

The Institute for Neuro Immune Medicine’s annual patient conference occurred a month or so ago. It brought news of some exciting growth in a program that’s taking a comprehensive approach to developing new treatments for ME/CFS.
The blog comes from my sometimes hard to read notes. At times I take riff’s on what the speakers say. These two factors add up to this blog being my personal interpretation of what happened. It may not always reflect what the speakers intended to get across.
Dr. Klimas Talks
“We are moving as fast as we can” Dr. Klimas
Speaking from off-site at a surprise birthday party, Dr. Klimas noted that the Institute For Neuro Immune Medicine at Nova Southeastern has grown enormously in the three years it’s been in existence. Employing no less than 34 people, my guess is that it may be the largest single treatment-research effort focused on these types of diseases anywhere.
The Institute is employing the most impressive multi-pronged “bench to bedside” effort to bring treatments to the fore of any group that I know of. Dr. Klimas, started off, though, by giving us a reality check. The answer or answers to any disorder rarely come easy or quickly. Even with a large effort focused on a precise target, the fight to produce effective treatments for hepatitis B still took thirty years.
She didn’t say it was going to take thirty years to find better treatments for ME/CFS. Given the work she and others are doing my guess is that better treatments aren’t that far off – but the wheels of medicine do turn slowly.
[Take the Solve ME/CFS Initiative’s Biovista project begun in 2012. It took Biovista less a year to plough through more than 90,000 compounds, 25,000 clinical outcomes and more than 6,000 biomedical publications – and identify a promising drug combination for ME/CFS. That was apparently the easy part.The Solve ME/CFS Initiative and Biovista announced in 2013 that a two-drug combination – never before used in ME/CFS – had been found. Because the drugs are known to be safe but have never been used together before, the next step was an FDA approved proof of concept trial. That expected to talk with the FDA in 2013 and begin a proof of concept trial in 2014. that obviously hasn’t happened yet. The drug combination remains a tightly kept secret.
This is not to slam the Solve ME/CFS Initiative or Biovista. Coming up with a potential new drug combination within a year is fast work! It’s exciting stuff and it’s taking longer than expected. “Longer than expected” seems to be the norm in medicine. ]
Everything they are doing, Dr. Klimas noted, has been done with the end goal of bringing new treatments to patients. A Translational Research Unit was specifically created to speed up that process – a process that usually must pass through two steps – cell based and animal studies – before it gets to humans. From the time a treatment idea is solidified, Dr. Klimas said, it usually takes three years to get to phase I safety trials in humans.
The Translational Research Unit has a number of treatment strategies they want to move from the bench (research lab) to the bedside (clinic) this year and in the coming years.
They are currently focused on three sets of trials.
- An autologous stem cell study that a donor has offered to completely foot the bill for – is set for this year.
- Trials are coming out of their computational efforts
- Continuing work with Ampligen
Clinical studies underway at the NSU include the big CDC multisite study, a Chronic Fatigue Initiative biorepository and microbiome study, a NIH funded microbial translocation, e.g. leaky gut study, the expanded “Good-day/Bad-day” study and a recently funded epigenetics study.
[We’re seeing some nice coherence in the field with these studies. The CDC multisite study, with its possibility of isolating or starting to isolate some subsets, will surely inform the search for a definition. The CFI’s microbiome study, Dr. Hanson’s NIH funded microbiome study and the Solve ME/CFS Initiative’s microbiome and leaky gut exercise will start to shed light on this complex and possibly critical area. The Nathanson epigenetics study at NSU and Patrick McGowan’s Solve ME/CFS Initiative epigenetics are moving forward at the same time as well.]Giving the CDC Props
As she talked about the Institute’s studies, Dr. Klimas urged some to reconsider their assumptions regarding the CDC. Calling the CDC’s ME/CFS experts study a “fantastic” study she said the CDC was getting a bad rap that it didn’t deserve. The expanded version of the study is going to expand its focus on groups that few research groups have attempted to reach: children with ME/CFS, people who are housebound and people who are just getting sick with ME/CFS.
Business Booming- Infrastructure Catching Up
“Business” is apparently booming. They’re adding an environmental medicine specialist and neurologist. Demand is great. Every time they add a doctor, Dr. Klimas said, their dance card is full within a couple of months. She asked for patience. They’re constantly overstretching ourselves and because of that their infrastructure suffers.
[ Those infrastructure problems have been with them for a long time. Everyone agrees the expertise is there, the tools are there, the empathy is there, but organization has historically been the practices weak point – a very weak point at times.]Training
“We’re working very hard to come with training strategies so that wherever you are you can get good help” Nancy Klimas
Obviously they can only do so much in southern Florida. The real answer, Dr. Klimas asserted, comes in training doctors to do treat ME/CFS correctly and they’re developing training modules to do this.
[That could be a very big deal. Giving primary care doctors training modules is an obvious and much needed step to improving care for everybody. Those training modules could also be folded into medical school curriculums.]Gulf War Illness (GWI) Funding Provides Boost to ME/CFS
It’s the critical mass we had been hoping for, now have in hand, and are pressing hard for the translational studies that follow.” Dr. Klimas
Funding, of course, is everything – and Dr. Klimas has gotten good funding for Gulf War Syndrome. The Veterans Administration has been impressed enough with the Institute’s GWI work, that they’ve asked it grow a whole service using their approach at the VA. That, in turn, is helping them inform their ME/CFS work.
It’s been about twenty years since a remarkably high percentage of young, formerly healthy Gulf War Vets (@ one-third) came back sick and stayed that way. Clearly those patients – despite the fact that they’re male and have a different trigger (chemical exposure) – still, with their similar symptoms and disease prognosis, present some sort of model for ME/CFS.
