



“The objective is to deliver relief as quickly as possible but to keep working on the problem until we find a cure.” – Gordon Broderick
Dr. Gordon Broderick of Dr. Klimas’ Institute for Neuro Immune Medicine at Nova Southeastern University (NSU) was in a loquacious mood. He likes what he’s seeing from his working group and from the field in general, and as we wandered from NSU poster to poster at the IACFS/ME Conference, he was happy to talk about it.
Defining Moment
He’s an interesting guy with a more than interesting approach to Chronic Fatigue Syndrome. He got into the field with the CDC and their big Pharmacogenomics study, but when that work wound down and he was having trouble getting funding, he was about to leave the field.
That changed when he bumped into a Gulf War veteran at a conference in Reno. A big man, probably 6’4″ and 280 pounds, strode rapidly up to him — eliciting alarm in the short and slight Broderick (“I thought he was going to snap me in half and send me home in little Glad bags”) — grabbed his hand, and tearfully thanked him for believing that he was sick.
Probably many professionals who work in this field have defining moments when they decide that no matter what the difficulties they’re encountering, no matter how much working in ME/CFS makes their own lives more difficult in so many ways, that this is what they must do… and this was Broderick’s defining moment. He said he could remember as if it happened yesterday.
Broderick has a unique approach to Chronic Fatigue Syndrome. A master at mathematical modeling and data mining, he analyzes enormous amounts of data to learn how systems work. He and his team use the data they find in the medical literature to produce engineering models of how the system works. Ultimately patterns emerge which show different stable modes of operation, some of which constitute good health and others that reflect chronic illness.
Chronic Illness … er, “Impaired Homeostatic State”
“Illnesses such as these continue to defy a conventional one-piece-at-a-time approach.”
Broderick believes chronic illnesses such as ME/CFS and FM, autoimmune illnesses, diabetes, etc. involve a kind of ‘homeostatic reset’ that enables the body to survive but also includes a kind of ‘stuckness’. Chronic illnesses, in other words, are chronic for a reason. If Broderick’s right, it’s possible that every chronic illness reflects a homeostatic state that is resistant to change.
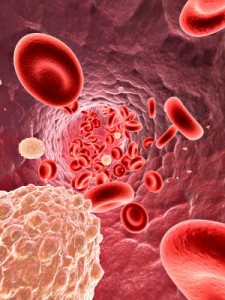
With the computational power and methods available now, it’s not just about NK cells or T-cells — it’s about how NK and T-cells and B-cells and hormones all work together to produce a disease. You still need the data on NK cell problems because that informs the model but the big picture is coming from the computational end. In fact Broderick would argue you’ll will never understand a complex disease like ME/CFS unless you look at it in it’s entirety – and that means modeling it.
That approach leaves some traditional researchers agog. They don’t the background to understand it and they don’t trust it. There’s simply too much data, too many places for something to go wrong (and too much math) for them to sign on. The NIH, on the other hand, has signed on. Broderick’s one the few ME/CFS researchers able to regularly obtain grants.
Others are starting to take notice of the NSU team’s work. The team has presented several talks to the Nationstal Cancer Institute. The breast cancer community is interested in the hormone/immune model Broderick is developing, and no doubt others will follow.
Pragmatic Approach
“We’re an embedded systems biology group. We’re applied scientists.”
Broderick’s approach with his complex computational algorithms seems ivory-towerish, but it’s all in service of a very pragmatic vision. He noted that he comes from a corporate background where investors have limited patience; they demand results, and he’s big believer in incremental results. He’s looking at both the big and little picture: the NSU team he’s a part of is focused partial relief today – or at least soon – for people with Chronic Fatigue Syndrome while they continue to peel back the layers of the onion and get at the source.
Finding FDA-approved drugs that can treat symptoms now is a major concern. If some people with ME/CFS, for instance, share similar inflammatory pathways with rheumatoid arthritis, then it makes sense that they should be given a chance to be treated with those same RA drugs. That means working on validating treatments for repurposed drugs, such as TNF-a blockers or drugs that are under development. Dr. Fletcher has repeatedly called for FDA trials NOW.
