



Highlights
- The assays Dr. Lipkin used in the CFI ME/CFS pathogen study would not detect the kind of ‘persistent, subacute’ infections some researchers and doctors believe are present in chronic fatigue syndrome
-
Fine needle biopsies of the thyroid gland in ME/CFS could uncover evidence of herpesvirus/enterovirus infections
- The co-discoverer of HHV-6, Dr. Daram Ablashi, believes from 15-25% of people with ME/CFS may have an difficult to detect, low-grade HHV-6 infection
- Kristin Loomis called Michael VanElzakker’s Vagus Nerve Infection hypothesis a ‘masterpiece’.
- Rates of chromosomally integrated HHV-6 (ciHHV-6) may be increased in ME/CFS and ciHHV-6 reactivation could account for some cases of ME/CFS
Background
How did you come to found the HHV-6 Foundation?

Kristin Loomis began the HHV-6 Foundation after a disabled family member responded well to antivirals
A family member who was completely disabled, responded dramatically to IV antiviral therapy (foscarnet) after HHV-6 DNA was detected at low levels in her spinal fluid. Her symptoms were identical to many with ME/CFS: cognitive dysfunction, depression, autonomic dysfunction, abnormal EEG and debilitating fatigue. Dr. Dan Peterson, who has always suspected HHV-6A in CFS, encouraged me to start a Foundation in 2004. I have been very fortunate to find very talented partners such as our scientific director Dharam Ablashi (co-discoverer of HHV6) and Mona Eliassen who has been chairman of our board for the past six years.
Lipkin/Hornig Chronic Fatigue Initiative Pathogen Study
When I talked to you last September you predicted that the CFI Lipkin-Hornig pathogen study would not find pathogens (other than chromosomally integrated HHV-6). I think many people expected a significant subset of herpesvirus-infected patients to show up, but you didn’t. Can you explain why you felt that way?
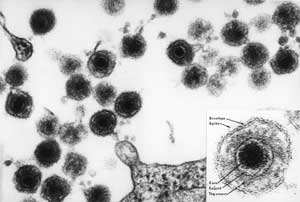
The type of initial screening assays Lipkin and colleagues used for their first pass works very well for high copy number viruses (such as annelovirus) or for acute infections that produce lots of viral DNA in the plasma. They don’t work as well for persistent, low-level infections of highly cell-associated viruses.
“…this testing confirmed what we already knew: there are no acute herpesvirus infections in ME/CFS”
The assays Dr. Lipkin ran may not have been strong enough to detect the kind of herpesvirus infections found in ME/CFS
Lipkin used a herpesvirus consensus PCR that has about the same level of sensitivity that you would find at a commercial laboratory, and those labs rarely if ever find viral DNA in the plasma of CFS/ME patients. So this testing confirmed what we already knew: there are no acute herpesvirus infections in ME/CFS, but it didn’t answer the question of whether there any of there are persistent low-grade infections of HHV-6 or any of the other “likely suspects”: c. pneumonia, m. pneumonia, enterovirus, EBV, HHV-6, CMV, HSV-1, HHV-7, parvovirus B19.
Absent a breakthrough in technology, we will probably have to wait for a biopsy study to answer the question of whether there are low-grade persistent infections of these pathogens in various subsets of CFS patients. What “likely suspects” have in common is that they don’t circulate in the plasma after the acute phase. Lipkin said he plans look for shadows of an infection (presumably antibodies). Hopefully he will use his considerable expertise to take a more in-depth look at the pathogens that have long been suspected as playing a role in ME/CFS.
Dr. Lipkin did find anellovirus in about 2/3rds of his samples, and a recent Stanford study indicated anellovirus populations explode in immune suppressed transplant patients. We recently saw an Australian study find more evidence of immune suppression in people with chronic fatigue syndrome. Lipkin said he didn’t know what to make of the findings, and that the annelovirus sequences he found were variable. Would you be willing to take a stab at what an anellovirus/ME/CFS connection might mean, if anything?
Unlike HHV-6 and EBV, anellovirus is relatively easy to find in the plasma because it is a “high copy number” virus. In one study healthy individuals had a mean viral load of 180,000 copies and HIV patients had a viral load of 3.7 million copies per ml. By contrast, you wouldn’t expect to find more than 40-75 copies of HHV-6 or EBV in the plasma of a CFS patient, using an ultra-sensitive assay and starting with a high volume of material, and that falls below the level of detection at almost every laboratory.
