The Missing Body
“It’s commonly claimed that, despite its severity and widespread nature, FM has not been associated with an identifiable peripheral-tissue lesion” Authors
Fibromyalgia has come mostly to be thought as a ‘brain disorder’ but recent studies are putting focus back on the body
The ‘word’ on Fibromyalgia, which was originally proposed to be a disorder of the muscles, has been that it’s a disorder of the central nervous system. Studies have found that both the pain-producing and the pain-inhibiting sides of the central nervous system in Fibromyalgia are clearly dysregulated. These are important findings, but they’re not the whole story. You wouldn’t know that from overviews of the disorder on the web where the central nervous system paradigm dominates.
Some have speculated that lower levels of a brain neurotransmitter called serotonin leads to lowered pain thresholds or an increased sensitivity to pain. Serotonin is associated with a calming, anxiety-reducing reaction. The lowered pain thresholds in fibromyalgia patients may be caused by the reduced effectiveness of the body’s natural endorphin painkillers and the increased presence of a chemical called “substance P”. Web MD
Even the National Fibromyalgia Association makes no mention of the peripheral nervous system (although it does mention cytokines) in its overview of causes
The FM patient experiences pain amplification due to abnormal sensory processing in the central nervous system. An increasing number of scientific studies now show multiple physiological abnormalities … including: increased levels of substance P in the spinal cord, low levels of blood flow to the thalamus region of the brain, HPA axis hypofunction, low levels of serotonin and tryptophan and abnormalities in cytokine function.
The Body is Back
The evidence has been mounting over time, but over the past year it’s become clear that Fibromyalgia is not a brain or a body disorder: it’s both. Recent studies have found immune, autonomic nervous system, and muscle issues in FM. With this fourth study in the past year showing substantial damage occurring in the peripheral nervous systems, the body is back in the FM spotlight big time.
- With small nerve fiber problems showing up consistently in Fibromyalgia, the body is back in the spotlight
The next big question is going to be what is the chicken and what is the egg in FM. The authors of this paper are clear that they believe nerve problems in the body are the egg.
The lead author in this study, Dr. Xavier J. Caro, reported finding large-fiber neuropathy in FM patients in 2008 and was the first to report small nerve fiber problems in FM. His work with large fiber neuropathy was curtailed by the invasive, painful and costly nature of the testing, but then he turned to looking at small fiber neuropathy (SFN)’
In the study, Dr. Caro and Dr. Earl Winter state their interest in the peripheral (body’s) nervous system (as opposed to the nervous system in the brain) is really quite simple. When people with FM describe their symptoms they’re describing neuropathic or nerve problems. They note that the ‘language’ of FM can seem fantastic to the uninitiated but clearly indicate that problems with the nerves are present. Terms like ‘burning’, ‘stabbing’, ‘pins and needles’, ‘hot’, even just ‘miserable’ all describe nerve problems.
For myself the hot, burning sensations I get after too much exercise are rarely found on symptom checklists. I don’t think they’ve been used as diagnostic by any physicians I’ve seen, yet for me they are a major symptom and a major part of post-exertional malaise. They are also nerve symptoms.
Nerve symptoms are very common in FM. Caro and Winter note that over 75% of their FM patients use nerve symptoms to describe their disorder, but only about 20% of rheumatoid arthritis patients do, and other studies have found even higher rates of neuropathic language in FM. In fact, people with FM use much the same language to describe their symptoms, as do diabetics who have peripheral neuropathy.
The Study
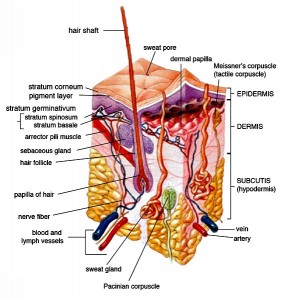
Between 2007 and 2011 Caro collected skin biopsies from about 40 FM patients and 40 healthy controls and examine their blood for immune factors. The results make up this present study.
A screen for an array of autoimmune and sensory disorders ultimately eliminated over 20% of the initial pool of FM patients due to the presence of diabetes, autoimmune disorders, hepatitis, etc.
Results
“We … report a surprisingly high prevalence of diminished ENFD (epidermal nerve fiber density) in FM” Authors

All people with Fibromyalgia had a ‘stocking distribution’ pattern in which nerve losses were worse the further ‘south’ one went
This was an older group of FM patients (mean age 60), every single one of which had some diminished sensory perception in their lower extremities. They also had significantly decreased nerve fiber density in their feet and thighs (p = 0.0002) – a sign that their peripheral nerves had been damaged – compared to the controls. In what’s called a ‘stocking distribution’, the further down the legs they tested the more damage they found – a pattern that is often found in small fiber neuropathy.