The Physicists Come to the Fore
Broderick is what used to be called a “Renaissance man,” and today is called a “polymath.” He followed up his PhD in chemical engineering with post-doctoral work in computer science and biochemistry. This unusual combination makes him uniquely qualified for development of sophisticated mathematical models of biochemical systems. (His eclectic background brings to mind another ME/CFS researcher breaking boundaries – Dr. Kogelnik of the Open Medicine Institute – and his fusion of biology, bioinformatics and computer programming).
Travis Crawford, his associate at NSU, has a Ph.D in biophysics and did post-doc work in systems biology. Broderick said physicists are all over medicine now. It’s not that biology is gone – this is like biology on speed; it’s biology that takes the dynamic interactions of the body into account. This is where biology uses physics, mathematics, and engineering in an attempt to reproduce what’s going on inside living systems.
Crawford said, “There’s nothing more fascinating or a bigger challenge for a physicist than an ‘open self-regulating system’ like the body.” Living organisms are more complex than anything they’ve taken on before, but now they believe they have computational methods to tackle them.
They believe that you can attempt to compensate for the new homeostatic state with treatments, but until you can determine what’s keeping that system in place, it’s going to remain in place. Once you do determine the factors holding the system in place, though, and treat them, the system should be able to return to its normal homeostatic state; i.e. health.
It’s a very different approach to illness. Calling Chronic Fatigue Syndrome the “New York City’ of chronic illness (if you can make it here, you can make it anywhere) Broderick believes demonstrating his approach works here will lead to its being adopted in other disorders. ME/CFS is a hard nut to crack, he said, and if you can crack it in a relatively short period of time with a relatively small budget – as he believes he’s on the way to doing (he really does) – that will lead to opportunities for treatment of other disorders, particularly neuroinflammatory and neurodegenerative ones.
Redirecting Systems
“Our eventual goal is not only to tap into pathogenic immune conversations but also more importantly to re-direct these conversations with a limited number of well-chosen and well-timed pharmaceutical messages”
The Institute team is building three models of neuroinflammatory disease: toxin exposure (GWI), infectious event (ME/CFS), and traumatic brain injury. Taking the system dynamics into effect has at times led to some counter-intuitive options.

Don’t try this at home! An early model suggested depleting the system completely of cortisol could cause the system to reset itself
The first model, a simple one produced at the CDC some time ago, suggested that the way to get out of the low cortisol problem was to reduce cortisol even more. Their model indicated that briefly sopping up all the cortisol in the system with a binding element would result in what Broderick called a slingshot effect, causing cortisol’s trigger, ACTH, to build up and catapult the system into a new dynamic. Nobody to my knowledge has ever tried this in a human being.
The Institute team’s approach is to use these models in association with the exercise studies to design interventions that occur in time. First, you give an ME/CFS patient X intervention to nudge the system in right direction. Then, as parts of the system reset themselves, another intervention is added to nudge it further, until the patient out of – or at least partially out of – the homeostatic state of illness they’re stuck in. The models will help them figure out which interventions to use, in what order, and at what time points to give them.
Low testosterone levels could be one example: you can flood the body with testosterone, but once you stop doing that the levels plummet again. Something is sapping the system of testosterone. Viruses and immune factors are clearly part of another homeostatic issue for some people with ME/CFS. Some people with ME/CFS can return to health with antivirals or immunomodulators like Ampligen, but most relapse after they stop taking the drug. Broderick isn’t just interested in getting rid of the pathogen; he want to know why the pathogen is there in the first place.
The modeling has been an evolving process. First they modeled the peripheral immune system. Adding the endocrine system demonstrated how different men and women are, and added another field of inquiry. They’ve found that women’s sex hormones (and men’s) strongly affect inflammation, fatigue, cognitive issues, and mood. High estrogen levels appear to push the HPA axis of susceptible women out of whack and into a alternative homeostatic state. Unless it’s low – which often happens in ME/CFS – men’s testosterone protects against HPA axis problems.
“A Fire in the Head’ – Neuroinflammation – A New Direction
Next up is the brain. Taking advantage of a new neuroimaging center opening up at the Univ. of Miami, the NSU team is moving into neuroimaging and neuroinflammation. They’ll build on their previous models of peripheral inflammation and tie them to neuroinflammation in the brain.