Anellovirus is found in a significant percentage of healthy controls as well. If Lipkin found a much higher viral load in ME/CFS patients this could be a very important finding because the Stanford study suggests that the anellovirus load is a good proxy for overall immune status.
There are so many clues pointing to immune defects. Kristin Loomis
If you believe that persistent pathogens play a role in ME/CFS then of course it makes sense that these patients have immune defects. Otherwise these pathogens would be under control. I was delighted to see that the NIH has funded a group in London to study NK cell function and the relationship to reactivated EBV, HHV6 and CMV in ME/CFS patients.
There are so many clues pointing to immune defects. For example, a new NIAID study just demonstrated that low RBC magnesium causes poor NK and T cell response against EBV, resulting in uncontrolled EBV infection, and more than one study has suggested that CFS patients have low RBC magnesium. HHV-6A reactivation in MS patients has been tied to two specific polymorphisms– IRF5 (which causes a reduction in interferon production) and MHC2TA (which affects MHC class II genes).
Dr. Lipkin announced at the CDC telephone conference that he found HHV-6 DNA in the plasma of 1% of controls and 1.4% of patients. Are these patients the ones with CIHHV6?
Yes, I assume so. This percentage is exactly what one would predict based on the prevalence of CIHHV-6 or 0.8% of controls (in the US and UK) and 1.9% of patients. CIHHV-6 patients are pretty hard to miss on any PCR DNA test because they are born with one copy of HHV-6 integrated into the chromosome of every nucleated cell, which is why we assumed he would find those – and nothing else. I expect he will explain this in a future publication once he has confirmed the integrated status.
Vagus Nerve Infection Hypothesis
It makes great sense that a low-grade viral infection of the sensory ganglia would have a dramatic impact on patient symptoms – and also be impossible to detect in the plasma. Kristin Loomis
Michael VanElzakker’s Vagus Nerve Infection Hypothesis (VNIH) for chronic fatigue syndrome proposes that a difficult-to-detect herpesvirus such as HHV6 (or other) infection of the sensory ganglia associated with the vagus nerve could trigger an ongoing case of ‘sickness behavior’; e.g. ME/CFS. VanElzakker’s theory could explain why antiviral treatments often need to be prolonged to work, why it’s so difficult to detect these viruses and why cytokine studies are so variable. Can you give us your take on the hypothesis?
VanElzakker’s hypothesis paper is a masterpiece — one of the best I’ve seen on the subject of ME/CFS in the past ten years. He did an amazing job of pulling together information from many different fields. It makes great sense that a low-grade viral infection of the sensory ganglia would have a dramatic impact on patient symptoms – and also be impossible to detect in the plasma. Van Elzakker also had a terrific suggestion to use radiolabeled antibodies to identify specific viruses in the glial cells and brain tissues. I hope that he and others are successful in pursuing this idea.
My only quibble is that I would have liked to see him expand the hypothesis beyond the vagus nerve. Latent HHV-6, VZV and HSV-1 are found in other cranial nerves as well as the brain stem and limbic system. In one German autopsy study, HHV-6 DNA was found in 25% of the vestibular, 30% of the trigeminal, 40% of the geniculate and 55% of the dorsal root ganglia, almost always as a co-infection of VZV or HSV-1. HHV-6A is suspected of entering the brain through the olfactory nerve, and is also found in the olfactory bulb.
- Find out more about the Vagus Nerve Infection Hypothesis
HHV-6 and Herpesviruses
“Daram Ablashi …guesses that 15-25% of ME/CFS patients may have a low-grade persistent HHV-6 infection” Kristin Loomis
Do we have any idea what percentage of people with chronic fatigue syndrome (ME/CFS) have an active herpesvirus-6 infection?
We believe that ME/CFS is quite heterogeneous with multiple infections and co-infections. Dharam Ablashi, our scientific director and author of over 90 papers on HHV-6 and EBV, said that based on work with samples he has done in the past, he guesses that 15-25% of ME/CFS patients may have a low-grade persistent HHV-6 infection. Dharam discovered HHV-6 in Bob Gallo’s lab at the NCI/NIH and is also one of the founders of both the IACFS and the EBV Association.
- Find out more about Dr. Ablashi here.
Are more sensitive tests available for HHV-6?
Although it is very easy to identify a primary infection or an acute reactivation of HHV-6 in a transplant by PCR DNA tests, it is very difficult to identify a low-level persistent infection in an organ.
