As we continue our series on Dr. Martinez-Lavin’s book “Fibromyalgia: How Stress Becomes Real Pain”, he takes us on a tour of pain and fatigue disorders that look like Fibromyalgia and are often misdiagnosed in people with FM (or vice versa).
Being given heavy duty immune suppressants or undergoing surgery to no avail is not a happy thing, particularly when you’re already suffering. This list will hopefully alert people to the pitfalls of misdiagnosis in disorders like FM and ME/CFS.

Two of the disorders listed are endocrine, two involve structural damage to the nerves, and several are neurological. Dr. Martinez-Lavin warns that if you are due to have surgery to decompress a compressed nerve, as in carpal tunnel syndrome or back pain, make sure that you actually have a compressed nerve and are not simply in pain from Fibromyalgia.
Poll
At the end of this blog we have a poll to see who has been diagnosed with any of these disorders.
Now let’s take a look at them.
The Fibromyalgia Mimics
Rheumatoid arthritis (RA) – Affecting mostly women, RA causes swelling in multiple joints, morning stiffness, fatigue, and pain.
- Telling the Difference between RA and FM – there’s less swelling in FM, and rheumatoid factors and antibodies are present in RA. One study also found far more neurological symptoms in FM than in RA; if you have lots of nerve symptoms like burning, tingling, or numbness, you probably don’t have RA.
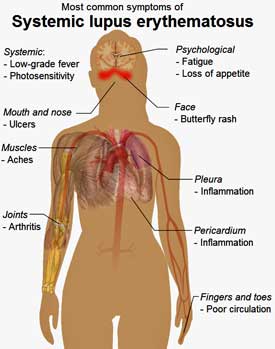
Lupus Erythematosus – Dr. Martinez-Lavin calls lupus misdiagnoses a “real problem” for FM patients. He stated it’s not uncommon for women with FM to be misdiagnosed with lupus and treated (unsuccessfully) as if they have lupus. Both conditions primarily affect women, and both cause fatigue, diffuse pain, joint pain, ruddy cheeks, and fainting.
- Telling the Difference between Lupus and FM – ANA (Antinuclear Antibody) tests can be positive in both diseases but are positive in lupus even after the individual’s blood serum has been diluted numerous times. Antibodies specific to lupus are also present. Anemia and kidney problems can be present in lupus and are not often found in FM.
Polymyalgia Rheumatica (PMR) – causes diffuse pain mainly in the neck and lumbar region as well as morning stiffness, mostly in people over fifty.
- Telling the Difference between Polymyalgia Rheumatica and FM – High erythrocyte sedimentation rate (ESR) and altered c-reactive protein levels indicate PMR is an inflammatory disorder. Those results generally are not seen in FM. PMR responds well, in contrast to FM, to low doses of cortisone.
Spondyloarthritis – affecting mostly young males but also women, ankylosing spondyloarthritis slowly fuses the spine. Inflammation in the tendons and joints is common. Women tend to experience more neck pain.
- Telling the Difference between spondyloarthritis and FM – x-rays show alterations in the spine, particularly the sacroiliac joint in spondyloarthritis. HLA-B27 is often positive in spondyloarthritis. As with PM, anti-inflammatories work in spondyloarthritis but usually don’t in FM. If you’re not responding to anti-inflammatories, you probably don’t have spondyloarthritis or PM or RA.
Gluten Intolerance – Like Fibromyalgia, gluten intolerance can cause pain, headaches, dizziness, depression, and tingling in the arms and legs as well as gut problems. Gut problems, of course, are common in FM. (Dr. Rowe would probably add dairy intolerance to the list of dietary ME/CFS mimics as well.) Recent studies suggest gluten intolerance may be common in FM.
-
Telling the Difference between Gluten Intolerance and FM – positive antibody tests and atrophy of the intestinal villi and intestinal inflammation are present in gluten intolerance.
- Check out Niki Gratrix’s blogs on gluten intolerance in ME/CFS and FM
Nerve Trunk Compression – anywhere nerves are compressed, whether it’s near the spine or in the limbs (e.g., carpal tunnel syndrome), tingling, numbness, and pain can result. The same symptoms, of course, are often present in FM, and Dr. Martinez-Lavin has seen undiagnosed FM patients undergo unsuccessful spinal, cervical, or other surgeries to try and relieve their pain.
- Telling the Difference Between Nerve Trunk Compression and FM – check to see if the symptoms are localized in the area of the suspected nerve. Check for signs of compression using electromyography including nerve conduction velocity studies.