Ultimately they should be able to determine what happens in the brain after you introduce a factor – a pathogen, toxin or drug – into the peripheral immune system. That ‘factor’, of course, is the environmental trigger that sparked ME/CFS.
Broderick is particularly fascinated by what role the vagus nerve, the object of much interest in ME/CFS, will play in the model. Broderick called the vagus nerve’s role ‘fascinating’. He likened the vagus nerve to the immune system picking up the phone, calling the brain, and saying, “Boss, we’ve got somebody on board – start the emergency protocol”
It’s not just the body talking to the brain, though; the brain talks back and regulates the immune system as well. The lymphoid organs send information to the brain, and the brain regulates their functioning as well. Broderick likened the immune system in the body to the ‘commander on the ground’ communicating to the rear command (the brain).
Broderick is quite confident in his models. The peripheral immune model has been run so many times and in so many circumstances that he believes it’s solid; the core is complete. The sex hormone and immune model he called a ‘pilot analysis’ but stated it provides a strong basis for understanding.
“Interface Points” for Change Pop Out (Thankfully)
‘(This) structure is very amenable to intervention.’
When first seen, the visual representations of Broderick’s networks – a mass of different colored lines seemingly darting through each other randomly – seem unintelligible until he points out what they mean. The internal parts of the maze are neuroimmune factors; surrounding them are single points – the key symptoms – general fatigue, reduced activity, depression-caused fatigue. The lines connecting the symptoms to the neuroendocrine factors indicate which factors are producing the symptoms.
Both Broderick’s and Younger’s work suggests single interface points may affect many factors in the body
In every case, a key factor has popped out of the maze to provide a target; i.e., the factor which, if properly targeted, should be able to erase or reduce the symptom. If the model’s prediction is correct, this is a key and very promising finding.
Broderick has dozens of factors in his model. Pain, for instance, could have been mediated by 10 factors; fatigue perhaps by 7 or 8. If that was the case, finding treatment options would have been more difficult. Instead, just a factor or two emerged for many of the major symptoms of the illness.
Broderick calls these key factors ‘interface points’. A lot of interactions occur to produce them, but they are key producers of symptoms.
It’s these interface points that appear to give Broderick assurance that the ‘structure’ of ME/CFS appears to be amenable to intervention. Broderick didn’t say that the treatments to do that were present right now (or that they weren’t present). The thing I took away from our talk is his models do not suggest ME/CFS is a horrid mess. They suggest ME/CFS is understandable and ultimately treatable.
For instance, fatigue and depression appear to be largely mediated by IL-17. Il-4 is another key factor. IL-2 appears to be highly involved in producing mental fatigue. If you affect IL-2 you should be able to increase mental endurance.
Dr. Jarred Younger at Stanford found a similar pattern in his “good day /bad day” study. His network charts looked very similar to Broderick’s: a mass – really more a mess – of complex interactions that made their way back to one factor (leptin) which correlated with fatigue in ME/CFS. Younger’s approach was different; he focused on one symptom – fatigue – and examined more immune factors and watched them over time. The NSU team focused on many symptoms, examined fewer immune factors, and did not watch them over time.
Nobody, in fact, in the ME/CFS field appears to have looked at leptin until Younger did. Younger, by the way, just got a major five-year NIH grant to dig deeper into his leptin and ME/CFS findings. He’ll reprise his “good day/bad day” trial with a much larger group and more factors.
The NSU and Stanford groups are demonstrating that ‘big data’ projects can identify targets that may be relatively easy to manipulate for better health. Broderick noted that the ‘structures’ his work has identified appear to be ‘very amenable’ to intervention. That’s potentially very good news for a disorder that doesn’t seem to be very amenable to much.
NK Cell Mystery Solved
Decreased natural killer (NK) cell functioning has been a key immune finding for ME/CFS – a consistently reproduced finding – until the NIH-funded Katz study found no problems at all with NK cell functioning. Broderick couldn’t figure this out until he got Katz on the phone and dug into the details of the study.