“..one can die of persistent HHV-6 myocarditis with no trace in the plasma.” Kristin Loomis
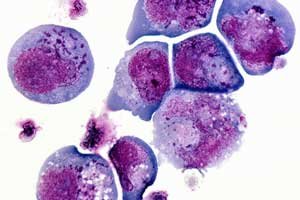
Once it is ensconced in the tissues, HHV-6 spreads from cell-to-cell through the cell wall. In fact, one can die of persistent HHV6 myocarditis with no trace in the plasma. Similarly, you can have a persistent infection in the liver, with barely noticeable HHV6 DNA levels in the blood. And the virus does not even have to be replicating to disrupt function. A recent study demonstrated that even cells latently infected with HHV-6 produce chemokines that chemo-attract pro-inflammatory monocytes.
Dan Peterson was able to find HHV-6A in spinal fluid and some plasma samples, but he used an ultra-sensitive nested PCR at a private laboratory and that laboratory is no longer offering the test. Commercial laboratories generally don’t use nested PCR because it is time-consuming and prone to false positives.
One way to increase sensitivity is to start with a larger volume of material, and then using a high-speed centrifuge to concentrate the material before testing the DNA. Several groups studying HHV6A in MS have used this type of ultrasensitive assay to detect very low levels of HHV6 DNA in the plasma. Otherwise, they say it is like looking for a needle in a haystack. There are some new technologies that have promise, but the assays need more time to be developed.
Lassner’s presentation at the Symposium on Viruses a couple of years ago on herpesvirus associated heart issues was fascinating. He told me at the time that researchers in the US simply didn’t look for pathogens even in people with ‘idiopathic’ ie difficult to explain heart problems. Has that approach changed at all over the past couple of years?
Nothing has changed. Most patients with viral myocarditis or dilated cardiomyopathy in the US never learn if they might have a treatable virus in their heart tissue. In Germany, they are routinely given a cardiac biopsy and treated for the pathogen found – high dose IVIG for parvovirus B19, interferon for enterovirus, Valcyte for HHV-6 and CMV, Valtrex for EBV. The original reason for banning most biopsies in the 1980’s was that a small percentage of the cardiac biopsies had complications. However, 25 years later, the complication rate is negligible. One German cardiologist told me that their group conducted 5000+ biopsies (done with a tiny catheter through a vein) without a single complication. Still, for reasons that I don’t understand, there is no movement in the US to change the guidelines to allow cardiac biopsies.
Active HHV-6 infections have been definitively associated with wide variety of disorders including seven different types of encephalitis, nine different complications from transplants, two different types of seizures, etc. and ‘possibly associated’ with many diseases (multiple sclerosis, chronic fatigue syndrome, epilepsy, heart disease, liver disease, AIDS, cancer, etc.) Dr. Peterson’s presentation at the Paris HHV6 conference indicated active HHV6 infections were present in a portion of his patients. What would be needed to move chronic fatigue syndrome out of the ‘possibly associated’ category in the eyes of the medical world?
“Direct evidence of infectious etiology is always very slow to be accepted.” Kristin Loomis

According to Kristin Loomis, the commitment to fully explore the role pathogens play in illness simply is not present at this time
Sadly, I am not very optimistic that we will get very far any time soon. Even if funds could be assembled for brain and tissue registry for ME/CFS patients, and scientists found direct evidence of multiple pathogens in brain tissue, it would probably still take 20 years to persuade neurologists. Direct evidence of infectious etiology is always very slow to be accepted. For example, pathogenic levels of HHV-6B virus was found in a large percentage of fresh brain resections of patients with refractory epilepsy in multiple studies and HPV was recently found in brain samples from epilepsy patients with focal dysplasia type IIB – yet these findings have been widely ignored by the epilepsy community. It was the same of course with h. pylori and ulcers, and there are countless other examples.
Look at the slow pace in solving the problem of post-herpetic neuralgia. Scientists suspected that varicella virus was latent in the neurons of the human ganglia for 100 years before it was finally established that VZV latently infects human ganglia — and experts are still arguing about whether persistent VZV causes post-herpetic neuralgia. If it has taken so long to make progress with shingles and post herpetic neuralgia, with a large number of top institutions and investigators working on it, there isn’t much hope that we will find a fast answer in ME/CFS with so little funding and so few interested investigators.
If you could pick one thing to resolve regarding HHV-6 right now, what would it be?