- Check out Dr. Rowe’s surprising findings on spinal cord compression in his young ME/CFS patients in Dr. Rowe on the Hunt: A Search for Chronic Fatigue Syndrome (ME/CFS).
Chiari Malformation (aka Arnold-Chiari Malformation) – refers to compression of the lower part of the cerebellum where the skull meets the spinal area, causing pain, weakness, unsteady gait, and diminished reflexes. Surgical intervention can be very effective in people with Chiari malformation.
- Difference between Chiari Malformation and FM – an MRI of the base of the spine shows compression in the main orifice leading to the cervical spine.
- Check out Dr. Rowe’s take on Chiari Malformation in his adolescent ME/CFS patients in Dr. Rowe on the Hunt: A Search for Chronic Fatigue Syndrome (ME/CFS).
Sjogren’s Syndrome (SS) – is an autoimmune disease that causes dryness of mouth and eyes, fatigue, and joint pain. In more severe cases it can affect the organs.
- Telling the Difference between Sjogrens Syndrome and FM – lab tests show positive autoantibody results, but only lip biopsies are definitive for SS. As with lupus, people can have both FM and SS.
- Check out Lauren Stiles story – Lauren was diagnosed with FM and ME/CFS and other disorders after her health suddenly fell apart. After much perseverance she was finally diagnosed with Sjogren’s Syndrome. Lauren’s story is a cautionary tale for anyone with ME/CFS or FM.
Early Stages of Multiple Sclerosis – MS causes inflammation in the brain and spinal cord and the loss of the myelin sheath that covers the nerves. Like FM, MS can cause enormous fatigue as well as weakness and abnormal sensations.
- Telling the Difference Between Multiple Sclerosis and FM – FM can appear like the early stages of MS. The two disorders can be differentiated by the neurological symptoms that only appear as MS progresses.
Thyroid Dysfunction – either too much or too little circulating thyroid stimulating hormone can cause extreme fatigue. Dr. Martinez-Lavin did not go into the specific thyroid tests to be taken, but it’s clear that the normal slate of thyroid tests will not always pick up thyroid dysfunction in either ME/CFS or FM. With Dr. Bateman stating that no less than 30% of her ME/CFS patients are hypothyroid, thyroid dysfunction is clearly a big deal in these disorders. A blog on thyroid dysfunction is coming up.
- Telling the Difference Between Thyroid Dysfunction and FM – thyroid tests will indicate dysfunction.
Adrenal Gland Disease – people with deficient adrenal cortisol production are chronically tired, weak, and lose weight. Sometimes they present with increased skin pigmentation and low blood pressure. They look more like ME/CFS than FM patients, but FM patients can be misdiagnosed with adrenal cortex problems.
- Telling the Difference Between Adrenal Gland Deficits and FM – when given ACTH the adrenal glands of people with adrenal cortex deficiencies will not respond, but people with FM will.
Chronic Hepatitis C Virus – causes liver infection that produces intense fatigue. Dr. Newton also finds many of the same autonomic nervous system irregularities as well as enormous fatigue problems in another liver disease, primary biliary cirrhosis, as in ME/CFS.
- Telling the Difference Between Chronic Hepatitis C Infection and FM – determine if the patient has a history of transfusions, tattoos, or intravenous drug use, All increase their risk for hepatitis C. If yes, test for the virus.
Vitamin D Deficiency – Dr. Martinez-Lavin states people with FM, in particular older people with FM, often present with vitamin D deficiency. Only rarely – in FM patients with very low vitamin D levels – does he find that people with FM respond favorably to vitamin D supplementation, however.
- Telling the Difference Between Vitamin D Deficiency and FM – low vitamin D levels in the blood are present.
Prescription Drug Use – statins are widely-used drugs that can cause muscle weakness and muscle pains. Laboratory tests will show a high level of creatine kinase.
- Check out more blogs in “Fibromyalgia: How Stress Becomes Pain” series.







Maybe I misread this piece, but it is of course possible to have several of these disorders in addition to ME/CFS/FM. I got a correct and necessary diagnosis of carpal tunnel syndrome after a thorough neurological examination. Surgery immediately relieved my pain, numbness and tingling. Without surgery the nerves would have died eventually and I would have lost sensation altogether. Scary! I don’t believe «unnecessary surgeries» are a major problem, probably more the opposite, people being dismissed and told it’s «only» their ME/CFS/FM.