It turned out that Katz had isolated NK cells and then tested them, while the Klimas team always tests them in whole blood. The light bulb went on. Something in the blood was axing the NK cells. Put the NK cells off by themselves and ask them to kill pathogens and they do just fine – but put them in the blood mixed with all the immune factors found there and they poop out.
This fits Broderick’s network approach to the immune system to a T, and possibly makes the problem more amenable to a solution. Instead of fixing the natural killer cells, you may simply have to find out what factor, what cytokine, what immune mediator is turning them off, and block that.
______________________
The Klimas team at the NSU Institute for Neuro Immune Medicine easily had more posters at the IACFS/ME conference than any other research group. With modeling efforts underway and with their eyes on repurposed drugs and on identifying new drug targets hopefully we’ll be seeing papers with clinically-applicable results stream out of her group over the next couple of years.











If Broderick sees “structures” that are “very amenable” to treatment why aren’t we hearing from patients out of NSU reporting of greatly improved health, reading papers of new treatments for our many ailments?
Theories are great, but they’re just that until they actually produce something.
I think it’s a work in progress. Working out how to move ‘the structure’ around; i.e. what treatments to do in the right order etc. will take time. It may even be that the right treatments have not been developed yet, but that the structure of ME/CFS is relatively simple and thus appears to be amenable to developing interventions to alter it.
We shall see!
”the structure of ME/CFS is relatively simple”, Simple? 🙂
Just imagining other disorders and how the protocol is step-by-step. Even with HTN, different meds are attempted. And new onset of Type I Diabetes requires even more “layers” of blood sugar adjustment to hit on the right dose for a particular individual. And they don’t start with short-acting insulin when trying to stabilize someone. Just seeing some similarities when it comes to protocols for treatment….
I know from my own medical history of scans and tests that I have neuro-inflammation and fall under that model. Given what you’ve reported Cort, does that mean I should be flying down to be studied by Broderick now?
I don’t know that they’re using patient data to put the neuroinflammation model together. I think they’re using study data. Once they put the model together I imagine they would apply it to individual patients. This is all guesswork on my part, though. 🙂
Exciting stuff,Cort. That’s just what we need- people thinking outside the box.
These guys are reinventing the box – that’s for sure. It’s a whole different way of looking at disease. They seem very confident.
We were thrilled when Dr. Broderick joined Dr. Klimas and the incredible team at NSU. We know how much time and energy these individuals put into finding treatments and hopefully, a cure for us and we are very grateful to them. As a patient of Dr. Klimas for many, many years, I’d like to remind each of you how important it is for you to volunteer for research studies whenever the opportunity arises. The researchers can’t find answers without patients volunteering for studies. Know that you may be a small piece of the puzzle that can make a difference in the big picture. Don’t hesitate to volunteer if you are asked.
Indeed, patient recruitment is apparently the most expensive and difficult part of a study…(who knew?)
I have been a patient for over 20 years at the Klimas group. I am now being told that at age 70 I cannot volunteer for any studies. Just praying for a treatment to work and get approved before it’s too late for me. 32 years of this disease is wearing me down to the point that I almost never leave the house and prefer being in bed to doing anything else. My disease was instant turn on during a C-section that I was given way to much epidural because I just could not dilate. So far nothing really has helped me, but I will stay hopeful and continue going to Nova and seeing Dr. Rae, whom works with Dr. Klimas and wait for the cure.
Good luck Sheila. May those studies you can’t get into point the way for you.
That’s really something about your onset. There are so many different ways to get this disorder started.
You NEVER know what the future will hold – truly.
I am 71 and I understand. I simply had to look outside of traditional medicine last summer. My pain and chronic fatigue from fibromyalgia was ongoing and the meds and otc drugs all had “mean” side effects. I read a most wonderful book recommended to me by my massage therapist, Healing Oils of the Bible by Dr. David Stewart. Since then I have been using pure therapeutic essential oils. I have not taken any drugs since I started using the oils last October. I suggest you do your own research and investigation. I don’t blame the doctors, I just know they are only applying what they have been taught in medical school and pharmaceutical companies. They are shackled by money and government restraints. I invite you to visit my FB page: Redeeming Health Solutions.
My best wishes for a hopeful future. We have a lot to give to the world.
