



(Many people haven’t connected histamine with fibromyalgia or chronic fatigue syndrome but it’s been a suspected player for over twenty years. The first study suggesting overactive mast cells were pumping high levels of histamine into FM patients bodies goes back to 1990. Greatly increased levels of mast cells in the skin of every FM patient tested in a 2010 Spanish FM finding, and then a small but successful NIH funded mast cell blocking FM study featuring ketiotifen suggested the theory might have legs. One patient in the trial remarked that she was pain free for the first time in years.
Meanwhile, Tufts University professor Theorharis Theorharides proposed stress induced mast cell release could be causing ME/CFS and other disorders and got a rare NIH grant to try and prove it. He noted that two helpful drugs, amytriptyline and doxepin elixir, just happen to have histamine reducing properties as well. He’s gone on to develop a series of histamine blocking nutraceuticals.
We also know that mast cell activation can cause postural orthostatic tachycardia syndrome (POTS). Biaggioni described a process by which mast cell activation (MCA) caused orthostatic intolerance, particularly in patients who experienced ‘flushing’, (POTS). In a small 2005 study . In fact Biaggioni found he could produce histamine associated episodes of flushing, shortness of breath, headache, lightheadedness, excessive urination, and gastrointestinal symptoms (including vomiting) simply by having some of his POTS patients exercise or stand for extended periods of time.
Dr. Klimas has called the mast cell theory one of the more intriguing and promising immunological theories to come along. It’s hard not to come to the conclusion that histamine and mast cells play a significant role in at least a subset of patients with FM, ME/CFS and POTS. Learn more about the research and possible treatments in
Now fibromyalgia patient Darden looks at histamine from a different direction – our diet and gut -and relates the effects an anti-histamine approach have had for her. )
A Histamine Overview
Histamine is a potent signaling molecule or biogenic amine made from the amino acid histidine. It is naturally found in plants and animals. Histamine helps regulate many bodily functions including digestion, sleep, sexual function, and blood pressure, and in the brain it functions as a neurotransmitter, carrying chemical messages between nerve cells.
Under normal circumstances small amounts of histamine help to facilitate health and balance in many systems of the body. In response to foreign pathogens, wounds and allergies, however, large quantities of histamine are released in our bodies by mast cells and basophils – two types of white blood cells that reside in blood and tissues respectively. People with allergies often take antihistamine medications to provide relief of symptoms associated with this inflammatory response.
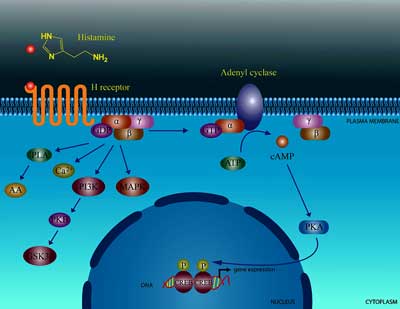
Histamine exerts its effects by binding to four different receptor sites on cells. Each site is able to produce different symptoms by impacting different tissues and organ systems. (See diagram below).
Because antihistamine drugs block histamine from binding only to its H1 receptors – they are not effective at countering all histamine-related symptoms.
Histamine and Diet
Histamine is found in a variety of foods. When ingested it is broken down by an enzyme called diamine oxidase of DAO found in the lining of the small intestine and the upper end of the large intestine. In the central nervous system, histamine is broken down primarily by histamine N-methyltransferase (HMT).
Reduced DAO activity in some people’s intestines can result in high histamine levels and a condition called Histamine Intolerance. These excess amounts of histamine can cause a wide variety of symptoms including low blood pressure, headache, sleep disturbances, diarrhea, heart rhythm problems, acid reflex, hypertension, vertigo, anxiety, flushing, runny nose, asthma, hives, flushing, itchy skin, painful or irregular periods and fatigue.
DAO is produced in very high concentrations by the placenta during pregnancy, and as a result women with Histamine Intolerance often report a remission of symptoms when they are pregnant. That’s an intriguing finding, of course, given reports of similar symptom remissions in some women with ME/CFS.
An association between estrogen and DAO levels, resulting in a decline in DAO levels and a worsening of the symptoms of histamine intolerance in perimenopausal and menopausal women also exists.
Histamine Intolerance
Histamine Intolerance is often misdiagnosed as food allergies, eczema or Candida. It is, however, an IgG, as opposed to the IgE mediated response that occurs in allergies.
The symptoms caused by histamine intolerance are dose-related; the amount of histamine present causes symptoms only when they’re above a certain threshold. (This is another important difference between histamine intolerance and allergies.)
The idea of histamine intolerance was initially conceived in Germany in the 1980’s. A Canadian Immunology PHD and dietician named Dr. Janice Joneja has also done a lot of research on this condition.
Reduced DAO levels can be caused by gastrointestinal conditions including small intestinal bacterial overgrowth (SIBO), Crohn’s disease, gluten intolerance, ulcerative colitis and inflammatory bowel disease. Alcohol and many medications can interfere with DAO activity and some evidence suggests low levels of DAO and HMT can be inherited.
Histamine Producing Foods
Dunwoody Labs is currently the only laboratory that tests for DAO levels. The accuracy of their test has not been thoroughly validated, however, and is based on studies performed on rats. Most experts agree that if one avoids foods that are high in histamine for a couple of weeks and the symptoms clear up, then it is likely that one has histamine intolerance.
Histamine levels are only known for some foods, however. Unfortunately, some lists of histamine releasing foods on the Internet are based on subjective reactions instead of objective scientific information. In general we know that alcohol (red wine has particularly high levels of histamine), fermented foods, black tea, cured meats, aged cheese, and ripe fruit and tomatoes, and many medications are high in histamine. (Histamine is a byproduct of fermentation when bacteria or yeast are added to foods or when foods ages, ripens or spoils.)
The foods that individuals react to vary and sometimes a person can become increasingly intolerant to more and more foods. Along with avoiding foods high in histamine, taking a supplement that contains DAO obtained from pigs 15 minutes before each meal can be helpful. An Austrian company called Sciotech Diagnostic Laboratories (www.sciotec.at/en) is the only producer of DAO micropellets. They market a product called DAOsin in Europe and they sell micropellets to a few American companies that produce their own DAO supplements. Those companies include Swanson (DAOsin), Seeking Health (Histamine Block), and Xymogen (HistDAO). Not all people with Histamine Intolerance benefit from taking these supplements, however.
My Story
My particular food and drug sensitivities began at the onset of my health condition forty years ago. I suffered from chronic tension headaches, which I eventually resolved by doing EMG biofeedback training on the muscles in my neck and eliminating alcohol, caffeine (I drank black tea), drugs and sweets.
Over the years, though, I became increasingly sensitive to more and more foods and wound up eliminating citrus and dried fruits, soy sauce, aged cheese, cured and smoked meat and fish, and tomatoes.

Darden noticed that some foods left her fatigued and experiencing muscle tension and heat – sensations and unable to sleep well
My reactions to these foods began within several minutes of consuming them and lasted 24 hours. During that time I experienced elevated muscle tension, felt uneasy, and had very disturbed sleep often associated with a feeling of heat.
I have never discovered an antidote to this reaction and simply have to ride it out; It often leaves me exhausted afterwards and I may need several days to fully recover.
Although there are some things that I can never consume without a reaction there are many that I can tolerate occasionally as my threshold is variable. I did not have these reactions when I was pregnant and my condition worsened as I approached menopause and has stayed about the same since that time.
My food and drug reactions do not correspond to any allergy testing whatsoever. In the early 90’s I underwent a year of electrodermal allergy treatments at the Tahoma Clinic, then several years later I did a year of Nambudripad’s Allergy Elimination Techniques (NAET) treatments, and more recently I tried Advanced Allergy Therapeutics. I experienced no improvement in my condition with these therapies. Last spring I discovered that I have Small Intestinal Bacterial Overgrowth (SIBO) and began treatments that have improved my digestion and overall health.
I wrote a post about this last fall and received two independent responses from persons that have SIBO and also Histamine Intolerance, a condition I had never heard of. Looking into this subject I quickly realized that the foods and drugs I react to are high in histamine and that I have inadvertently been on a low histamine diet for years as a way of managing it.