Fourteen of 40 FM subjects had evidence of hypercholesterolemia, and 11 had hypertriglyceridemia.
The fact that pain levels were not significantly associated with nerve fiber loss suggested that the pain in FM was not solely due to that loss.
Given their past findings of large fiber neuropathy in FM, they assume the FM patients with SFN also have large fiber involvement as well.
Immune System
“We consider it likely that an immunopathogenic mechanism is at work” Authors
The lead author in this study, Xavier J. Caro MD, is a rheumatologist and has quite a history in studying and treating FM. Thirty years ago he reported finding IgG at the dermal/epidermal junction in FM patients, and in 1989 he proposed that FM was in part an immune disorder. In this study he and his co-investigator, Earl F. Winter PhD, noted a variety of abnormal nervous system and immune findings associated with the skin in FM patients, with most of those abnormalities dating back to the late 1980s.
More recent studies have found evidence of increased mast cell activation, changes in collagen structure, and increased cytokine levels in the skin. In 2013 Caro published a chapter in a rheumatology textbook where he called Fibromyalgia a ‘neuroimmune’ disorder (“Fibromyalgia: Evaluation and therapy of a neuroimmune disorder”). One has the feeling he’s been looking forward to having this discussion for a long time.
In this study, low nerve densities were significantly correlated with increased IL-2R levels. Il-2R activates T-cells and macrophages, and high levels have been associated with autoimmune disorders including multiple sclerosis.
They noted, as have others, that intravenous immunoglobulin (IVIG) does help some people with Fibromyalgia. (In Dr. Sivieri’s experience, small fiber neuropathy in FM is associated with IgG subclass deficiencies, particularly in the IgG subclass. IgG’s or immunoglobulins refer to antibodies produced by B-cells.)
Pointing a finger straight at the immune system, the authors suggested that a ‘cytokine-related’ lesion (i.e., small fiber loss) would not be unexpected and noted that IL-2R administration in cancer patients can produce an FM-like state.
(Discovery of cytokine-induced small fiber neuropathy might be a good thing because it presents the possibility of producing a drug to block IL2-R.)
Pain
Why the pain if the nerve fibers – the source of the pain – have been destroyed? Because they haven’t been completely destroyed and those that are still left are understandably upset (hyperexcitable) and they’re also communicating that upset to the secondary nerve fibers that are intact around them.
‘Central’ Sensitivity Not So Central?
The authors clearly have not been taken with the central sensitivity paradigm that’s held sway for past decade or so in FM. They bluntly stated that the two CNS factors primarily blamed for FM, wind-up and central sensitization (CS), are likely to be secondary rather than primary. They went so far as to state that there is “no credible scientific or clinical evidence that reducing, or even eliminating, CS down-regulates pathological peripheral pain input at all.”
They’re not saying that medications that reduce factors associated with central sensitization don’t work; they may reduce pain, but they play no role in reducing pain inputs from the periphery.
In the past it’s been thought that small pain inputs from the periphery or body in FM get jacked up by a process of central sensitization. These authors believe the pain inputs from the body – from the damaged nerves they and others are finding – are pathological.
If central sensitization was responsible for the pain coming in from the periphery, then diminishing it should result in reduced pain coming in from the body. But they see no evidence of that.
Instead, they provide hope that the going after the problems in the peripheral nerves can eliminate the ‘dysfunctional’ nature of the body pain in FM, and that treating the nerve problems lends itself ‘very well’ to ‘everyday clinical management’ of FM. In response to an email Dr. Caro stated that the treatment of FM is complex and that no two cases are alike but that in the main most Fibromyalgia patients require ‘immune modulators’ – an amazing statement given the current focus on the brain in FM.
But with small nerve fiber damage showing up, and studies proposing that an immune signature has been found, and with Dr. Pridgen reporting ‘impressive results’ from his antiviral trial, perhaps an approach using immune modulators in Fibromyalgia isn’t so amazing after all.
Dr. Caro has written a chapter on evaluating Fibromyalgia patients and is planning to write a chapter on FM treatment. A study on immune deficiency in FM has been completed as well and will be released at a National Arthritis Conference in the fall.
Two more things: The authors don’t talk about the autonomic issues arising from small fiber neuropathy, but they do note that autonomic nerve fibers are involved. Nor do they talk about the effect of SFN on exercise. We don’t know how far the neuropathy in FM and presumably ME/CFS extends, but a loss of nerve density in the muscles would reduce muscle activation as well.
