



 FACT 5 – Autoimmune Disorders Occur Ten Times More Commonly in People with Celiac Disease (CD) Than in the Normal Population.
FACT 5 – Autoimmune Disorders Occur Ten Times More Commonly in People with Celiac Disease (CD) Than in the Normal Population.
“Autoimmune diseases are the third leading cause of morbidity and mortality in the industrialized world, surpassed only by cancer and heart disease.”Annals of the rheumatic diseases Sept 2007
Autoimmune disorders are believed to affect approximately 8 percent of the US population or 24 million people. That’s more people than are affected by heart disease (22 million) or cancer of all forms (9 million). This suggests autoimmune disorders may be the number one cause of death in the U.S.
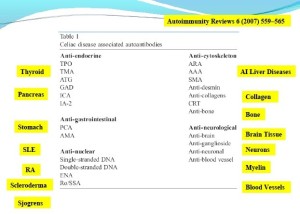
Autoimmune disorders occur 10 times more commonly in CD than in the general population“with type 1 diabetes and autoimmune thyroiditis leading the list. The presence of celiac disease in type I diabetes, for instance, is approximately twenty-times higher than in the general population. The autoimmune antibodies associated with CD include anti-endocrine, anti-gastrointestinal, anti-nuclear, anti-cytoskeleton and anti-neurological antibodies.
CD is believed to trigger autoimmunity through a variety of mechanisms including HLA and non-HLA genes, mimicry, altered intestinal permeability, epitope spreading and others. One study suggested long duration exposure to gluten products is associated with higher rates of autoimmunity in celiacs.
The longer celiacs are exposed to gluten the greater the risk they have of developing an autoimmune disorder.
“Our data show for the first time that the prevalence of autoimmune disorders in Celiac disease is related to the duration of exposure to gluten Gastroenterology August 1999
|
The age the patient was Diagnosed with CD |
The presence of other autoimmune condition in addition to CD |
|
2 |
5% |
|
2-4 |
11% |
|
4-12 |
17% |
|
12-20 |
27% |
|
>20 |
34% |
Unfortunately most celiacs spend 5-10 years going from doctor to doctor before a correct diagnosis is made.
Immune, Liver and Cardiovascular Affects
CD is linked with many other diseases including liver and heart diseases, osteoporosis, myopathies, schizophrenia, small- fibre neuropathy and more: Celiac disease was associated with an 8-fold increased risk of death from liver cirrhosis. One study found osteoporosis in 50% of celiac patients. In fact, the rate of celiac disease in osteoporosis is high enough that some recommend all osteoporosis patients undergo CD screening.
CD triggered inflammation appears may be to cause or contribute to myopathy, a muscle disorder characterized by muscle weakness. A large epidemiological study involving almost 80,000 individuals suggested that every type of cardiovascular disease (heart attack, heart failure, stroke, etc.) is increased in patients with untreated celiac disease.
The Nervous System
IgG antibodies were present in 34% and biopsy demonstrated villi destruction (celiac disease) in 9% of people with idiopathic peripheral neuropathy including small-fiber neuropathy. (Another study, however, concluded the two were not linked, but a large Swedish study involving 14,000 people with celiac disease and 70,000 healthy controls found increased risk of peripheral neuropathy (but not increased risks of neurological disorders such as Parkinson’s, Alzheimer’s, multiple sclerosis, Huntington’s disease, myasthenia gravis.)
The study authors suggested people with peripheral neuropathy get tested for CD. Recent studies suggest a form of peripheral neuropathy called small fiber neuropathy is common in fibromyalgia.
Gluten sensitivity was present in a third of patients with sensory ganglionopathy (SG), a disorder characterized by damage to the cranial and spinal ganglia, usually by autoimmune processes. Autopsy’s of the three gluten sensitive, SG patients indicated damage to the dorsal ganglia.
Large Swedish Studies Highlight Risk
Sweden’s large medical databases have helped to elucidate the remarkable impact celiac disease can have on the body.
Adult celiac disease was associated with increased risk of pancreatitis. A large Swedish study found celiac disease to be associated with increased risk of a raft of liver diseases including hepatitis, liver failure, primary biliary cirrhosis, liver cirrhosis and fibrosis and fatty liver.
Immune dysfunction and inflammation is believed behind the increased rates of sarcoidosis in people with celiac and kidney disease. Even fractures got in the act with the Swedes finding increased risk of hip and other fractures in people with CD. Increased risks were also found in diabetes (relatively low risk), thyroid disease and adrenal disease (greatly increased).
Not surprisingly, given the impact Celiac disease can have on the body rates of depression are increased after celiac disease (but not before it).