My naturopathic physician ordered a test to measure my DAO levels from Dunwoody Labs, the results of which are still pending as the lab is revamping its procedures. I had a phone consultation with Wendy Busse, (www.HistamineReducingDiet.com) a Canadian nutritionist who worked closely with Dr. Janice Joneja.
In terms of my particular reactions, Busse said that every person is unique however the fact that I am without symptoms when I adhere to my diet and that I did not have symptoms when I was pregnant is pretty strong evidence that I have Histamine Intolerance. She was skeptical about the validity of the test performed by Dunwoody Labs, however, because histamine levels in the blood fluctuate a lot.
Two months ago I started taking 2-4 HIST DAO capsules 15 minutes before each meal. HIST DAO is manufactured by Xymogen (www.xymogen.com) and contains DAO micropellets and a small amount of ascorbic acid (vitamin C), which is an antihistamine. The instructions on the bottle are somewhat misleading: “Take 1-2 capsules no more than 15 minutes before the consumption of histmaine-rich foods, or take as directed by your health practitioner.”
Busse says that according to ScioTech, the DAO micropellets are only active when taken 15-30 minutes before eating. Taking these supplements has not allowed me to expand my diet but it seems like when I have a reaction it is less severe and I have not become sensitive to additional foods.
My health has been on a gradual trajectory of improvement for the past seven years due and adding DAO supplements seems to have contributed to this trend. Since taking HIST DAO I’ve experienced better sleep, energy and muscle function. As an experiment I discontinued taking them for 5 days and I did not feel as well.
It appears that Histamine Intolerance and Small Intestine Bacterial Overgrowth (SIBO) are overlapping conditions. This makes sense because DAO is produced in the lining of the small intestine, which is also the location of the bacterial overgrowth.
A number of studies show an increase in the activity of mast cells in persons with fibromyalgia and chronic fatigue syndrome. I think that histamine intolerance may play a role in sleep disturbances in persons with CFS & FMS because histamine is known to modulate sleep and histamine releasing neurons produce a wakefulness firing pattern.
The research on histamine intolerance and its connection with other health conditions is, however, preliminary at best. It’s possible, though, that it is a key player for many persons with CFS and FMS. An experimental trial on a low histamine diet and then taking DAO supplements before meals is a reasonable approach as it may yield improvements in one’s health.
- Check out Darden’s posts on Health Rising
- Check out her website here.







Hi Cort~
I appreciate you writing about histamine intolerance. I also have histamine intolerance and have written about my experience on my blog. http://www.youseasonwithlove.com/blog-posts/
I also have a lot of resources listed on my resources page: http://www.youseasonwithlove.com/resources/
Giving up foods high in histamine (along with taking antimicrobial medication) has helped me a lot. And while I’m not well, I am functioning the best in the 11 years of my illness.
Besides histamine, I also seem to be sensitive to foods high in putrescine. And unfortunately, I have also reacted badly to some foods that are not high in histamine (oats, rice and egg yolks come to mind).
I suspect that the viruses and other pathogens have caused the food intolerances. Prior to getting CFS I could eat anything and I was very healthy!!
At least I’m feeling better (as long as I don’t eat a problematic food) and with time I hope my body will continue to heal and I will feel even better.
All the best to you,
Tina
Hi Tina,
Nice to hear you are make some headway with this protracted illness. I have a daughter, just 19 now who has had CFS for 6 years already. She functions at a very basic level. I am curious about your onset..can you identify the ‘beginning’ of the illness? A specific event, or gradual? I am curious as I am trying to get a grip on whether the type of onset results in a different journey. So complex! I will check out your blog soon but wanted to catch you whilst the conversation thread was fresh.
I wish you always 10 steps forward and only 1 small step back! Unfortunately life is never all forward motion.
Linda
Hi Linda,
My condition began at the age of 19 – 41 years ago. I’ve been successful at managing many of my symptoms. The specific diet, which turned out to be low histamine diet was something I figured out very early on. Other therapies that have been crucial are Oral Systemic Balance, reversing Wilson’s thyroid syndrome, LENS neurofeedback, treating SIBO and now taking DAO supplements. I am able to lead a very stable and functional life at this point with no fatigue. Check out my blog http://www.fibrofriends.typepad for more specifics on the treatments that helped me.
Hi Linda~
My illness started 3 weeks to the day after I got a steroid shot to my knee. Looking back, we think that shot reactivated a pathogen in me (likely bacterial based on what happened after that). Then, it appears, viruses reactivated (based on labs and symptoms). So, I know exactly when I got sick…but I could still function (at least most of the time). Then I gradually got worse and worse until functioning was very difficult.
Antibiotics and antivirals have both helped me. About 2 years ago I began to explore the diet end of things. Since my background is nutrition, and I worked as an RD for a number of years I knew something about food intolerance. And I really didn’t think I had any….but I was very wrong about that. I am so surprised that food is a pretty major player in my health.
I am so sorry for your daughter’s illness. I wish her a full recovery….and soon! I have 4 kids and my heart would just break if one of them had this…..so hugs to you….and your daughter!
Tina
Great to hear Tina…
I am going to “cook up” (ha ha) a histamine resources page as well and I will be sure to get your blogs on there.
Such an interesting disease this is….
Hi
could you share the difference between histamine intolerance and Mast Cell Activation Disorder/Syndrome?
Thank you
Rebecca
That’s a good question and others probably know better than me. I do know that mast cell activation syndrome can affect many different cells. In MCAS there may be too many mast cells and/or they may degranulate easily – releasing histamines and other factors into the blood stream.
From what I gather from Darden’s blog is that the effects of histamine intolerance – too much histamine in the system coming in from the gut – can be similar but I don’t if the two disorders are strictly related or not.
When the mast cells degranulate they release histamine and im learning they are connected somehow.
Here’s a link to a website about Mast cell activation syndrome or mastocytosis. http://www.mastocytosis.ca/ Mastocytosis is a rare condition where the patient has an overabundance of mast cells and/or mast cells that are excessively active. The symptoms are more severe than Histamine Intolerance. Histamine Intolerance is not caused by an overabundance of mast cells or over active mast cells. It is caused by a deficit of the enzyme DAO found in the intestine, which breaks down histamine in foods and drugs.
Oh boy! This blog keeps coming up with new findings that make so much sense in my own experience.
The role of stress; the suffering of excess body heat as a symptom; the “inadvertent cures” that bring improvement:
“…I have inadvertently been on a low histamine diet for years as a way of managing it…”
Me too!
And I never heard of this term before:
“Postural Tachycardia Syndrome” (PoTS)
I note that the medical term really relates to symptoms provoked merely by standing up. But they say “1/3 of people with CFS have PoTS”. Only 1/3?
I say they are not thinking broadly enough about this phenomenon. It is exactly what I have been describing as the unwarranted outcome of numerous “stress positions” which I had hypothesized as restrictions in blood flow in inelastic myofascial tissue. While many people might not be so bad that they experience PoTS merely by standing up, I believe that it will be found that everyone with CFS and Fibro, will be provoked into episodes of PoTS by adopting “stress positions”, at a threshold far below that of healthy subjects.
For example, there are numerous stretch exercise positions that trigger obvious PoTS episodes in me (I had no term for it and have referred to them as “breathlessness and heart pounding”) within seconds. For example, quad stretches or squats. Merely going into the position itself.
I have been frustrated all along that I am physically strong, with big muscles, yet merely going into certain positions put me into a state of semi-collapse in no time. I can do a seated leg-press of 2.5 times my own (high) body weight and yet I can’t squat! I can pull quite some kilowatts on a rowing machine yet stooping from the waist (because I can’t squat) to check tyre pressures is exhausting! I can win arm-wrestles against strong young fellows but holding a paint-brush out perpendicular to my own body and using it for 1 minute is exhausting! Of course I end up being accused of malingering by my own family!
If this is an identifiable medical condition that is on its way to being solved it will make such a difference to my life!
I have been improving recently with a massive, time-consuming, costly “all of the above” regime that may well just have an “inadvertent cure” or two in it. I still say PACED exercise has been of major significance. Doing stretches that I can’t do otherwise, with my weight supported by water, particularly in a hot spa that pre-warms the muscles. I have slowly been increasing my tolerance for those stress positions, so that “PoTS” takes longer to set in. And massage therapy that works on the myofascia. And other things that I have already bored the readers of this blog with too much.
