

(In part two of our series on BDNF and Chronic Fatigue Syndrome Dr. Courtney Craig looks at natural ways to increase BDNF levels.)
A Modifiable Piece of the ME/CFS Puzzle? BDNF
Leading ME/CFS researcher Lenny Jason and his group just released a novel study showing that the protein brain derived neurotrophic factor (BDNF) was below normal levels in Chronic Fatigue Syndrome patients (1). This study provides another biomarker that validates the illness as real and organic. But, most importantly, it presents another modifiable piece of the complex puzzle of CFS.
What is BDNF?
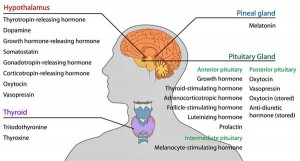
BDNF is a central nervous system growth factor protein coded for by a gene of the same name. The BDNF gene is expressed in the greatest quantity in the dorsal vagal complex and the dorsal motor nucleus of the vagus—both housed in the hypothalamus. A new theory posed by neuroscientist VanElzakker, suggested that infections may migrate via the vagus nerve and perpetuate ME/CFS symptoms (2). If correct, this theory may also encompass BDNF gene activity in these key vagal areas in the brain.
In the body, BDNF is found primarily in serum, plasma, and platelets. It is also produced by immune cells such as lymphocytes and macrophages. To a lesser extent it circulates in cerebral spinal fluid.
BDNF acts like fertilizer for neurons—prompting sprouting of new neuronal connections in a process known as neural plasticity. Suppression of BDNF has been found to lead to neuronal atrophy within the hippocampus—a key area for memory formation and implicated in depression. Higher levels throughout life are associated with reduced risk of age-related cognitive decline from oxidative stress (3).
The BDNF-Gut Connection
Excitation at the HPA axis and reduced BDNF levels have been linked with altered gut bacteria in mice
In animal studies, altered gut flora is believed to regulate the HPA axis. In mice without gut flora (germ-free), the stress response is exaggerated at the HPA axis and consequent reductions in BDNF are also found. These mice exhibit impaired cognition and increased stress as measured by plasma neurotransmitters. One study reintroduced the bacterial species B. longum which normalized BDNF levels and reduced markers of stress (4).
The mechanism in animals is believed to be mediated by the vagus nerve, which directly links the gut to the brain—a gut-brain axis. As mentioned above, the densest concentration of BDNF genes are found in vagus nerve nuclei in the hypothalamus, further supporting that bacterial species can migrate or perpetuate their effects via this important cranial nerve.
Could disrupted gut flora be the underlying reason for Dr. Jason’s latest discovery?
BDNF’s Role in Fibromyalgia
Many studies have been conducted that measure BDNF in fibromyalgia. Interestingly, the majority of these studies reveal increased levels of serum BDNF in fibromyalgia patients. Here, BDNF appears to influence painful sensory input and hypersensitivity (5). This could be a defining characteristic that differentiates ME/CFS from Fibromyalgia.
BDNF’s Role in ME/CFS

Neuroinflammation = high rates of oxidative stress = neuron damage = probably low BDNF levels in ME/CFS; e.g. the patients in the neuroinflammation study probably had low BDNF levels as well
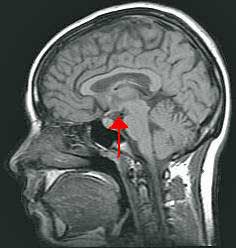
An advanced imaging study in ME/CFS found widespread neuroinflammation in various key brain regions including the cingulate cortex, hippocampus, amygdala, thalamus, midbrain, and pons. Inflammation in these areas was 45%-199% times higher in ME/CFS patients than in healthy controls (6). Since neuroinflammation leads to oxidative stress and mitochondrial damage, it is reasonable to extrapolate this data and speculate that BDNF levels would be reduced in this cohort of patients if measured.
The only other study examining this comes from an animal model of ME/CFS. Decreased BDNF was associated with brain atrophy and cell death at the hippocampus. When these animals were given therapeutic BDNF stimulants, hippocampal size increased and daily activity level increased (7).
Simple Ways to Raise BDNF
Eat a Healthy Diet and Fast

Caloric restriction as well as gentle fasting can help raise BDNF levels. On her website Dr. Craig notes found that fasting helped her with her ME/CFS.
Caloric restriction and intermittent fasting promote cellular pathways that reduce oxidative stress and raise BDNF levels (sirtuin family of genes). Rodent studies where the diet consisted of high sugar, “junk food” rat chow, resulted in greatly reduced BDNF levels and increased oxidative stress (3).