Cheers,
Margie Barnes
HI I WOULD GLADLY GIVE MYSELF FOR RESEARCH. I AM 47. AND I HAVE EVERY SYMPTOM EVER MENTIONED WITH FIBROMYALGIA AND AM CERTAIN THAT I HAVE CFS. I AM GETTING WORSE ALL THE TIME. I NEED HELP. I LIVE NEAR PHILADELPHIA PA. THANK YOU FOR CONSIDERING ME IN YOUR RESEARCH AND INTERVENTION TRIALS.
SINCERELY,
DEBRA J HANGE
Hi Debra. My Name Is Julie Saunders. I Live In Brantford Ont. Canada. I Am 48. I Was Completely Dissabled By All Of The Symptoms Mentioned In This Site As Well. To Top It Off, I Have An Adult Son Who Is Severely Dissabled bY Something Completely Different And Depends On me For All His Needs. I Was Desperate, Tired And In Unbelievable Pain. It Looks Like You Are The Same. I Keep Writing About Vyvanse. It Has Saved Mine And My Sons Lives Together. The First Day All Major Symptoms Went. Pain, Fatigue, Mood, Waking Through the Night. I Had My First Good Nights Sleep In Years. I Have Been Able To Concentrate Again, Enough To Actually Read These Posts. I Have Been Studying ever Since And Am Now Riding A Bike, Stretching, Changed My Diet and Keeping My Thoughts Positive Which Is Pretty Easy Since Im Better. Someone looked At The Muscles In My Arms The Other Day And Said “I Wouldnt Want To Mess With You”. Lol! I Am Hoping That Ultimately I Will Get Off This Medacine Too. For Now, My Codiene phosphate Pills Are Down From 8 A Day To 3/4 Of A Pill A Day. Please Ask Your Doctor To Try It. If Indeed We All Suffer From The Same Dissorder, This Should Kickstart A Healing For You As Well. God Bless.
SO, something in the blood is toxic to immune cells? Effecting much more women than men?
What do women deal with much more than men?………….. CANDIDA TOXINS!
For thirty years I’ve been crying, we need a Candida Toxin Neutralizer! RP
Regarding Candida and its toxic byproducts: Those who have been using integrative methods to manage symptoms better or resolve them altogether have had success of varying degrees over the last 30 years with powerful probiotics, abx avoidance/repairing “leaky gut,” Chinese herbs/acupuncture, homeopathic remedies of varying approaches, diet changes and energy medicine modalities. MDs and other practitioners prescribe these, or else the patient undertakes the treatment independently: They could not wait for orthodox conventional medicine to address this. Now that more researchers are thinking more out of the usual constraints while Eastern and Western paradigms partner, there is no telling how many creative, successful, and affordable approaches to healing NID will present themselves. –As long as Big Pharma and the FDA are not successful in banning 30,000 natural supplements and co-opting them into chemicalized, patented prescription-only meds affordable to the few. Though this last comment is somewhat off-message, people who depend on supplements should know that their access is being threatened at this time as never before. Action is required by those who want to keep their free access to the very safe supplements that the NSU pioneers, for one example, recommend for their effectiveness. At least we have these food supplements as a partial NID solution for now.
New…and not new. I think many of us are aware that CFS means that ‘something has pushed you over the edge’ and now a number of your systems are out of balance, to the extent that your body does not have the ability to get itself back ‘into balance’ (a healthy homeostasis).
Pretty much all the people I know who got better, worked at helping one or more of their systems – hormonal, immune, energy etc. – ‘back on its feet’, eventually creating the condition where their body could do the rest of the job. So, it’s nice when models confirm what we know, and maybe provide new ways to tackle the challenge – but this will not be the one and only path to recovery.
Agreed. In this disorder there can only be numerous pathways to recovery….It’s too heterogeneous for anything else to be true.
Thanks, Cort, for putting out this information. It’s apparent that you put alot of effort into these write ups. I find it encouraging that research like this is going after the very essence of what has gone wrong in our systems.