Really interesting Phil. You have a finely tuned understanding of how your body is responding.
I agree with this. I think POTS or a similar condition is much more common in ME/CFS and FM than believed.
“I say they are not thinking broadly enough about this phenomenon. It is exactly what I have been describing as the unwarranted outcome of numerous “stress positions” which I had hypothesized as restrictions in blood flow in inelastic myofascial tissue. While many people might not be so bad that they experience PoTS merely by standing up, I believe that it will be found that everyone with CFS and Fibro, will be provoked into episodes of PoTS by adopting “stress positions”, at a threshold far below that of healthy subjects.”
If you haven’t read the stuff Peter Rowe is doing on “Neuromuscular Strain” in ME/CFS – I think it will fit in there as well.
Cort! Thank you very much for referring me back to that article on Peter Rowe’s work. I had not read that before. That absolutely fits with what I am hypothesizing about myself.
He describes a vicious circle effect that makes total sense, and on the other hand, the possibility of reversal of this vicious circle into a virtuous circle also fits exactly with the improvement I am experiencing.
“…This in turn increases the load on the peripheral nerves, making them less able to elongate, more likely to be associated with reflex muscle guarding, and therefore more likely to sensitize the nervous system to further stresses…
“…Conversely, as I am able to modulate the autonomic dysfunction and improve lightheadedness and other symptoms with medications directed at POTS or neurally mediated hypotension, Rick and his PT colleagues are able to treat people more effectively, often because the tissues are less irritable. We speculate that there is an interaction between the autonomic nervous system and the movement restrictions, as has been observed in other physical therapy research on adverse neural tension and the sympathetic nervous system…”
YES! But it is not prescription medications at all that are helping me. It would be nice to have one that hurried things up a bit!
“…the upper body in particular is often affected by these neurodynamic problems in ME/CFS. From my sternum upwards it feels rigid and kind of frozen. I have no doubt that this area of tension and rigidity makes it difficult for me to take deep relaxing breaths…”
YES! I used to tell my doctor that my lungs felt like a large balloon inside a small box that stopped them inflating as much as they should!
“…manual forms of physical therapy have been quite helpful for improving overall function, especially when people had not done well with exercise-based therapies alone. The exercise ended up being “too much, too soon.” After the areas of restricted movement have been treated, people find that they can tolerate gradual increases in exercise without as much post-exertional worsening of symptoms. This then allows them to obtain some of the expected benefits of regular exercise…”
I feel so ridiculous, saying all the stuff I have and claiming I have never read that! I honestly hadn’t…! That just “IS” me over the last few months! And the “too much too soon” exercise, was me for the previous 25 years!!!
The thing that is frustrating me now, is that the exercise of sufficiently low intensity to not provoke the post-exertion worsening of symptoms, is so low intensity as to require a LOT of time spent on it to provide benefit.
I really feel for people whose threshold is so low that maybe there is NO exercise that is enough to help them improve? Scary, scary thought. I have been fighting through pain for 25 years staying active, so have probably kept my threshold “high enough” in spite of all the perpetual post-exercise damage I was incurring.
Now I have read the comments on the Dr Rowe article, I see a story of a bedridden CFS victim who worked up from 2 minutes per day on the recumbent exercycle to 1 hour, in the course of a year. This is encouraging for others who are this bad.
My threshold was high enough already when I discovered pacing, that I could go almost indefinitely at moderate intensity, walk, bike, swim, whatever. It is just a question of sacrificing enough time every day to reap definite improvements in my condition. My income has suffered over the last few months as I have grabbed this potential life-line, exercising instead of following up my clients and filling my days with appointments. We have had an amazing summer, which could not have been better timed, though. I have walked and tramped many of the trails that my region is famous for, that I have never been on before! My neglected Moulton bicycle has been dragged out, serviced and is clocking up miles like it hasn’t ever before.
This fits my experience as well!
YES! I used to tell my doctor that my lungs felt like a large balloon inside a small box that stopped them inflating as much as they should!
I wonder how many people experience this. It’s another symptoms that is rarely described but I’ll bet that it’s common.
Me also. I do have (controlled by inhalers) asthma x many years. However I noticed my lungs don’t expand the amount they should. People in the past noticed this when teaching me meditation. It fills like I have a tight corset on (those poor unfortunate women in the 1800’s).
Four years ago I was sent to the respiratory clinic at a major hospital. Had all kinds of tests done. Really didn’t show any problem at all but I was put on oral medication as well as the inhalers I was already on. Didn’t change a thing.
I did read somewhere that this is a common complaint of people with ME. Our intercostal muscles, for whatever reason, are weak.
I’ve had success managing my blood pressure irregularities with Oral Systemic Balance. The therapy is very expensive and time consuming but directly relates to all of this. Check out my post: http://fibrofriends.typepad.com/fibro_friends/oral_systemic_balance/
I remember one time, I was feeling sick in a flight when going back home, and along with that, a lot of pain (as always). I took a Dramamine for the sickness feeling and I realized that my pain got really better.
Right when I got home I started researching about it and saw that Dramamine belongs to the class of Anti Histamines. I found a lot of material about histmine intolerance, mast cell and fibromyalgia connection. For a moment I thought I’ve found the cure hehe.
I even took the medication again to test sometimes. It really felt like my pain got better with it… But nothing conclusive. I try to look my diet and read about it but it as you said on the article, the informations are totally mixed up.
I was trying some other stuff at the moment and thought “one thing at a time” so I ended up dropping that.
But what made me really wonder was that when I drank alcohol I used to get something like 80% pain relief. But sometimes I got all red (like REALLY bizarre red) on my face and chest and strong heart palpitations. I was thinking, could that be something like the histamine intolerance even though alcohol still works as a relaxer?
Also, for people with fibromyalgia alone (no CFS) it’s though that exercise made them feel better… But exercise also releases histamine so…??
Folk~
Most alcohol (especially red wine) is high in histamine. They symptoms you describe could be because of histamine intolerance. Or it could be another substance in the wine giving that symptom.
How do you do with fermented vegetables? Soy sauce? Those are also high in histamine.
All the best,
That reaction I described was more with distilled beverages, but then again I drank much less wine then those.
I never did really well with soy or soy sauce! But mainly gastro intestinal problems, don’t know if they made a difference on pain. I didn’t pay attention on it, and now I don’t eat soy, but certainly eating chinese food or something loaded with soy sauce used to gve GI troubles!
“…for people with fibromyalgia alone (no CFS) it’s thought that exercise made them feel better… But exercise also releases histamine so…??”
Hmmm, I am a fibromyalgic who claims to be benefiting from exercise.
Perhaps the careful pacing of this exercise that I am doing is also the secret to releasing less histamines?
I have also found this on another article about exercise and histamine release:
“…Warming up properly can help to decrease symptoms…”
I am pretty much every day, not exercising until after I have been in the spa pool doing my stretching routine.
But does this histamine-release hypothesis too now make a lot of sense to me! Besides the post-exertional damage to muscles that I was experiencing from exercising too intensely in the past, I often did have a diabolically itchy rash around my midriff. And I have mentioned in my comments that my body temperature would be elevated and I would be sweating, for hours afterwards. It all seems to be related – the things that made me reluctant to exercise, included the social inconvenience from the sweating and related body odour, and I also put the rash and itching down to the prolonged sweating. Now it all makes sense that it was histamines all along!
I never suffered from the asthma-type effects though, but my breathing was consciously restricted from the effect Cort describes on an older thread, of my lungs feeling “boxed in” within a too-tight rib cage – the sensation being tight muscle fibre and lack of mobility in the spine and ribs. I don’t know whether I am mistaken and this actually IS histamine/asthma related; Cort’s explanation (with Dr Peter Rowe’s help) made more sense to me.
Strangely I don’t sweat at all.
If there’s a bunch people in a hot place and I’m sweating, you can be sure the rest of the people are drenched.