The Institute’s GWI models were the first to indicate how important a role sex hormones play in these disorders. Once the GWI research opened that door, Dr. Klimas was able to parley those results into more funding to investigate why women with GWI and men with ME/CFS get sick. Those are two groups (particularly the second :)) that need more attention.
Dr. Klimas GWI funding has been good enough for her to adopt a very aggressive computational approach that will allow them to quickly from cells to animal models to clinical trials – beginning this year – if I got it right. A big DOD grant will enable test treatments in animal models of GWI. One GWI treatment trial was in phase I as of September last year. Others are coming.
Couples Needed!
We all know how tough chronic fatigue syndrome and fibromyalgia can be on relationships. Seeing your partner decline, seeing them be unable to partner with you to do the things you used to do, the financial problems that often crop up, the feelings of helplessness and guilt – on both sides – the issues just go on and on.
This couples study – which takes place over the internet/phone – is taking couples from across the country and helping them tackle these issues in an effective manner.
Want to be more peace with your significant other? Want to recover some intimacy that’s been lost? Get on the same page? Enroll in the couples study. They have only three months left to fill up this study.
(Not filling up an NIH funded study, by the way, is not what the NIH likes to see. It’s important for the Institute that the study gets filled.)
Contact – call 305-355-9200 or email at cfsvideohealth@med.miami.edu if you’re interested in learning more. Delores Perdomo is in charge of the study.
Environmental Medicine
Environmental Medicine is another field that sorely, sorely needs more research. If you’ve ever had chemical sensitivities you know how incredibly impactful they can be. The Institute of Neuro Immune Medicine is creating a training program for a fellowship in Environmental Medicine to help investigate this area.
Fertile Ground
Dr. Klimas has clearly found fertile ground at Nova Southeastern and the continued growth of the Institute and the many studies they’re engaged in is encouraging. Now if we can just get the NIH to start funding some Centers of Excellence – one of which would surely be Dr. Klimas Institute – we could really get the ball rolling.
Dr. Klimas ended her presentation on a high note – showing a picture who is completely cured. We don’t hear about them much but there are actually quite a few of them out there. No one should give up hope – it can happen.
Then it was onto Gordon Broderick….
Gordon Broderick
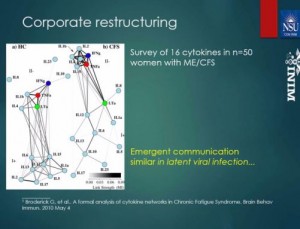
Broderick is all about trying to capture how the systems in our body work. He proposed to view the interactions between these complicated systems as “conversations”. One immune cell converses with another immune cell, for instance, and has it do “X”. Factors such as hormones and cytokines engage in conversations with a wide range of immune and other cells.
Broderick modeling efforts indicate that different types of conversations are occurring in the immune systems of people with chronic fatigue syndrome than in healthy people. Some conversations are “louder”; i.e. – they’re more active. Some conversations are taking place between different players.
Betsy Sue, for instance, – who used to talk only to her buddies before – may be buzzing around now interacting with all sorts of new people (immune cells). Fred – who never got past the doorman before – maybe in the party now. Those altered conversations indicate that the immune systems of ME/CFS patients have been fundamentally changed.
Broderick intensifies those conversations more by having ME/CFS patients exercise. Before, during and after that exercise he takes blood at 7-9 time points to determine a couple of things. He wants to know at one point new players (immune cells) enter into thte conversation and take it in a new direction. He also looks for choke points – points in the system that are getting overloaded with information. (Picture one person in a corner getting shouted at by a crowd.) He’s found that natural killer and B cells appear to have been backed into that corner. They’re getting funneled tremendous amounts of information – more than they can handle – and appear to be getting burnt out.
Whether these changes are triggered by an ongoing pathogen attack, autoimmune processes or some kind of other system reset Broderick did not say. The key thing, though, is that these abnormalities are showing up big-time in his analyses – and that’s good news for a field that’s had more than it’s share of inconsistent immune findings.
Caution Warranted
One of the big questions facing anyone proposing to intervene in this process is whether the altered immune network is protective or the problem. If it’s protecting the patient from a pathogen you might want to actually strengthen parts of it. If it’s simply bollixed up you might want to push it in another direction.
The immune system is so complex, though, that it’s not entirely clear what a healthy immune system looks like. (Mark Davis is studying just this question at Stanford.) It’s not even clear what a normal, healthy immune response to a pathogen like Epstein-Barr virus looks like. That makes it difficult to know if ME/CFS patients system are responding normally or abnormally to a pathogen attack.
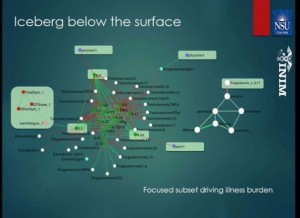
It hasn’t been easy to get this far. It’s taken supercomputer time – lots of it: 10,000 processors humming 24 hours a day for 7 days to do the calculations needed to understand these networks and perhaps how to tweak them back to normalcy.
Broderick is using his computer models to figure out what cytokine he should address first, how much should he should impact it and when he should go after another one – in order to stop ME/CFS patient’s immune systems from going off like an atom bomb every time they exercise.
He has a list of 16 cytokines all of which may respond to IL-2 modification in ME/CFS. Then there’s IL-15 – an NK cell activator – which keeps showing up.
The combination that’s performed best for him is an IL-2 and IL-17 one-two punch. First you take down IL-2 and then you pump up IL-17. According to his models that should help ME/CFS patients recover from exercise. In fact, his models indicate they might get them very close to having a normal response to it.