When one person with SFN noted how her muscles kept locking up the day after exercise, her neurologist explained that most muscles have several sets of nerves feeding them. When one set of nerves is ‘used up’ during exercise, the others kick in (and activate more parts of the muscles). If’s you’ve only got one set of nerve fibers left, if you keep sending messages down that nerve the muscles will just lock up. Symptomatically that sounds a lot like the muscle stiffness that I experience after exercise.
Check out other small fiber neuropathy posts







Thanks for the very interesting article, Cort. For me, the most relevant part was the comparison between the pain of FM and rheumatoid arthritis. I was diagnosed with RA approximately 20 years after my ME/FM/MCS diagnosis. Thereafter, I attributed my numb extremities and the stinging/stabbing/burning pain in my hands and feet (and occasionally up my legs)to RA. Each time my rheumatologist advised that my RA medication was keeping this illness under control (based on blood tests), I was skeptical. Only recently have I suspected that my significant nerve pain is related to ME and FM — not
RA. This article seems to confirm my suspicions.
Has anybody else out there developed rheumatoid arthritis long after being diagnosed with ME, FM or MCS?
Karen, I was diagnosed with FM in 1991, RA in 2003 (though I think it had gone undiagnosed since 1997) and CFS/ME in 2010. For me I think CFS actually was occurring long before 2010 but on a diminished level until I had a traumatic injury in 2010 which unleashed full-blown CFS. This is an interesting finding; it’d be great to see some genuine progress on at least one of these diseases.
I’ve had FM, with the severe neuropathic-type pain in legs and elsewhere, as well as the more rheumatic-like pains bones and muscles, for 25 years. Maybe I’m a “cup half-empty guy” but, at 65 y.o., I find it depressing that medicine really has no WTF idea what is making us ill. CNS, peripheral, rheumatic origin (let alone etiology) …this is what diabetics must have felt like before they discovered insulin. Depressing.
Yes me!
Hi there,
That’s really interesting! I was just wondering if you could link us to the original article/report?
Thanks, Melissa
I forgot again! It’s in there now and here’s the link to the study – http://www.ncbi.nlm.nih.gov/pubmed/24719395 – thanks for reminding me.
Many thanks! 🙂
Cort, on my computer, the little box at the top of this screen with quotations in praise of your work resizes each time it the quote changes. This makes the whole rest of the screen jump down a couple of lines and then back, making it almost impossible to read, at least not without getting a headache. I like to read what you have to say, but not at that price. 🙁 I hope that can be changed so I can go back to reading your column.
Cort, my page jumps around, too, and it adds to my dizziness, etc.
I hope you can fix it soon. Your site is the only one I know of where this happens. Thank you.
I’m experiencing the same thing and I thought it was just another new symptom of FM!!
Mine too Cort, doesn’t stop me reading 🙂 but much nicer it didn’t.
Just copy and paste the text somewhere else
SFN is also found a lot with POTS. Newest research is finding autoimmune and autoantibodies as connections.
http://www.dysautonomiainternational.org/blog/wordpress/new-evidence-of-autoimmunity-in-pots/
Issie
http://onlinelibrary.wiley.com/doi/10.1002/mus.24245/abstract
New study showing SFN causing cardiac denervation with POTS. More connections! Still could be autoimmune at the core.
Issie
Thank you, it is reassuring to find decent research as to cause going on out there.
Twenty patients is a very small number. This data needs confirmation with further studies!
Actually according to the abstract it was 47 FM/ME/CFS patients and 47 healthy controls. Maybe I misrepresented the numbers in the blog.
Have you noticed that Cort has a link to Amazon on each page? If you come back to that link to enter Amazon before shopping there we will all benefit. Let’s support Cort!
P.S. Where may we find this study?
Very interesting Cort.
It seems that other researchers have come to the same conclusions in respect of ‘spontaneous/neuropathic’ pain associated with peripheral neuropathy generally (ie not just in fibro) :
Primary afferent input critical for maintaining spontaneous pain in peripheral neuropathy.
http://www.ncbi.nlm.nih.gov/pubmed/24704366?dopt=Abstract
Which attracted an interesting comment (albeit with academic interests declared) :
“1) Most importantly, it demonstrates very clearly and convincingly that spontaneous and evoked pain abnormalities associated with either traumatic nerve injuries or polyneuropathies are all sustained by some peripheral input. This is not to say that there are not important pathologies taking place in the CNS – or that CNS changes do not contribute to persistent pain states. They probably do, but this paper says that for these types of neuropathic pain, a peripheral abnormality is critical to sustain all forms of abnormal pain signalling. And of course it also follows that strategies to treat pain by targeting PNS or CNS processes could still both be effective.”
http://www.painresearchforum.org/papers/39252-primary-afferent-input-critical-maintaining-spontaneous-pain-peripheral-neuropathy
This seems to favour a twin track approach to treatment but who knows how the brain might recuperate if the peripheral damage was addressed?