…When the finely tuned trafficking of macromolecules is dysregulated in genetically susceptible individuals, both intestinal and extraintestinal autoimmune disorders can occur… Nature clinical practice. Gastroenterology & hepatology Sept 2005
Although research has yet to confirm the link between autoimmunity and non-celiac gluten sensitivity (NCGS), the largest study ever completed on gluten sensitivity suggests mortality rates are higher for people with NCGS than Coeliac disease (CD). That suggests it’s probably just a matter of time before similar correlations regarding autoimmunity are made.
Indeed, the study found that people with gut inflammation (which is characteristic of NCGS) are also highly likely to suffer from “leaky gut” – which is strongly associated with the onset of autoimmune disorders – and appears to be common in ME/CFS/FM.
The GI track regulates the flow of macromolecules between the gut and the rest of the body. Some researchers believe the introduction of harmful macromolecules into the blood stream commonly triggers autoimmune processes, both inside and outside of the gut.
It is also important to understand that even if your gut exhibits no villous atrophy (celiac disease), and no intraepithelial lymphocytosis (inflammation), gluten sensitivity (positive IgA and IgG blood tests to gluten), may still be triggering an autoimmune process that’s attacking other organs in your body.
“Antigenic mimcry” is one way CD is believed to cause autoimmunity outside the gut. As the body becomes sensitized to gluten, it can mistakenly attack molecules similar to gluten, such as those associated with the thyroid gland.
The common immunogenetic theories ….are sharing common HLA and non-HLA genes, antigenic mimicry, damage-induced neoantigen exposure, altered intestinal permeability, idiotype network dysregulation and epitope spreading” Autoimmunity Reviews Sept 2007
The below autoantibodies have been associated with CD; notice that most involve the gut.
According to the latest textbook: Advancing Medicine with Food and Nutrients 2nd Edition, correlations between the illnesses below and NCGS have been confirmed:
- Epilepsy
- Myalgia/Miotosis
- Cereballar Ataxis
- Peripheral Neuropathy
- Brain atrophy
- Irritable bowel syndrome
 FACT 6 – If You Are Sensitive to Gluten – Going on a Gluten Free Diet is Probably Not Enough
FACT 6 – If You Are Sensitive to Gluten – Going on a Gluten Free Diet is Probably Not Enough
Where CD/NCGS has affected the gut, taking gluten out of the diet may NOT be enough for clinical improvement. The fire of inflammation in the gut must be put out, and intestinal permeability MUST be healed to restore absorption. Taking gluten out stops feeding the fire, but the inflammatory cascade has a life of its own, and unless there is a specific healing intervention gut permeability may continue.
Less than half of patients with coeliac disease on a gluten-free diet have complete normalization of intestinal biopsies, intestinal permeability defects, and antibody levels (after a mean of 9.7 years on a GFD) Digestive diseases and sciencesApril 2010
It is important to understand that children with CD had a 3 fold increase of long-term mortality – whether they were on a gluten-free diet or not.
This suggests taking gluten out of the diet is not enough. Although the villi of CD patients does grow back after 1 year on a gluten-free diet, the evidence suggests that increased intestinal permeability and poor absorption – both linked with autoimmunity – is still present. So the gut must be healed and any inflammatory cascade dealt with even after gluten is removed.
The difficulty of adhering to a gluten-free diet can make prognosis difficult. Strict adherence to a GFD does greatly improve nutritional status but one study found it did not completely normalize ‘body composition’. Metabolizing B-vitamins, in particular, may still be reduced even after a gluten-free diet. Hallert et al. found that celiac patients on long-term gluten-free diets with normal gut villi, had reduced plasma B-vitamin (homocysteine) levels. Forty-five percent of celiac disease patients on a gluten free diet for decades had reduced bone mineral density (osteoporosis).
Increased rates of peripheral neuropathy even in ‘well treated coeliac disease’ indicate that neurological problems can manifest themselves even when ‘overt malabsorption’ is not present. While substantial improvement in gut mucosa and other factors did occur 2-4 years after beginning a gluten-free diet, lactase activity was still reduced. One study suggested ‘leaky gut’ was still common a year after beginning a gluten-free diet.
Finally, quality of life measures that improve after initiating a gluten-free diet but are still somewhat reduced relative to the general population also suggest that simply removing gluten, while beneficial, is often not sufficient to return one to full health.
 FACT 7 – The Cross-sensitization Factor: Taking Gluten Out of the Diet May Not Be Enough if You’ve Become Sensitized to Other Foods As Well
FACT 7 – The Cross-sensitization Factor: Taking Gluten Out of the Diet May Not Be Enough if You’ve Become Sensitized to Other Foods As Well
Even minute traces of gliadin or their cross-reactive foods are capable of triggering a state of heightened immunological activity in gluten sensitive people Journal of neurology, neurosurgery, and psychiatry.Dec 1997
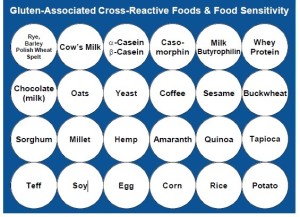
Cross-sensitization refers to a process whereby a person becomes sensitized to new substances. For instance, people sensitive to the gluten proteins called gliadins found in cereals in the Triticum genus (wheat, rye and barley) can become sensitized to other types of foods.