Get Some Sun
Animal studies show reduced BDNF levels with light deprivation. A 2012 human study described the seasonal variation of serum BDNF levels in a European cohort. Results indicated that BDNF concentrations have seasonal variation—levels increased over the course of the spring and the summer and decreased over the course of the autumn and the winter. Also, there was a positive correlation between the number of sunlight hours and the concentration of serum BDNF (8).
Exercise or Learn Something New
Animal and human studies have demonstrated that moderate exercise can stimulate BDNF production and the creation of new neurons. If health allows, light aerobic exercise seems to be the best means to increase BDNF (3). Additionally, learning a new task or completing a challenging activity can promote neurogenesis through BDNF (3).
Supplements That Raise BDNF
Curcumin
Curcumin is widely studied as a possible drug target for Alzheimer’s disease and other neurodegenerative disorders. Many studies show this spice is a potent activator of BDNF and may even reduce amyloid beta deposition and brain atrophy—hallmarks of Alzheimer’s (3,9).
Resveratrol & Green Tea
Resveratrol is a potent antioxidant found in red grape skins. In an animal model of ME/CFS, supplementation with resveratrol raised BDNF levels and improved activity levels (7). A compound in green tea, epigallocatechin gallate (EGCG), may be a more potent stimulator of BDNF than resveratrol, however. Animal and in vitro studies comparing the two compounds show that EGCG readily crosses the blood-brain barrier and stimulates the BDNF signaling pathway (10).
Omega-3 Oils (EPA and DHA)
The long-chain, polyunsaturated fats EPA and DHA have numerous benefits for neurological health. Several studies have examined the biochemical mechanism of action of these fats and demonstrated their ability to promote BDNF expression. The cellular effect of EPA and DHA administration is the creation of new neurons as well as neuron protection via anti-inflammatory signaling (3,11).
-
- More on the BDNF study – Knackered Nerves: Do Low BDNF Levels Spell Nerve Exhaustion in Chronic Fatigue Syndrome? Pt. I
______________________________
Dr. Courtney Craig D.C. was first diagnosed with CFS as a teen in 1998, and recovered in 2010 utilizing both conventional and integrative medicine.
Trained as a doctor of chiropractic and nutritionist, she now provides nutrition consulting and blogs about what she’s learned at www.drCourtneyCraig.com/blog.
- Check out more of Dr. Craig’s Health Rising blogs here
Support Health Rising – We Love Small Donations!
_____________________________
1 Sorenson M, Jason L, Peterson J, Herrington J, Mathews H (2014) Brain Derived Neurotrophic Factor is Decreased in Chronic Fatigue Syndrome and Multiple Sclerosis. J Neurol Neurophysiol S12:S2-013. doi: 10.4172/2155-9562.S12-013. http://omicsonline.org/open-access/brain-derived-neurotrophic-factor-is-decreased-in-chronic-fatigue-syndrome-and-multiple-sclerosis-2155-9562-S12-013.pdf
2 VanElzakker MB. (2013) Chronic fatigue syndrome from vagus nerve infection: a psychoneuroimmunological hypothesis. Med Hypotheses. 81(3):414-23. doi: 10.1016/j.mehy.2013.05.034. Epub 2013 Jun 19. http://www.ncbi.nlm.nih.gov/pubmed/23790471
3 Gomez-Pinilla F. (2008) The influences of diet and exercise on mental health through hormesis. Ageing Res Rev. 7(1):49-62. Epub 2007 May 5. http://www.ncbi.nlm.nih.gov/pubmed/17604236
4 Wang Y, Kasper LH (2014) The role of microbiome in central nervous system disorders. Brain Behav Immun. 38:1-12. doi: 10.1016/j.bbi.2013.12.015. Epub 2013 Dec 25. http://www.ncbi.nlm.nih.gov/pubmed/24370461
5 Nugraha B, Karst M, Engeli S, Gutenbrunner C. (2012) Brain-derived neurotrophic factor and exercise in fibromyalgia syndrome patients: a mini review. Rheumatol Int. 32(9):2593-9. doi: 10.1007/s00296-011-2348-2. Epub 2011 Dec 31. http://www.ncbi.nlm.nih.gov/pubmed/22210272
6 Nakatomi Y, et al (2014) Neuroinflammation in Patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An 11C-(R)-PK11195 PET Study. J Nucl Med. 55(6):945-950. [Epub ahead of print]. http://www.ncbi.nlm.nih.gov/pubmed/24665088
7 Moriya J, Chen R, Yamakawa J, Sasaki K, Ishigaki Y, Takahashi T. (2011) Resveratrol improves hippocampal atrophy in chronic fatigue mice by enhancing neurogenesis and inhibiting apoptosis of granular cells. Biol Pharm Bull. 34(3):354-9. http://www.ncbi.nlm.nih.gov/pubmed/21372384
