



When I saw that the video “Fibromyalgia: It’s Real It’s Manageable What You Can Do” had been viewed almost 85,000 times I had to check it out. In it, Dr. Andrew Gross, the head of the Rheumatology Clinic at the University of California at San Francisco presents a a birds-eye view of fibromyalgia.
The grace in this video – which has been viewed over 100,000 times – is Gross’s engaging presentation style. If you want enroll somebody in your life in the idea is that fibromyalgia is a real and serious disorder – this might be the video to do it.
At the same time the video is by no means comprehensive; Gross’s treatment approach to FM is decidedly conservative and it’s getting a bit dated. Still, for an easy to understand lecture on the basics of FM, it may be the best out there.
Fibromyalgia or Chronic Fatigue Syndrome? – You Choose
Gross didn’t talk about chronic fatigue syndrome but as someone who was diagnosed with it decades ago, it was interesting to see how well Dr. Gross’s description of fibromyalgia fit me. Most people with fibromyalgia, he stated, wake up in the morning feeling unrested, stiff, and in pain. As the day wears on they feel better around mid-afternoon, and then feel worse in the evening, particularly following prior busy days (PEM). That pretty much fits me to a T.
Widespread pain, fatigue, and unrefreshing sleep are the three hallmarks of FM. [That’s a bit different from the post-exertional malaise, cognitive dysfunction, and unrefreshing sleep believed to be hallmarks of ME/CFS]. Difficulty concentrating, headaches, jaw and chest pain, bowel problems, frequent urination, pelvic pain, numbness and tingling, itchy skin, and chemical sensitivities round out the short list of common symptoms.
As Dr. Gross explains how he diagnoses FM, it’s clear that I fit the list pretty well: widespread pain, often focused in the upper body, fatigue, poor sleep, and difficulty thinking. With the sleep issue it’s not that FM patients are up all night necessarily (although some are), but that when they wake up they feel unrested, tired, and “out of it”.
He doesn’t use tender points – the standard of FM diagnosis for years – because he has found that they’re not all that tender in some people with FM.
His FM model fits chronic fatigue syndrome fairly well, which brings up the question whether what most of us get diagnosed with depends on which kind of doctor we see first. If you were extremely fatigued and had no pain symptoms – no muscle or chest or head or gut pain – but had problems with sleep and concentration you would have ME/CFS… but how many people with ME/CFS are like that?
Take the poll and let’s find out.
FM and ME/CFS Major Symptoms Poll
Infection? Gross Says No To Infection
The ME/CFS connection gets another twist when Gross states that the one thing people always ask him about is an infection – do I have an infection? That’s an interesting question given how little infection has been assessed in fibromyalgia research. Although Gross doesn’t mention it, many cases of fibromyalgia do begin with a flu-like illness. Gross does not feel that some underlying infection is likely. [This talk was given well before the Pridgen antiviral studies began and the small nerve findings and cytokine studies popped up in FM.]
Stating that most infections (including EBV) are self-limiting, he quickly moves on. If his approach is emblematic of that taken by most FM doctors, a dividing line between FM and ME/CFS practitioners may be the idea that a significant chronic infection may be present.
A Common Syndrome
The five million people with fibromyalgia in the U.S. is more than rheumatoid arthritis and lupus combined. He noted that hypermobility, thyroid, sometimes diabetes, cancer, autoimmune disorders, lupus, multiple sclerosis, and Parkinson’s can all look similar to FM.
[Fibromyalgia gets considerably more research funding from the NIH than does ME/CFS, but per patient funding is actually considerably lower. Neither disease gets more than a modicum of support from the NIH.]Nervous System Disorder
When Dr. Gross states there is no reproducible evidence of inflammation in the muscles or joints or damage to the nerves as seen in diabetes, he’s clearly a few years behind the times.
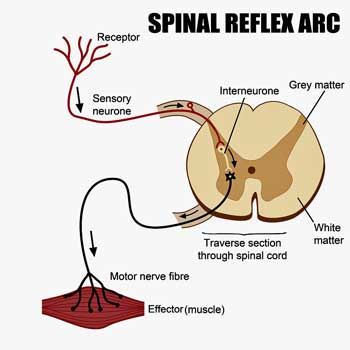
If the body is not the problem – and apparently it wasn’t then – then up we move to the central nervous system. It turns out that in times of danger our body can move faster than our brain. If you touch a hot surface, a pain reflex will jerk your hand away before the signal gets to your brain. This reaction occurs between the site of the stimulus (heat on your hand) and your spinal cord. Studies using an electrical current to measure this reaction (twitch reflex) found that it occurred at a lower level of stimulus in people with fibromyalgia than in healthy controls.
Again, note that the brain is not involved at all; this is all taking place between nerves in your body and the spinal cord. This finding helped cement the idea that oversensitive dorsal root ganglia (a collection of nerve bodies just outside the spinal cord) and/or an oversensitive section of the spinal cord called the dorsal horn – both of which process pain signals from the body – are making people with FM more sensitive to pain than normal.
