



“The Autonomic Nervous System is the interface between the mind and body.” – Martinez-Lavin
This is the second in our series of blogs overviewing Doctor Martinez-Lavin’s short primer “Fibromyalgia: How Stress Becomes Real Pain”. (Note that Dr. Martinez-Lavin has a very specific view of Fibromyalgia, and his is one among many.)
Martinez-Lavin believes the development of Fibromyalgia is ‘related’ to physical, infectious, or emotional agents (illness, divorce, broken arm, etc.) that produce stress. He doesn’t appear to be saying the infections, psychological stress, etc., cause FM, but that the stress response system plays a critical role in this disorder.
His major focus is on the autonomic nervous system, one of two stress response systems in the body. (The HPA axis is the other.)
The Autonomic Nervous System (ANS)
Martinez-Lavin takes some time to describe what is a surprisingly complex and pervasive feature of our bodies. Originating at the base of the brain, the ANS is kind of a master controller. Its job to maintain homeostasis – the healthy functioning of our body.
The ANS:
- Controls basic functions such as blood pressure, pulse rate, breathing rate, and temperature.
- “Harmonizes the functioning” in all our internal organs.
- Enables the body to respond to stress, and after the stress, returns the body to rest and recovery mode.
- Works closely with the HPA axis – the other major stress response in the body and an important immune regulator.
- Regulates the immune system.
The ANS has two branches: the sympathetic nervous system (SNS) or ‘fight or flight’ side which gears the body up to respond effectively to stressful situations, and the parasympathetic nervous system (PNS) or ‘rest and digest’ side which helps the body recover from them.
These two branches of the ANS exist in a kind of yin-yang relationship: when one is up, the other is automatically down. A third branch – a non-adrenergic, cholinergic branch which utilizes nitric oxide and affects the gut and the lungs – is also present, and a fourth branch (see link below) has been proposed.
Check out Immobilized by ME/CFS or FM? The Polyvagal Theory
The SNS primarily uses epinephrine (adrenaline – produced by the adrenal glands), norepinephrine, and dopamine to do its work, but Martinez-Lavin calls the last two the true sympathetic transmitters. The PNS, on the other hand, primarily uses acetylcholine to do its work.
Stress Redefined
Martinez-Lavin redefines ‘stress’ as we ordinarily know it when he notes that, from the body’s perspective, the simple act of standing – moving the body from a resting position to an upright position – is a stressful act. During that act the ANS takes many actions to keep gravity from driving our blood into our feet and out of our head. The fact that most people are able to stand without any issue at all doesn’t mean the act of standing is not inherently ‘stressful’ to the body. After all even a healthy person has trouble standing still for long periods of time.
Portraying standing as a ‘stressor’ helps us redefine our notion of stress. ‘Stress’ is anything that takes the body out of it a restful, inactive state.
Digestion, then, is another stressor – one that very well demonstrates the yin-yang nature of the ANS. When activated, the ‘fight/flight” branch of the ANS, the SNS, inhibits gut movements and gut secretions in order to provide energy for more immediate concerns. In turn the ‘rest/digest’ (PNS) branch promotes peristalsis and gut secretions once the SNS quiets down.
Given that the ANS regulates basic aspects of our body’s functioning, it’s not surprising that it in turn is regulated by the organs lying deep in the more primitive areas of the brain that are responsible for some pretty primitive responses.
Because the fight or flight system is responsible for removing us from danger, it needs to have
- a lightning quick response, and
- a straight shot to those areas of the brain that will produce emotions that make us move and act quickly; i.e., those parts of the brain that produce emotions like fear and anger which propel us to quick action in the face of danger. The ANS, Dr. Martinez-Lavin believes, is the interface between the mind and body.
A Holistic Approach to Fibromyalgia
“Our working hypothesis was that every manifestation of fibromyalgia could be explained by an alteration in the autonomic nervous system.”
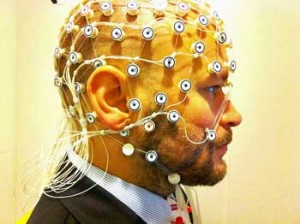
Dr. Martinez-Lavin believed it was possible that every aspect of FM could be explained by autonomic nervous system problems. He began assessing ANS functioning through the use of heart rate variability analysis – a means of determining ANS functioning.