8 Molendijk ML, et al (2012) Serum BDNF concentrations show strong seasonal variation and correlations with the amount of ambient sunlight. PLoS One. 7(11):e48046. doi: 10.1371/journal.pone.0048046. Epub 2012 Nov 2. http://www.ncbi.nlm.nih.gov/pubmed/23133609
9 Chen Q., et al. (2011) A novel neurotrophic drug for cognitive enhancement and Alzheimer’s disease. PLoS One. 6(12):e27865. doi: 10.1371/journal.pone.0027865. Epub 2011 Dec 14. http://www.ncbi.nlm.nih.gov/pubmed/22194796
10 Nath S, Bachani M, Harshavardhana D, Steiner JP. (2012) Catechins protect neurons against mitochondrial toxins and HIV proteins via activation of the BDNF pathway. J Neurovirol. 2012 Dec;18(6):445-55. doi: 10.1007/s13365-012-0122-1. Epub 2012 Aug 11. http://www.ncbi.nlm.nih.gov/pubmed/22886603
11 Su HM. (2010) Mechanisms of n-3 fatty acid-mediated development and maintenance of learning memory performance. J Nutr Biochem. 21(5):364-73. doi: 10.1016/j.jnutbio.2009.11.003. Epub 2010 Mar 16. http://www.ncbi.nlm.nih.gov/pubmed/20233652









Great article. Well written. The Holtorf Centers have been using this hormone/enzyme in the brain angle in treating ME/CFS and Fibromyalgia for some time. This article appears to agree with Holtorf that serum levels (?) of many factors are actually opposite between the two conditions. Holtorf also indicates different key areas are most active between the syndromes.
I can think of two factors – both involved in the brain – which differ. I believe brain blood flows are increased in FM and substance P levels are increased in FM (but not in ME/CFS).
What treatments do Holtorf offer and how often and how effective are they?
Is this why some people get benefit from antidepressants? Maybe it’s not so much from their antidepressant effect but more the fact that they raise BDNF.
Maybe the two serotonin drugs from Biovista were doing similar things.
Anyone know what has happened with these?
It is looking more and more likely that the nervous system, the brain and the gut (the second brain) are all involved.
We just need some guidance on how to fix it
Also is the fact that some people are seeing improvements with things that work on opiates connected to this?
Good thinking Grant! You’re absolutely right, many drugs act either by direct or indirect mechanisms to upregulate BDNF gene expression.
Here’s a good summary: http://www.nature.com/npp/journal/v29/n4/full/1300345a.html
nervous system + brain + gut + immune system all involved here likely via the vagus nerve
“It is looking more and more likely that the nervous system, the brain and the gut (the second brain) are all involved.”
yes yes yes!
And not viruses!
When I read about her recovery it reminds me of all I have been reading lately on Systemic Mastocytosis. At the age she got sick she fits into the category of Cutaneous Mastocytosis. I have no doubts now that cfs or whatever thousand names given to this illness is Mast Cell Activation Disorders ‘undiagnosed’ by the entire medical establishment an illness already recognized by the W.H.O. and Haematologists are what’s needed not other Doctors.
yes, diet plays a major role but knowing which foods to eat is key as everyone has different reactions to histamine foods. that is the key not drugs in systemic mastocytosis.
numerous people recover from vfs from diet and this still does not rule out lyme disease with mastocytosis…Everyone will be different and I will bet that 9 months of I.V. did not cure patientsit was their diets that cured them possibly low histamine type foods. histamine/cytokines is Major in this monstrous illness.
Want to point out that Hip suggested in the last BDNF blog this treatment:
The smart supplement noopept has been shown to increase BDNF as well as NGF (nerve growth factor). See here:
http://www.ncbi.nlm.nih.gov/pubmed/19240853
It might be worth trying noopept for ME/CFS.
Noopept is inexpensive and readily available online. Noopept doses are in the 10 mg to 40 mg range, taken sublingually. If you read some accounts online, people often anecdotally report a great cognitive boost with noopept initially, followed by a loss of effect after some days. However, the above-cited study found that BDNF was still boosted even after 28 days of taking noopept daily, so noopept would seem to have long term benefits with regards to BDNF boosting.