With exercise is the same, before I decided to stop exercising totally, I could walk and run and would sweat almost nothing…
Although that lack of breath/lack of stamine (not histamine hehe :D) was true to me. It was incredible how I couldn’t run for ten minutes straight even though I was in good shape, good nutrition and could stay underwater for something like a minute….
I meant stamina
Amazing how different we can be, yet presumably with fibro and CFS, there is a common mechanism disabling us.
I have a friend who is like you, almost impossible to provoke him into a sweat with heat and/or exertion.
But you still have the fibro lack of stamina?
Another guy commenting a couple of weeks ago, said that his threshold was high enough to be able to run, so he does run. It is “running faster” that puts him over the threshold. I think he hinted he is quite skinny, which would be a major advantage in terms of the load on the cardiovascular system from running. I am a big build and terribly inclined to pile on weight with the slightest dietary indiscretion.
If someone is collecting the information about the completely different types of physiques involved with fibro sufferers, surely it should help to start eliminating causes and co-factors and arrive at the one that is common in all cases? I still believe it is chronic stress, but maybe there is a factor that precedes that, that creates the vulnerability to the stress?
Well I’m not sure how’s my stamina now or anything since I became a mess…
For 8 years all I had was pain. For me it was like “Fibro equals pain and that’s it”
6 months ago I started having gastric problems and everything went downhill. Brainfog, vision problems, MUCH more pain, huge fatigue (Which I’ve never had before)…
Now I don’t even know if I have Fibro or ME/CFS, or both, or if they’re the same… (Depending on the doctor I choose to follow… cause I”ve heard them all)
But I ensure you: It is not chronic stress…
About CFS, it’s pretty much common thinking now that is even a contagious disease, they just don’t know how, how much, why, or when (it’s CFS after all… haha)
I know I can run right now, but afterwards I would probably die… haha So I don’t even test my stamina but I’m sure it’s worse than before…
I used to think I had lack of stamina just because I wasn’t a sportsman, but then I saw that some guys like me, or even some guys and worse shape, they could run nonstop for like ten minutes and I would have to give it all to do that so I realize now that it was probably due to my Fibro….
It’s pretty confusing…
hello – can you point me in the direction of the blog you reference above re: boxed in/too tight ribs? i am having this issue at the moment and wonder if it is due to some of the issues described in this post. thank you ,much!
I’m another with SIBO leading to other food sensitivities, including amines. Which amines exactly I don’t know, but I strongly suspect histamine. It’s difficult to explain to people who urge me to treat my gut problem with the fermented stuff that is so trendy just now (kombucha et al). I don’t doubt these do help those without this particular chemical sensitivity, but not me – and yes I have tried them.
On a diet low in FODMAPs and amines my GI symptoms and my scary night-time cardiac arrhythmia have disappeared, my energy is back and I can think again – most of the time. I appear to have other chemical sensitivities as well and it’s hard to avoid all of them all of the time, but in general I am much better than I was.
Darden, I would be interested in how you treated your SIBO. I had a very expensive course of Rifaximin (not funded by the Govt here in NZ) which worked for a while but my SIBO has now bounced back.
Check out my post about SIBO. http://fibrofriends.typepad.com/fibro_friends/2014/07/small-intestine-bacterial-overgrowth-a-complication-of-chronic-fatigue-and-fibromyalgia-syndromes.html
I also have a pretty stubborn case of SIBO that requires lots of maintenance. Between courses of Rifaximin I take Allimed, which is pretty effective and a prokenetic drug called Reslor.
Darden~ Thank you for sharing your story and your blog. I am going to take a closer look at SIBO for myself.
I wish you increasingly better health!!
DAO also breaks down other amines so eating foods with them will lower the histamine tolerance threshold.
I also have/had SIBO. Treated with Xifaxin & Neomycin for a month at a time, with additional herbal antibiotics on the side….then rechecked, repeat etc. After close to 8 months on this regimen, I switched to multiple herbal antibiotics only. (Also- LD erythromycin is a permanent prescription.) Almost a year into it I finally had a “clean” test. It took a very long time to tame it— and there were also significant dietary adaptations. Paleo, no FODMAPS, very low sugar.
For the record, I had slowly developed food sensitivities 10 to 12 years before the final blowout which led to a diagnosis of ME/CFS. Started with dairy intolerance, then soy, then gluten…. (Oh the ice cream sundaes I used to be able to put away!!!)
From my own experience I’d say treating SIBO isn’t a hasty or easy fix. The “diet” is worth maintaining though, to try and prevent it from coming back. I do feel somewhat better than before, but I still clearly have ME/CFS. As I was only recently declared “cured” of SIBO, it remains to be seen if it will come back to haunt me. I’m hoping such a long treatment course will have kicked it to the curb permanently!
Good luck Lissa!
@Lissa, if you wouldn’t mind sharing, could you please tell me what dose of Erythromycin & what herbs? One week ago I finished a two week trial of Xifaxan (550 mg 2xday). I am taking probiotics now, but am sliding downhill fast. On the Xifaxan, I had 3-5 times the energy. I can’t believe what a difference it made in my energy level! (I had very little to begin with, maybe 4 hours a week.) Evidently, the Xifaxan isn’t going to be enough, so if you wouldn’t mind sharing what herbs you took, I would appreciate it. Also did you take probiotics? Thanks.
Check out the website: http://www.siboinfo.com
A year ago I researched mast cell disorders and histamine intolerance and how it may be working with my own ME/CFS. For me, it come to nothing for now, below, but it certainly seems connected–and of course everything is in our bodies. It also seemed to explain a couple of incidents of severe abdominal cramping accompanied by a drop in blood pressure. I’ve had POTS, so I knew what the blood pressure drop was but didn’t understand why it would happen after eating cashews. Food allergy tests showed no problem with that food, too. I have had allergies since childhood but food allergies (more and more) only in adulthood. I have had ME/CFS since 2003, developed Interstitial Cystitis (IC) in 2006, and chronic h. zoster/shingles in 2009 for which I’m still being treated with the highest/acute dose of Acyclovir and still have break-through flare-ups. I see Dr. Chia, and to help boost the Acyclovir he added Cimetidine, which is generic Tagamet. Cimetidine is a Histamine2 blocker, so it works on mast cells, a bit differently than anti-histamines but similar enough that it helps all of my allergies and IC. Hearing all this at my regular appointment, Dr. Chia was supportive of my interest in seeing if I have a mast cell disease and sent me to a local immunologist. He did a baseline tryptase test and I was most surprisingly smack in the middle of the normal range. I know many who read this can relate, but I was so hoping we’d find something that was obviously blood-testable wrong that could be treated! We did find deficiencies in my immune system with IGG tests, and that was validating, but I will meanwhile wait for more of the dots to be connected between all of these conditions. Because of the IC I had to cut out many beloved foods, but I’m thankful for the Cimetidine which makes a few of them possible in very limited, infrequent amounts IF my other allergies are not flaring and my over-all health is on the better side. If I’m less well or allergies are flaring, I don’t dare get close to the smells of those foods. I also carry Benadryl and an Epi-pen with me at all times. My immunologist/allergist and I discussed how I should share the information with other physicians and he settled on “severe sensitivity” though conceded that it could be an allergy. He also said that this is a very new field and that he thought much would be done in the coming decade.
Hey Carollyn! The tryptase test isn’t conclusive if it’s normal. I have POTS and finally got diagnosed with Mast Cell Activation Disorder last year.. they did blood tests including the tryptase, histamine, etc. And yeah my tryptase came back normal. The histamine though came back slightly elevated, but I also did a 24 urine test for leukotriene E4 that was insanely off the charts. These were the first tests to really come back abnormal! My doctor wrote a great post about how MCAD/MCAS is diagnosed. I really encourage you to find a doctor that can test a little more. Being treated for MCAD has really given me a huge quality of life boost. Cromolyn has really changed my life. Best of luck!
http://www.dysautonomiainternational.org/blog/wordpress/a-tale-of-two-syndromes-pots-and-mcas/
Thanks, Megan. I’m glad you’ve found relief and improvement.
I may circle back to this some time. As we all find our way, I am on the trail of another treatment right now, with the usual high hopes after some initial positive response. TBC!
Could you share the name of your doctor?
