Measuring Fatigue Finally?
How to objectively measure fatigue has dogged chronic fatigue syndrome field for decades. Until researchers can tell how fatigued a person really is people with ME/CFS and FM will always have to deal with the “I’m tired, too” response from both their friends and from the medical community.
An objective measure of fatigue, on the other hand, would differentiate the normal fatigue that healthy people experience from the numbing exhaustion that people with ME/CFS and FM often experience. It would allow the measurement of a fatigue that is more than fatigue; it would enable researchers to measure a pathological state of exhaustion.
These Japanese researchers have been examining fatigue closely for decades now, and they think they may have not only found a way to measure fatigue but to assess post-exertional relapse as well. That sounds like a recipe made for ME/CFS.
They did this by a) knocking people on their butt a bit and b) then carefully measuring how their autonomic nervous system (ANS) responded.
Autonomic Nervous System Breakdown = Fatigue?
Prior studies have found that giving healthy people short-term fatigue-inducing mental exercises results in decreased parasympathetic nervous system (PNS) activation and increased sympathetic nervous system (SNS) activation. A longer eight-hour test designed to simulate an eight-hour working day indicated that fatigue was also associated with SNS hyperactivity and a corresponding reduction in PNS activity.
This is the same pattern of autonomic nervous system functioning found in ME/CFS and fibromyalgia. The difference, of course, is that you don’t need to whack ME/CFS patients with a fatiguing inducing mental test to institute this type ANS ‘breakdown’; studies indicate it’s present all the time – even when they’re asleep.
The Study
Fatigue correlates with the decrease in parasympathetic sinus modulation induced by a cognitive challenge. Kei Mizuno, Kanako Tajima, Yasuyoshi Watanabe, and Hirohiko Kuratsune. Behavioral and Brain Functions 2014, 10:25 http://www.behavioralandbrainfunctions.com/content/10/1/25
In this study, they used a difficult cognitive test called the Kana pick-out test (KPT). It had the 28 healthy college-age female participants in the study read a story while asking them to simultaneously count the vowels in the story, and then answer questions about the story afterward.
Prior to and after the 4-minute KPT the subjects rested with eyes open for 3 minutes and then eyes closed for 3 minutes. During the entire 16 minutes, the researchers recorded electrocardiography (ECG) for subsequent statistical analysis to assess ANS functioning. Subjects self-reported their fatigue on a 0 to 100 scale at the beginning of each period.
Results
The researchers found that the self-reported perception of fatigue was, as they had found earlier, positively correlated with decreased parasympathetic nervous system (‘rest and digest’) activity and increased sympathetic nervous system (‘fight or flight’) activity.
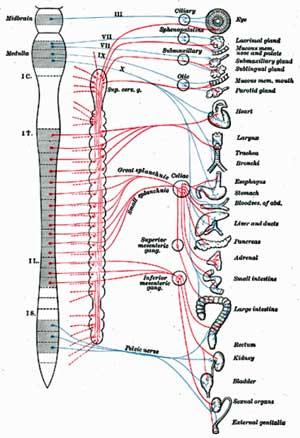
The authors targeted the brain’s autonomic network that controls the wide array of ANS functions in the body.
They noted that the autonomic nervous system is controlled in the brain by a central network composed of the prefrontal cortex, anterior cingulate, insula, amygdala, hypothalamus, and periaqueductal gray matter.
Note that the 2011 Barnden ME/CFS study we just covered found reduced grey or white matter in three of these areas; the prefrontal cortex, hypothalamus, and periaqueductal regions, and reductions in these areas were associated with autonomic nervous system problems in ME/CFS.
Prefrontal Cortex Targeted
These Japanese researchers focused on the prefrontal cortex in the front part of the brain. The prefrontal cortex is in charge of knocking down sympathetic nervous system-charged ‘threat circuits’; i.e. it’s the part of the brain that turns the threat response off.
A Region of Concern in Chronic Fatigue Syndrome
Studies suggest that the prefrontal cortex has indeed taken a hit in ME/CFS. Along with other parts of the autonomic network in the brain, the Barnden study found reduced white matter levels in the prefrontal cortex were present in people with ME/CFS. Since white matter is the communication conduit through which the signals in the brain pass, reduced white matter in the prefrontal cortex could reduce its ability to turn off the ‘threat circuits’ in the brain.
The same Japanese group found that reduced grey matter in the prefrontal cortex was highly associated with fatigue in ME/CFS. A 2002 study by this group finding reduced acetylcarnitine uptake in the prefrontal lobe (and other regions of the brain) in ME/CFS suggest the prefrontal cortex was not up to snuff. Ten years ago this group suggested “the prefrontal cortex might be an important element of the neural system that regulates sensations of fatigue.”