EEG studies suggest the brains of people with FM and/or ME/CFS never really ‘rest’ when they’re asleep
His studies revealed people with fibromyalgia had an ‘incessantly hyperactive sympathetic nervous system” that was particularly hyperactive during sleep.
Paradox
But a paradox emerges when we dig a bit deeper. Constant sympathetic nervous activity should stimulate the heart and put the squeeze on our blood vessels, resulting in high blood pressure – which is rarely seen in either FM or ME/CFS. Instead, low or lowered blood pressure is the norm.
How does one explain low blood pressure in disorders characterized by a hyperactive flight or flight response? By the ‘cry wolf’ syndrome. In the face of a system which has apparently been stuck continuously on – crying wolf all the time – the body simply begins to ignore the signal by turning the receptors for the SNS off. That causes the blood pressure to slide instead of increase.
Asking FM patients to stand up after 15 minutes of lying down also revealed that their sympathetic nervous systems – which are turned on during ‘rest’ – under-responded when prompted to respond during standing.
Dr. Martinez-Lavin suggests that having the SNS essentially ‘on’ all the time has burnt it out. That sets the stage for constant fatigue and, of course, poor sleep and feeling ‘beaten up’ and tired upon waking.
Martinez-Lavin’s next step was particularly interesting given the Stanford ME/CFS EEG studies soon to be published. His EEG studies found high levels of ‘startle’ and awakening in his sleeping FM patients. (The Stanford EEG studies will suggest people with ME/CFS are in a kind of sleep mode when they’re awake and vice versa.)
Dr. Martinez-Lavin believes that sympathetic nervous system hyperactivity is essentially ‘startling’ people with FM into poor sleep. Poor sleep, by the way, is highly correlated with increased pain sensitivity, even in healthy people.
A Common Theme Emerges in the Pain and Fatigue Disorders
We know a similar kind of SNS hyperactivity is present in ME/CFS, but it’s also present in two other mysterious pain disorders: irritable bowel syndrome and interstitial cystitis (IC). All have similar heart rate variability findings, and people with these disorders display a similar SNS collapse when faced with stressors.
IC is characterized by burning and pain when urinating (but no sign of infection). Because IC, in contrast to ME/CFS and FM, has a localized occurrence, it offers a window into its pathophysiology that ME/CFS and FM do not. Increased epinephrine (adrenaline) levels in the urine and increased sympathetic nervous system fibers in the bladder wall appear to set the stage for a twitchy, over sensitized urinary system in that disorder.

Dr. Martinez-Lavin believes that being ‘on’ all the time has caused the sympathetic nervous system to ‘burn out’
The same Th1/Th2 immune system imbalance (Th1-low/Th2-high) that appears to occur in ME/CFS also appears to be present in FM, according to Dr. Martinez-Lavin.
Sympathetic nervous system hyperactivity tends to inhibit the Th1 (antiviral) branch and upregulate the Th2 (allergy, bacterial defense) branch of the immune system – precisely what’s seen in ME/CFS and FM.
Martinez-Lavin is even able to tie in the gender imbalance with ANS dysfunction. Women, he reports, tend to have a ‘higher basal sympathetic tone’ than men, and after trauma tend to develop more ‘irregular connections’ between pain pathways and the sympathetic nervous system.
Conclusion
Dr. Martinez-Lavin believes the autonomic nervous system is ground zero for FM. Not many would go that far, but the ANS clearly plays a role in both FM and other pain and fatigue disorders that mostly plague women.
We haven’t gotten to the heart of Martinez-Lavin’s hypothesis that SNS overactivation is key in FM, however. That’s coming up shortly as we watch him dig into the very nerves that are responsible for pain in Fibromyalgia.
By opening and closing blood vessels it determines which organs and tissues are going to receive blood.




 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



I think this fella is full of it. I contracted fibro/ibs/tachycardia within hours of exposure to toxic chemicals in a home product. This particular issue is not confronted by this website.