This all makes such good sense to me. I eXperienced all the above when i was sick in the 1980s. I am better now and think i also probably found inovertant solutions. Maybe this can eXplain some of the comi g and going aspects of otherwise myztery symptoms. I remember i could write my name on my Skin in Hives just by running my finger over my skin. Someone did say at the last Invest in ME conference that that was not allergy it was histermine intolerance but i didnt know what they meant. I had severe POTS at the time and trackycadia and had a heart monitor test for 48 hours which didnt fi d any structural ab ormality but the a duty now s continued for a time and stopped when i got better. I still sometimes try before axis flushing and wierd sweats but at 71 am heaps fitter than many of my contemporaries and i consume lots of vitamin C now
thanks to your post perhaps i know why.
Phillida, not many people on this subject, say “I am better now”.
I agree that you probably found inadvertent cures, but I want to ask you and anyone else who says “I am better now” – have you somehow gained emotional peace about everything, the past, unalterable stressors, etc?
One practitioner I stay in touch with says this is the most important thing. But there does not seem to be any file of “success stories” that says, “psychological change x” has cured “data set y” of fibro victims.
One thing I have got from this blog, is that the chronic pain and tension is part of a vicious circle that itself acts on the part of the brain that controls worry, and so on. How has anyone broken out of that purely psychologically, if anyone has?
I think gaining emotional peace is probably very helpful. I am working on it! Being upset and disturbed is just more exertion for a whacked out nervous system to heal in my experience.
I caution that we all be gentle with ourselves about the “emotional stressor” theories. We are human, and in that are challenges physical, emotional, psychological, whether we have full health or very limited health. The breaking down of our physical bodies is part of this human condition, though it is of course a terrible thing that some of us encounter this at ages we imagined would be our “prime.” Making peace with this change and loss may preclude somewhat better health–but some thinking about the “emotional stressors” leads to blaming the sick for their illness, as if they/we are not doing something right, as if doing it right would mean we’d be healed (by now!). Look at how earnest all of us seekers are in our replies! Looks at how hard we look, all of the tiny shifts we celebrate and hope are turning a huge corner! I don’t think we could find a group of people more hopeful and diligent to improve their health. If how humans deal with “emotional stressors” were chief in determining their level of health, our whole world would be disabled. If dealing with “emotional stressors” were enough, we’d all be well by now.
Thank you, Carollynn – that is what I think too. I tell the practitioner concerned – where is your evidence, your data set of cured fibro sufferers from having got some of this inner peace you are talking about, from a shrink, a shaman, whoever? If anything has been said to work for anyone, you can bet other fibro sufferers would be all over it.
I would say that everyone who has made progress, like I have, does have a positive frame of mind as an essential building block, but it is the multiple actual physical-medical strategies that we have done so much research to discover, that truly help. And it can’t be placebo effect, because if it was, absolutely anything would have helped, and there would be more people claiming one magic bullet had done it for them. What I am seeing all the time, is people saying “I have tried everything, and here are the 3/4/5 or more things that seem to help me when I am doing all of them”.
I think there is a lot of hurt done because of the arrogance of ignorance of mainstream medical practitioners who want to blame the patient every time their big-pharma coloured pill does not work.
Oh so much I can talk about on this subject. Not only do I have HyperPOTS but also MCAS (mast cell activation syndrome) and along with this comes what we call the trilogy EDS (Ehlers Danlos syndrome). For some reason so many of us have all three. MCAS is very unpredictable. There is no rhyme or reason. As for foods, most of us will have things that will always trigger a response. But sometimes things that don’t usually bother us -will. We don’t usually test allergic to anything, yet can react to everything. Exertion can for sure cause a degranulation. As something as simple as a position change. Highly emotional or stressful situations can cause an issue. Which can include pleasurable things – including sex. As mast cells degranulate, as Cort said, they release more than just histamine. They release other things that can increase inflammation response. FMS – anyone???? For those of us with MCAS it’s hard to catch as for testing. There are test but you have to get to a lab within an hour have certain test done and start a urine collection immediately and keep testing for 4 hours. Most of us feel so horrible when it’s a bad reaction, we don’t have the energy nor brain clarity to get ourselves there to get tested. So thankfully some of our docs have recognized this and are treating us with great success. The treatment is to block as many of the histamine a as possible. There are three kinds that meds can successfully suppress. H1s by Allegra, H2s by Zantac and if needed H3s by Singular. There are other brand names that will work. But Allegra and Zantac work best for me. Singular doesn’t agree with me. I take these two nightly. Some of us have to have a mast cell stabilizer the one I use is GastroCrom. I recently tried to go without it and that was a major disaster of a trial. It makes a huge difference. It affects the immune system and helps me to be better all the way around. Since MCAS affects so many functions of the body, including mood, digestion, energy and pain levels. It’s worth taking a look at. Since I have one of the hardest subset types of POTS to try to live with. Anything to make it better is much welcomed.
Since I also have a protozoa that is similiar to Lyme and the way you address it is with antimalarial herbs/drugs and antibiotics (doxycycoline) this also addresses the immune system. The last two years of addressing this along with becoming a lowfat, whole food vegan – has changed my life. I’m functioning and sometimes don’t even qualify to have POTS now. I have reversed Chronic Kidney Disease and everything on my labs have improved. I have a life now. Seldom do I participate in any forum now. I try to help individuals when I can. But I no longer feel the need to do endless research. Those that know me know how much I love science and I go deep into the functioning of the body when I get on a project of research. I feel like I’ve got it figured out. Do I still have issues? Yes, I’m still unwell. But I think I’m the best I can be with what I’m dealing with. I hope that continuing to address these things will continue to improve my function. For now, I’m extremely happy with the direction things are going.
I recently found that I must stay on the low dose antibiotics and antimalarial herbs, turmeric and my MCAS meds. Without them and if I slip to much on my diet all the old Uck starts to come back.
Issie
Significant relief from POTS from quercetin. It’s the only supplement/nutraceutical that has ever helped me so much and so quickly. I first used Querca Max from Clark’s Pharmacy where I get ketotifen filled and within a week, I no longer needed midodrine. I had to take midodrine before I got out of bed and now can get out of bed before taking my first quercetin of the day… Now I take Neuroprotek because it has luteolin. Querca Max is similar to D-Hist and both contain quercetin dihydrate.
Gastrocrom reduced systemic inflammation but took many months at full dose of 8 vials a day and recently raised to 12 vials a day (seems to help even better).
After adding ketotifen, livedo reticulitis faded signficantly and bone pain significantly lifted.
Singular is a given for me.. used it since CFS started… which also started with an attack which I think was my first mast cell attack.
H1-H2 helped with exposures and use daily as recommended to keep things calm as possible.. and add in more to control “break through” attacks.
Anaerobic threshold was at pulse of 85. I feel it’s better now but still a huge exertion wall and now it makes a ton of sense that this is exertion anaphylaxis (as opposed to exercise anaphylaxis).
I wonder how far treatment can get me. This seems huge to me and the idea of microglial activation might be connected to mast cell activation… glad Dr. Theohardides is going there and really find it it interesting that there might be a leptin connection to mast cells as well. I hope Younger will look into this.
I also find it interesting that several of Shoemaker’s markers may have connections to mast cells and I do think that at least some people with mold illness have MCAS or a form of mast cell activation. TGF-b1 and I think MMP-9 are released by mast cells. C4a may trigger mast cell activation through C5a receptor. C3a is a very potent anaphylactoid and directly triggers mast cells. VEGF is released by mast cells as is leptin, it seems. There is a VIP relationship I think but might be inverse.. off top of my head.
I think CIRS is MCAS or they are connected.
Could you please specify what exact protozoa you got infected with and how it happened if you know? What antimalarial herbs do you take? They checked me for Lyme and bunch of other stuff- nothing shows up.. ( 8 months ago I got infected with something at the dentist’s, they treated me with different antibiotics, when I got worse, the docs said it’s probably a virus… my life turned into hell..i can barely take care of my toddler …and am very sick now with constant body/ bone aches…
whatever infection it is/was triggered my fibromyalgia..( I am sure that if any fabromialgia patient thinks carefully, s/he can link it to some infection or stress… Thanks a lot!
