, CFS, MS, cancer with something —even though it may not have the millions of dollars of research behind it to make the pharmaceutical company money —-then take note.
The vegan lifestyle has lowered my grocery bill. It is a cheaper lifestyle. And I buy mostly organic. So, that’s no excuse to use. I’ve gone to the Farmer’s Market and taken $30.00 and bought enough veggies and beans to last me for 2 weeks. How much cheaper can you get? And I am gluten free too.
Ha!Ha! Told you I could go into a rant about this. Better stop before I get a book going on this. 🙂
Issie
Getting off gluten and dairy and most sugar I am feeling remarkably better in these past ten weeks or so. My cognitive abilities have been returning to an almost acceptable level. I am sixty now and have to recognize I have lost some major brainpower in a decade of having minimal usage of it.
I also went through menopause during some of that time and that also affects our brainpower. I have more energy and wake up more refreshed now than I have in years. I was sleeping 10-12 hours a night, now six or seven hours does the trick. My psychiatric nurse practitioner took me off of the gluten saying she could blame half or better of my symptoms on the gluten and dairy and she was right.
Not as much drainage of the sinuses now that I am off dairy. I drink almond or lactose free milk. I miss some of the pastas and breads but it’s worth staying away from.
I highly advise every single person who has any of these diseases to try the gluten free diet and those with chronic sinusitis to toss out the dairy goods. Sugar seems to affect my muscles and I get headaches too. I usually use Stevia now, on everything.
Congratulations Brenda, getting off dairy and gluten products can be difficult. I noticed that lots of bread etc. made me feel foggy and tired and cause my joints to ache. Now I’m now removing all gluten from my diet.
Niki’s statement that even small amounts of gluten can be problematic kind of woke me up. Congratulations on feeling better 🙂
That doctor must not have read this incredible story of a young boy with juvenile rheumatoid arthritis who recovered completely – but only after getting off of gluten for a full SIX WEEKS! This is what kind of keeps me up at night….
Dr. Klimas also said you have to be on a diet for 6 weeks to tell if it’s working. Except for the macrobiotic diet I tried early on (in which I did feel much better at first (hmmmm) but then started losing weight like mad)) I’ve never been on a diet for six weeks in my life. Some wheat always crept in there…
Anyway, check out this story..From a cripple really, to healthy – it’s amazing.
http://www.nytimes.com/2013/02/03/magazine/the-boy-with-a-thorn-in-his-joints.html?pagewanted=all
Beautiful story. Makes your heart glad that these parents didn’t stop until they found an answer for their child that made sense. Now, he may have a life.
There is one girl who has POTS on one of the forums that I’m on, that had ataxia (unsteady gait and walk – that required assistance). It took almost a year of being gluten free and this resolved for her. She tells everyone to get off gluten – because many of her neurological problems got better.
Issie
I think this is a great topic to bring up particularly to doctors. There is a huge rate of misdiagnosis and this seems to be something a lot of people don’t get tested for. My understanding is that they have new gene tests now which can help especially when the biopsy or antibody tests are indecisive, but no matter how good the test is, it won’t do any good unless someone orders it. 🙂
http://celiacdisease.about.com/od/diagnosingceliacdisease/a/Celiac-Blood-Tests.htm
BTW, I micromanage my diet and this helps control certain symptoms, but I am still severely ill and disabled.
I am confused about total villous atrophy being required to diagnose Celiac because it looks to me like a Marsh score of 1 could be used to support this diagnosis (as well as other diagnoses). (total atrophy looks like a Marsh score of 4).
http://celiacdisease.about.com/od/diagnosingceliacdisease/ss/MarshScore_3.htm
Maybe this is a requirement unique to NHS? (Though I could think of a US HMO that I wouldn’t be surprised to find doing something similar.)
I’d encourage everyone to try a gluten free diet. I suffered from fatigue, sometimes brain fog, depression, dizzy spells for years. When I went gluten free I had enough energy for trips to the gym and was gradually improving my fitness levels. The brain fog and dizzy spells vanished. However excess exercise caused a very severe relapse and I was more ill than before, I could barely get out of bed. So it certainly isn’t the entire answer for me but it gave me my life back for several years and might have been permanent but for my crappy gps advice.
I have since improved thanks to vitamin D and N-acetyl-csteine and went back onto gluten for a month for a coeliac blood test, should have been 6 weeks really. My test was negative. During that time the symptoms didn’t recur but as I fear it may have been causing inflammation that would eventually cause damage I am again gluten free. It is more expensive and it’s tricky to eat prepared to food unless you are used to reading labels. I find travelling very difficult.