This suggests an improperly set central pain control improperly interprets normal sensations as pain. That is, if you have neck pain the problem is probably not in your neck. If you have gut pain the problem is probably not in your gut. If you have muscle pain, it’s not in your muscles. The problem, Gross believes, is an improperly set sensory system that’s telling your brain to produce the sensation of pain where there’s no real injury.
[It’s no longer as clear that FM is simply a nervous system disorder. The nervous system, however, is clearly involved.)Not Just Fibromyalgia
One bit of good news about this central sensitization problem is how prevalent it is. Dr. Gross noted that many people without fibromyalgia who don’t have widespread pain still have difficult-to-explain pain, sleep, and fatigue issues. That means there are more researchers working on these problems perhaps resulting in a better chance of getting at the cause.
[A concept called the ‘fibromyalgianess’ of disease, refers to back or knee pain or fill-in-the-blank pain patients who end up, over time, meeting the criteria for fibromyalgia. For them their pain began with a specific injury which appears to sensitize the nervous system, eventually turning them into fibromyalgia patients. It’s likely that this process occurs in a significant percentage of all pain conditions.This is good news for fibromyalgia patients, because it should mean more attention to the processes that cause FM. The bad news is that, despite the huge economic burden and suffering that pain produces in the U.S., the NIH still spends a negligible amount of money on understanding and treating it. Because there is no research institute at the NIH, for instance, focused on pain, pain research is underfunded and scattered. We’ll get more into that in another blog.]
“Fibromyalgia: It’s Real It’s Manageable -What You Can Do” by Dr. Andrew Gross
Triggering Factors – Chronic Lyme Disease… err, Fibromyalgia (err, Chronic Fatigue Syndrome?)
Gross’s explanation of what happens with Lyme disease is fascinating. People infected with the Lyme spirochete (helical bacteria), he noted, feel terrible and the infection can take a while to get over. But if you came down with Lyme disease and took your medication, and tests indicate the bacteria is gone and you’re still sick, Gross doesn’t believe you have Lyme disease anymore – you have fibromyalgia.
Gross also suggested that severe traumas deep in a person’s past can set some people up for FM. [That turns out to be true for many disorders including autoimmune ones.
Getting Diagnosed
Why get diagnosed with fibromyalgia? Besides the obvious reason – to find appropriate treatments –there’s the less obvious reason – getting diagnosed with FM helps you not to get diagnosed with something you don’t have. [Both Clauw and Martinez-Lavin have noted how hard physicians try (particularly with men) to find something they can pin a diagnosis on. Multiple MRIs later they may finally find a little something that might account for the pain. A failed surgery later the patient is in more pain than ever.]
Prognosis
Do people with fibromyalgia tend to get better over time? Yes, they do. Gross showed a slide indicating about an average 25% reduction in pain for most people over about a dozen years. Do they get cured? The short answer is, at this point, probably not.
The big question about that 25% drop in pain is why it happens. Is it happening naturally? Are they managing their illness better? Are treatments helping? Or have they just gotten used to the pain? No one knows.
Treatments
The theme regarding treatment is that it takes a village — a multidisciplinary approach that includes a variety of treatments – to really make a difference in Fibromyalgia. This is not a take a pill and get better kind of illness.
Drugs

Dr. Gross didn’t appear to be particularly excited about any of the drugs, but it’s clear they help some people. They are one part of a multi-disciplinary treatment plan
The first drugs Gross talked about were aimed at reducing the amount of central sensitization produced at the dorsal horn of the spinal cord. Noting that during fight/flight situations pain sensitization is usually decreased, one approach is to ramp up the fight/flight response using antidepressants such as Elavil, Cymbalta, Savella, and Effexor prescribed at doses lower than used for depression. [Studies have indicated that people without depression, but with pain can benefit from some of these drugs.] Studies suggest they may reduce pain by 25% in about half of FM patients.
Dr. Gross described them as “reasonably effective” in a “limited” number of people. He was not clear, however, how long the effects would last.
Lyrica (pregabalin) and Neurontin (gabapentin) attempt to block the release of neurotransmitters in the nerves sending pain signals to the spinal cord. These two similar drugs (Lyrica is an updated version of Neurontin) “can” he said, “be helpful.” They seem to work best at inhibiting burning and tingling type pain. They often, however, make people sleepy and foggy, and he’s not particularly fond of either drug.
Flexeril (muscle relaxant) – helps some people.
Tramadol – a codeine-like drug that can be helpful for some people. It can cause constipation, though.
NSAIDS (e.g., ibuprofen, naproxen) – have been studied quite a bit but no one has been able to show they’re very effective over a long period of time in fibromyalgia. He generally uses them for people with specific pains such as arthritis.
Corticosteroids (prednisone) – noting that anyone given prednisone will probably feel better for a short time, Gross reported that the effects tend to be short-lived and, if you take it for very long, the side effects are extensive and severe.