Forgot to mention – it has been found by some MCAS people that Tagament blocks the DAO enzyme and could potentially make MCAS worse. Many of us switched over to Zantac or Pepcid. I find I can only use 1/2 or it makes my stomach hurt. But 1/2 for me is enough.
Another thing of interest is I had a doc tell me to never take an H2 blocker alone. He said to always take an H1 with it as the H2 would convert into an H1 and cause it to be worse. So we have the combo treatment.
Issie
Interesting, Darden,
I have MCAS, POTS and EDS (all diagnosed by lab work/testing supporting clinical diagnosis). Recently discovered I have SIBO. I have not started treatment for SIBO. I have been treating mast cells since maybe fall of 2014? Not sure. After upping sodium cromolyn to 12 vials a day, I feel a significant relief in inflammation. I have a slightly expanded exertion capacity but a definite wall. I also take h1-h2, ketotifen, and neuroprotek.
I am very curious about a potential connection between mast cell activation and microglial activation. I found a few articles (by the same authors) explaining a potential connection. What’s interesting is that many of the supplements/herbs that address microglial activation also address mast cell activation or release of specific mediators from mast cells. Neuroprotek contains quercetin and luteolin, which can impact mast cell and microglial activation.
R
Would love to have links to the research you found on the connections.
Issie
http://www.fasebj.org/content/26/8/3103.full
The emerging realization is that glia and microglia, in particular, (which are the brain’s resident macrophages), constitute an important source of inflammatory mediators and may have fundamental roles in CNS disorders from neuropathic pain and epilepsy to neurodegenerative diseases. Microglia respond also to proinflammatory signals released from other non-neuronal cells, principally those of immune origin. Mast cells are of particular relevance in this context. These immunity-related cells, while resident in the CNS, are capable of migrating across the blood-spinal cord and blood-brain barriers in situations where the barrier is compromised as a result of CNS pathology. Emerging evidence suggests the possibility of mast cell-glia communications and opens exciting new perspectives for designing therapies to target neuroinflammation by differentially modulating the activation of non-neuronal cells normally controlling neuronal sensitization, both peripherally and centrally. This review aims to provide an overview of recent progress relating to the pathobiology of neuroinflammation, the role of microglia, neuroimmune interactions involving mast cells, in particular, and the possibility that mast cell-microglia crosstalk may contribute to the exacerbation of acute symptoms of chronic neurodegenerative disease and accelerate disease progression, as well as promote pain transmission pathways. We conclude by considering the therapeutic potential of treating systemic inflammation or blockade of signaling pathways from the periphery to the brain in such settings.
Mast cell stabilizers, while suppressing development of hyperalgesia, do not address microglia. Glial inhibitors commonly utilized in pain models rely on their anti-inflammatory properties; issues relating to nonselectivity in targeting one cell population and risk of either acute or cumulative toxicity could hamper their chronic use. Our incomplete understanding of mechanisms underlying the induction and maintenance of neuropathic pain has hindered more effective treatment, including elucidation of a mast cell role and how these two cell types might interact.
The information discussed in this review makes us aware that much remains to be learned about signaling mechanisms that regulate neuroinflammation and that targeting regulators of neuroinflammation may prove to be a useful therapeutic strategy capable of affecting a diverse array of nervous system disorders. It also raises the question of whether we are missing important therapeutic avenues by studying glia and mast cells in isolation from each other. Future studies should investigate the role of mast cells in inflammatory diseases as a network, which requires a critical examination of specific tissue localization, function, and dynamic interaction with endogenous cells.
Another article: Chronic Microglial Activation and Excitotoxicity Secondary to Excessive Immune Stimulation: Possible Factors in Gulf War Syndrome and Autism
http://www.jpands.org/vol9no2/blaylock.pdf
Abstract
Communication between the immune and nervous systems depends a great deal on pro-inflammatory cytokines. Both astroglia and microglia, in particular, constitute an important source of inflammatory mediators and may have fundamental roles in central nervous system (CNS) disorders from neuropathic pain and epilepsy to neurodegenerative diseases. Glial cells respond also to pro-inflammatory signals released from cells of immune origin. In this context, mast cells are of particular relevance. These immune-related cells, while resident in the CNS, are able to cross a compromised blood-spinal cord and blood-brain barrier in cases of CNS pathology. Emerging evidence suggests the possibility of mast cellglia communication, and opens exciting new perspectives for designing therapies to target neuroinflammation by differentially modulating the activation of non-neuronal cells normally controlling neuronal sensitizationboth peripherally and centrally. This review aims to provide an overview of recent progress relating to the pathobiology of neuroinflammation, the role of glia, neuro-immune interactions involving mast cells and the possibility that gliamast cell interactions contribute to exacerbation of acute symptoms of chronic neurodegenerative disease and accelerated disease progression, as well as promotion of pain transmission pathways. Using this background as a starting point for discussion, we will consider the therapeutic potential of naturally occurring fatty acid ethanolamides, such as palmitoylethanolamide in treating systemic inflammation or blockade of signalling pathways from the periphery to the brain in such settings.
http://rstb.royalsocietypublishing.org/content/367/1607/3312
From article above: Mast cell stabilizers, while suppressing development of hyperalgesia do not touch microglia. On the other hand, current glial inhibitors for pain largely rely on their anti-inflammatory properties, and carry issues, such as non-selectivity in targeting one cell population, while risk of either acute or cumulative toxicity could hamper long-term use. (this is not true. list of natural microglial activation inhibitors from Jarred Younger: Luteolin, panax ginseng, tumeric, resveratrol, gastodia elata, obovatol, inflexin, piper gadsura, ganogerma lucidum, berberine, epimedium brevicornum, isodon japonicas, stephania tetrandra, stinging nettle, fisetin, pyncogenol, boswellia, kratom. (Several of these including panax ginseng work on mast cells.. I have not gone through entire list but I know luteolin, tumeric, resveratrol, stinging nettle, pycnogenol, boswellia impact mast cells)
4. Mast cells and glia: are you talking to me?
Oh, east is east, and west is west, and never the twain shall meet
Rudyard Kipling, The Ballad of East and West (1889)
Mast cells and microglia would appear to be an exception to this. Indeed, a number of potential contact points exist between these cell types, and include: Toll-like receptors (TLRs), especially isoforms-2 and -4 (upregulation of cytokine/chemokine release and recruitment of immune cells to site of injury); purinergic (ATP) P2 receptors (e.g. IL-33 from microglia binds to its receptor on mast cells and induces secretion of IL-6, IL-13 and monocyte chemoattractant protein 1 which, in turn may modulate microglia activity); proteinase-activated receptor 2 (PAR2) (e.g. mast cell tryptase cleaves/activates PAR2 on microglia, resulting in P2X4 receptor upregulation and brain-derived neurotrophic factor release, while IL-6 and TNF- from microglia can upregulate mast cell expression of PAR2, resulting in mast cell activation and TNF- release); CXCR4/CXCL12 (promotes microglia migration and activation, and in microglial cells CXCR4/CXCL12 are both upregulated in hypoxia/ischaemia; CXCR4 acts as a mast cell chemotaxin); C5a receptor (C5aR; in microglia C5aR is upregulated upon activation, C5a peptide is released in neuroinflammtion, and there is crosstalk between C5a and TLR4; for mast cells C5aR is upregulated upon activation, and C5aR is a strong mast cell chemoattractant signal towards C5a peptide; there is also crosstalk between C5a and TLR4; table 1). The above points are discussed in greater detail elsewhere [108].
http://rstb.royalsocietypublishing.org/content/367/1607/3312
Regarding Mast Cell Activation and Microglial Activation: Dr Theo and Dr Martha Hebert of Harvard Medical school have been looking at this as a central part of autism. Completes the picture of how autism starts and develops
https://www.facebook.com/groups/350125058387434/permalink/819772798089322/
Mast cells, microglia and brain inflammation, By Theoharis C. Theoharides, MS, PhD, MD
http://www.autismfile.com/science-research/mast-cells-microglia-and-brain-inflammation
Lastly full circle back to Younger and from the Mast Cell Activation world (and Lisa Klimas from Mast Attack, excellent resource):
Leptin: the obesity hormone released by mast cells
http://www.mastattack.org/2015/03/leptin-the-obesity-hormone-released-by-mast-cells/
Thanks so much for the links and research.