Of course immune therapy is no joke. Tweaking the incredibly powerful and complex immune system has to be done carefully. For that reason they’re mostly focused on already available drugs with substantial safety records behind them.
Then there are the sex hormones. Their role in modulating the immune system has turned out to be surprisingly significant. Broderick’s is trying to put it all together.
His models right now are suggesting he can get the system back to normal – for a while – but then the effect fades.
The Programmer!
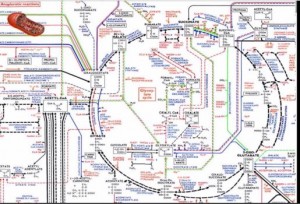
The next speaker – the chief programmer of the Pegasus supercomputer at NSU – began by expounding on the stunning capabilities of his machine. He can do what used to take a decade in a week. He can plug a patient population’s data into the computer and run hundreds of thousands of simulations on it.
It’s this kind of incredibly thorough approach that apparently gives Broderick so much confidence in his data. The data is apparently run again and again and again in every conceivable formulation..
The data suggests that ME/CFS patient’s have become trapped in a suboptimal homeostatic state. Some external stressor – an infection, stress, an injury, a toxin – some event or events – pushed their systems so far out of normal that they can’t find their way home.
The question of how to push them back into normalcy is complicated by the complex hormone-immune interface in the body. They’ve found five different stable homeostatic states in men and eleven in women. Each of these states resists change and only one apparently reflects optimal health.
They’re beginning to get a grasp on what it takes to move a typical ME/CFS patients homeostatic state back to normal. They’ve identified several treatments which, if given in the right amount, at the right time, in the right order, returned the system to normalcy (health) one out of two times. (It took the supercomputer a hundred thousand runs on a million person patient pool to come up with that treatment protocol.)
Calling this stuff “cutting-edge” almost makes a mockery of that word. “Revolutionary” is a better descriptor. How this disease with so little funding got access to this kind of potentially revolutionary technology is anyone’s guess. Broderick, in fact, almost left the field a couple of years ago. A chance meeting with a veteran who expressed his profound thanks for Broderick’s work caused him to stick with the field.
Chance and the human element [plays a big role in all this. What causes Lipkin to take an interest in ME/CFS? Who could have predicted that uber- geneticist and technologist Ron Davis’s son would get ill – pushing him into the field?
Now they’re adding drugs to the mix. They just put in a grant to fit the pharmacokinetics of repurposed drugs into the computer – how fast they break down, what they effect, etc. – into the computer.
It’s a brave new world.
Richard Deth – Oxidative Stress, the Mitochondria and Fatigue
Deth believes the precipitating events (infections, stress, toxins) that trigger ME/CFS produce insults to our oxidative stress systems.
Antioxidants
Free radicals are also a by-product of ATP (energy) production. Antioxidants mop up the free radicals but if antioxidants such as glutathione (GSH) are low then oxidative stress rates are going to go up. That means increased levels of electrically charged particles (free radicals) that go around tearing into and tearing up the membranes of the cells around them in their effort to achieve balance.
GSH, the key antioxidant in the body protects the body in two ways. One, it reduces or tames free radicals – a process that causes it to become oxidized. The key glutathione measure to look at is the ratio of reduced to oxidized (used up GSH). It should be from 20-30/1. Anything less indicates the antioxidant system is not keeping up and increased levels of oxidative stress are present.
Two, if oxidized levels of GSH become too high it will bind to the mitochondria shutting them down. Because dysfunctional or damaged mitochondria can produce very high levels of free radicals this GSH “shutoff valve” is an important way of eliminating both a source of oxidative stress and poorly functioning mitochondria.
The end result of high levels of oxidative stress is termination of the energy production process – and fatigue.
Rich Von Konynenburg
Deth credited Rich Von Konynenburg with making a major impact in his thinking. He noted that Rich Von Konynenburg and Nathan found 50% lower GSH/reduced GSH in ME/CFS patients. When they used the Yasko protocol (B12 and folate) to increase GSH levels and methylation, energy, well-being and mental clarity went up.
[Konynenburg’s protocol was founded on these foundations (from the treatment study):- A stressor (physical, chemical, biological, and/or psychological/emotional) places demands on glutathione
- Glutathione levels drop, producing oxidative stress, interfering with the intracellular metabolism of cobalamin (vitamin B12) and allowing toxins to accumulate.
- A functional deficiency of vitamin B12 is produced, resulting in lowering of methylcobalamin and adenosylcobalamin.
- Lack of sufficient methylcobalamin inhibits the activity of methionine synthase, placing a partial block in the methylation and folate cycles.
- Methylfolate drains from the cells into the blood via the “methyl trap” mechanism.
- An interaction (vicious circle) is established between the partial block in the methylation cycle and glutathione depletion, and the disorder therefore becomes chronic.
- Dysfunctional detoxication and immune systems allow toxins and infections to accumulate over time
Konynenburg believed that
“treatment should be directed primarily at increasing the activity of methionine synthase. The resulting normalization of the methylation cycle, the folate metabolism, and glutathione levels will restore function to the immune system and the detoxication system as well as to a wide range of other parts of the overall biochemistry.”
[Von Konynenburg and Nathan’s 21-person study made in into the Townsend Report but not into a medical journal. The study was successful but lacked rigor, probably because of lack of funding, in some areas. For instance, they used an index of referenced laboratory measures for healthy people as controls instead of healthy controls.Study results with regard to GSH depletion in ME/CFS are actually very mixed. While oxidative stress is consistently elevated in ME/CFS, most studies have found normal GSH levels in ME/CFS (normal glutathione peroxidase, normal reduced GSH levels, normal GSH levels, increased GSH.)