Benzodiazepines – Gross is not a big fan of benzodiazepines. They can help people sleep at first, but over time people may require them to get any sleep at all.
Opioids (Vicodin, Oxycontin) – Gross noted that some rheumatologists do prescribe narcotic pain relievers and that they do provide pain relief, but that FM patients often need more narcotic pain relievers than usual to get the same level of relief.
He’s fan of methadone, calling it a fantastic narcotic with long lasting effect, but his experience is that people with FM often need to take higher and higher doses to get the same relief. Methadone and other narcotic pain relievers can be effective, however, for short-term relief.
The Body
Exercise
Gross reported that many, many studies have shown exercise to be helpful with reducing pain and helping with sleep in FM. Gore recommends walking, bicycling, swimming, stretching and Tai Chi and Qi Gong.
People with FM aren’t being asked to run marathons. The ‘workouts’ that work tend to be very mild indeed. Starting exercise programs can consist of 5-10 minute walks that slowly build up over a period of months to 30-60 minute walks. Gross loves water aerobics and swimming, and doing them a couple times a week can be very helpful.
It is at exercise fibromyalgia parts ways with chronic fatigue syndrome to some extent. Some studies suggest exercise is helpful in ME/CFS, but reports of negative effects from mild exercise are legion. Surveys of ME/CFS patients indicate exercise produces more negative side effects than just about any other therapeutic approach to ME/CFS.
It is clear, on the other hand, that the right kind of exercise can help some. Some physicians, using very carefully prescribed exercise programs involving heart rate monitors, report considerable increases in fitness, functioning, and quality of life with some ME/CFS patients, but the ME/CFS population as a whole appears to be more fragile with respect to exercise than people with fibromyalgia.
Stretching and Body Movement Therapies
A stretching program every morning and perhaps twice a day can be very helpful at relieving the stiffness that is so common in FM, but finding a physical therapist familiar with FM that will devise a mild stretching program is important. Finding stretches that attack tight spots in the neck or back or wherever the stiffness occurs can be very helpful at reducing the level of pain signals hitting the spinal cord (and setting off the central sensitization).
The poses in Tai Chia and QiGong that have an isometric, stretching, and meditative components can be very effective.
At the end of this section, Gore noted how difficult these approaches can be. He said he often has FM patients come back and say that after 15 minutes of walking a day for three days they couldn’t move for a week. Starting at something that is ‘ridiculously easy’ and very gradually building up is important, he reported, but he also suggested that it’s important to make a plan (say 10 minutes of walking a day) that keeps you within “reasonable pain boundaries” and that you can stick with even if you feel lousy at first.
Diet
Nothing convincing has shown up in the studies indicating diet is important BUT studies have shown obesity does increase the risk of getting fibromyalgia and, if you are obese, losing weight can help.
[Since this presentation one study suggested celiac disease is present in about 10% of FM patients with IBS. Another found that a gluten-free diet resulted in a “slight but significant” improvement in symptoms in people with fibromyalgia and IBS. Personally, I have found that eliminating dairy, gluten, eggs and reducing beans was very helpful for what was an ever-increasing and worrisome problem with IBS. Surprisingly, getting rid of tomatoes reduced my knee pain as well.]The Sleep – Pain Connection
Gross related a fascinating study where it took just three days of knocking healthy people out of deep sleep for them to develop what appeared to be fibromyalgia. It took just three days of interrupted deep sleep to turn them, with their widespread pain, headaches, and abdominal discomfort, into “a mess.” With the periodic arousals and difficulty attaining deep sleep found in FM, people with FM are in much the same boat. It’s clear that increasing restorative sleep results in reduced pain, but how does one do that?
Gross presented a list of good sleep hygiene practices familiar to many with FM and/or ME/CFS. That was it for sleep! He gave no recommendations for drugs, although earlier he noted that Trazodone can be helpful.
The Mind – Training Your Brain
The mind often gets discounted, Gross said, because most people with FM see medical doctors who don’t have any expertise in this area, and because of a backlash from patients who have been told too many times that FM is all in their head.

Since studies indicate that negative thoughts do enhance (not cause, but enhance) pain, it’s best to get rid of them as much as possible.
Chronic pain, he asserted, is such a distressing symptom that it almost inevitably leads to increased anxiety – which interferes with sleep – which causes more pain. Neurologically this process starts at a key pain processing center – the dorsal horn of the spinal cord. The dorsal horn can either increase pain signals or inhibit them, and the brain can either increase or decrease the dorsal horn activity as well. Studies indicate that negative thoughts from depression, anxiety or catastrophizing activate the neural pathways the brain uses to increase pain signals at the dorsal horn of the spinal cord.
This process is getting clearer and clearer for me as I slow my thoughts down. Negative thoughts – coming from the subconscious – really do, at least in my case, directly translate into increased heart and breathing rates and increased pain and stiffness.
Gross then asked, “What would life be like if you could influence the way you think and feel?” There are many ways – from meditation to mindfulness to CBT – to do this, but it led him into a discussion on cognitive behavioral therapy which he called “very effective” … without saying what he meant by that.