I have found a supplement that helps with leptin resistance. Irvingia from Life Extension, is the brand I use.
I had read that lutolin and quercetin are supposed to be as effective as GastroCrom. I’ve used quercetin for awhile but not the lutolin. I tried going off my GastroCrom and had to go back on it. Have you found this to be true for you too?
Isie
Treating SIBO normally is kind of really easy and could make a huge difference for you.
I had a SIBO test done and it came out negative, however I experienced the worst pain of my life after the test for something like 4-5 hours (even threw up on the plain back home :S ). I felt like I was on labour (and I’m a man). It was some kind of contractions that came and went in seconds.
I wonder if that means something…
I hope so, Folk. I hear mixed stories. Some with fast and lasting results with abx, others needing herbs, others long term treatment with either, others having to change diet forever… I would think that any positive shift should impact mast cell activation.. hope so anyway.
I would think that reaction might mean something. Did they test for methane producing bacteria?
This all sounds very familiar. I’m remembering when I got allergy testing done last year and the skin test I had the largest reaction to was the histamine control. Could this indicate a histamine intolerance or is it not related?
Rachel, you might well be experiencing some kind of histamine reaction/allergy. Even though the skin tests didn’t reveal particular sensitivities or reactions, be cautious and note if there are triggers: foods, smells, and thing you react to only when you are more depleted from other health issues. My throat swells and I get hives from eating basil or any kind of peppers (and the response is not related to their level of heat; good old bell peppers are as bad as sriracha sauce), yet the scratch and blood tests come back as if I have now allergy to them. The allergist said: “Then you are allergic. What happens to you is a better test.” And he made sure I have an Epipen.
very interesting article that would certainly explain why so many people with ME voluntarily give up alcohol.
Fr those interested in virus reservoirs this article about one vspecific virus may be of interest http://www.newscientist.com/article/mg22530125.600#.VQleBY6sU9Y
I wonder if it could be adapted for other viruses?
There are so many reasons to think about the cause of FM / ME / CFS / SEID. There is so much speculation. My head gets dizzy 🙂
Indeed! I was just thinking the same thing. My brain is full! It seems there are many pathways to the same endpoint.
A genetic mutation can result in an excessive number of mast cells in your body. It is not only FM and CFS, that overactive mast cells are pumping out high levels of histamine, but other chronic illnesses such as Lupus, Chronic Lyme Disease, Interstitial Cystitis and Multiple Sclerosis are doing the same. Many chronic illnesses that have overlapping symptoms seem to be compatibled with Systemic Mast Cell Activation Disorder (MCAD).
Mast cells normally help protect you from disease and aid in wound healing by releasing substances such as histamine and leukotrienes. But if you have Systemic Mast Cell Activation, excess mast cells can build up in your skin, around blood vessels, in your respiratory, gastrointestinal and urinary tracts, or in reproductive organs. When triggered, these mast cells release substances that can overwhelm your body and result in symptoms such as, a rapid heartbeat, abdominal cramps, nausea, low blood pressure, diarrhea, fatigue, confusion, general weakness etc.
The following triggers may influence a mast cell response: drugs, alcohol, preservatives, stress, sunlight, environmental toxins, bacteria/fungi/mold, artificial colors or flavorings, heat/cold, etc.
Interesting read: Mast Cell Activation Disorder (MCAD), Chronic Illness, and its Role in Methylation
http://geneticgenie.org/blog/2013/01/31/mast-cell-activation-disorder-mcad-chronic-illness-and-its-role-in-methylation/
I think methylation does have an effect. I have mutations in BH4 as well. Addressing this has been of benefit too. It’s been awhile since I read that thread. Thanks for posting it. Many of the people who are researchers of years ago are contributing there. It’s nice to see they are still doing research and finding answers.
As for FMS and EDS III I question that they may very well be a very close connection. They may be MCAS related too. My FMS DX came before my EDS DX. It’s hard to tell where the pain from one leaves off and the pain from the other starts.
Issie
My histamine tale: I have (officially ‘diagnosed’) ME/CFS, POTS and Reactive Hypoglycemia. I’m in the UK. My sister in Canada has been diagnosed with Histamine Intolerance and closely watches her diet for accumulated histamine (I only learned of this very recently). I knew I had some intolerances but wasn’t able to pin them down until I started reading about histamine – not surprising, it seems. Slippery stuff. I recently read about ‘Adrenaline Dominance’, which may or may not be a ‘thing’, but describes me perfectly, as I’m often permanently in fight mode, even amongst bluebells and kittens.
I got ill in my early 40s (peri-menopause? I menopaused in my late 40s). At that time I was exercising vigorously (hiking, dancing, weight-training) and had previously felt strong and healthy. I was also under significant amounts of emotional stress (desperate boredom at work, unable to find a new job, lots of anger-inducing relationships). I developed terrible back stiffness and also could get very little sleep, ‘wired and tired’. Too sleep-deprived to think, I left work and drifted downwards into bed-bound fatigue, night sweats, nightmares etc.
Over the years these are the things I’ve done to treat myself, with some – but not total – success:
1. Emotional clear-out: stress makes any illness worse, and I have to be able to keep myself calm in low-blood sugar/high adrenaline periods.
2. 3+ litres of good water daily. It raises my low blood pressure so is good for the POTS, but also perhaps helps flush out histamines? I know that if I lower the amount, my brain quickly clogs up again.
3. Six grams of soluble vitamin C a day. It makes the high water-intake possible, and I now gather it’s an anti-histamine. It also makes me quite limber: if I stop taking it I start to get very stiff again indeed.
4. Low carb diet: my insulin-production is too high, leaving me with low-blood sugar, leading to adrenaline-production, leading to feeling dreadful, angry and utterly exhausted. Low carbs keep me more stable, if permanently hungry/bit tired. Insulin is also a big problem for fat-burning.
5. Pacing: keeping it all quiet. I’m paying today for a bit of community work I did over the weekend. Not especially strenuous but I feel like I’ve been in a train wreck.
6. Gut repair: I gave up the wheat, nuts, legumes etc and supplemented like crazy. I’m not aware of any particular change from that, yet my body definitely objects when I re-introduce those foods.
7. Bio-identical progesterone, to calm the insulin/adrenaline cycle, applied just before meals. Seems to help but I couldn’t swear to it.
8. Low-histamine diet and histamine-blockers (DAOsin): my latest venture. Seems to be having an effect inasmuch as my eyes aren’t as swollen as they’ve seemed to be for a decade, but perhaps too early to tell.
So: histamine. I’m thinking maybe I was particularly at risk: food = histamine, heavy exercise = histamine, emotional stress = histamine, hypoglycemia = histamine, gut problems/inflammation = histamine, genetics (perhaps) = histamine (low DAO), menopause = histamine (end of estrogen protection).
If this is the case, I’m hoping that attending to all of these and finding foods/supplements that help (pea sprouts, olive oil and Vit C, anyone?) will help hugely. I’ve also listened re the building up exercise tolerance, stretching etc, so will add that in.
I want to respond carefully to Phil and his question about ‘peace of mind’. I think Carollyn is on the right lines in her response where she notes a connection to stress but asks us to go easy on ourselves about this as everything else. The last thing I want to do is ramp up expectations, but I want to endorse hope too, because I had what felt like intolerance to everything, I was so so reactive, call it chemical sensitivity or whatever, it was a nightmare and yet I am writing this today in a comfortable pain-free body.
Phil I think most people with the ghastly illness have a degree of Post-Traumatic Stress Disorder because it IS distressing and there is of course a back and forth, or should I say round and round relationship between the pain and debility and the stress. But I also note that the model of ‘fighting’ illness is unhelpful too; we so often talk of illness in terms of ‘overcoming’ and ‘struggle’. This language is all around us and underlies and reinforces our competitive unstable anxiety provoking economic system. We use a model of ‘battling’ disease and winning and losing the fight, but what we are talking about is fighting ourselves, of using energy in one part of ourselves struggling with another.