Thanks Greg
so he thinks it’s amenable to intervention but I don’t see any suggestion that they have yet identified where to intervene, or what the interventions might be. Too optimisitc a tone for me, Cort. SOunds like a researcher’s puff to get more grant money
🙂
There were those immune factors that appear to be able to affect key symptoms but the future will, of course, tell about how close anybody is to understanding and treating this disorder.
It always takes longer than one would hope, that’s for sure.
Fascinating, Cort!
Did he identify any factors related to orthostatic intolerance? That’s a major issue for many of us. Prof Julia Newton thinks (I believe, unless I’ve misunderstood) that OI, when provoked, can drive a lot of our other symptoms. She has patients do a tilt test and their ME symptoms pop up, not just the classic orthostatic symptoms.
I don’t think he’s looked at OI…He’s plugged in a variety of symptoms in his model but I don’t remember OI being in there. I could be wrong though…
I don’t remember a lot on the ANS either come to think of it. He’s been focusing on more immune stuff but the ANS (which is an immune regulator) clearly will come into play. Dr. Klimas, after all identified that neuropeptide Y, an ANS regulator, as a possible biomarker in ME/CFS. She also believe ANS problems during exercise kick off an immune cascade…. (I wish that paper would come out :))
Greetings all. The amount of info to deal with in any chronic illness is massive, and it really needs modelling and reliable ways of dealing with mass data. Good on these folk for giving it a go, and I look forward to what comes up, whatever it is. I think the Tricorder diagnostic tool is getting much closer with this step. [Serious, but said lightly]
Thank You, Cort!
Every time I hear about a dedicated doctor who is committed to finding a treatment/cause/cure for ME/CFS, I rest a little easier. ME/CFS requires only those doctors who are willing to run into brick walls. It sounds like Dr. Broderick is just such a person and is up to the challenge. As patients, we are not alone. Dr. Broderick thinking “outside the box”, conferring with other doctors and bringing in a physicist — what an awesome collaboration! Good things might very well come of this. Thank you, Dr. Broderick.
As we have hopefully all realized that this is not a one system disorder but rather the interactions of our endocrine, neuro, and immune systems, I would say as a layperson that Broderick is indeed on the right track. I’ve often wondered myself if my system could be “shocked” into a re-boot such as he envisions by, for example, taking all the cortisol away and hoping that the cortisol-producing hormone ACTH will then kick in and begin making it’s own supplies once again. And his observation that NK cells must remain in whole blood with all the antigens and immune dysfunction to show a lower count. As well the cytokines involved in certain areas such as fatigue, mental fatigue, and the like. To have I.D.’d WHICH ones are involved as has already been demonstrated…. and to put it all into a mathematical computation that would blow us all away to reach all the interactions…. dude’s got my vote. M
Well Said Marcie. I Agree. This Kind Of All Around, mathematical research Is Definately key.
Destroying all the cortisol sounds a bit dangerous to me as it is essential for life. What if the production doesn’t kick start as hoped? Walking a fine line, I would say. Also, one study done reveals normal ACTH output but a blunted cortisol response from the adrenals so it would be the adrenals that need kick starting.
Dr Broderick is no doubt a very promising figure here, but I must say I also really like the idea of a physicist jumping in! I am curious to see what Travis Craddock’s contribution will be… Modern medicine breaks down the body into parts, and we know ME/CFS requires a view of it as a whole, and that is how a physicist can only view the body from the start, – a little “cosmos” where everything interacts! And where energy is to be transformed…I have a hunch that someone who deeply “gets” the laws of thermodynamics can have a very unique perspective on energy production issues and homeostatic issues in our illness…
Ha! Yes, the thermodynamics energy production link – hadn’t thought of that. 🙂
I find this article a great source of hope. I’ve always believed that it’s the interaction of different malfunctioning body symptoms that causes ME/CFS. My approach has always been to do everything I can to take the pressure of each system and hope that the body finds a way to reset itself. It worked for me once but hasn’t yet this second time. I’m excited that one day there might be some treatment that can work as a reset button!
Thanks for bringing us more hope!
Desire a study with the timing of the onset of this disease with what technologies were taking place same time in our culture.
Suggestions: microwave ovens, fast food, electronics going through our bodies, pollutants, changes in how we get our food supply, artificial foods, climate chage bringing on more pollution, especially water and air. What unnatural components came into our homes like what our homes and furnishings have in them.