Throughout the course of the talk Gross will call several different treatments (exercise and CBT) “very effective or effective”. I think most laymen would assume an “effective” treatment would be effective at removing the illness, but that’s clearly not what Gross means. His statements suggest that most people with FM, even after treatment, are still quite functionally impaired, and cures, if they occur, are rare. Obviously they’re not enjoying stable health if something like that is going to happen. My guess is that his experience is that these approaches are effective at relieving pain and improving quality of life. Note that he rated some of the top FM drugs as being only “reasonably effective”.
CBT for FM consists of educating the patient about how the pain in FM occurs, realistic goal setting [read pacing], relaxation training, and identifying dysfunctional thought patterns and using techniques to counteract them. Studies have shown CBT can reduce that overactive pain reflex Gross talked about earlier.
Relationships
Relationships can have either a negative or positive effect on pain. Understanding and support from your significant others can help to reduce your pain level. Denial and the “buck it up and get through it approach” results in more stress and more pain. [Gross never talks about the autonomic nervous system, but people with fibromyalgia have the same pattern of fight/flight activation as do people with ME/CFS.]
An overly protective caretaker approach, in which the caretaker does everything for the FM patient, is just as bad in Gross’s experience.
Relationships can reduce or increase pain levels. Surprisingly, too much care can be counter-productive as well.
Effectiveness of Non-Drug Therapies
As Gross goes over how much evidence there is for how effective non-drug approaches to FM are, again he takes a conservative approach. If an approach hasn’t been studied, it’s not going to be in his list. Presumably it’s not in his treatment plans, either.
We don’t know if the treatments in the weaker categories failed to produce effects or if the studies were too small or too poorly designed to provide strong evidence for effects. Since Gross doesn’t address how effective treatments are – he addresses the evidence for efficacy – we don’t know if CBT, for instance, was highly, moderately, or weakly effective – we simply know that there’s moderate evidence for its efficacy, whatever it is.
Note that “moderate evidence” for effectiveness is as high as it gets in FM.
- Moderate Evidence of Effectiveness – aerobic exercise, cognitive behavioral therapy, patient education, group therapy.
- Weak Evidence for Efficacy – strength training, acupuncture, hypnotherapy, biofeedback, balneotherapy.
- Very Weak Evidence for Efficacy – chiropractic, manual and massage therapy, electrosound, ultrasound.
- No evidence for efficacy – trigger point therapy.
Gross believes acupuncture is probably more about the placebo effect than anything. It’s less where the needles are put, he said, and more about having a reassuring and supportive acupuncturist. Gross’s explanation of why there’s weak evidence for trigger point therapy – the only treatment in the “No evidence for efficacy category” – was more about process than results. Explaining, to some laughter in the room, that trigger point therapists appear to be able to inject everything from novocaine to steroids to salt water to water and get similar results, he never actually addressed what the results were – he simply dismissed the therapy.
Questions
Is there a relationship between mental illness and fibromyalgia?
This is a good question particularly after the emphasis on CBT, isolation, and relationships in the last section. Gross’s answer was “no” with some caveats. Mood disorders do not predispose someone to getting fibromyalgia and the depression found in FM is a more or less normal consequence of being in pain all the time. Anxiety, interestingly enough, may predispose one to FM. (Baraniuk believes anxiety is probably more important in ME/CFS than depression as well.)
What Kind of Pain is Present in FM?
The pain in FM is very varied, tends to be strong, and has a functional impact; i.e. it’s the kind of pain that keeps you from doing things.
Conclusion
Gross presents an appealing talk that focuses on the conservative management of fibromyalgia. You’ll have to go somewhere else for cutting edge approaches to FM, but the talk is good on basic management practices that can be helpful – and gets across the point that FM is a real disease. It also reveals how little treatment of FM has progressed. With Gross not finding a great deal of effectiveness from the FDA approved drugs, his “management” protocols – and he is mostly talking management – not treatment – focus mostly on behavioral actions people with FM can take: very moderate stretching and exercise practices, relaxation, reducing negative thoughts, improving relationships- the tough stuff basically.
- Coming up: a very different take on diagnosing and treating thyroid dysfunction and fibromyalgia from Dr. Holtorf.










I think this was a waste of time……..and energy.
I disagree with Richard
Ugh….that was a really awful youtube presentation of half truths, guesses, unsubstantiated opinions and flat out falsehoods. I don’t even know where to begin…..
no offence Cort – your synopsis is first rate but the video made me cringe.
I was surprised there was no more “there” there given how popular that video is. Still, I think the things Gross lays out can be helpful – they’re just not easy to do – and they’re focused on management not treatment – and I think many more possibilities exist.
I thought the exact same thing – I suspect the video is so popular because this is a desperate population looking for answers – I just don’t think Gross has them. I am really curious to know where he got the statistics with regards to pain reduction after 12 years. The literature actually states the opposite – FM people do not generally get better, they get worse.