Foods known to cross react with purified gliadins (wheat proteins) make up the first line (rye, barley, spelt, cow’s milk, whey protein plus milk chocolate and coffee) of the chart above. The other foods on the chart (most grains, soy, egg, potato, yeast, coffee, sesame, buckwheat) are foods people often turn to on gluten-free diets but which they may have become sensitive to. Some foods such as oats are prepared in facilities where gluten contamination is common. Even small traces of gliadin can trigger an immune response in very gluten sensitive people.
 FACT 8 – The Current CD Test Does Not Test for Gluten Proteins People Can React to or Cross-Sensitized Foods.
FACT 8 – The Current CD Test Does Not Test for Gluten Proteins People Can React to or Cross-Sensitized Foods.
Also there are at least 24 celiac-associated auto-antibodies that could be tested for, not just gut related autoantibodies
The Standard coeliac test is made up of three elements:
Two antibodies to parts of the BODY i.e.; AUTOIMMUNITY in the gut:
- To the endomysium – the sheath which encloses the villi
- To transglutaminase – an enzyme inside the endomysium
Plus antibodies to gluten.
- Antibodies to the gluten protein gliadin. Recently this has changed to deamidated gluten which has been found to be more accurate to diagnose CD, but not NCGS.
Problems With The Current Testing Protcols
( Antibodies to endomysium and transglutaminase are EXECELLENT markers for TOTAL VILLUS ATROPHY (ie celiac disease) but are highly unreliable diagnostic markers for the partial villous atrophy or increased epithelial lymphocytes found in non-celiac gluten sensitivity (NCGS). Only between 30% and 24% of patients with partial villous atrophy (NCGS) and coeliac disease were diagnosed correctly using antibody tests in two studies.
The antibody test to the gluten protein ONLY checks for one TYPE of gluten (called the 33-mer peptide.) If all you do is check the gluten 33-mer (the standard test) you’ll miss gluten sensitivity 50% of the time. Studies consistently show that most people with CD react to a range of gluten peptides, some as strongly as the gluten-33 mer that is typically tested for.
Note that gluten is found in ALL grains, however a subset of gluten proteins particularly toxic to some humans are found in wheat, rye and so on. An assay that includes IgA and IgG antibodies for a range of gluten peptides ( see www.CyrexLabs.com), therefore, is desirable;
Our present results indicate that CD patients are capable of responding to a large array of gluten peptides. We found that 50% of these patients do not respond to the alpha-GLIA peptide but to a diverse set of gliadin and glutenin peptides, including 6 novel epitopes.”
Gastroenterology June 2002
Niki to find referenced paper link for the above.
Prevalence
If we take into account that gluten sensitivity doesn’t just cause CD, but also partial villous atrophy and gut inflammation, AND probably triggers many disorders outside the gut including autoimmune disorders, AND the fact that people react to a range of gluten molecules, not just the one in the standard CD , it begs the question how much of the population is sensitive to some form of gluten?
Dr. O’Bryan believes between 10 and 35% of the population.
“Gluten Sensitivity (GS) is a state of heightened immunological responsiveness to ingested gluten in genetically susceptible people. It represents a spectrum of diverse manifestations, of which, the gluten sensitive enteropathy known as CD is one of many. Adverse reactions to the toxic family of gluten proteins found in wheat, barley, rye, and their derivatives may trigger a heterogeneous set of conditions, including wheat allergy (IgE), NCGS, and CD, that, combined, affect between 10 – 35% of the population.”
Celiac Disease and Non-Celiac Gluten Sensitivity: the Evolving Spectrum
- Read Part 1 of this article covering a epidemic of misdiagnosis, comorbidity and mortality.
- Read Part 3 which focuses on the direct link between CFS and Gluten Sensitivity and next steps
Resources
- Dr. O’ Bryan’s 1 day Doctors training on Gluten on DVD for US Practitioner
- Dr O’Bryan’s 1 Day Training on Gluten for Practitioners in the UK
- Dr O’Bryan’s DVD on Gluten for patients in the US
- Dr. O’Bryan’s 1 day seminar on Autoimmunity
Keep Health Rising….RISING










Argh, that’s a bummer that quinoa and buckwheat might also be off the menu if gluten is a problem. Some months ago I cut out wheat and within a day, was able for the first time in years to lie on my side and breath through my nose at night instead of my sinusitis rapidly clogging it up. So I stayed off wheat and switched to quinoa and buckwheat. That was a while back – but in the last few weeks, that night-time problem is back. I had thought it was maybe hay fever but argh…
Still, better to know than not know. I’m running out of ideas for what else to have for starch, though. I’m already on sweet potatoes for two of my meals as the starch portion. I had thought quinoa and buckwheat were OK because they’re seeds rather than grains (though I’m not sure of the difference, since surely grains are seeds?).