We don’t have a lot on toxic chemical exposures and FM/ME/CFS etc. As someone who has had to battle chemical sensitivities for over a decade – that’s unfortunate In fact we have almost nothing – and could use some help there if an interested blogger is out there. An interview with Dr. William Rea is planned 🙂
Surely if it is stressful to just stand, image what toxic exposure would do to the functioning of the ANS. (The explanation for this goes down to the level of the mitochondria and the CYP 450 enzymes that detoxify the body. Both cortisol and these enzymes make demands on pregnenolone production). Dr Martinez-Lavin cites infection as a cause but surely this is just anther environmental stressor as opposed to internal stressors. The most important point being that the weakness to succumb was already there. It has been documented, at least in FM, that we have dozens, if not 100s, of SNPs (polymorphisms) in common. Kira brought our attention to the COMT gene in the first part of this series. This is a very important gene for us as it deals with dopamine metabolism. Dopamine competes with adrenalin for its production which would explain low dopamine levels in the illnesses brought about by an overactivated SNS. We also have a serotonin transporter polymorphism which is why we have problems with mood, sleep and digestion. I firmly believe that genetics play a very major role and that gene expression varies greatly amongst our common polymorphisms, resulting in different symptoms in each individual ( hence the sub-sets). The fact, for example, that studies have shown that other members of a family of a person with FM also have the same COMT polymorphism but with a different expression, leads one to think that it may just be hereditary after all.
Looking forward to learning more about COMT. I’m pretty sure its been implicated in ME/CFS as well.
The link below is to a study that confirms this. I’d forgotten I had record of this study which also claims to be able to differentiate genetically between FM and CFS/ME. A very complex study though and difficult to understand.
http://www.institutferran.org/documentos/estudio_genetico/JCR%20106%20140408.pdf
Cort, you mention that high blood pressure is “almost never seen” in ME/CFS. Despite it’s infrequency, can you direct me to any
information or resources about HBP in ME/CFS?
I don’t have any. I must say that I’m sure that it occurs given the amount and variability of autonomic nervous system problems in ME/CFS and FM, if not the heterogeneity in the disorders themselves.
Thanks Cort. I will continue to search as I tend toward high blood pressure. I’d used caffeine, and still do a bit, to function till the blood pressure issue caught up with me!
Thank you too for this website – I often gain insight and hope from the information you provide and so appreciate that!
This makes a lot of sense to me, perhaps since it fits my particular case of ME/CFS. I have low blood pressure and dysautonomia issues such as orthostatic intolerance, common to ME/CFS. I have had the tilt table testing done plus additional autonomia/syncope workup done by a cardiologist in which they tested for things such as alpha and beta adrenergic sensitivity, intrinsic heart rate and catecholemine levels while undergoing tilt testing and cardiac blockade. I had a few abnormal results one of which was decreased alpha adrenergic sensitivity, exactly what this article is talking about. My alpha activity test itself was normal. Basically when they injected me with phentolamine (after performing a cardiac blockade using atropine and propanolol, then starting phenylephrine) my BP didn’t respond as it should have. It was reduced, or blunted.
I wish all ME/CFS patients could get this level of testing done and then we would have a lot more detailed information about ourselves and wouldn’t have to guess or assume that we might have these issues. I live in Canada and was very fortunate to be able to get into the Syncope/Dysautonomia Clinic at the Hamilton General Hospital via Dr/Hyde. Plus it would give more credence to theories expressed in this article and would go a long way to educating people (like physicians) about this illness. I try and get every test I can possibly get done and now have a binder full of evidence backing up my illness that I can carry to to new doctors for show and tell 🙂
Claire
Thanks again Claire for sharing your experience. The autonomic nervous system is something that the medical community is only slowly getting a handle on.
This was fascinating: “one of which was decreased alpha adrenergic sensitivity, exactly what this article is talking about”.
I wonder if the SNS is turned down if the adrenergic system will adjust back?
I hate to be the “odd man out” here but: as I have mentioned before, I have been taking Vyvanse for several months now which has increased my pulse rate. More than this; Vyvanse controls the norepinephrine in the brain. As a result of this treatment my: pain, fatigue, sleep disorder, bipolar and executive function problems have literally disappeared.
Again, as I have mentioned, I was disabled by these problems to the utmost degree. I was unable to read anymore as I could not absorb information due to the executive function problem. I have been reading every one of these Health rising posts and even taking notes along with anything else significant on the internet.
Dr. Martinez-Lavin has brought forth information in this article that is the most identifiable to me of all. As a child I grew up with severe IBS. As a teen, I found out I had low blood pressure. People in my family (myself included) tend to have almost too much energy, sleep problems, difficulty gaining weight due to stress and disorders involving norepinephrine.