:). I had the same thought actually…is this worth it? I committed to doing it though, and while it’s definitely not cutting-edge I did get some stuff out of it.
Although Ramsay and Acheson were unequivocal that complete rest gave the best prognosis for ME/CFS, I have not seen anyone prepared to set up a research program using this as a first call treatment. Yet all the information about the negative effects of exercise, and the fact that patients who are allowed to minimise activity and resume in their own time gradually improve would indicate that this would be an approach worth trying. But who would undertake it? It would not fall within the remit of any research speciality, and it won’t make any money for a pharmaceutical company. So we are never recommended a treatment which might be the most beneficial of all. In the meantime, told to exercise, we are the equivalent of people with a peanut allergy being advised to go home and practice eating peanuts.
too long to read in one go but I’ve done the poll baed on my condition when diagnosed. I recently began to suffer from severe pain and have been prescribed Carbamazepine which certainly helps and I wake more refreshed. I probably do have nerve damage but the NHS wont do a scan and i’ve yet to arrange a private one. I wonder if it would help others?
Also came across an article suggesting that some people improve after treatment by an osteopath.
And please dont use a peanut allergy analogy. Bad as this condition is exercise wont immediately kill me. Eating peanuts can cause death within half an hour.
As a fibromyalgia sufferer for almost thirty years I find the most interesting aspect of this article is the comment by Baraniuk, who believes anxiety is probably more important in ME/CFS than depression as well. This is, indeed, insightful to me.
The only other connection I’ve seen with anxiety and ME/CFS is a study by Naschitz of autonomic nervous system signatures in various diseases. Anxiety was the only one that was similar to ME/CFS.
Good write up, Cort! I have thought you had FM rather than ME/CFS, but am very grateful that you have done so much for those of us in the neighboring camp.
I used to go to a large support group for people with FM and gradually realized that I wasn’t quite one of them. Pain was the primary complaint and sleep the first need. They had more intensity, and also more ability to work and have relationships–a higher activity level. They had some cognitive trouble but not nearly as much. I had a high level of cognitive trouble, in terms of memory and slow processing, in and out of complete blanks/blackouts during the day–as well as unable to make exertions without days of payback, with flu symptoms, fatigue and more cognitive trouble. I had less capacity to work and have relationships. Later I have developed increasing autonomic nervous system problems as well as neuropathy. Gut problems too, but they are down the list. But here is my point:
If there were a large room full of people with ME/CFS and FM, all comparing notes, over time they would sort themselves out. We have neighboring ailments but the overall patterns differ.
I think they would sort themselves out.
The poll thus far shows that most people reading this had FM or FM plus CFS but the degree of PEM is very high. In fact a higher percentage of people said PEM was a major problem than with pain! or fatigue. A higher percentage said fatigue was a major problem than with pain as well.
Time for FM practitioners and researchers to get how big of a problem PEM is in the FM population.
Weakness – which is not really a problem for me – was pretty high – there’s a lot of weakness in FM as well.
Agreed – PEM has been largely overlooked in the FM population which is weird because it is the underlying factor behind the need to pace. I think most FM patients use pacing as a primary management tool.
I agree with this and would also like to say that from my own experience, I believe the pain results are reduced in the poll due to the fact that pacing will also reduce pain levels and to more of an extent than the PEM. In my own case, my pain levels are also much lower than fatigue or PEM due to continually working on my trigger points. Gross shows a great deal of ignorance of trigger points as deactivation with a needle is the method and so injecting anything will achieve this, even with what’s known as dry needling, though this can cause a lot of post- treatment soreness.
Cecelia in my 13 years running a support group for people with FM, and CFS/ME I would say it’s not that black and white. Many with FM have severe brain fog. I like Dr Myhill’s suggestion that there should be a horizontal line with pain one end and fatigue the other and we are somewhere along that line. Even that can be too black and white, for example 9 years ago I was so disabled by both pain, fatigue and had severe brain fog that I was about to buy an electric wheelchair. I now help people in the UK try out the microcurrent device called the Alpha-Stim. An interesting distinguishing point is I find I can help 70% of people with FM and CFS improve their symptoms but I frustratingly can’t help those with ME. My thoughts are that this is possibly because there is more viral involvement with ME and more neurological and hormonal issues with FM and CFS.
Dr A Gross, is def old school. People with Fibromyalgia do not get better, they get worse. He does not know much about chronic Lyme Disease tho. Chronic Lyme Disease excists and persists in many cases, it is true that people with chronic Lyme Disease develop Fibromyalgia. A lot 80-90%of chronic lyme patients get a ‘Fibromyalgia’ diagnosis, because doctors dont believe in CLD, like dr A Gross. Then they actually misses the underlying cause – that is Chronic Lyme Disease and Co-Infections.
The problem I found is this, doctors do not listen to their patients that “do know” what caused their symptoms.