Maybe Niki can join in here. In the next post she’ll talk about how to repair the damage; hopefully so that the sensitization really dies down.
Are you rotating those foods? I eat sweet potatoes and potatoes quite a bit and, honestly, for me, I think I should really cut down starch….but I think that’s another issue.
Hi Sasha
The only foods it may be prudent to avoid in addition to gluten are the confirmed ones that tend to cross-sensitize, which is all dairy, coffee and milk chocolate. Most oats are contaminated with gluten (in the delivery trucks).
Generally there’s no need to avoid the other foods like buckwheat and quinoa without at least first testing them, which you can do with the Cyrex Labs testing array for cross-sensitivity.
Personally I wouldn’t eat all genetically modified versions of foods either (which are mainly soy and corn). I’d eat them GMO-free…More will be written about that in part III of the article series.
According to Aristo Vojdani coffee per se is not a cross reactor. It has been instant coffee that has been shown to be cross reactive and not fresh coffee. It is postulated that this is more likely to be caused by contamination in the manufacturing process. “Instant coffee is reactive at 20% to anti-gliadin antibodies, a significant finding that often reflects the presence of wheat fractions in the factory. Yet when we tested espresso from five different well-known coffee houses, we found no reactivity due to anti-gliadin antibodies. We also found no reactivity in tests on coffee beans purchased from Israel, Turkey, Greece, Colombia, and Brazil. Therefore, coffee beans do not appear to be cross-reacting with wheat, but some instant coffees are apparently cross-reactive due to contamination. These results indicate that drinking pure coffee, but not instant coffee, is safe for individuals with gluten sensitivity and celiac disease as long as these individuals do not have a classic allergy to coffee.” (Vojdani A, 2013, Enhanced Testing for Gluten and Food Sensitivity Townsend Newsletter January 2013)
Thanks Nikki – I’m already avoiding that other stuff 🙁
I’m in the UK and don’t have access to Cyrex Labs. How well-established/sensitive/specific are the tests? Would a conventional doctor recognise them?
I’m stopping buckwheat and quinoa for a few days to see if it affects my sinusitis. I really hope it doesn’t – I’d really miss them!
Hi Sasha – good news, Regenerus Labs are due to become the Cyrex Labs agent in the UK in December this year – http://www.RegenerusLabs.com.
Bearing in mind a large part of this article was called “The 10 Facts your Doctors are Unlikely to Know About Gluten” – most conventional doctors are not up to date with the research. This is despite the fact the main aim of this article was to summarize the key facts from 19,000 papers already published in the main stream medical literature – it’s a case of patients being more up to date than the doctors if you read this material I’m afraid.
It’s better to base knowledge on what the expert researchers in the specialism are saying than your local GP. Cyrex is state of the art testing, i understand the lab is currently double checking all tests at the moment, the testing will be more sensitive and specific for Non Celiac Gluten Sensitivity than anywhere else on the market at the moment…
Hi Cort – no, I’m not rotating them. I’m having quinoa instead of toast, basically (which I used to eat for breakfast and last thing) and buckwheat instead of toast (which I used to snack on when I was hungry).
Ah, toast…
Autoimmune Disorders Occur Ten Times More Commonly in People with Celiac Disease (CD) Than in the Normal Population does not mean that more people than may be expected with ‘autoimmune’ (jury is still out on that one) disorders like fibro/CFS/ME have all of these gut/food sensitivities. Anyway, there’s a world of difference between correlation and causality.
I’m starting to get exasperated by some of the posts on this site, I signed up in the hope of getting some serious, up to date info about state of the art research taking place in the fibro/CFS/ME research community and keep finding slightly dodgy science/leaps of faith and it’s all in your guts stuff. I’m not convinced that there is much in common with the (horrible if you have them) gut diseases and fibro/CFS/ME, much as some would have us believe (especially private healthcare/health food/1 day training course providers). I’d be happy to be proved wrong, but there is currently no tangible proof that there is much of a correlation, even. More than this, I just don’t find the above to be a very well written piece.
It may well be that for a tiny minority, there is an association between gut and autoimmune diseases, but I am starting to get cheesed of with all this baloney about those of us who have illnesses that leave us cream crackered. I am living working in Africa where most people are grateful to eat food, of any kind, most of which is heavily starch based, because people need the calories and to keep ‘belly full’. That’s how it is for most people in the world. People eat the starchy foods to stay alive, and to be honest most people absolutely thrive on them. People in the West are spoiled silly about food. Enjoy the ride, because in 10-20 years we’ll be thankful to get what we can.