When gluten is unavoidable I take Peptizyde enzymes (Brits can get them here http://www.mandimart.co.uk/afp-peptizyde-original-90-capsules-112-p.asp) to reduce the damage. There are other enzymes but these are available in the UK.
Of all the interventions I have tried this was one of the best. I know others have gained nothing from it but everyone should first have the coeliac blood test, then give it a try for a month.
Thanks Tatt, I think alot of people fit into your category – staying away from gluten helps and is not the answer but they’re very grateful for that 5 or 10 or 20% increase is wellness.
Some doctors liken ME/CFS to leaking lifeboat; I can’t imagine with all the food and other sensitivities that gluten sensitivity isn’t one of the leaks in many peoples lifeboats.
I don’t find being gluten free difficult at all at home; during travel – you’re right – its a real bear 🙂
Hi Tatt, and others who have pointed out they went gluten free and got some improvement, and to others who may have gone gluten free and not improved at all, there’s some very important information coming up in part 2 of this series of articles about the fact that it is known many diagnosed cases of Celiac don’t improve on a gluten-free diet. It’s likely due to ongoing unhealed leaky gut and a self-perpetuating cascade of inflammation which has been triggered and which must be halted, so being gluten free is necessary – but probably not enough for significant improvement in some. Watch this space for part 2 and 3 where we’ll cover this.
Best
Niki
been away on holiday or I would have commented before – for me gluten free was not 5-10% improvement but more like 50% within a month and 90% over time. I thought I’d completely solved my problems and just needed to recover from the deconditioning. Sadly it wasn’t true but you see why I’m keen for people to at least try. And it doesn’t have to be too socially limiting as a standard meat and potato meal is fine if you don’t add gravy. In Britain there are even a few places where you can get gluten free pizzas and more restaurants include GF options all the time. I do encourage the trend by posting on the Facebook pages of places that don’t.
Hi everyone,
I have had ME/CFS since 1990, but was not diagnosed with silent celiac disease until 2005. 15 years of unfound autoimmunity.
I believe my celiac disease was triggered during the birth of my child. If genetically susceptible, it can be triggered by anything at any time. It could have also been triggered during a gut flu I had prior.
Anyway, it was not found early enough and then I caught the flu which turned into ME. I believe that my gut was damaged at that point already by celiac disease, allowing the infection to invade gut to brain very easily (I have enterovirus diagnosed by Chia). Unfortunately the gluten and dairy free diet has not helped many symptoms at all and the healing is as silent as the active illness was even 7 years later.
Everyone missed the diagnosis (and I had some good docs) because I did not have typical gut or deficiency symptoms so that is where the silent came in. My two sisters were also then diagnosed celiac. They both are in excellent health (unlike me) with no GI symptoms. So we are a family with silent active celiac disease. Weirdly, none of us feel better off the gluten and I am the only one due to ME to do the diet as strictly as required. My gut biopsy showed pretty healed within two years but not M.E. I was very disappointed.
Gluten free labelling of foods is also interesting. One has to remember there is a tolerance of about 20 ppm on foods even if labelled gluten free and many times there is more than that in there. It is tough to keep cross-contamination away even in my home, (my husband eats gluten); never mind in packaged foods or at restaurants. It is socially isolating which is not what an ME person needs. ie: No one has invited us for dinner because of it except my parents. Everyone is afraid to cook for me.
There are gene studies available that you can order to see if you are a candidate for it, and also a self-blood test from a pharmacy.
It turns out about half of my ME/CFS friends have celiac or severe sensitivity to gluten/ some dairy and the other half have been diagnosed with Lyme. These are things that must be ruled out first thing and are now both in the ME/CFS Primer along with all the other conditions which must be checked.
Lastly never do a gluten-free diet until you find out by at least blood work if you have celiac disease or it will not be found once you heal and people find it very hard to stay on the diet if there is no noticeable improvement and no positive celiac test.
There are tax breaks on the extra costs of gluten free food in Canada and many other advantages in the medical world to know if you have it. Also all other first degree relatives should be tested once one family member is found.
Sorry for the length on this but it has been quite a learning curve for me and my family, and I feel very strongly that there is a strong association between ME and Celiac and that they may even have common genetics for some of us. (I have been trying to get researchers to look at this)
I was positive on two different blood tests for celiac disease and the villi after biopsy was an absolute mess. Here I had been trying to heal ME/CFS for 15 years with full-on active celiac disease. I strongly suggest people ask for the blood work. It is very sensitive as long as the IG A IGM and IG G antibodies are at good levels. Those need to be tested as well to make sure that you have enough antibodies to react. They can change the test to an antibody type that you do have acting.