Dr. Gross gives much misinformation. I have gotten worse, then better, then worse with issues such minor kidney damage, and severe hyper sensitivity to sound and tinnitus. After 14 years (caused by an injection), I am at poverty level. I worked many years at UCSD, School of Medicine in Research. I was always identified as being 15 years younger than my actual age. My brown hair turned white within one month; plus, many other issues of gross pain. I started aging immediately.
I was diagnosed with fibromyalgia, but it was simply that I was poisoned. I continue to work with the “poison” issue, trying to get if out of the body. Not an easy thing to do. I now know my name, i.e., “cognition improved”, muscles improved, all senses improved, except for hearing. Still much pain that I cope with.
I feel blessed to be alive, as I nearly shot myself due to the extreme head pain that caused severe seizures only at night.
I was a meditation groupie since 1965, very particular about what I ate, never smoked, in perfect physical condition, active, rock climber, martial arts, tai chi, qi gong, rode bike, rowed boats, ran 10K’s. I could hardly walk the day after, and for years.
My life has been a nightmare due to this injury that I received no money from. and I still work on it constantly. Ironically, I had an injury in 1968, 8 weeks in hospital, (removal of tonsils and lymph nodes of right groin) several years to really recover, that was similar, yet not as intense. Took only 2 years to recover.
It is interesting that one can earn a living off NIH grants a lifetime and never resolve the problems of many conditions that they study.
My gosh Barbara what a story! You were doing everything right – eating well, in great shape, meditator – you were like me 🙂 (except more so) and still got ill. It’s just amazing.
Hang in there!
Hi Cort, thank you for reviewing the teaching video from Dr. Gross. I had asked you to take a look at it because when I saw him earlier this year, I had said that my FM has changed and I wanted to know if I also had ME/CFS. His response was absolutely. He puts ME/CFS under an umbrella like illness/syndrome with FM as the lead and ME/CFS falling under that umbrella. Dr. Gross shared with me he put this video out and also said to me continue researching and reading. Not many Drs. give that advise but he did.
This is why I asked you to review his lecture which was done for interns and seasoned Drs. in the video you have shared above. He was then approached and asked to share that same video with the public. He agreed. I’m grateful he did because as you mention I think anyone that is new to these illnesses will learn more than many others that don’t see the video. Mostly because he recognizes both as being real. That is often the 1st step to overcome with non believers.
I also think that he touches on many good points as you mention and bring to light. He is very conservative and he did put me on Neurontin 6 yrs. ago and some other meds and I couldn’t handle the central nerve pain without the Neurontin. I shared with him that for me it helps. He is gentle. When he re-evaluated me for FM (long story short old PCP wouldn’t accept when Dr. Fye (the Dr. that Dr. Gross took over for Dx’d me with FM apx. 10-12 years ago) Dr. Gross said yes you have it and by then I had a new PCP. Dr. Gross only touched me in 3 spots and saw my face and said I’m not putting you through this pain again.
I have been going to the Rheumy department at UCSF for about 14 years or so and will continue to keep Dr. Gross as a Dr. with the understanding we have between us that I will also be seeing a local Rheumy for some of my concerns and I also have an auto-immune called Sjogren’s and I feel as if I have something else going on. If I do I would want Dr. Gross in my corner.
As you know I’m very active in support for FM, ME/CFS and auto-immune illnesses. Mostly for support and sharing as much info as I can. Between your article and the 1 hour lecture by Dr. Gross, it isn’t a waste of time in my opinion to get through all this information even if someone needs to break it up into 10 minute segments daily. I think what Dr. Gross and you Cort have shared as a result of you watching his video is very important information that needs to get out and then I suggest to everyone, don’t stop there. Use this as a base for getting more knowledge and even sharing with your Drs. that others suffering see and family and friends that don’t believe FM and ME/CFS are very real indeed. U.S. News named Dr. Gross as the #10 Rheumy in the nation. What he offers is more than what many Drs. have offered to those suffering. I agree that even more information has come out since and I reckon Dr. Gross will one day do an updated video with even more information as time goes by.
In conclusion, Dr. Gross looked me in the eye in front of my bf and said to me, “REMOVE ALL STRESS FROM YOUR LIFE”. He didn’t look away from me until I looked at him without excuses and agreed with him there are ways of doing just that. I wish that was in his information (maybe it is). Sleep is healing. I have finally gotten to a point that mostly I can sleep now and sleep deep. Not every night but very often in a week. I take supplements and my meds, reduced stress (considerably), and added some cooking back in my life weekly and some walking even though I’m mostly bedbound/housebound. I notice I sleep even deeper just doing some cooking even if in a pressure cooker or slow cooker. I’m up and down a little bit and we need this WITHIN LIMITS. If I push myself beyond my limits, it works against me. However it wasn’t until the CFS kicked me in the rear end that the sleep came. Prior to that when before my FM advanced as it has to ME/CFS included, I slept 3 hours for 2 years. I couldn’t do anything. I couldn’t think and I had no life at all. Dealing with both, I learned to sleep whenever my body wants sleep, anytime it wants sleep. Sleep has helped some with pain, attitude, brain fog, etc. I’ve shared much but did so as this time I felt it was the right time to open up and share some of what I have been through and being that Dr. Fye and Gross shared the same department, same hospital and treated me for 14 years. Dr. Gross will still treat me when I need him but now need additional help close to home.