Shungu’s compelling findings probably provide the best evidence that GSH depletion is important in ME/CFS. Shungu found that reduced levels of GSH in the brain were highly associated with symptom severity both in ME/CFS and depression and were negatively correlated with high lactate levels. They suggest high levels of oxidative stress and low antioxidant levels could be shutting down ATP production in the brain. ]
Diet
Diet can play a role as well. Deth explained that the peptides released when you digest gluten (from wheat) and casein (from milk) activate opiate receptors and block the transporter that brings GSH into the cell. As cellular GSH levels fall, methylation is impacted. First it goes up and then it goes down – negatively affecting dopamine production.
Dopamine turns on a receptor that appears to play a central role in producing focused attention. Alterations in dopamine receptor are a risk factor for ADHD (which is probably increased in ME/CFS and FM).
Meanwhile, opiates released in the gut rob the mitochondria of cysteine – a foundation for antioxidant production– reducing antioxidant levels and possibly setting the stage for inflammation in susceptible individuals.
Deth credits this process with the reduction in gut, neurological and immune symptoms that some people experience when they go off milk and wheat products. [Dr. Peter Rowe has found that if his adolescents with ME/CFS are sensitive to milk that getting them off it is crucial to seeing improvement with other treatments. ]
Deth noted that he is not a medical doctor, but suggested that nasal administration of methyl B12 can increase glutathione levels in the brain. Since Shungu has found that reduced glutathione levels in the brain are associated with symptom severity increasing them is probably a good thing.
Jon Kaiser- Synergy Trial
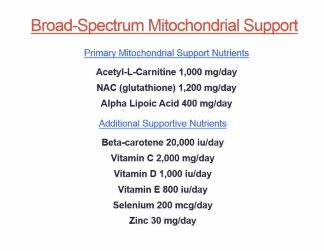
Kaiser’s focus on boosting the mitochondria and immune system in ME/CFS fit in well at this point.
His work in this area dates back decades to the HIV epidemic. The HIV drugs were a huge help but disturbing side effects – many of them due, he thought, to oxidative stress induced mitochondrial damage – began to show up after about five years. He developed nutritional ways to reduce the oxidative stress and improve mitochondrial functioning and it worked. Similar to Deth, he asserted that the number one symptom of low antioxidant levels is fatigue.
Kaiser believes mitochondrial dysfunction is one of the only hypotheses that ties all the symptoms in ME/CFS, Gulf War Illness and similar disorders together.
He noted that a small but apparently well-done study recently suggested that GWI, whatever else it is, may be a mitochondrial disorder as well. Golumb et al’s finding that “mitochondrial response to exercise (PCr-R) was blunted in GWI patients suggested GWI was a mitochondrial disorder. The muscles and brain are particularly affected in GWI because they are the most energetically challenged tissues in the body.
[Phosphocreatine findings including phosphocreatine recovery in ME/CFS have been mixed with most studies not finding significant problems. It’s not clear if the same test done in the GWI study was used, though.Ironically and tragically Golumb suggested that Department of Defense’s attempt to protect the troops using high numbers of multiple vaccines, anthrax vaccine, pyridostigmine bromide nerve agent pretreatment pills, pesticides and insect repellents, and permethrin-impregnated uniforms played a role in the wide-spread health collapses that occurred. Throw heat, depleted uranium tanks/munitions, chemical agent resistant coating paint, oil fires and battle conditions into the mix and you have an unwitting experiment on a grand scale of just how many toxins even a young, healthy body can handle at one time. ]
Kaiser noted that two muscle studies and Shungu’s three studies suggest that ATP problems are present in ME/CFS. The same process that produces muscle cramping during exercise, he believes, maybe reducing blood flows to the brain in ME/CFS.
He used n-acetyl cysteine (NAC) – a critical component for him – to improve GSH levels in his HIV/AIDS patients. Using acetyl l carnitine and alpha lipoic acid to increase energy increases oxidative stress, but animal studies indicated that adding NAC to clean the free radicals up makes a huge difference. (He also suggested that acetyl-l carnitine works better than L-carnitine and that it works better at low doses.)
A 2006 placebo-controlled, double-blinded trial indicated that his micronutrient formula boosted immune functioning in HIV/AIDS patients.
Those mitochondria – they’re pretty complex. Kaiser reported it took him quite some time to come up with a formulation that worked
After that he thought he’d give it a try with ME/CFS. [Got to be easier than AIDS right? Wrong!] After the rapid, positive effects he’d seen in HIV/AIDS did not materialize in his ME/CFS patients, he started rearranging the formula – adding other nutrients, hormones, etc..
It was not until he tried something he’d held off on that something clicked in his patients bodies. Kaiser worried that central nervous stimulants would be over-simulating but instead, in combination with mitochondrial and immune factors, they proved to be simply energizing. .
Energy level, alertness improved rapidly followed by a gradual improvement in functional status. Some patients had incredible results.
After an open-label proof of concept trial produced good results (one indicator of symptom severity approached normality) he moved on, and designed a double-blinded placebo controlled multi-center trial using ME/CFS experts. We are just a couple of months away from results of the trial but he could report that the safety profile was good.
If the results are positive the FDA is the next step. If you want to get the results as they come out send your email address to ask@KPAXpharm.com
Mitochondria
The mitochondria appear to be indeed catching on. Deth and Klimas have written a grant proposal to help them develop a better understanding of the role the mitochondria play in GWI. They will do same for ME/CFS.
A donor has helping the Institute for Neuro Immune Medicine buy a machine to analyze the mitochondria better. We just had a study suggesting the mitochondria play a role in fibromyalgia. Another study suggested they play a role in post-chemotherapy pain. The Chronic Fatigue Initiative may be heading for the mitochondria as well.