Yes, but did they rule out trigger points as a cause before you got your carpal tunnel diagnosis?
Oh yes, I underwent physiotherapy, trigger point treatment and ultrasound treatment for 1,5 years – only getting worse by time. When I finally saw the neurologist he said my nerves were so damaged that he couldn’t guarantee that surgery would save them. It was a close call, and the surgeon commented that I’ve must have had extreme pain before the operation. I didn’t take any painkillers or anesthetics the days after the operation even if I had open surgery, the improvement was so profound compare to the pain before the operation.
I too was told for years that the pain in my back was either “all in my head” or from FM. Finally I was encouraged by friends to see a neurologist who was disgusted that so many doctors did not EVER order an MRI to be sure there were no structural issues. In my case, it was determined that I have degenerative disc disease with stenosis in 2 areas for starters. I had 2 surgeries in one year when if I had been seen sooner, the treatment could have been a simple laminectomy.
This is great info, thanks. But the real and true problem, at least in my life, is finding a doctor who will actually get off their butt and attempt to make a proper diagnosis. In my experience, every single thing is attributed to fibro and they don’t want to go any further.
That can be a big problem. FM can cause so many different symptoms there is the possibility that a doctor will ascribe everything to it but that can be a big mistake. FM patients get other disorders as well.
I have had joint, skin, internal organ problems for years. They started over 24 years ago and gradually progressed to the point of disabling me. I have been treated for a dozen individual issues for over 22 years. My mother was diagnosed with sjogrens syndrome about 4 years ago, so I was familiar with the symptoms. My mother has lost her vision in one eye so far from the disease and has only about 50% left in the other eye. She has the joint and muscle issue as well. She also was diagnosed with fibromyalgia. ISeveral years ago I began asking my PCP if sjogrens was a possibility for me. He always gave me a no answer and kept treating me for all the individual symptoms. Back then I was seeing my PCP about 28 times a year plus my other doctors. After my 3rd no it cant be that from him I proceeded to research rheumatologists’ and found a good one about 2 hours away. I rounded up all of my medical records I could from all the doctors throughout the years and sent them ahead to her. When I first met her she already went through my records and began checking me for fibromyalgia. Right away she diagnosed me with that and continued with her exam and told my wife and I that she was pretty confident I had sjogrens but wanted the lip biopsy to confirm. Two weeks later I had my Lip biopsy and she was correct. I have been seeing her 2-3 times a year since and my visits to my PCP have went from over 25 a year to about 6. Naturally when I first seen him with my sjogrens confirmation he tried to say he suspected that all along. At least now he knows what to look for when diagnosing others.There are about 10% of us men who have sjogrens and from what I have been seeing is that most with sjogrens also have fibromyalgia.
What a story Doug! Good for you for perservering. It’s kind of shocking your PCP wouldn’t just get the biopsy done when your mother came down with Sjogren’s. It reminds me that I should get a lip biopsy done – my mother had a severe case of Sjogren’s.
Good concise information.
Oh, how they love to blame FMS for everything. I have been having what I thought were heart problems for several months but no one really took any notice or did anything. The doctors I’ve been seeing at the clinic I go to are still in training. Last Friday (not yesterday) I had to call the ambulance with chest pain. The ambulance man treated me on the way to hospital, gave me the spray under the tongue (which worked) and said I have a heart problem. I was kept in the emergency section at hospital for several hours. They did an x-ray, ECG, blood and urine tests. I had a young locum from America, lovely man,good bedside manner. I told them my last bus home was 5pm. At 4:15 (I went in around 12 noon and had to wait in the corridor for quite a while for a bed) this lovely doctor came and told me the x-ray was clear and all the tests were OK. IT’S PROBABLY SOME FUNNY THING TO DO WITH THE FIBROMYALIGA, that I could go home. I couldn’t believe my ears.!!!
Yesterday I saw the Head Doctor at the clinic here. He did an ECG and told me that I HAVE A SLOW HEART RATE. Am on a tablet (Deraline) to regulate it and have to see him in two weeks. The hospital did not pick this up when they read the ECG and the ambulance took a couple of ECG’s which they gave the hospital as well. No not everything is FMS, though they sometimes like us to think it is.
Jazel
I can’t see the poll?
Recently (two weeks ago) I was found to have way too much epinephrine and norepinephrine secreted in my system, which points to an adrenal tumor. Haven’t seen an Endocrinologist yet, but am now wondering if this is something I have in ADDITION to Fibromyalgia, or INSTEAD of Fibromyalgia. Both could disturb sleep, and cause fatigue, sweating and temperature abnormalities. And, of course, without sleep, anyone will have pain to some degree. Frustrating!