And now I am deprived of it, If only I could get decent, bread, yes, wheat, lovely wheat, I’d be so happy. I don’t eat chocolate despite working in the second biggest cocoa producing country in the world and it’s got nothing to do with what it may or may not do to my health, and everything to do with the health and impoverished conditions of the people who labour to produce the raw materials that go into making it. But right now I’d kill for a decent cup of coffee, much as it probably isn’t that good for me, but I haven’t had one for months.
There is a tiny minority in the general population that have gluten sensitivities. Celiac disease and the like is a bummer for the small number of people that have it, but most of us fibro/CFS/ME sufferers don’t, thankfully. Can we have some more of the cutting edge research on fibro/CFS/ME, please, a
and less of the Dr O’Bryan’s 1 day training courses/DVD sales pitches, or I shall be voting with my unsubscribe button.
Tell me what you really think :).
We’ll see how it all turns out Italass. After my recent success with a dietary change I’m more and more interested in diet. I do think the problems with celiac and gluten sensitivity are pretty well substantiated in the literature, and it’s an area that I, as a person with ME/CFS, haven’t had much exposure to. Whether that’s because its not present much in the ME/CFS/FM communities or because it’s been missed by doctors and patients, only time will tell. I was eager, therefore, to hear what Niki had to say.
I do recognize that many people have gone the diet route without much success but that its been varying degrees of helpful for others. I wonder if that’s kind of par for the course for these rather heterogeneous illnesses – that most treatments work for a minority of patients.
We’re focusing on diet at the moment; if you stick around I think you’ll find more of the blogs that attracted to this site in the first place.
There is an indepth discussion in the final part 3 of this series of articles about the connection between CFS and celiac disease, the percentage that might have it and the fact it is important enough researchers have stated it should be part of the differential diagnosis for CFS, so many of the direct connections with CFS will be covered shortly.
In reading the above with interest re diet–Celiac disease (CD) and NCGS (non-celiac gluten sensitivity) — I have information to share that I hope will be helpful to others.
In 2005 I was diagnosed by a Gastroenterologist doc as NCGS–and have been on a strict gluten-free diet ever since–8 years now; I have small amounts of dairy only occasionally—NEVER gluten–really takes the body down, etc., etc.! My adult daughter also has NCGS and must adhere to a strict gluten-free diet as well.
In 2007 I became verrrry ill after a surgery–just wasn’t recovering from a successful surgery; in the fall of 2008 I was diagnosed by my Internist doctor with ME/CFS. (AND, at that point, I had already been eating gluten-free for three years.)
I am pretty much ‘house-bound’ and as such unable to work. Usually I get out of the house once a week and that is a PUSH–as is everything with any kind of activity with ME/CFS. Obviously, eating gluten-free is NOT the cure for ME/CFS–however, it is necessary if one has CD or NCGS–and could impact on ME/CFS.
Peripheral nueropathy is mentioned above–I was diagnosed with a mild peripheral neuropathy in 2008 (symptoms occurring for years before)—in my latest nerve conduction test–June 2013–it showed improvement in the peripheral neuropathy AND I can also feel some improvement with the neuropathy. The Neurologist doc felt that the improvement in the neuropathy could be due to the gluten-free diet!
MORE—my father also had peripheral neuropathy AND cerebellar Ataxia—and the specialists say that it is quite possible that he also had undiagnosed ME/CFS. My father did NOT eat gluten-free and that became suspect (gluten) with the neuropathy and the ataxia. By the way–I started having balance problems, felt like I was walking like a spastic and was occasionally walking into walls (ataxia)—and once eating gluten-free that stopped!!
There is more to add to the picture as to how ME/CFS came along — intestinal parasite in 2003–lead to IBS–(going gluten-free helped with IBS–still have some issues with this because of ME/CFS). Parathyroid disease and surgery to remove tumour in one of the four PARATHYROID glands in 2004 — this is an autoimmune disease in the ‘endocrine system’–parathyroid glands are located behind the thyroid. Thyroid is mentioned above; there is usually not mention of ‘parathyroid’ — most of us have never heard of it.
Interesting with all the connections above–I hafta tell you–altho necessary/mandatory for some of us–eating gluten-free is NOT the answer to curing ME/CFS.
Hey, nobody ever said this disorder was anything but complex. Staying away from gluten helps you feel better but you have a long way to go. It sounds like you have intestinal and other issues above and beyond the gluten plus autoimmune stuff.
Thanks for relating your experience..:).
Hi, thanks, Cort and also to Niki. The reason I mentioned the intestinal and autoimmune–and neurological conditions–is because these were all mentioned in the info regarding ‘gluten’. Soooo, proof in the pudding, so to speak on that! I did experience these health problems BECAUSE of gluten.
CD and NCGS are separate medical conditions apart from ME/CFS–BUT can be comorbid–i.e., occurring @ the same time.