Q and A
Glutathione
Deth and Kaiser agreed that NAC is the best way to supplement glutathione. Deth recommended using liposomal varieties of NAC. IV treatments such as a Myers cocktails can help but Kaiser prefers to use the cheaper oral methods.
Kaiser warned that you can throw your system out of balance by taking too much of one supplement. He’s found that his formula has worked well.
His drug/supplement combination includes Ritalin 5 mgs with breakfast and lunch plus 4 tablets of the immune formula. By 8pm everything is out of your system and you’re ready to sleep – which has come easier in his patients. In response to a question he stated he would only increase the Ritalin to 10 mgs/day if a patient saw response after the first couple of weeks.
Every patient may not, in fact, need Ritalin. Kpax’s Immune and energy contains a small dose of caffeine (60 mgs). It’s only about 25% less potent than Ritalin version. Some people have had excellent results. [I am trying the Fatigue Trial Pack. I have had good results. In my hypersensitive state I only need 1 and 1/4 tables not four or five to get results.]
The Ritalin in the Synergy formula “pushes” the system a bit and Dr. Klimas agreed that sometimes you have the push the system a bit – with small amounts of exercise or other factors – to get it to respond.
LDN and Immunovir
An LDN and Immunovir question brought a response from Dr. Klimas that (their in-house) study has shown that it improves NK cell functioning….They are trying to get a grant to get a full-blown study going. She warned that you often have to start very low with LDN and that it may take 4-6 months to see improvement.
Animal Hormones
Both Kaiser and Klimas avoid animal hormones. Klimas suggested anything could be in them and noted that hormones suppress things. If you take an adrenal hormone it will suppress your adrenal hormones. “Don’t do that” she said.
Klimas again asked patients to have hope. She does see home runs and some people do get completely well. [I have a database of about a hundred people who have.]
On the treatment end let’s note several possibilities that have cropped up
- the Synergy trial
- the Open Medicine Foundations Folate/MTTHR trial underway
- the Rituximab trial
- the two-drug combo trial from Solve ME.CFS and Biovista
- the INM’s stem cell trial
- the continuing Ampligen trials
- the trials that will come out of the INM’s models
And probably more…















Wow, Cort, that report and your ability to make it exciting and somewhat understanding is fantastic. Add in the results of Simmeron’s pilot study and we have so much to look forward to very soon. I had no idea about how many studies are producing such promising results. Good stuff and lots of reasons to be hopeful, so thanks so much for all you do to keep us informed.
Thanks Lynda, it does seem like we have some momentum building. I think a combination of patience and excitement, if that’s possible makes sense 🙂
Cort, Thank you so much for writing another great article. This was easy to process for a non-scientist, and you truly helped shed a light of hope… I don’t really want to wait another 3 years, but 3 years can go by very quickly. 😉
From this article, I wonder if I don’t have (not only ME) but GWI. Like the veterans I was exposed to 2 powerful vaccines too closely together which got the ME ball rolling. A concussion, and then a major insecticide poisoning. Hit the ball out of the park. Not only MCS, but super-sensitized to any insecticide. (Including topical flea meds, which makes life complicated: “Please keep your dog away”…).
I have had ADD/ADHD my entire life, and was only properly diagnosed in my 30’s. Only in the past year or so has my PCP permitted me to go back on Concerta, then Ritalin (now @ ~5 mg tid). I argued it was a quality of life thing, so that I could read again. It has been hugely beneficial – except when in a real flare, the Ritalin can’t help with reading much. My experience with Ritalin and Concerta regarding supplements and caffeine comes with a caution. I have found that combining Ritalin with caffeine has to be monitored very carefully – thus I’m a little wary of the KPAX formula. I take a tiny amt. of caffeine in the morning (with decaf), if I take too much I get irritable and a bit hypomanic when taken with Ritalin. And, that leads to a sickly crash feeling.
I’d also wonder how the L-glutamic acid (in the immune formula) might interact with Ritalin.
It would be great to have a protocol for PCPs.
Thanks again 🙂
Fabulous reporting of some really complex science. You make it graspable even to get he brain fogged! Finally real scientists are working on this who have gained enough depthful understanding of the complicated functioning of the neuro immune system to even ask useful questions.
We owe Rich K a real debt of gratitude for his cogency, patience and persistence over so many years, starting with his glutathione hypothesis and bearing fruit in these methylation results just before he was taken from us.
Glimmers of hope just as spring is threatening to arrive and melt all the snow! May it all be so.
Thank you for the comprehensive reporting! I have tried so many of these protocols with no relief from my CFS. I have not tried the KPAX Immune & Energy with the other supplements.
Any comments on that protocol? I’ve had CFS for 12 years now, have tried Meyer’s Cocktails IVs for years, Vitamin injections, Gamma Gobulin shots, LDN, Hormone Therapy, Imunovoir, many, many supplements and special diets…..the list goes on.. but I will never loose hope.
Thank you Cort, for your amazing work!!
I’m going to have a blog on it soon…..I’m a bit different than most. For years I tried everything and nothing worked then suddenly many things worked except as I got more energy I would relapse and fall into a fluey state. So I respond well – for a short time anyway…So far so good with KPAX
Cort…
KUDOS, KUDOS, KUDOS
Absolutely amazing…can only process so much at a time, but…this brings such hope!
As always, my hats off to you! At 66 I am moving up on my third decade with this
illness.