An interesting article, but one thing occurred to me: if BDNF is increased in Fibromyalgia, and decreased in ME, what about people who have both disorders?
Whew! That’s a good question…I imagine there are a lot of people in that category…I wonder if there are more pure FM types (tons of pain) and pure ME/CFS patients (extreme fatigue and debility) and they are the ones who are different from each other (?????)
I was wondering the same thing myself. At my doctor’s suggestion I recently added some turmeric powder (curcumin) to many of my foods and was pleasantly surprised that it significantly reduced my rheumatoid arthritis pain. So far I can’t tell a difference on the fibromyalgia or cfs/me but I’ll start paying closer attention to both.
Just to say that I find quite high doses of cod liver oil keeps me from being severe-it seems really important , I thought its primary job in me is to increase blood circulation. Does this noopept which I’ve never heard of before now improve sleep? Mine’s getting really bad now with all the knock on effects.
this is the first time I have seen anythung that includes get some sun in the recommendations – but I and others with ME are better in the sun.
Although my brain doesn’t cope well with scientific articles these days my main problem is exercise intolerance, is there a reason to believe this would help with that?
Tatt –
wouldn’t that be great?
I, too find exercise intolerance and an inability to focus on intellectual (or scienc-y – G) reading and thought processing. I can tolerate the pain, but fatigue and not being able to “do things” either physically or mentally may drive me batty.
funny, though – a lot of sun will affect me just like exercise does.
cheers, y’all and best of luck for relief.
although I use tumeric (curcumin) in cooking I didn’t realise that to be effective it needs to be combined with black pepper. Also it can lower blood sugar and increase bleeding so there is a miscarriage risk in pregnant women. It increases the flow of bile and that can meal problems for those with gallstones.
Reservatrol is another supplement to be wary of if there are bleeding problems.
Shouldn’t articles like this include some comment about potential risks and who shouldn’t try anything mentioned without medical advice?
Hi
Help me out here people with big brains. If BDNF is raised in FM and lower in ME/cFS does that mean one would want to avoid raising it if they were primarily FM? I would guess its a separate issue. I have fatigue and I wake up every day with flu like symptoms but I believe I am primarily more FM. I read about ME/cFS and these people can’t get out if bed where I can get out of bed but it hurts like hell and my fatigue makes it hard to motivate my body. I love this article and research because it showed some measurable difference. Thank you Cort.
Please help? Why would pepper be needed while taking Curcumin to help it work better? What does it do to make better effects? Thanks for your help. I love this article. It brought alot of sense to my understanding of things while dealing with these illnesses and trying to find relief. Andrea
“Black pepper enhances bioavailability of Turmeric: One important question which must be popping in your mind right now would be why among so many spices are we talking about black pepper? The answer is really interesting too. One problem with curcumin is its low levels of bioavailability. Most of the curcumin that is ingested gets metabolized before it can get absorbed. Piperine is said to help make curcumin more bioavailable. This could be because it could inhibit certain intestinal digestive enzymes. This increases the amount of any drug or supplement that can be absorbed by the body. They also do not get degraded quickly. Hence, there are studies to test if co-administering curcumin with piperine could improve the bioavailability of the former. These studies have been conducted on humans and laboratory animals. One study found that when even 2g of curcumin was ingested, its serum levels were very low. However, when 20mg piperine was added to curcumin the bioavailability increased by 2000%. The bioavailability, serum levels and levels of absorption of curcumin all improved dramatically. Thus, if one takes turmeric, most of it is unutilized unless supplemented by addons such as black pepper.” http://www.turmericforhealth.com/turmeric-benefits/health-benefits-of-black-pepper-and-turmeric
The article below recommends a ratio of 3 parts black pepper to 97 parts turmeric to make the turmeric more effective/absorbable. I have also read that it is important to consume the turmeric with fats/oils because it is fat soluble and this enhances absorption in the gut. I’ve been experimenting with turmeric capsules I make myself with ordinary turmeric spice. I will now add black pepper to the capsules. I think the turmeric alone is helping me, but it would be great to get a boost by using these techniques to increase its effectiveness. And maybe I can use less. I am taking 4-8 big capsules per day on the advice of some of Ken Lassesen’s articles.
http://www.methowvalleyherbs.com/2012/01/turmeric-medicine-cabinet-in-curry-bowl.html