I would like to see a fine needle thyroid biopsy study of HHV-6A, parvovirus B19 and enterovirus infections in CFS/ME patients for three reasons: 1) there is reason to suspect subclinical thyroid disease in a significant number of ME/CFS, 2) the thyroid may be a good proxy for the brain/vagus nerve to determine the type of infection, and 3) only 1% of the general population has a history of thyroid disease. Yet, most physicians will tell you that at least half of their ME/CFS patients have a history of thyroid disease.
There was a fascinating Swedish study reported in Lancet in 2001 that examined fine needle biopsies on 219 patients with chronic fatigue. An astounding 40% of these patients had chronic lymphocytic thyroiditis even though half of them had normal or near normal thyroid levels. Also, a recent study in Italy found that 82% of fine needle biopsy tissue samples from patients with Hashimoto’s thyroiditis were positive for HHV-6A DNA, compared to only 10% in control tissues! Furthermore, they demonstrated that the infection was active, not latent. Enteroviruses, parvovirus B19, EBV and HSV-1 infect the thyroid as well.
First on my list, however would be a treatment trial for the infants with HHV-6B induced status epilepticus (prolonged seizure). We know from a 10-year NIH funded study that 1/3 of febrile status epilpeticus is caused by HHV-6B. The mortality rate is over 20% and the infants who survive often have mental retardation or develop epilepsy, yet these infants with life threatening HHV-6 induced seizures are given no antiviral treatment.
At the Symposium on Viruses a couple of years ago, Dr. Robert Gallo, co-discover of HHV-6 said HHV-6 was a virus in search of a disease and when it found one, if it did, research would take off. I took that to mean that HHV-6 looked and acted dangerous, but that no disease specifically caused by HHV-6 had been identified. Are we any closer to finding that kind of signature HHV-6 disorder?
The closest to a signature disease is limbic encephalitis. In fact 8-10% of cord blood transplant patients develop HHV-6B induced limbic encephalitis, according to a recent meta-analysis.
HHV-6 is very similar to CMV (HHV-5) in that is has broad cell tropism and therefore causes a wide range of complications in transplant from seizures, to lung disease, to retinitis and liver failure. Transplant physicians call it “CMV disease”. I suppose we should call this condition “HHV-6 disease”. I wish we had a better name for it!
Chromosomally Integrated HHV-6
There’s also the issue of chromosomally integrated HHV6 (ciHHV6). Approximately 1% of the population is born with HHV-6 integrated into their DNA. Whole blood PCR DNA tests indicate this group has very, very high levels of HHV6 DNA in their blood; levels (>1,000,000 copies per ml – whole blood, > 1000 copies/ml – plasma) otherwise only seen in transplant patients with encephalitis and patients with severe Drug Induced Hypersensitivity Syndrome (DRESS). The high numbers indicate a person has HHV6 integrated into the genome of every nucleated cell. While most people with ciHHV6 are healthy, the virus can become reactivated under some conditions. Do any of those conditions apply to chronic fatigue syndrome (ME/CFS)?
Chromosomally integrated and reactivated HHV-6 could play a role in a small proportion of people with ME/CFS
Yes. Peter Medveckzy at University of South Florida has been working on the connection between CIHHV-6 and CFS for several years, in collaboration with both Jose Montoya and Dan Peterson. In a recent study he created a new term for CIHHV6 patients with ME/CFS. He calls it “Inherited HHV-6 syndrome” and believes that ciHHV6 may be overly represented in ME/CFS. It is also overly represented in children referred for encephalitis evaluation at 3.3%. Our foundation is encouraging more research on this condition because of the very real possibility that certain drugs (such as HDAC inhibitors) could cause HHV-6 reactivation in CIHHV6 patients.
At the Paris Conference a group of researchers including Dr. Montoya described successfully treating several patients who had ciHHV6. Upon further examination they found these individuals didn’t just have ciHHV6 but were also infected with a different strain of HHV6 picked up from another individual, and it appeared that the neurological problems these patients were experiencing were not due to the chromosomally integrated virus but, perhaps, due to a community acquired strain of HHV-6. Is it rare for a person to have both ciHHV6 and a separate strain of active HHV-6 infection –or do we know?
Yes, Medveczky reported that CFS patients with ciHHV-6 reactivate with community-acquired strains of HHV6, suggesting that since they were born with HHV-6 integration, they cannot mount an immune response when they encounter other strains or when their own strain reactivates in response to specific triggers.