Thank you Cort and hugs to you. I hope your feeling as well as possible and I want to say that your sharing the information that you do is vital to us and I love reading your newsletters. Regards, Eva N. 🙂 hugs
I am so glad you shared your experience with Dr. Gross Eva. I think he does provide important basics and more are more I believe in this: “REMOVE ALL STRESS FROM YOUR LIFE” and that includes for me external and internally added stress (frustration, worry, anger, fear).
It’s great to hear that he’s such a compassionate doctor and it’s great to get a first hand experience of him. These illnesses are very complex and there’s a lot to learn 🙂
My rheum is Morehead,MD at UCSF. She says I don’t have any autoimmune rheum disease cuz I’m seronegative. I’ve been in such debilitating pain for 3 yrs. Working w pain mgmt UCSF David Jun Lee, MD for 3 years. I have bad Neuropathy working w Jacques, MD at UCSF Neuro. Have gut issues. Working w Kathpalia, MD & A pancreatic specialist who’s name I can’t remember at UCSF Gastro. Derm issues too- UCSF Derm, Can’t remember her name cuz of brain fog. Can’t type normally cuz my arm muscles instantly become so fatigued they start burning & burning then the Neuropathy in my hands starts. Sleep probs- been begging UCSF PCP for sleep study for a year. Ditto psych diagnostics & evaluation for dementia (I am 51 w zero Fam history & Grandmother, great grandma, maternal & paternal aunt’s all in their 90’s b4 developing such mild dementia that hardly affected them. No one had any in their 80’s or younger. Both parents 80 years old & zero dementia. I’m a Medicaid patient who gets treated like crap cuz of poor reimbursement rate. I’ll have to ask to switch from Morehead to Gross? Will that even help? His view of accupuncture is so uneducated….also, 1 last thing, UCSF Rheum doesn’t treat osteoarthritis. Period. They don’t accept self refered clients. Period. Your PCP must believe U need a rheum evaluation first. U can’t self refer & pay cash. They r that horrifically over burdened w patients. What else might they do to keep people out so as to not b so overwhelmed??!!…….
May I add a quick note here. I read through the comments as well and I am not saying that Dr. Gross has the treatment down nor that he has all the answers. If you read Corts words very carefully he clearly states that Dr. Gross is on the conservative side. As his patient I can attest to this.
For example: I have Sjogren’s. Last time I saw him which was to discuss many things including that I had the ME/CFS symptoms and he confirmed I do indeed have FM and ME/CFS, we then discussed the Sjogren’s issue. On that issue even though he put me into a worldwide study for Sjogren’s, he was unable to find the paperwork I carry with me almost always. I didn’t have it with me the day I saw him and therefore he said the study proved the 14 nodes taken out from my lip were all damaged and therefore he was unable to address my Sjogren’s that Dr. Fye the Dr. that Dr. Gross took over for said I had Sjogren’s. His comment was to me there was nothing he could do for me for the Sjogren’s even if I had the paperwork that the study Dr. marked as being at a stage 4 of Sjogren’s. No saliva, no moisture on paper put in eyes at all. zero. He isn’t wrong, there is no cure, very little treatment and is treated just like FM, ME/CFS which are symptoms unless it hits our lungs or heart or kidney. That is one of the main reasons I am going to go to another Rheumy closer to home and one that is more aggressive. However, I am defending his work to the date he did that lecture only because he shared that FM (therefore ME/CFS – remember he puts it into the same umbrella as FM) is very real.
Think about this please. Do you remember when you were 1st diagnosed with FM or ME/CFS? 1st it depended upon which Dr. you saw and each Dr. will either label our illness as FM or ME/CFS…they do overlap very much so as I live it. I could have been easily Dx’d 1st with ME/CFS depending on the Dr. I saw. So here I was newly Dx’d 12 years ago and lost and had a PCP that said no way will I allow that Dx. Then 6 years ago again told yes you have FM and this year yes of course you have ME/CFS…I then needed help with understanding. He has a Nurse Practitioner that would meet with me once every couple weeks to teach me or answer questions and just help me accept that I had something else that had no cure at the time and still doesn’t. For a newbie that is Dx’d, Dr. Gross’s information is still good info. As of the date he did that teaching seminar, since then yes much more is known. He needs to do an update. He is very scientific and a little black and white and I know that 1st hand. But I appreciated the video and his teachings because it helped me teach some of my family that what I am suffering with is very real.