Thanks Valerie – your story shows what a convoluted situation Celiac and NCGS is. It was really eye-opening for me to learn that you don’t need to have gut symptoms to have celiac or NCGS..
Did I get this right? You don’t feel better on a gluten free diet but your gut villi are better; so your gut has healed which is good – but it hasn’t really improved your symptoms; ie something else is going on.
Is that right?
That is exactly right, Cort. The GI specialist who I begged to run the celiac test (who laughed at my request I might add due to my CFS history), did it hesitantly. In the end, he was wrong.
It was sad because I just finished elaborate CFS testing and treatment with an independently paid Canadian medical doctor/alternative expert costing about $10,000 that year. It was when I did not improve from that including IVs, supplements, diet changes, acupuncture, etc. that I went to the GI specialist as a last resort and just asked for the celiac test (I have no idea why I came up with that).
It was devastating to see all the excellent docs and research I had done did not include that as something I should have pursued long ago.
I was really hoping I would heal up nicely after that, but I did not.
Before knowing, while on small amounts of gluten, I did not have gluten symptoms that I knew and ate out in restaurants regularly(probably did neurologically react but didn’t know because of the CFS). But now, seven years later, if I make a small mistake and ingest gluten, within four hours I am projectile vomiting as if the body has been poisoned. So weird. Even the GI doctor could not guarantee improvement because I had been ill with ME for so long with a very neurological case.
There is the immune and infection properties that remain unaddressed now with ME/CFS along with all the stuff we don’t know.
I will add that I had experts assert anorexia as well as that I just wasn’t eating because I was thin before the celiac diagnosis. Noone tested me for celiac at that time. I ate like a horse and very healthily my whole life, growing up on a grain farm (ironic). My parents are not active celiac but I have a DQ2 gene from each of them so I have two ( not good luck and a serious form) which means I have passed at least one to my daughter. She is sensitive but not celiac at age 24.
I have learned that gluten these days has a huge percentage more gluten per grain than when my parents were young raising us. They are now 85 and healthy. Food modification is triggering celiacs due to increased gluten volume in the foods.
People have to remember that herbs, powders, oriental extracts, and supplements can be riddled with gluten containing fillers, excepients, and preservatives. Some are not labelled. So much fun…. I hope this info helps someone.
I write about it a lot in my upcoming book about ME/CFS including my experience and the stories of others. Good topic and easy to test for. Everyone, do it.
It’s been awhile since I’ve seen an ME/CFS doctor but no one has ever suggested an Celiac test or the test Niki will refer to in the next blog, which looks for inflammation in the gut.
With that vomiting after ingesting a little gluten – you’re definitely still Celiac… Niki will get into the permanence of the condition, as well, in the next blog.
With the EDS, Sjogren’s Syndrome and now this Celiac stuff, this has been a month of learning for me. 🙂
Cort, I just wanted to enforce that celiac disease is mainstream medicine – unlike CFS or ME in North America. There is no excuse for ignorance in the medical profession for this. It is well known and well taught. Anybody with an immune illness of any kind should rule out celiac disease and doctors know this. The blood work is simple and advanced, and the biopsy, although golden standard, is not absolutely necessary if the blood work is obviously positive. This is so different than ME/CFS so I don’t understand why people are not tested and helped in this area early on. I was reading an article today called “Your Brain on Gluten” in the Spring 2013 publication of Allergic Living, and it speaks of almost identical symptoms and signs of ME/CFS such as brain white matter lesions and grey matter diminishing of the brain if undiagnosed and untreated. So similar and yet so separate.
I have had a third cousin at age 5 diagnosed with celiac and she too is not recovering in a quick and normal fashion with gluten-free living. They are trying removal of all grains and other things. It is tough and creates so many problems for so many. Again, the biomarker is easy and affordable. And yes, it is a life-long condition…no cheating…ever….
“it appears that most people with CD who have neurological symptoms don’t have gastrointestinal symptoms.”
True for me. I didn’t have any gastrointestinal symptoms but the doc recommended I try gluten free anyway. To humor her I did and it didn’t make any difference that I could notice. Then I read a book about GRAIN INTOLERANCE and lactose intolerance: Breaking the Vicious Cycle
(http://www.breakingtheviciouscycle.info/) It explains the Specific Carbohydratre Diet in a book by Elaine Gottschalk, biochemist and nutritionist. It also says these problems can cause autism. It has recipes. You can read excerpts from the book on Amazon.
I stopped eating any grains and within a month my neurological symptoms were much better. I began to lose excess weight without dieting for that purpose and to have more energy.