Any CFS patient with a positive plasma DNA result for HHV-6 should explore ciHHV6 status and contact the HHV-6 Foundation’s ciHHV6 registry.
The HHV-6 Foundation
- About the HHV-6 Foundation.
- Information For Patients
- Information for Doctors
- HHV-6 Treatments
- HHV-6 Research







Excellent interview Cort! Thank you for doing it and thanks to Kristin Loomis for pushing the agenda for real research and translational medicine. We need 100 Kristin Loomis and more Dr. Montoya, Peterson, Kogelnik … The role of viral pathogens such as HHV6 A and HHV6 B cannot be stressed enough, together with the other herpes viruses (which have the capacity of mutual transactivation) CMV, EBV, HVS1/2, VZV and handful of other culprits Mycoplasma P., Parvo B19. Let’s not forget the infamous Enteroviruses. Some of us have abnormal MRI’s, many of us harbor a great majority of these deadly viruses, we’re also passing them to our children. We need tissues/organs biopsies, we need A/V treatments, we have ME as per the WHO a neuro immune disorder as serious as RRMS.
Good call Cort, I’ve also been wondering about Lipkin’s results in the context of Lassner’s findings. If it were as simple as looking in blood one wonders why it would be necessary for the German group to do biopsies. I wonder if it would be feasible for Lassner to send Lipkin blood samples from patients that Lassner has confirmed positive by biopsy PCR and see if Lipkin can detect which ones are positive with the tests that he’s using for ME/CFS patients. If Lipkin can’t confirm the German biopsy results by looking in blood then who gives a hoot what his ME/CFS findings are?
That would be a great study. I imagine the patients with the positive biopsy results would test out as pathogen free in the blood.
I wonder why Lipkin wouldn’t be aware that MORE SPECIALIZED testing was needed ??? Doesn’t seem to make a lot of sense . . . Good information above; thank you 🙂
I agree that it’s odd. I don’t know the answer. I thought that Lipkin would do the most intensive testing possible. We’ll find out more when the paper is published.
.
If so, then THAT also is very interesting–why not go the extra mile ESPECIALLY now?? Anyways, as you say, we’ll find out more!!
What I find odd about this is that Carlos Montoya – Stanford’s HHV6 expert, has advised and been funded by the HHV6 foundation yet is a key player in the Lipkin study, providing hundreds of patients. I find it hard to believe he would take part in a study he thought was wasting its time on HHV6. Any chance of a comment from him on the points Krisits Loomis makes?
IT may be that the antibody work still to be done by Ian Lipkin and co is the main plan for finding HHV6 an other herpesviruses that might be persistent infections; would be good to know
The study looked for all sorts of pathogens not just HHV-6. However, Kristin did state she didn’t think it would be able to pick up any of the ‘persistent, subacute’ infections she believes occur in ME/CFS.
We’ll see exactly what Dr. Lipkin’s assays were when the paper is published probably in the near future.
For what it’s worth, Dr. Montoya is a member of the HHV-6 Foundation’s advisory board as well. We haven’t heard his thoughts on the Lipkin study yet. He has never thought pathogens were causing problems in most patients; if memory serves right, he usually refers to a rather small subset, but he does find them and treat them.
His Stanford Initiative’s primary aim is to “study the roles that infection and the immune response play in the symptoms of patients suffering from chronic, unexplained diseases.” He must have chosen that aim because he had direct evidence of infection in ME/CFS patients generated from years ofstudying and treating them, yet his patients were all (except for a couple) were clear of viruses according to this study. We’re obviously missing something here.
I know of one person who had an established infection and did very well on antivirals. I don’t know if his blood was in there, but if it was he did not show up as a positive on PCR in the blood.
oh dear more viral distraction
DIRECT evidence of an infectious etiology is always very slow to be accepted, says Kristen Loomis!
Why?
It impacts the bottom line, that’s why. RP
Thank you for this very informative interview, Cort!
Do you know why VanElzakker supports the Vagus Nerve Infection Hypothesis for Chronic Fatigue Syndrome dropping a retrovirus protein into rodent`s spinal cord?
http://simmaronresearch.com/2013/12/one-theory-explain-vagus-nerve-infection-chronic-fatigue-syndrome/
You wrote:
“First, researchers mimicked a localized nervous system infection by dropping an HIV protein known to activate glial cells into rodents’ spinal cord.”
Why did he use a retrovirus and not e.g. HHV-6? Any idea?