The Zinn study reported at the Stanford Symposium found increased delta brain waves primarily in the frontal and limbic areas of the brain. They suggested a prefrontal-limbic connection between the prefrontal cortex and these important ANS-regulating areas of the brain was important. This was intriguing given the Barnden study finding that the prefrontal cortex might not be communicating well with the rest of the brain.
A small study found that reduced prefrontal cortex oxygenation during exercise implicated exercise in the prefrontal cortex findings in ME/CFS. The prefrontal cortex is also in charge of executive functioning which cognitive studies indicate is impaired in Chronic Fatigue Syndrome. Executive functioning is commonly measured with the KPT mentioned earlier.
Other studies indirectly link prefrontal cortex dysfunction with increased fatigue. Increased prefrontal cortex lactate levels that were found in people with Gulf War Syndrome who did worse on a cognitive test after exercise, again linked energy production in the prefrontal cortex with exercise issues.
Alpha interferon (IFN-a) administration in hepatitis C patients creates similar levels of fatigue and the same kind of basal ganglia dysfunction that’s present in ME/CFS. The fact IFN-a administration also reduces glucose metabolism in the prefrontal cortex suggests that damage to this part of the brain (and energy production again) could play a key role in fatigue production.
If these researchers are right, the inability to effectively rest and recover from ‘stress’ in ME/CFS may reflect an inability of the prefrontal cortex (and perhaps other parts of the autonomic network in the brain) to knock down sympathetic nervous system-derived ‘threats’ and reinstate the rest and digest (PNS) system. Fatigue appears to be correlated to the extent to which the parasympathetic nervous system fails to assert itself during rest.
The prefrontal cortex is clearly a part of the brain to keep an eye on in ME/CFS.
Another Way to Explain Why You Need Peace and Quiet
This study also revealed one reason people with ME/CFS often go to a dark place and close their eyes when they’re fatigued. It turns out that sympathetic nervous system activity is higher when our eyes are open.

Why do people with ME/CFS and FM seek quiet places? Perhaps to calm down their sympathetic nervous systems…
The ECG revealed no differences in sympathetic nervous system functioning in the healthy controls whether their eyes were open or closed before the cognitive test. After the cognitive test, however, when their eyes were open, their SNS activity was increased, their PNS activity was decreased, and as expected – their fatigue was increased. When their eyes were closed, however, their SNS activity decreased, their PNS activity increased, and their fatigue was reduced.
It appeared that the strain of the cognitive test had momentarily wiped out the ability of even these healthy brains to rein in their SNS when their eyes were open.
This, of course, makes perfect sense to ME/CFS patients who recognize that lying down in a dark place with their eyes closed is helpful. This study suggests they’re engaging in an instinctual attempt to calm down their SNS (fight or flight system), bump up their PNS (rest and digest system) and reset their autonomic nervous system. (Unfortunately studies indicate that the sympathetic nervous systems in ME/CFS tends to remain engaged even during sleep.)
Has an Objective Measure of Fatigue Been Found?
“The extent to which parasympathetic nerve activity is inhibited in the recovery phase of the resting state in the eyes-closed condition may depend on the extent of fatigue.” The authors
The link between autonomic nervous system (ANS) dysfunction and fatigue is growing. Studies both in healthy people and in severely fatiguing disorders such as Chronic Fatigue Syndrome, multiple sclerosis, and primary biliary cirrhosis indicate fatigue is associated with alterations in ANS functioning — specifically, increased sympathetic nervous system and reduced parasympathetic nervous system activity.

An objective test of fatigue would validate an often-dismissed component of
“Chronic Fatigue Syndrome”
This Japanese research group proposed that their test protocol described above might be able to quickly and easily assess the degree of exertion-induced fatigue present.
The degree to which the parasympathetic nervous system fails to return to its normal resting state after a short cognitive test would determine the level of fatigue present.
Being able to objectively validate the fact that the fatigue in ME/CFS or FM is not similar to the fatigue healthy people occasionally experience would be a major step forward. A pathological state of fatigue associated with a pathophysiological finding – a damaged parasympathetic nervous system – would validate the seriousness of ME/CFS and open new fields of research.
This is the same team, by the way, that startled the ME/CFS community this year with its finding of widespread neuroinflammation in the brain.








What a teem!!!
Dr Sarah Myhill and John Maclaren-Howard can measure fatigue from the mitochondrial function profile test. With health subjects being anywhere between 100-300%. Sufferers can be measured at below 100%..one has even been measured at 2%…I have done this test and scored 49% 12 months ago.