I don’t find that eating grain-free is any more expensive. I just eat a lot more vegetables, which are pretty cheap. Beets, carrots and lettuce are my daily staples now. I once tried to be a vegan — disastrous results. No energy at all. I’m carnivorous, probably genetically, but eat only eggs, cheese, poultry and fish. There are dozens of kinds of beans and hundreds of different ways to prepare them. Once you start eating them regularly, your body will produce the enzymes to digest them, but use Beano at first if you need to deal with gas.
I still eat dairy, but only cheese and my homemade yogurt and kefir, fermented for at least 24 hours to convert ALL the lactose to protein. Commercial yogurts let some lactose remain because it makes the yogurt taste sweeter, something marketing tells them customers want.
I stopped eating any sweets, sugars, etc long ago. I do think of them as poison. I see white sugar and I think of rat poison. In fact, most white foods are contraindicated for most people, if they have been refined at all.
“Enriched” on the label of cereals and breads reminds me of a joke told by George Carlin:
I’m waiting at the bus stop and a mugger takes my money but gives me back enough for bus fare. When I get home I say “Guess what, Mom! I’ve been enriched!”
I didn’t know that 24 hour fermentation got rid of all lactose – that’s huge. I just started making soy yogurt but I would love to make kefir.
I’ve toyed with removing all grains. Rice sometimes gives me instant lethargy. Sweets I’m going to have to keep working on…I know they’re no good for me.
Thanks for the ideas…and the link.
Great article Niki, and those terrifying mortality figures will have me rethinking my attitude to the occasional ‘treat’ gluten and diary wise.
What does HR stand for in your article above? Many thanks
Hi Annie
Good question. It stands for Hazard Ratio for death. So people with Celiac have a 39% increased risk of death, those with gut inflammation have a 72% increased risk of death…
Thank you for the article! It makes me wonder about some things.
I wonder how gluten sensitivity is related to sensitivity to biological neurotoxins.
If you have an HLA-DQ 2, then you automatically have a mold-susceptible haplotype. There are only two haplotypes with the DQ2, as far as I can tell from what Dr. Shoemaker has published: the 7-2-53 and the 17-2-52a. Both make a person less able to detox mold toxins. How would those sensitivities interact?
I wonder how gluten sensitivity is related to blood type. Dr. D’Adamo (I think) who invented that eat right for your type diet, says that only blood types A and AB can eat wheat. Blood types B and O are not supposed to eat it. In my family, there are four of us with a DQ2. The two people with blood type B have Celiac Disease and borderline Celiac Disease. The two people with blood type AB do not. (at least by the standard tests that have been done so far).
I wish there were a branch of medici e that just studied inflammation, and the things that cause it. I wish someone would figure out how all these factors are related.
Hi Forebearance
Well I don’t think the two are necessarily directly linked (mould sensitivity and gluten sensitivity) however what is interesting is that gluten sensitivity is a type of immune mediated intolerance, where gluten can drive inflammation, eventually increasing the risk of autoimmunity, and it is not the old conventional understanding of “allergy” – which was IgE mediated. And interestingly mould and a whole range of chemical toxins can cause exactly the same immune response as gluten. So in the next post we will be talking about state-of-the-art testing for gluten sensitivity, and interestingly this same lab has brought out its latest test array for autoimmunity which includes testing for about 20 chemicals and mould…
So chemicals and mould can have not just a toxicological effect on the body (i.e. being poisonous to humans) , but also an immunological effect. This will be covered in the next planned series of articles on this site.
Who is susceptible to developing sensitivities to these things depends on genes and other environmental factors like processed food in general in the diet for example. So you mention the genes Shoemaker has stated which may possibly make some people more susceptible to mould intolerance – perhaps because they are not detoxing it properly. There could be similar polymorphisms in some people’s methylation cycle and CYP450 liver enzymes which means they don’t detox chemicals as well as others.
We know there are genes which make people more susceptible to developing Celiac disease, in fact a recent study just showed over 50% of the population of Australia is susceptible to developing Celiac disease! This may seem to fit with the very common blood type 0 who should avoid wheat according to D’Adamo, but I think that is more to do with tolerance of lectins in foods – I haven’t studied the papers on which specific genes make people susceptible to CD but we will be covering it very likely in the next articles (probably part 3) and a planned “Gluten Alert” page on this site…So I guess, watch this space!
By the way there are definitely branches of medicine studying inflammation and connecting all the dots – anyone working with a “systems biology” approach – which includes the Institute for Functional Medicine and also anyone involved with the science of psychoneuroimmunology (PNI) – there are many, it’s certainly my main approach and all my up-coming articles will be based on this kind of “complexity theory” approach.