I don’t know, but my guess is that HIV is so well known and studied that they would start this process with a pathogen like that. I don’t believe VE was involved in the study.
Kristin passed this along
“The answer to Katharina is that HHV6 can only infect monkeys naturally. You can make a transgenic mouse (CD46 transgenic mouse) that can become infected with HHV6A and there is a group in France that has them. That means they have the CD46 receptor that allows HHV6 to enter.
The HHV6A infected mice and monkeys develop CNS lesions by the way.”
Thank you very much for answering my question! Very interesting what Kristin writes about HHV6A infected mice and monkeys developing CNS lesions!
Everybody talks about infections. We don’t even know what is ‘infected’, which place? I think researcher will never find it in the blood, it is the wrong place. Spinal fluid, mri of brainstem, ganglia and nerves along the spine should be examined now. I am very confident that this is the place to be… 🙂
I think Kristin Loomis and VanElzakker would agree with you 🙂
I wonder if all CFS/ME patiënts have had high fever during their infection before this illness starts. I still believe this can be the trigger.
Sophie Mizra and Lynn Gilderdales’ autopsies showed dorsal root ganglionitis.
http://niceguidelines.blogspot.com/2011/04/lynn-gilderdales-autopsy-showed-dorsal.html
A neuropathologist testified at the inquest that four out of five of Mirza’s dorsal root ganglia showed abnormalities and evidence of dorsal root ganglionitis, inflammation of the dorsal root ganglion
http://en.wikipedia.org/wiki/Sophia_Mirza
Thanks, I didn’t know that.
My goodness, what a wonderful interview, Cort. Thank you! I’m deeply appreciative to Kristin Loomis and to all of the researchers she mentioned who are piecing together some possibility of recognizable patterns in ME/CFS patients.
Re: the cardiac biopsies and antivirals being given in Germany, I’m wondering if there are any studies following the patients long-term. I’d like to know whether the antivirals and other meds given to those patients have healed them. Are they well after that?
Again, many thanks.
Thanks. It’s nice knowing a bit more about Kristin Loomis.
Well… my HHV6 Titres are off the charts…you don’t even have to search hard for them…but Valcyte makes me sooooo ill I couldn’t take it… Maybe I should look in to the IV viral aspect of things?
I also should add my EBV, HSV1 and HSV2 titres are also all extremely elevated… So I do think there is some connection. I have been ill since I was 12 years old which coincidentally was the same age that a tick decided to crawl in my ear and was there who knows how long…so long I couldn’t hear… So I was later at age 16 diag with RA, then FM, CFS, Hashimotos, Lupus, Chiari Malformation, and now ME/CVID… there has GOT to be something I can do to STOP this constant viral activation!!! I have NO life… can’t commit to anything… It is so dismal it is ridiculous….
I get it Jacques – you’ve been through the wringer. Hang in there 🙂
Have you looked into mold illness or mold toxicity? Toxic by Neil Nathan or Break the Mold by Jill Crista are great books. Basically the mold allows the pathogens to overcome by inhibiting the immune system.
So much knowledge; so little help to be found. Discouraging: even if the studies were completed and proof was at hand, it would take neurologists 20 years to wrap their heads around it. Like we all knew forever that ulcers were a result of STRESS, right?
Particularly ominous: ciHHV-6, A vicious perpetuating cycle. Perhaps before treatment is available, we shouldn’t breed?
Encouraging: Will Kristin Loomis and others serve as an impetus for future HHV6 study design to get a meaningful end result?
Feeling more sure about: the US government, HHS and CDC, do not want to get to the real nitty gritty of ME/CFS because it will cost a small fortune to research and treat. Can you imagine the insurance lobbyists descending on Washington? In all honesty, we should beat them to it.
Great insight. Thanks. Very interesting to read the connection about the thyroid. One of my doctors thinks that there is definitely a connection between ME/CFS and thyroid issues because most of his ME/CFS patients also went on to develop thyroid disease.
Hi Cort
Thanks for the great articles.
Michael VanElzakker tweeted in August 2013 that he and Anthony Komaroff were putting together a pilot study. (On his vagus nerve infection theory no doubt).
Have you heard anymore about this?
Rather eager for that research to go ahead.
beaverfury
Love about Lipkin, this article written above in 2014 & when Lipkin said he would find answers way back then we still have no answers & he got his Grants & nothing more…All talk talk talk & no damn answers thanks Lipkin