Our bodies are trying to help us through their exquisite sensitive feedback loops. I do notice that people often feel better when they see themselves as on the same side as their bodies or to use Cort’s militaristic metaphor they ‘surrender’ i.e. don’t use too much energy fighting themselves. There is so much judgment and blame around and our social ideology gives so much weight to success and failure and achievement and the idea of constantly overcoming our limitations etc. The ideas are everywhere and we almost don’t notice them. Stress is inherent in a winners and losers ideology. And I think the sports medicine model of training and over-exertion and battling through pain is incredibly unhelpful to us. So I am indulgent of myself ……
One thing that really helped me was friends. So often the stress of this illness is made worse by the social isolation. Relentless illness is isolating. I didn’t appreciate the contribution of some accepting friends at the time, I was too caught up in the misery, and when I recovered I regret I didn’t keep up with them. I just allowed the relationship to dwindle as I got on with being busy. I am now much more careful about valuing my friends and I try to offer as much as I can to those who continue to suffer. AND I THANK CORT FOR OFFERING ONLINE FREINDSHIP TO ALL OF US.
So I haven’t found that elusive ‘peace of mind’ but 1. I recognise that my illness was associated with a very long period of unremitting stress and that I put extreme expectations on myself for dealing with what were actually intolerable demands. Looking back I really wonder why on earth I thought I should be able to cope with intolerable expectations. And 2. I now recognise and acknowledge the reality of my internal and external stressors and accept my limitations in dealing with them and 3. I manage my stress states more realistically and don’t put the same ridiculous burden on expectation on myself.
I have done heaps of psychotherapy over the years and some I found very unhelpful even destructive and others really helpful. I do think that self-insight helps me manage myself more constructively but I am very choosy about who I work with. If it doesn’t feel safe – it isn’t and if they want to tell you about your illness and its causes leave –quickly. I had a wonderful and surprising encounter with an indigenous healer but that doesn’t mean that everyone should rush off and try and find a spiritual mentor, but simply that remaining open to what might help you – well it might help you.
Anything you can do to promote deep relaxation is helpful but my memory of that horrible pain is that it made relaxation impossible. The more I actively tried to relax the more the pain intruded. So what did I do?
Once I realized that this was a multisystem illness and there was no single answer I did everything I could think of, all at once, and with as open a mind as possible. So long as it didn’t harm me I did it. (I am very suspicious of the idea of a healing crisis and don’t do anything that makes me feel worse). I know that many people try one thing at a time to try and find what ‘works’ but I don’t think any one thing ‘works’ so I accepted both conventional and alternative therapies. For example these including medication and magnesium etc. for sleep. When the pain was bad I took really large doses of valerian at the same time as meds. They work in different ways and both helped. But I had to be very careful of meds because of the severe reactions. I had horrible reactions to things like dental anaesthetics i.e. racing heart, etc etc.
I took and still take any amount of supplements but carefully and always starting in low doses. I have had heaps of Vit C including Intravenous. I am glad to see liposomal Vit C on the market and I use liposomal glutathione still. One supplement I still can’t tolerate is 5HTP as it upset my gut and causes muscle pain and weakness.
I really identify with the sweating by the way, I would drench in cold sweats and carried dry underwear with me. If you describe sweating, heart pounding, wobbly walks, feeling like you can’t get up a step etc. to most doctors they think you are deranged, so I became very careful about doctors too.
But what I most did was get rid of everything I might be reacting too. At the time I thought I had become allergic to everything so I had a massive clean out. I got rid of everything that I might be reacting to (Including an unsympathetic husband).
I reacted to stainless steel or rather the nickel in it so most jewellery went out. I did a ‘healthy house’ dousing and installed things to reduce the electromagnetic fields. I switched off all appliances at the wall at night. I changed personal and household cleaning chemicals which were totally replaced by organic safe substances. I went totally organic and still never eat anything GM. Organics included my clothing and anything touching my skin like sheets. I used scentless simple soap for me and my washing. The smell in the super market made me feel horrible so I avoided it. I made a huge fuss about avoiding smells including new plastics and new carpet or glue, New buildings were a bit of a nightmare. I became a bit of a pain quizzing friends about perfumes and so forth – you name it I avoided it……..This sounds bonkers to anyone who hasn’t experienced these debilitating symptoms. (Including my rapidly becoming ex) I remember insisting on getting out of a taxi with a horrible air freshener because I was swelling up with hives and I hated smoke too. A lot of therapists would say anyone describing this behaviour had social phobia, a lot of people would say you were just being difficult. So I avoided anyone like that and ignored those I couldn’t avoid. Like colleagues…..
I do believe diet was important. I have done any number of elimination diets and yes they helped but I never developed a list of allergenic foods which I now find explicable in light of the histamine hypothesis. I have followed an excellent omnivorous diet since and this includes a high protein breakfast which does help I find with avoiding palpitations, blood pressure wobbles, the ‘afternoon lows’ as I call light-headedness and so forth.
I really wish I could be more specific BUT it isn’t specific IT’]IS systemic.
I really benefit from all your posts and this line on histamines especially. I do hope this helps somebody –all I can say is I am grateful for whatever did work for me and that these possible symptoms are just a memory….
Phillida
Thank you for your thoughtful reply, Phillida, and Phil, too. I have wished the word “stress” to have fewer uses/meanings so that we could pars out when scientists are using “stress” to engage subjects in an activity or response that pushes the system to reveal its dysfunction or when we as individuals are reacting to complexities and inanities of life. Using the same word can add a burden to the chronically ill, an implication that we are creating the situations that evoke the illness. Indeed, learning to be more skillful at recognizing reactions, emotions, and how to articulate them adds peacefulness that is helpful for some healing, but that may still not cure us. I don’t mean to be hard on you, Phil, for looking into that. It’s essential to our humanness as much as for living with what we have and improving our health. But I do still fear that whole bodies of “science” what to simplify what we have into the notion that a couple of mental habits cause a giant systemic effect.
Phillida also wrote about shifting thinking away from war talk, that when we think of it as fighting our body rather than listening to it we may not further healing. An interesting–and perhaps polar opposite notion–is something I read once (sorry I didn’t note it for a proper reference point) is that humans may have learned war from our immune systems. Battle may truly be innate. It may not be the most helpful response, but it may be literally part of us.
This idea helps me bring equanimity to the times when I want to fight my situation, of being disabled by chronic illness but end up over-doing activity then and hurting myself in pay-back PEM, even though I’m aware of the repercussions as I chose to act out in frustration. It also underscores how nothing is just black and white, this or that, good or evil; surfing the complexity is more the point of this human experience, illness or not.
Thank you very much, Phillida. There is an incredible amount of similarities between how you coped and improved, and how I am also doing so now.
The imagined invulnerability to stress and pushing oneself too hard for too long. The switch to a lower pace of life with more enjoyment. The letting go of “friends” and family who think toughlove is all I need, and the finding of new ones. The “trying everything” until you were improving, and working out what worked.
I agree too about the unhelpfulness of thinking in terms of of “fighting”, which is taking me a long time to change. I was absolutely constitutionally an over-exerter without understanding it at all, I just thought that is what you did when you “exercised”, no pain no gain, all that kind of thing. Even at my lowest state of fitness, walking too briskly on too steep slopes, that kind of thing. The whole massively important discovery of pacing absolutely fits with an attitude change to “don’t fight, go with your body’s flow”.
Looking back at the worst times, prior to the fibro diagnosis and for the first few years after it, as the mainstream medicine protocols were only messing me up worse, I can see so much harm I was copping from the work environment especially. Changing to piano tuning as a career (with a long semi-holiday as I got tuition in it) meant I got out and about a lot, and generally don’t get affected by any one particular problem smell or what have you. Being stuck in the same place every day with something would be a major problem. The stress and the lack of sympathy and understanding of it was the major problem, I was a fool to tolerate it and tough it out for so long.
I won’t prolong my comment, but there was still more in what you say that gels with me.
Hi, I just wanted to add in one thing: Raised Histamine in blood causes blood pressure drop, this can make you feel tired. If blood pressure drops too low our body will release Adrenaline to get the blood pressure back up and to degrade the histamine in the blood. This may be why the histamine blood levels vary so much and why our muscles tense up (headaches) and we wake up hot in the night from the adrenaline released. Hope that helps. The effects of rising blood histamine should be noted in a sequence of events as it rises it has different effects on the body.