Having experienced gluten-sensitivity (NCGS)–and feeling awful with that—and then being well and feeling good after going completely gluten-free — AND then a few years later contracting ME/CFS—I can tell you that eating gluten made me feel very unwell—BUT–ME/CFS — no comparison—far worse and life-restricting/debilitating !!
IT sucks and sure would be nice to find the answers and get our collective lives back.
By the way—as a person with diagnosed ME/CFS, I agreed to be a research participant in a medical study investigating ‘Complex Chronic Diseases’ (Canada)—have had the testing—it will be a while before the results are out. You are right–ME/CFS is a complex chronic disease–another reason why I mentioned the other medical conditions—body ‘down’—easy for the nasty ‘whatever’ to walk in and/or resurface–and let ME/CFS ‘attack’—darn thing is—it does NOT go away–nor do we ever wake up feeling refreshed and ready ‘to go’ for the day.
The only good thing about getting ME/CFS in ‘this day’ is that there is now so much attention given–after the XMRV ‘stuff’–they KNOW it is a ‘biological’ disease–that there is much research going on world-wide. It is so important to get answers–not only for the collective ‘us’—BUT for our offspring–as there is deemed to be a genetic component–and this seems to be the case in our family. The medical people want answers because more and more people are being diagnosed with this horrid ridiculous disease!
Never give up–who knows what might be around the next corner 🙂
Hi Ess – yes seconding Cort’s comment there about thanking you for sharing your experience.
I have to agree that what we’re finding is that a percentage of CFS/ME patients will need to go gluten-free, but it is not enough – it is an absolute necessary for that group – but it’s not always going to be enough on its own for complete recovery. If people with confirmed CD still develop osteoporosis and show nutrient deficiencies and leaky gut even after 20 years on a gluten-free diet – it confirms more intervention is required, just being gluten-free alone wont fix it all.
Healing any leaky gut and identifying any other sources of gut inflammation (parasites, use of antibiotics etc) is going to be top priority – and something I will be covering in a new set of articles.
But I also think for some there may have been a level of damage done to the immune system, fats, proteins and mitochondria already which may need regenerative medicine approaches for some (e.g. stem cell), and of course there are a whole range of chemicals in the environment which have the same autoimmune impact as gluten (to be covered in an even later article), electromagnetic stress may be a new factor and psychological and social and cultural aspects – so I agree again with Cort. This aint simple!
To get a positive note in here (!) someone with a success story just commented on the last gluten piece
http://www.cortjohnson.org/blog/2013/08/29/celiac-disease-gluten-sensitivity-and-chronic-fatigue-syndrome-pt-1-misdiagnosis-and-mortalit/
“I suffer from CFS. It started long ago when I was 12 yrs old after I got mono. The fatigue just never left. I am now 34 & the fatigue is much, much worse. Over the last 8 yrs a lot of random symptoms have gotten much worse & through my extensive healing, a few have gotten better. In regards to this article, completely cutting gluten out wiped COMPLETELY wiped out all of my joint pain!
I highly suggest for anyone who suffers from any health issues to do an elimination diet & slowly reintroduce foods to see if you notice a difference w/ any of your symptoms. Or you have the opition to get a blood test done to test your IgG antibodies to certain foods.
I started eating gluten again thinking I needed some in “my system” to get an accurate test. The way I felt the next day was enough confirmation!
The test was $560… A lot of money when I had the answer I needed on my own.”
I realize this may not be completely on subject- but I am on a Gluten free diet. I am Gluten Sensitive not Celiac. It has helped but I find anything fried also
upsets the applecart.
One point I want to make is- I do Animal Rescue. We get dogs that are very abused and sick. I have found that a Grain free diet (Pricey) gets all of them back to normal quicker than a reg dog food with wheat or corn. Actually have had ear infections cleared up with just a diet change. Vets are way ahead of the Md’s in a lot of nutrition focus. This may not seem important to you who eat what you want. However, Even a bowl of oatmeal can set me off for a week. Gluten causes us to have more Mucous!!!!!!!
San Diego #1
I enjoyed reading italass’s comments and have similar views. Gluten sensitivity seems to be the new one-size-fits-all “explanation”. We have been through this before with Lyme, B-vitamin deficiencies, toxic poisonings, dental poisoning, etc, There are indeed some who have these issues and who benefit from the recommended protocols, but others of us, who have labored for years trying to revamp our diets and lives with each new fad diagnosis, find that we still have ME/CFS. I avoid all these diagnostic crazes now, especially the ones for which there always seem to be “no accurate tests”, or the only ones which are accurate are obscure and expensive and you could never talk your local doctor into ordering them. A diagnosis you can’t be sure you have but which explains supposedly every symptom, with expensive or arcane treatments that run to extremes such as throwing out all your food, or moving out of your house, etc., now seem suspect to me, just on the basis of the pitch. Structurally they do now seem to me like a leap into quackery and the placebo effect for the sake of maintaining hope. Yes, some have these particular ailments, and hope is important for everyone, but these one-size-fits-all diagnoses and cures can make people a lot more hopeless when they don’t pan out. They function like temporary highs, “A diagnosis! A treatment!!, however expensive they are in terms of time, money, energy, effort and sacrifice– in fact, the more extreme and arcane the better, it seems, for attracting new adherents–but the hangover or crash later on when they fail is never mentioned.