That sounds like a good marker for fatigue – the mitochondria being our energy producers…I hope they can get it validated and more researchers interested in it.
i too had dr sarahg myhill and john maclaren-howard mitochondrial function profile test and my score was 10% and truly reflected the level of fatigue i experience. like gulf war syndrome i was given 9 vaccines in one day and became very ill. i have been ill for six years now. my eyes hurt a great deal and any cognitive demands bring on migraine type headache and a dreadful sensation on my right side of brain. this article is very interesting. Is there any medical groups in the big teaching hospitals in the NHS like the royal free hampstead or other whom would work on these findings and others to help bring greater understanding, correct testing and treatments up to date !
Ten percent – wow…Maybe someone else knows about some medical groups.
I sure like the exercise physiology tests better than anything that could be interpreted as involving the “brain” or ergo “psychological” problems!
Why not do a short exercise test and then test ANS functioning in the same way?
If this pans out it is so much easier and less stressful than doing an exercise test – it’s a 16 or 18 or whatever is minute test that simply requires a short cognitive stressor..
Grear article Cort. Combine these findings with the work Jarred Younger is doing on leptin and I think we may have a complete model.
Incidentally, in type II diabetes, exercise intolerance has been shown to be related to anaerobic threshold (as with ME/CFS) and hitting the anaerobic threshold correlates with a reduction in heart rate variability (as seen in ME/CFS) with the possibility that heart rate variability may be a simpler and non-invasive measure of anaerobic threshold which might make this type of testing more feasible outside of specialist exercise physiology labs :
Noninvasive method to estimate anaerobic threshold in individuals with type 2 diabetes
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3033241/
It all seems consistent with physical and mental stressors causing a sustained shift in the ANS.
Good !
Thanks, Cort. Any idea if and when this test will be available? I’ve been trying to secure disability but the SSA in my state keeps on demanding measurable “evidence”.
I think it will be awhile…It seems to have a good basis in healthy controls – now they need to test it in disorders. One good thing is these are ME/CFS researchers who developed the test. I would be surprised if they didn’t take the next step and validate it in ME/CFS. They are from Japan, though – not the US. Not sure if that will delay things or not.
There is the two-day exercise test – pretty bulletproof for disability if you can handle it.
Hi Cort do you have any links to specific studies? Im interested by this…:
“(Unfortunately studies indicate that sympathetic nervous systems in ME/CFS and FM tend to remain engaged even during sleep.)”
S
Exp Brain Res. 2010 Jul;204(1):71-8. doi: 10.1007/s00221-010-2296-1. Epub 2010 May 26. Reduced heart rate variability predicts poor sleep quality in a case-control study of chronic fatigue syndrome.
Burton AR1, Rahman K, Kadota Y, Lloyd A, Vollmer-Conna U.
http://www.ncbi.nlm.nih.gov/pubmed/20502886
This research is on the right track, imho. I’ve had big functional improvements through learning and using EEG neurofeedback, to rebalance the ANS (autonomic nervous system), decrease excessive delta, theta, and hibeta waves, correct alpha and beta anterior/posterior and interhemispheric reversals, improve sleep, etc. And I’m not even done rebalancing yet — it takes a while, and takes a lot of training, effort and patience, but ultimately it can pay off.
Margaret Ayers, one of the pioneers in EEG NF, actually brought people out of comas using neurofeedback. And someone in that state is a lot less functional than even someone with CFS, lol. This all indicates that the brain tends to prefer homeostasis, no matter how dysfunctional it may be, and thereby often gets locked into these dysfunctional patterns until we provide the proper feedback to the brain for it to adjust itself more optimally. Add in some immune involvement, and there is a strong environment for the brain to malfunction. But improving brain function can also help adjust and improve immune function — to some degree the two even go hand and in hand — and therefore helping one tends to help the other.
Hi Jrez,
Can you recommend any helpful resources on EEG Neurofeedback, please? I live in Norway so couldn’t attend a US based clinic but would be interested in reading about EEG N.
Thanks
Belén
Interesting statement jrez – Broderick would approve
“This all indicates that the brain tends to prefer homeostasis, no matter how dysfunctional it may be”
I imagine it does take awhile using neurofeedback and patience is required. Congratulations on your improvement.
The literature suggests if you can reduce SNS activity it could very well improve immune functioning.
Awesome!!
Look forward to the ME/CFS results for fatigue. I wish that team could get on it and find out of there’s a virus involved lurking in the nervous tissue or the B cells. I have a lot of faith in their competence.
One of the downsides of ME/CFS is the lack of guidance from medical authorities in regard to the effects one will experience. This fatigue test should help fill that need.
I have no trouble convincing anyone that my body can’t perform; however trying to convince that cognition is also out, that, I find, is more complicated… “Can’t walk? – Just read a book then! – Nope, can’t do that neither… There is something about my brain…in general!”. I feel this Kana pick-out test would wear me out as much as a CPET. I really salute a study such as this one that goes at the root of exhaustion, beyond physiological exhaustion in a narrow sense.