Great comment – thanks for highlighting that….
Caro et al stated that addressing the peripheral source of pain is more effective than addressing the CNS problems – so maybe doing that does allow the CNS to calm down. Unfortunately there was no ‘one treatment fits all’ approach; FM and ME/CFS are complex and he takes them one patient at a time. However, he did focus on immunomodulators…(which makes me think of Ampligen).
It would be fascinating and I imagine at some point someone will hit the periphery with treatment and examine how the CNS responds.
Cort,
You have a gift for writing. I’m running out of superlatives to describe your posts.
This struck me as a key question I’d to see answered..
…….Nor do they talk about the effect of SFN on exercise……
Does/can SFN cause muscle pain and PEM?
Once again, I punched the donate button. You are a unique resource.
Love it Tim – thanks again for you support. I do know really wonder about the effects of SFN on PEM and exercise. I do believe that a brain study done quite some time suggested normal muscle activation was not occurring in ME/CFS. Could it because the nerves that trigger the muscles to act are damaged? What an interesting idea!
PS – There are those that try to equate centralization of pain as FM. I have long maintained it is not the same. If it were, patients with low back pain, as an example, would also have at least one of the comorbid conditions, thyroid disease, migraine, AS, IBS, etc. This simply is NOT true.
I would agree with you Celeste – central sensitization may be present but most, if not all CS syndromes require a steady state of peripheral nociceptive input in order to maintain the CS. The trend to discuss FM in terms of CS has led to the assumption that the centralization is a self perpetuating cycle which is incorrect.
I wouldn’t rule out the overlap between ‘central neuropathic pain’ and FMS. Complex regional pain syndrome appears to share many of the multi-system symptoms found in FMS and ME/CFS :
http://www.cortjohnson.org/blog/2013/11/09/chronic-regional-pain-syndrome-fibromyalgia-mecfs-spreading-neuroinflammation-model/
Right here is the right blog for anyone who wants to understand this topic.
You understand a whole lot its almost hard to argue with you (not that I actually would want to…HaHa).
You definitely put a new spin on a subject that’s been discussed for ages.
Excellent stuff, just excellent!
Feel free to surf to my web site: how to increase Testosterone levels
Very interesting! And it certainly makes a lot of sense. It is a shame that we are being sent to rheumatologists when it really should be neurologists. A study in Canada suggested that a high percentage of rheumies don’t want to deal with FM – because they feel it is completely out of their remit and area of expertise!!! Agreed!
When there is the mention of ‘immune modulators’ this is most likely why LDN is helping so many people with fibro…as it helps rebuild the immune system.. It certainly has made a difference for me – even just being able to SLEEP again and reduce my pain has made it the best out of all the things I have tried – holistic, western and eastern medical approaches.
(For more information on LDN please look at the LDN Research Trust website – they can help you to locate a doctor in your area – in over 150 countries). http://www.ldnresearchtrust.org
A.
Alyssa,
I certainly agree with the suggestion that rheumatologists don’t want to deal with FM. I’ve seen two (Canadian) rheumies for Rheumatoid Arthritis during the past few years. Both also confirmed FM, but neither has shown any interest in addressing it.
With respect to LDN, I’d like to refer readers of this blog to Dr. Ellie Stein’s website, and the International Awareness Day event she has scheduled for May 4. The following link gets you to her website.
http://www.eleanorsteinmd.ca/news/
Click where it says “May 4th Poster” in blue for details.
Those who are unable to attend in person can register for the webcast. Jarred Younger will be one of the presenters, and based on Cort’s April 14 article on LDN (which mentions Doctor Younger), I’m wondering if this will be one of the topics he covers in his presentation on FM treatments that may be available in the next few years.
But is so great. I found ldn about 6 months ago . I can say my pain level has decreased immensely and I sleep again. Brain fog is gone.
I am aware. Fibromyalgia is a life long disability and flareups happen but my life is livable again.
I keep stress down and am thankful for each day.
That is so great to hear Sherri. Thanks for passing it on.
🙂
I run a network of support groups in wales. All this info is really interesting. When I have attended conferences in Ireland and UK the central nervous system was continuosly mentioned so was the brainstem
Its interesting as all the reseach goes back to our nervous system being dysfuctional. Yet you get a neurologist to define fibro as a neurological condition. Keep up the good work x
Thanks Yvonne
I’m experiencing the same thing and I thought it was just another new symptom of FM. Your blog is very interesting! It certainly makes a lot of sense. It is a shame that we are being sent to rheumatologists when it really should be neurologists.