It wasn’t until the FM took over that my energy went way down and all the other problems continued to get much, much worse. I have been searching for an answer as to why the Vyvanse has worked so well. I do believe what the good doctor is working on is right along those lines. I’m no doctor and I certainly don’t presume to know all but there is a reason why I went from a disabled person to a completely healthy, energetic and capable human being again.
I do, of course, understand that there is now more damage that has been done due to my years of sitting, laying and literally no exercise of both my body or brain. This is why I continue to read and take notes. I am now: doing stretches and exercise, changing my diet and taking supplements to further heal my body and mind. None of this would be possible though if I hadn’t started on the road to recovery by taking the Vyvanse which, to me, is obviously working on the problems that have been there for a lifetime.
That’s amazing – and congratulations!
For those interested in Vyvanse – check out a blog we did on it last year – http://www.cortjohnson.org/blog/2012/12/28/26/
I don’t see how stimulants can work long term, what with our problem of post exertional fatigue. Seems you’d be playing with a loan shark so to speak.
SNS overactivation is the key problem for ME! But what drives this overactivation? That is the big guestion. Compensation, infection, defect? I think the PNS is defect, that is my view for almost 2 decades now.
Cort, can you ask this doctor what causes this overdrive in his view? Thanks!
Good idea Gijs…..
I’ll bet you are right – I’ll bet it is defective PNS…the vagal nerve
Wouldn’t it be great if we could all get genetic testing to see for certain which CFS subset we fall into? Then we would know with more certainty where our weaknesses are, which medications, herbs, supplements would help. It could tell us what to avoid as well, perhaps help identify nutritional recommendations for each individual, some way to work around defective genes. I love being able to get on a website like this and finding someting new to try. Since different things work for different people, genetic testing could be a way to figure out what works for the individual, and should save money by not having to spend it on things that probably won’t work.
Julie Saunders
That is absolutely amazing about the Vyvanse having had such a profound positive effect on your fibromyalgia symptoms. It does seem to correlate well with this article and opens up many questions and possible avenues to explore. Thanks for sharing!
I don’t know if you’ve covered changes to the endothelium of blood vessels or arterial wall stiffening. One of these studies cited another which says stress and the catecholamin(adrenal hormones: dopamine, epinephrine & norepinephrine) also affect the endothelium. I had not read that FMS patients would tend toward low blood pressure. I would suppose high blood pressure and arterial stiffening would be an unfortunate combo pack eventually.
https://www.healclick.com/posts/10727-fibromyalgia-and-endothelium-changes-including-wall-stiffening
Enjoyed your comment Claire. I live in Hamilton but got no help when I saw Dr. Hyde. Individual resourcefulness, such as yours, is still to be valued, like Cort’s contributions, while much of medicine’s practitioners are confused.
Hi
In 1977 I was thrown into a brick wall and my skull connected with the brick windowsill causing a slight dent. This caused my body to go into permanent ‘flight/fight’. I was diagnosed with chronic fatigue around 20 years ago and although I seemed to get past that, three months after I was operated on for a ruptured appendix in 2002 I started experiencing pain throughout my body and the use of one arm became very limited. Joint and muscle pain could also become quite severe at times. The Doctor diagnosed fibromyalgia. Since I react to most medications including pain killers, I decided to look for alternate methods of treatment. I was seeing a Chiropractor who used ‘Applied Kinesiology’. I put the problem to him. Although blood tests had shown my T3 to be normal, he targeted the thyroid as, since I had numerous symptoms indicating a problem with the T3 he thought that I had ‘Reverse T3’. Using Kinesiology, he tested each chemical involved in the process of converting the T4 to T3 and discovered that I needed Ionic Molybdenum in order to enable the T3 to do its job. To this day, I am taking the Ionic Molybdenum as most of the symptoms disappear with its usage. If I don’t take it, the pain and a range of other symptoms, come back. Over the years, as an alternative, I tried Thyroxine, (both the synthetic and the natural) but it didn’t help. It would seem that the impact of stress caused by the dent in my skull (which I cannot change), in my case at least, makes it impossible for the T4 to convert effectively to T3.
I hope that this information is helpful.
Amazing story, Joan. It’s really something that your T3 seemed to be normal but was not and that thyroid meds did not help and you had to go deeper and when you did – it worked. Thanks for sharing.