I have read almost everything Cort has written and I commend you Cort on how you took this video and sounds like you may have had a chat with Dr. Gross to get more information because you shared even more with us then he mentioned to me or that is in his video. I am grateful you shared this. Some will be helped just knowing it isn’t in their head. Some will be helped knowing that we can do small things very gently to help ourselves to feel better. What needs to be stressed is not to over do things and as Cort said, stretching can and is even better for us than any conventional type of exercise which can hurt us more. Water movements slowly can help us also but in moderation but that isn’t for everyone either.
Thank you for sharing and I’m glad that you did. Yes I am going to see another Rheumy for Sjogren’s due to the pain that illness causes in addition to FM and ME/CFS. I also have a skin condition, my hips and back have been affected and I personally believe my hips and lower back are from having these illnesses and I can’t help but still wonder if a virus triggered all this and in the end will FM and ME/CFS come down to an auto-immune illness? My lower back and hips have become involved.
Best Regards Cort
Thanks Eva,
I have listened to other patients who have seen good ME/CFS/FS doctors and I must say that my general feeling is most of them are missing something. Some don’t do full immune panels, others don’t really know anything about the autonomic nervous system, others don’t do anything about exercise or stress.
I’m glad Dr. Gross is so commpassionate – I’m not at all surprised that he is and it sounds like he goes the extra mile for his patients and I’m glad you’re looking for other options to take care of the Sjogrens. (How about IVIG for that?)
i just turned 60, and I was wondering if any of you had come upon their diagnosis in any way like mine. I’ll try to summarize what I know now were the hallmarks of FM/CFS:
1. Abusive childhood (constant hypervigilance); infectious mononucleosis at 12.
2. Insomnia developed, depression and anxiety increased and by age 35, I was sleeping 2-3 hours/night, nightly pacing the house in frustration.
3. Tried CBT; was told: “Just join groups, get more involved” which increased my guilt and depression because I was too tired to do anything.
4. Back pain/sciatica caused me to leave a job I loved, being on my feet most of the day did not help the fatigue. Surgery in 2005: spinal fusion, L-4/L-5 helped temporarily.
5. Developed unexplained whole body pain–felt like one big bruise. “Take Advil, we don’t give out pain meds for mental conditions, see a shrink” I was told by a rheumatologist. Instead, I went to my family doctor for consultation, and before I could protest, he had given me a flu shot. The flu shot put me in an irreversible tailspin; not only did it ‘give’ me the flu, it exacerbated my previous symptoms where the ‘flu’ never went away. Those of you with FM/CFS know what I mean–persistent sweats/chills, that ‘run over by a Mack truck’ feeling.
6. In 2010, found a knowledgable rheumatologist familiar with treating FM. I was excited and thought I was on the road to recovery.
7. Muscle relaxants, narcotics, and sedatives were prescribed to lesson the pain, but combined with brain fog, dizziness caused a fall from a ladder in my garage and I broke my neck; C-6 and C7. The requisite MRI also revealed groups of follicular thyroid nodules.
8. Blood tests revealed antibodies for Hashimoto’s thyroiditis. If I hadn’t had the ladder accident, I’m not sure if anyone would ever had thought to run a thyroid panel. As most informed doctors now know, symptoms of hypothyroidism overlap or mimic symptoms of FM/CFS as well as other conditions.
9. Pain continued to increase, despite steroid injections, 90 mg Oxycontin twice a day, Skelaxin, Klonopin, Lidocaine patches meloxicam (an NSAID), and 30 mg Oxycodone for ‘breakthrough pain’ every 4 hours with no relief. I was now on a cane and my left leg atrophied, shortened, and began to turn in. I thought for sure it was CRPS. I begged my doctor for a script for an x-ray of my hips, and it revealed end-stage osteoarthritis of the left hip!
10. Last May I had a total hip replacement and the pain was reduced by at least 2/3. Great, but the trauma of surgery is not well-tolerated by FM patients, but I did feel a lot better. I’m still on the same drug regimen (minus the steroids) plus Lyrica, but the narcotics were greatly reduced. Unfortunately the depression is worse than ever.
Sorry this is so long, but I’m sure others have similar stories they would like to get off their chests–misery lives company!
Boy Sally you have been through it! Glad the hip replacement helped – I take it them a long time to do something as an x-ray. That’s unfortunate but I imagine that that happens quite a bit.
Thanks for sharing your story!
Sally, look into heavy metal toxicity from cobalt hip replacement. Watch “The Bleeding Edge” documentary if possible. Good luck, I hope U didn’t get a defective hip replacement product.
Migraines are a huge issue and can cause lesions, per my MRI; therefore, anti-seizure meds are often given to limit the migraines. Social Security Disability is still an act of Congress. I received it once and was given a 5 year grace to try and work…well, I managed to return to work…but, after 10 years – I am worse than before. Now, I have to start all over again. Medicine sensitivity is real. I have had my throat close with an Aleve after a hysterectomy. It was the timing. Vertigo with exercising on certain equipment. ADHD without the HD. Costrocondritis – inflammation from using my chest muscles. Mammograms with pounds of pressure kill me. Sensitive to smell, sound, movement, taste. Surgeries for breast masses. Pre-cancer. Fatigue.