This is how I think it would go — the pre-test ECG would indicate the PNS is under-active in ME/CFS – then it would probably get wiped out in the post-Kana pickout test ECG….
One study showed ME/CFS patients brains were having trouble turning off their attention to background stimuli – so here their brains would be – listening to the background noise, trying to pick out vowels in the story and trying to remember the story….
That would be rough :). I think there’s something so crucial in ME/CFS about cognition…
I too have cognitive difficulties. I was an excellent reader and speller before contracting Epstein-Barr and ensuing CFS/fibro!
Thanks Cort. I would never learn about these studies without your summaries. These findings add much needed hope that enough clues will come together for a treatment plan – hopefully soon.
Indeed – thanks Greg.
This makes so much sense to me. I have CFS and I can sense that my brain doesn’t rest at night even if I’m sleeping. My question, of course, is “What can I do about it”. I regularly use relaxation tapes, I relax before bed, I have a darkened room but all to no avail. Anyone know of a solution?
Yes, good question :)…those are things that can work for some people. Xyrem is very expensive but it can help with those deltan intrusions I think they are, that disrupt sleep. We have a blog coming up on something else that may help but it’s brand new stuff – probably not available.
Cort, you are really the best ‘blogger’ for ME/CFS. Thanks. The ANS is a major key player in ME.
Thanks Gijs. I have no doubt that other systems are involved but the ANS is showing up more and more.
Great article- Cort is there any way of contacting you privately? I have something to ask. thanks
Yes. Just use the contact tab on the menu on the top of the website. 🙂
Totally stupid. I feel for their ‘test subjects.’
Way to go – now find a way to measure fatigue (which VARIES throughout the day) WITHOUT stressing the person!
I use Sudoku Hard puzzles. Fewer than 7 min – functional to semi-functional. More – nap time.
The ‘mental dialysis’ that washes the junk out of my brain while I’m taking a 35 min total rest can then give me up to 2.5 hours of being semi- to fully-functional (for me – not normal people). Then I REPEAT.
I know how I feel fatigued – I don’t REALLY need the Sudoku, but I hate taking the naps because I’m an adult who shouldn’t need them. Most of the time I try for a 35 min. nap every three-hour period. And then I can write for a bit.
These studies drive me crazy – what are they going to do – test to exhaustion every day several times to see ‘how you’re doing’? Totally stupid.
1. Delta Waves mentioned!
I am amazed that someone finally validated the delta waves (Zinn study). I had two ECGs about 20 years ago. The only thing they said they found was that I had periodic delta waves while I was awake. At the time, I said “Well, duh!” I wonder how the delta waves during waking state have anything to do with concentration difficulty and difficulty expressing thoughts in verbally.
2. Might there be some enzyme(s) that would help us process the “fight or flight” chemicals?
My sister and I have both had CFIDS (ME/CFS) since we were very small (although we weren’t diagnosed until we were 32 & 21). We have been saying for years that we need a better way to process the fatigue chemicals. We recently found out that we are slow caffeine metabolizers (genetic analysis 23andMe). (We had already realized that caffeine caused us problems, and had virtually eliminated it from our diet.) We recently found an enzyme, rutaecarpine, that helps us process caffeine. Rutaecarpine is available through Linnet Biopharaceuticals:
Amazon, Rutasomn
http://www.amazon.com/s/ref=nb_sb_ss_i_0_7?url=search-alias%3Dhpc&field-
keywords=rutasomn&sprefix=rutasom%2Chpc%2C213
or Linnet Biopharaceuticals Ruta Cleanse
http://rutasleep.com/products/rutacleanse
Also Ruta Sleep, rutaecarpine with melatonin
http://rutasleep.com/products/rutasleep
Yes this could all be helpful to the seventy-five percent who don’t have the tme/cfs “terminal me/cfs” that the other twenty-five percent of us have. We’ll probably be long dead and gone before they discover the hidden retrovirus killing us.
I wonder if the Transcranial Magnetic Stimulation I’m having will help as it’s aimed at that part of the brain? I’m having the treatments at Avera Behavioral Health in Sioux Falls, SD. It involves 6 wks of treatments every weekday and only 2 1/2 wks in the terrible chronic depression is lifting
Interesting! Enrolled in the synergy trial offered by Dr. Nancy Klimas, NOVA Southeast University, Fort Lauderdale, Florida in conjunction with Sandford University, California. Combination of a low dose of a stimulant and nutritional formula working at the mitochondrial level. Also, proper nutrition a pacing activity level. It is working great for me!
Glad to hear it Ana…Good luck with that and please keep in touch with how it’s going.