Not a doctor but I would bet in addition to….I’m a laymen but what about seeing someone specializing in dysautonomia. If the endocrinologist doesn’t pan out I would try that. See Dysautonomia International for more information on doctors.
Nancy, when you say you “found to have way too much epinephrine and norepinephrine secreted in my system, which points to an adrenal tumor. “…what kind of test did you do to find that out?
I have just recently been diagnosed with fibromyalgia by my rheumatologist, but I’m still not convinced that what I have is actually fibro. I’ve had widespread pain and fatigue for the last 6 months following a hysterectomy. However, I also feel tingling on the left side of my back, around the rib cage area, and pain and a vein that keeps on popping out only on my left arm… I had a brain/neck/spine scan on Thursday, and am anxiously waiting for the results.
According to Dr. Klimas and my neurologist, fibro wouldn’t cause tingling on my back…
My symptoms confuse me. Any comments/suggestions would be appreciated.
Thanks
join pain I express gratitude for the help in this question
It’s not true that thyroid tests will always indicate a dysfunction. I had hypothyroidism for seven years before it showed up on any tests. In the meantime, I was repeatedly diagnosed with depression and given anti-depressants that made me sicker. I was also diagnosed with FM and no doctor has ever done much of anything for me for that. I also developed reproductive problems, including PCOS and its resulting issues. While the doctors messed around, my health deteriorated and my three small daughters suffered from neglect because their father was frequently away and I had no help caring for them. My eldest became more parent than big sister and at one point, I almost lost them to child welfare authorities because amitriptylene made me sleep as much as 20 hours a day and the prescribing physician refused to take me off of it. Taking myself off of it was a disaster. I have never trusted doctors or anti-depressants since then.
Yes, I agree. It took years to get regular thyroid tests to show I had severe thyroid disease. It only shows on ultrasound of thyroid and biopisies. I have had to have radioactive Iodine uptake scans also. My children were toddlers and I completely lost my professional career before I was properly diagnosed.
I was diagnosed with FM & CFS 20 years ago. I also have cervical stenosis & osteoarthritis. I was hospitalized 5 years ago for very low blood pressure and low heart rate. I believe I have anemia but dr says taking iron supplements won’t help. My bones have recently been hurting a lot more. If I bump my elbows or knuckles even lightly it hurts. So worried I’m not diagnosed right and aftaid drs will just dismiss it all as FM or arthritis. Not sure my dr knows what tests to order or how to read them.
Hi all
Ive just seen rheumatologist, who poked me for about 30 seconds and diagnosed me with FM!!!! Ive made a list of all the symptoms but he didnt even bother to look at it!!! ive argued about different diseases and how they symptoms are alike to FM. He said its nothing else!!! Nothing else has the same symptoms!!!! Im going back to different family doctor to see if they can help. Any advise how can I make them to rule out other things first?
Many thanks and wish you all good health xx
I am wondering if I have fibromyalgia. For a while now I’ve been having pain in my chest that spreads all over my body in places such as my jaw, throat, arms and legs. I have also been experiencing dizziness. I have seen a cardiologist, who says there is nothing wrong with my heart. Could fibromyalgia be a possibility?
Widespread upper body pain is common in FM. Poor sleep and cognitive problems are as well.
Regarding the dizziness you should consider orthostatic intolerance – Go to the resources section on Health Rising and check out orthostatic intolerance and POTS. If they make sense then check out Dysautonomia International maps with dysautonomia experts. Good luck!
I was diagnosed with fibromyalgia over a decade ago. Before that, almost 20 years ago, I was borderline for lupus, but never diagnosed. It is possible, all these years later to have both and not know it?
I don’t know but FM and ME/CFS seem to fit in the borderline between these and other diseases. You’re certainly not alone in this.
Fibromyalgia is often misdiagnosed Lyme Disease, wondering why that was omitted here. I have been suffering with fibromyalgia for years, finally figured out it was actually Chronic Lyme Disease that caused my fibromyalgia. Dr. Rawls has been crucial in my healing journey. Dig deeper, it’s never just fibromyalgia.
I’m definitely intolerant of gluten (joint pain, irritable bowel, headache, skin changes) but I did not have positive antibodies. My understanding is these antibodies are seen in celiac disease, not with intolerance.
Yes, the celiac test doesn’t begin to cover all the possible problems with gluten.