Bless you…Linda
hi Cort,
Thanks for all the hope. We need it! I was wondering about those supplements you are trying. Do you have to see Jon Kaiser to get them? Can anyone try them? I sure would like to.
Sandra
The KPAX formula with caffeine in it can be bought through KPAX. I’m going to have a blog that describes it better actually…
Thanks for replying, Cort. Are you using the immune and energy pack or what? There are several supplements at KPAX. i know everyone is different but it would help me to know if you don’t mind sharing the information.
Thanks,
Sandra
I am trying the fatigue trial pack – http://www.kpaxpharm.com/vitaminsandsupplements/immunesystemboosters/FatiguePack
this is the one Kaiser said is similar to what is used in the Ritalin – mitochondrial booster trial.
The energy tab has 60mgs of caffeine in it – about half a cup of coffee. Since I am supersensitive to caffeine I asked him what to do about that and he said
“Both formulas contain essentially the same mitochondrial support foundation. In addition, the Energy formula contains a stimulant component, which consists of caffeine and tyrosine. This acts to augment the treatment’s effects.
In ME/CFS, the mitochondria (of many bodily systems) are dysfunctional to a varying degree. As you know, there is a great deal of variability in the severity and sensitivity by individual.
Some people may only need “Mitochondrial SUPPORT” which can be provided exclusively by K-PAX Immune 4 tabs twice daily.
Other people need and/or can tolerate what I call “Mitochondrial REJUVENATION” which I liken to the need for their mitochondria to be “jump-started” with a little more “juice”. This has proven safe in my clinical experience because of huge dosages of the mitochondrial support nutrients being present.
The key is really for each individual to fine the right balance of the two products for them.
Your Options
1. K-PAX Immune 2-4 tabs twice per day by itself
2. K-PAX Immune 2-3 tabs twice per day with an occasional K-PAX Energy taken when it’s really needed.
This is the reason that the caffeine is only in K-PAX Energy. So each person can take just the amount of “juice” they need to keep them both functional and feeling good.”
Cort:
Do you consider that these K-Pax Immune supplements would help with Fibromyalgia, especially in light of the Mitrochondrial/Fibro connection.
Thanks,
Lorraine
Hey, If they work in ME/CFS I would be shocked if they didn’t work in fibromyalgia.
Time will tell.
Thanks so much for taking the time to write all of the KPAX details, Cort. Very helpful information. I look forward to your future blog about it.
Sandra
Cort- I am wondering how this would work with POTS patients. Or is it rec for them.
Great article and great facts.
Thanks for all your efforts and help.
Carole
Thanks for all the great info Cort. I look forward to your blog on K-Pax as it looks like a typical good vitamin to me and if the highest dose of the trial pack is taken that’s a huge amount of Vit. A.
Cort, I got tired last night and didn’t read to the very end of your blog and read the comments first today. (bad idea.) :-). I see now how K-pax has been carefully formulated. It’s still a bit of a concern to me given the recent info coming out re higher dosages of all vitamins, even the natural form of A, but then our bodies aren’t typical so it’d be great if this works for us…
Betsy- I have been on 4 drops Micellized Liquid Vit A .5000 IU daily for about 3 years. with 25 IU of beta-carotene/ take it with adrenal supplement for support as my adrenal were not functioning at all. Can tell a big difference
in energy level. Also take Purple juice (cell signaling factors.) These are all mixed into high PH Spring water.
Cannot take the Myers Cocktail. Don’t know why. Just shuts me down.
I am interested too if anyone has tried Enteragam for SIBO issues?
Great info here.
Thanks Cort
That’s interesting Carole – thanks for letting me know and I’m so glad your energy has improved. I’ve never heard of the purple juice, high PH water or Enteragam – will look them up, thanks.
Carole, with your adrenals not functioning at all, I’m assuming you were put on hydrocortisone (Cortef). When I went on an adrenal supplement (bovine adrenal extract), it was not sufficient to increase my cortisol. I’m hoping that using both Cortef and the K-Pax one month trial kit will have me feeling more ‘alive’.
Cort, does your database of the 100 people who have recovered from CFS/ME, hold details of how they recovered. Are a proportion of these through psychological therapies like Lightning process?
Thanks for all you share with us,
Suella
Yes, it includes how they got better. People get better through all different means. For one person, believe it or not, sinus surgery did it. Others do it through diet, through supplements, through antivirals, mold avoidance and mind/body practices and others. I think the mind/body practices are probably the most prevalent but it runs the gamut.
I am going to be releasing them in the new Forums package coming out soon. We have a recovery story sections in it.
Great. Thanks for sharing this. I look forward to see your new forums package.
Suella
Thank you Cort for this article I had missed the article you wrote “Is Fibromyalgia a Mitachondrial Disorder” glad you mentioned it here, I look forward to catching up. With many trials coming to fruition I’m hoping we all get what we need to help us heal, among other things I would like to ride my bike again.
That would really be something – being able to ride the bike again. I would love that. You never know….
It’s wonderful to see so much good news! :’) Thanks for reporting!
Thanks for all you do Cort! Your articles offer hope…we need much of that.
I’m wanting to clarify something –
“Both Kaiser and Klimas avoid animal hormones. Klimas suggested anything could be in them and noted that hormones suppress things. If you take an adrenal hormone it will suppress your adrenal hormones. “Don’t do that” she said.”
Would this also mean prescription hydrocortisone (Cortef) or does the comment relate to only supplements such as Bovine Adrenal Extract etc.?
My sense was that for Dr. Klimas it extended to hydrocortisone but was particularly aimed at the animal hormones. She did mention, if I remember correctly, a patients whose adrenal hormones were turned off by the use of prescription hormones.