Compare state of tech, chemical, etc. Was in place before this disease. Compare our environment, new meds, long list of what entered into contact with us when we started these symptoms.
Map out areas to demonstrate concentration pockets of this disease; and what do these pockets have in common from before and time this epidemic started.
Again, keep in mind what has occurred with other life forms on our planet during this same time block. Can only think of drop in bees, deformed frogs.
Can our tearing up the forests be a contributor, oil spills?
Scientists should be on the top of who is investigating.
Recycling so much plastic, our overflow of garbage. The radioactive material we buried??
Gasoline, car exhaust, goes on and on.
Study healthy people and the differences in their living conditions. Compare.
Are we being poisoned in any way?
Look at the drastic change that has happened to our human relations.
Women’s lib in 1960’s, birth control, family life deterioration, both parents working. Single moms getting by on anti- depressants, media total wave, people lacking support systems, relatives scattered all over, mechcanization of man.
No conversation face to face, use email. Mothers can’t reach their kids let alone keep their families together. Neighbors not as social. We have been pulled into emptiness with our electronics.
We are islands trying to survive on our own. I feel like we got sucked up into a media vacuum cleaner. Stress of money way too high.
Our adrenal glands are shot.
Sociologist have a lot to share in the time block of before fibro and then there was fibro.
Would studying the pockets on the globe explain our culture shock. Heck we are in the wars in our living rooms on TV.
Last, but not least, big business- oil, land developers, money handlers sucked the life out of us and ruined existing community living that our ancestors rejoiced in.
Thanks to Julie Sanders for telling us about her great experience with Vyvance. I take generic Adderall, 90Mg as 3 30Mg doses a day in the immediate release form. Adderall is primarily dextroamphetamine with some amphetamine mixed in. If you want to save some money (depending on your insurance) you might want to try the generic Adderall XR (extended release). Vyvance is lisdexamphetamine, which is inactive until your metabolism strips off the amino acid L-lysine converting it to dextroamphetamine. Perhaps Vyvance is made this way so it will be long acting or perhaps for the patent? I have used both and could not tell the difference. I cannot take Vyvance or Adderall XR because I am hypersensitive to any anti-cholinergetic side effects. With the longer lasting drugs I cannot urinate which is very inconvenient. My doctor thinks I can use the quick acting formulation because it is peaky and I can urinate as each dose wears off.
I have read and heard a lot of negative commentary about the use of stimulants by ME/CFS patients, mainly associated with the theory that we should stay within our energy envelope or the idea that stimulants will lead to cycles of push and crash. My mileage differs – I have ADHD and Narcolepsy both of which bear some relationship to an insufficiency of the neurotransmitters dopamine and norepinephrine. I don’t get high or stimulated my brain just gets a little closer to normal and I get by. I have not had the same level of recovery as Julie Sanders, but without them I am mentally flatlined.
Cort,
I really appreciate your attending the IACFS/ME conferences and reporting back. I met you and Hillary Johnson and had the good fortune to spend a couple of hours with Nancy Klimas at a conference in Miami, I think it was 2007 (can not trust my memory of the order of past events and dates). I have the interest but not the energy to attend.
This is good news to hear about researchers with a physics background taking an interest in ME/CFS. My dad (who was a microbiologist) used to say that MD’s are just a bunch of car mechanics, an apt analogy, a good one can be great but mostly start with low expectations.
Dr. Klimas is top notch so no surprise that good research is happening under her watch.
I have proposed that there is a good analogy between medicine at the end of the 20th century and physics at the end of the 19th century – the mechanical model of the universe was just about complete and then the Theory of Relativity and Quantum mechanics blew the doors off, similar to the nearly complete mechanical model of the human body (medical science and training based around organs!) and then the Genome Project, instead of putting the icing on the cake (cupcake?) of medical understanding opened a window into the amazing complexity of living organisms. So I think it is encouraging that researchers who are not just looking for singular answers, but who are looking for understanding of complex systems are taking an interest in our illness.
Best wishes to all – keep your eyes open something amazing happens every day,
Greg
Has anyone here tried out the reset of the HPA axis mentioned in the article above?