I would never dream that anything would be a ‘one-size fits all solution’ for this disorder. Our history – with one person doing well on something which has not affect on somebody else – suggests that’s just not possible.
I think the unfortunate truth is that if you have ME/CFS you have to spend the time and money (if you have it) to go through alot of different trials and hope that something works out – knowing very well that nothing may (!).
The goal here is not to find the one-size fits all solution but to provide a broad range of treatment possibilities that fit for some people. Nothing is going to work for everyone but for those who get benefits the search is probably worth it.
I wish it was less frustrating and easier (and less expensive) 🙂
Ditto!!!
You put it into perspective very well, Cort. Some people out in the world, however, come on very strong these days for a gluten-free diet, and I have developed an allergic reaction to this pitch. What would help me the most, probably, is a whole lot of fasting, but I don’t want to do this either, for obvious reasons. Yet fasting seems to help my body put itself into better order–
Through Google Translator :
In the end the solution will be eating nothing directly. I think that instead of thinking in countless foods that harm us and cause the diseases or modulate them, the more I am inclined to think is that the disease itself, with all viruses , parasites , bacteria and inmune issues causes the food problems.
I’m not saying that diet is not important or have influence on the CFS and others but It dont have the relevance that arises I mean.
It is impossible for a sick person to do all these tests and have some kind of guarantee to start a complex and strict diet .
I was diagnosed with CD based only on Marsh 1, but after testing deeper, diagnosis was discarded ( The marsh 1 never appeared in subsequent biopsies). But if I am guided by the article, I can’t be sure of anything!
I did a GFD for 6 months and did not notice much. Genetic testing and antibody negatives too .
Finally thank you , Cort, for the web. I learn a lot .
A big hug from Spain
In contrast to a few other comments I just wanted to say how much I appreciate the focus on the digestive system. I have been following Ken’s recommendations and they definitely been helpful. I have been gluten-free for three years and that step greatly reduced my bloating and GERD within a week. Almost everyone I know with ME/CFS has some digestive problems, whether IBS/GERD/IBD or gut pain so I don’t think focusing on the gut is a distraction. There is a ton of evidence that there is a large change in intestinal permeability and gut bacteria in most auto-immune diseases, CFS, and autism and reason to believe that are contributing to some (and potentially all) symptoms in this seemingly diverse set of illnesses. I know most of our experts think our gut problems are downstream, but I suspect they hint toward the root of the disease.
Going gluten and dairy-free hasn’t healed anyone I know, but almost always reduces symptoms. When I am careful about diet my POTS is greatly lessened and I feel much less light-headed. Unfortunately healing the gut is not easy since there are still a lot of unknowns, but it’s worth aiming for.
Thanks Cort for this series – I appreciate the information on digestive issues! It finally occurred to me that years (decades) of stress, probably including that heavy exercise done prior to the onset of CFS/ME, had logically left my gut dysfunctional. With a recent worsening of IBS symptoms, my primary care provider (a PA) recommended a specific digestive aid. In this first month of use my digestive functioning has improved to the most “normal” it’s been in years. I still have CFS symptoms of course and don’t expect a cure with this approach. I find that improving any symptoms helps the whole to some degree.
Fifteen years ago I used the elimination diet for gluten and had that “aha” experience of realizing my joint pain was gone. Budget and convenience made sticking with gluten-free eating difficult and I resumed my old eating habits. Ten years ago I got testing confirmation of gluten sensitivity and went gluten free for several years. The same derailment of budget and convenience happened again.
This series has reminded me of the potential benefits of an improved diet and has motivated me to transition back to gluten (and dairy) free eating. I’ve learned in the 20+ years of CFS/ME symptoms to fix what I can and enjoy the benefits that come. (I use the same approach with chiropractic care: it doesn’t “cure” CFS/ME but fixes what’s fixable!) Thanks again Cort and Niki!
P.S.: Niki, can you include a glossary and/or phrases to accompany acronyms in upcoming articles? If so I’d be grateful as either would allow me to absorb the information easier 🙂
Thanks Jan for sharing your experience. Glad to hear you got some help out of altering your diet.