Some doctors use them and others do not. Some of the doctors who do not are very against them. It’s a gray area in my experience. I’m sure others know more about it than me, though.
Cort
I think I’ve mentioned the following study quite a long time ago:
http://www.wellnessresources.com/studies/inflammation_and_fatigue/
I’m not aware of any CFS researchers looking at this avenue. Which would seem a pity. This compelling study would seem to suggest a potential model for CFS. And then treatment options (blocking CCL2 signalling…drugs exist for this or are in development….)
I emailed the Calgary researcher a couple of years back and CFS didn’t seem to be on his radar.
Any chance of raising it with the ‘Elite CFS researchers”???
I like Nancy Klimas she is Always so optimistic but i doubt that we will ever get better. It gives hope for new patiënts, not for us. I even don’t think we will see a real breakthrough in our life and ever now what really causes our disease. Sorry, but i am not so optimistic. This disease is much, much to complicated and invisible.
Gijs, As a thirty year sufferer, I knew this years ago. I knew, if I was ever going to have any sort of a life, I would have to find my own solutions. Through research, and an understanding of what was happening in my own individual case of ME/CFS, I have found ways to control my illness. However, what works for me probably wouldn’t work for someone else. There are so many variables with ME/CFS; so many different things going on in each sufferer. In fact, I don’t believe that we all have the same illness. So, how are they going to find a one-size-fits-all solution, for an illness they don’t truly understand, and is unique to the individual?
I agree, I am happy you can ‘çontrol’ your symptoms. 30 years that is long me almost 20 years. Good luck!!!
Thanks Cort,
I so wanted to go to this but couldn’t and have been dying to know what was said. I was surprised the various forums weren’t buzzing about it since to me there was so much crucial information discussed.
I have tried all sorts of supplements over the years and the mitochondrial supplements that I have been taking for the last 5 months or so have really made a difference. I’ve tested whether it really is the supplements by ( accidentally) running out every so often and after about 5 days I go downhill. I get more and within about 3 days of replenishing my supply I start to recover again. I especially notice a difference in brain fog, headachy, tired brain feeling.
I take the 3 supplements in the KPAX formula – acetyl-L-carnitine, NAC, and alpha lipoic acid but also take 4 additional mitochondrial supplements: ribose ( my most important one), coQ10, creatine and magnesium.
I wonder why these four are not in the formula? They are also essential for mitochondrial dysfunction and are included in protocols by Dr. Myhill and others and also by mitochondrial disorder specialists.
The main issue I have at the moment with my protocol is that it costs about $300 a month. Because it is not a drug it is not covered under my drug plan. If this KPAX formula got FDA approval does that mean it would be considered a drug? Would that mean we could get it prescribed and it would fall under a drug plan?
Claire, I saved quite a bit on my ‘micronutrients’ by doing online Swansons vitamins. I got the N-acetyl Cysteine, Acetyl-L-Carnitine and Alpha Lipoic Acid all for under $30. I’m on SSI disability so I know how tight we have to be on our treatment choices. At the same time, after the recent discussion of dopamine & glutathione, I also got the acetyl-l-tyrosine. I am taking Resveratrol for the leptin/microglial issue and have just resumed the 1.5 mg LDN in 1 liter of water, a teaspoon for now. Apparently I am allergic to the LDN so we’re working on desensitizing. So at this point I’m doing all I can do, in conjunction with my Primary Dr, Alt Med Dr and LDN pharmacist. Now if we could just find out what those 2 drugs are from Biovista…
Yes, if you look at KPAX’s web page about insurance it does look like the ultimate goal would be the Synergy protocol covered by insurance. I suspect that Dr Kaiser, having had CFS for some time, is also very aware of CFS patients trying to cover supplements from disability checks. But for insurance purposes the Synergy vites would have to be prescribed by a Dr. Most private insurances won’t, maybe the RX coverage with Medicare’s RX people. I have not enquired. But I did see that if a customer faxes their Medicaid card along with a Dr’ s RX then that might bring a 20% discount. That,my friends, is called empathy. And compassion. And I am awed.
Hello Flora,
K-PAX does offer a 20% discount to anyone on disability, no doctor prescription required. Furthermore, we do offer a heavily discounted “Fatigue Pack” for individuals to try the over-the-counter regimen in the most affordable way possible. For people who have sensitivity to supplements, you can always call and request a sample.
K-PAX believes that in order for a mitochondrial vitamin formulation to work best, it is necessary for it to be a complete formula (i.e. a broad-spectrum supplement) rather than taking individual, isolated vitamins. This is necessary as the components act as precursors to one another and create the synergistic effect.
Secondly, the quality of the ingredients is vital for optimal absorption and benefit. K-PAX uses the highest quality pharmaceutical-grade ingredients available.
The ultimate goal for the Synergy Protocol is to have it covered by insurance which would require FDA approval. It is our hope that with a positive outcome of the Synergy Trial we will be able to move towards FDA approval for this innovative treatment and in to the hands of those who need it most!
I am a case study of 1 – but it’s going well for me so far.
By helping you so far, does that include PEM or was that never much of an issue for you?
PEM is a huge issue for me, and yes, the KPAX formula has definitely helped. Other things have helped in the past. The big question for me is whether my strange reaction to improved health kicks in – and I’ll be to keep on taking it. For me, it’s quite a potent formula.
I got mine today Cort. A new doc gave me Ritalin ( main PCP never would let me try it, only the ungodly expensive provigil) so I got the immune formula. I thought it was interesting that the Ritalin isn’t added for energy but to help the body accept the nutrients although I wonder how that works… and, if it helps with energy, we’re not supposed to act on it. Easier said than done but I can only hope I’ll be confronted with that challenge. :-).