Hope this helps 🙂
Hi Niki,
Thank you so much for your reply. I am really glad that you are one of the people who are interested in connecting the dots! And that we have you here.
Have you ever read the work of Ritchie Shoemaker? If not, I would encourage you to take a look at it. It sounds like there is a lot of overlap between the effects of gluten and the things he has figured out about the immune system. He describes a condition he calls Chronic Inflammatory Response Syndrome.
Hi – ah very interesting. I have read Desperation Medicine by Shoemaker and studied his early work in some detail – his work links with people like Dr Patricia Kane’s on lipid membranes, neurotoxins and fat metabolism in general, and I just had a look at his latest published papers online. I may go back on what I previously said about a link between gluten and mould sensitivity. This paper by his research group http://www.survivingmold.com/docs/Exposure_to_water_damaged_buildings_causes_a_readily_identifiable_chronic_inflammatory_response.PDF
…seems to suggest that people exposed to mould in water damaged buildings develop gluten sensitivity – could this be a another cross-sensitivity risk with gluten! Thanks for the prompt – more research required…
I suffer from CFS. It started long ago when I was 12 yrs old after I got mono. The fatigue just never left. I am now 34 & the fatigue is much, much worse. Over the last 8 yrs a lot of random symptoms have gotten much worse & through my extensive healing, a few have gotten better. In regards to this article, completely cutting gluten out wiped COMPLETELY wiped out all of my joint pain! I highly suggest for anyone who suffers from any health issues to do an elimation diet & slowly reintroduce foods to see if you notice a difference w/ any of your symptoms. Or you have the opition to get a blood test done to test your IgG antibodies to certain foods. I started eating gluten again thinking I needed some in “my system” to get an accurate test. The way I felt the next day was enough confirmation! The test was $560… A lot of money when I had the answer I needed on my own.
Cort, I heard of your site from Dr. Teiltelbaum’s Facebook page. I am currently a patient of his. I am curious… Have you tried IVIG? Also, are you familiar w/ Dr Beck & his micro current device? Great info! Thank you!
Thanks Gina. Glad to hear you got relief from that. As I noted earlier something is definitely going with me with nightshade plants, joint pain and inflammation and probably wheat as well but only when I eat alot of it.
We are an interesting group. Unfortunately, it seems we all have to try everything and see which ones work…..(sigh).
I haven’t tried IVIG or Dr. Beck’s approach but thanks for reminding me of that. I meant to look into that.
Thanks for relating your experience.
Thanks for your reply cort. We sure are an interesting Grp 🙂
Curious… is your response to the nightshades immediate? I will surely look into this for myself too.
I am Gfree, dairy free, sugar free & recently stopped eating meat (just to see if it helped). Also, I eat almost everything organic & very clean (no processed food). It isn’t easy!!! :-). But, desperate to feel better! I am towards the end of my protocol w/ D. T. Though a lot of things have improved, I still have a lot of fatigue & muscle pain. We are starting to focus on all of the active viruses. My high titters maxed out the blood test through my GP. Next week I will get my results to see where they actually are.
So… I am hopeful that treating the viruses & boosting my immune system will be the final piece of my health puzzle. Have you checked your IGg antibodies to CMV, EBV, HHV-6, etc?
Thanks for your article.
I had ME/CFS 20 years ago and found cleaning up my diet – no wheat, no dairy, no caffeine, alcohol or sugar – helped me to recover the most of anything I did. Now sadly I have overdone it again and have been back with CFS for the last 18months.
The first consultant I saw was a complete waste of time and told me that diet was irrelevant. Stupidly I followed his advice and didn’t get better. Now with two new consultants I have just tested positive for CD and for secondary hypothyroidism (I am on thyroxin) and had a vitamin D deficiency that was undiagnosed also. It seems finding the right doctor is the first battle!
I have now not been eating wheat for a month however I feel the best when I cut out all grains completely. I have started on the paleo diet and have found it gives me the most amount of energy – it really makes a massive difference. Even my beloved porridge is out.
My immunologist has put me on Vitamin B12 and a form of Vitamin E – Tocotrienol – that he says should help my cells repair from the damage done by wheat. I wait and see, although he has also suggested B12 injections.
I have also been reading about the drug Rituximab and its ability to help those with chronic fatigue and auto immune disorders (I have two – CD and secondary hypothyroidism). What are your thoughts?
Thanks again for a great article.
Congratulations on getting better and thanks for passing your experience on. 🙂