I have had GI issues since I was 10 years old. I have had ME for 10 years and tested positive to multiple viruses in my RNA. My GI issues seem to be climbing a severity ladder as the number of co-morbidities that I have increase. I have had phone consults with Dr. Chia and he has tested GI biopsies I have had done and found sevral strands of echoviruses in them. A year ago I took myself off of gluten and “dabbled” in that realm. The longer I went without gluten the less my gi symptoms were. Now I rarely eat anything out because it hurts so bad when I am accidentally exposed to gluten. My next step is going to a Celiac Specialist. We have a center in Chicago that runs all the right tests but my appt is not til December. I have no doubt in my mind that some subsets of us have co-related gi issues. Dr. Montoya has said that they have seen some ME patients cured from a gluten free diet. This really is important info that many are not aware of, IMHO. Thanks Cort.
Thank you very much for this series on gluten sensitivity. I am very much looking forward to the next article.
I was curious if Niki is also a proponent for those with autoimmune issues to cut out nightshades, seeds and nuts from the diet too? Will this be addressed in the next article?
Thank you again.
Hi Renee
Thanks for you question – which is actually slightly complicated! Even with people with autoimmune diseases I wouldn’t automatically just eliminate gluten, I’d test for CD and NCGS, leaky gut and gut inflammation, then asses if gluten should be avoided long-term based on test results and the results from clinical intervention to heal the gut lining and so on.
Now an issue is, if you have gut inflammation and leaky gut – this could have been caused by using antibiotics, a genuine gluten sensitivity, or a parasite for example, the result can be increased sensitivity to many foods because of undigested particles getting through a leaky gut lining. If you have gut inflammation, you may also be more vulnerable to foods high in lectins (which are high in the nightshade family for example).
So it’s tricky, you want your gut to be 100% healed, any genuine food, drug or bug which is going to cause permanent long term gut inflammation would need cut out. Then you might be fine on nuts/seeds/the nightshade family!
Everyone is so different and for some, they may well have a genetic propensity to permanently react to the nightshade or some nuts and seeds the same as gluten, if that were the case you’d just keep having chronic leaky gut and inflammation until you removed these foods while on a gut healing program!
I’m going into gut healing in much more depth in the next series of articles after part III.
It’s also tricky with CFS because we don’t want to encourage fanaticism about food and increased stress and worry either! Eek:-)
I am one of the people who encourages everyone to try a gluten free diet. It has not cured my fatigue problems but it did give me a normal life for quite a few years before excessive exercise provoked a relapse. I am now recovering again. A coeliac blood test is not expensive, a gluten free diet is difficult at first but becomes easier in time (except when travelling).
I’m only too aware that it isn’t the whole answer. My suspicion is that it reduces inflammation and/or improves the immune system. A months trial should tell you if it helps – not much for a possible massive improvement in health, even if it doesn’t last forever. For me brain fog was the first thing to go, then I became able to do more physically.
As for the person who had problems with mucus – can I recommend N-acetyl-cysteine and that you consider putting a block of wood under the head of your bed to raise the head about 6 inches. You may want to start with 4 and then increase as it feels peculiar at first. Night-time reflux (often missed by doctors) provokes sinus problems for me, NAC thins mucus. One or both may help.
Personally I suspect the gut is at the root of my problems and I’m trying different probiotics. So far the best I’ve found is actually a prebiotic (see below) but some of the research found through ME sites means I’ll try others.
http://www.boots.com/webapp/wcs/stores/servlet/ProductDisplay?storeId=10052&catalogId=11051&productId=1127366&langId=-1&callingViewName&cm_mmc=Paid%20Search-_-Plusbox-_-Link-_-BimunoIBAIDPastilles30g&cm_mmc=pla-_-google-_-Boots+Beauty-_-Beauty+-+PLAs+Brands
For those unable to face GF these are what I use when travelling http://www.amazon.com/Houston-Nutraceuticals-Enzymes-AFP-Peptizyde-Vegetable/dp/B001NXM5I8 In the UK you can get them here http://www.mandimart.co.uk/afp-peptizyde-original-90-capsules-112-p.asp
Hi. I was diagnosed with M.E. 6 years ago and have become bedbound these last 3 years. I took a leap back into the medical arena for answers and thanks to prof Mathias in London was diagnosed with PoTs and sucessfully treated. A year on an mri scan with pituitary contrast revealed that I had lost more than %75 of this crucial gland and explained my almost non existant hormonal output which was also causing secondary Addisons Disease. So i’m hoping that the hydrochortisone will show some improvement in the long term. It was then discovered that I was running high levels of histamine and after further testing by a dr Senerviratne was found to be allergic to gluten and dairy etc. So I am on a very strict diet eliminating all foods high in histamine, those that cause cells to release stored histamine and gluten free, dairy free. Sounds hard but I really only had to tweak what I was already doing. This area is really about mast cell activation disorder and is maybe slightly more comprehensive? Have you Niki/John come accross this? I am only just starting treatment so it’ll be quite sometime before i’ll see any improvement.