Hi Cort –
I include the link below to an article from the Science Based Medicine website. Risking sounding like a climate change or evolution denier ( I am neither), the truth is I’m not a scientist or researcher and would appreciate comments or edification from those who are. As you say, you’re a study of only 1 person. I, for one, would like more reliable information before I invest my limited time, money and hope in this product.
Also, when will the Synergy trial results be made public?
Thanks
http://www.sciencebasedmedicine.org/a-nutritional-approach-to-the-treatment-of-hiv-infection-same-old-woo/
For sure Jody – I think they’ll be available within the next couple of months – not long.
Thanks for the informative link Jody – those are questions I have about this formula but maybe science will catch up with it…
For treatment of ME/CFS, that is actually caused by an over-active immune response (autoimmunity) resulting in sickness behavior (malaise, fatigue, inflammation), I believe we should be looking into the Suppress the Immune System trial.
Hi Cort,
l have been on LDN for 4 mths now starting at 1mg and now up to 4mg. l have noticed that during the last 4 mths when l have relapsed l have not gone into a full on fluey state. It seems to be stopping that from happening. l also am not going into the deeper relapse coma like state that has happened many times and the last episode was in august last year. l have been also putting together supplements for myself that l have seen others take and going by this article l am on the right ones. l cannot take carnitine though it makes me feel as if l am going to have a stroke. My liver marker was high so l went off vit A but will look into the drops as mentioned in the comments. l do feel hopeful now and encouraged that there is some light at the end of the tunnel and getting closer. Just need my brain to work better so l can read more now.
Thanks so much, l have been following your articles for ages now but not always able to comment due to serious brain fog and fatigue. Cheers, hope you have success with formulas. HOPE 🙂
Thanks SO much for your exciting and extraordinary writing. It is so encouraging to know you are out there, researching, consolidating and writing it for all of us. You communicate and write very well and you should be very proud of the great contribution you make to our lives on a daily basis. After 34 years of this, and at age 69, I don’t expect to be well in my lifetime, but when I read your information I get really excited and hang on to the hope that I could at least feel and function better!!! MANY, MANY thanks for your genuinely “bright” spot in our days.
Thanks Connie..
You never know what’s around the corner…
Dear Cort,
Go ahead, SURPRISE US!!!! :o) Thanks again, profoundly.
Cort, thank you for your thorough coverage of the NOVA/Neuro Immune Institute’s patient conference. Your ability to distill and translate such complex concepts in to material for all to understand is remarkable. We appreciate your support of the Synergy Trial and are eager to answer any questions your readers may have. If any one would like updates on the results of the trial as they become available, please forward requests to: ask@kpaxpharm.com
I have severe brain fog and struggle to understand complicated treatment, supplement and methylation protocols. So I never really try anything anymore. LDN has been helpful for my pain but can someone tell me clearly what to order and take from Kpax? I would really like to try something. Do I need to buy two products- Kpax immune and Kpax energy and take as below?
With Breakfast:
K-PAX IMMUNE: 2 tablets
K-PAX ENERGY: 1 or 2 tablets
With Lunch (before 3pm)
K-PAX IMMUNE: 2 tablets
K-PAX ENERGY: 1 or 2 tablets
There are so many supplement options that it is overwhelming. If I try this combination is it enough to make a difference or would I need to add more supplements?
Elizabeth, the above combination would be considered the K-PAX over-the-counter Fatigue Protocol. This does include two different products: the Immune Formula and the Energy Formula taken together. Alternately, some people choose to mimic the actual Synergy Trial protocol under their doctor’s supervision (using the Immune Formula with a RX for methylphenidate).
There are representatives at K-PAX Pharmaceuticals (877-777-5729) who would be happy to review the Fatigue Protocol with you and to answer any specific questions about the Synergy Trial protocol or the over-the-counter version. We realize this can be overwhelming and we are here to help!
Deidre, Indeed the representatives at K-PAX are very helpful. I ordered the fatigue pack through Anne 2 days ago. She was very informative and patiently answered my questions. For some of us who are often experiencing intense brain fog while communicating via phone, the kindness of staff can make or break our day.
Thanks Rita – good luck!
Rita,
We are very happy to hear that Anne was of good assistance to you. Please feel free to call back with any other questions. We wish you best with your trial of the Fatigue Protocol.
Boy isn’t that the truth Rita re kindness of staff. I’ve always wondered why doctor’s offices or similar places don’t make that a necessity in hiring – it makes such a difference. Indeed the K-PAX reps are great.
Although we may have been in the same room I think I was at a different conference! Thanks so much for ‘chunking it down’ into digestable pieces!
Hi..
thanks for sharing your valuable insight with us. This is really very helpful for me.
please keep sharing such informative blogs.
It’s interesting that a stem cell study is in the works. I’ve wondered if this has been looked into for CFIDS after reading that David Foster’s wife was in Germany getting a stem cell transplant. She has Lyme and sounds like can barely leave the bed. Some people commented they think she has something else going on because she’s been so very sick for so long.
growing for fine mind, the reception is getting better. Do not think I walk around constantly in euphoric state, absolutely not. A negative slant, I have always had, and cynical defeatism still simmers in my genes. But less and less often takes the upper hand is replaced by positive things. It is sometimes given Brainfocuspill to people who are deep in the well, to write something every day, which was positive. Whether you are grateful for. The idea is, if you persist long enough, you will automatically notice more positive things. And if your thoughts are slowly bent toward the positive things, and not downward into the pit. Thus, this section also works. Each week to reflect on something beautiful or more appreciation came on .
http://brainfocuspill.com/
Hello, this blog is very useful for Health!
Thanks for giving this information.