Late last year (2012) I celebrated my 50th birthday. The first symptoms of ME/CFS began in 1985 which means, like many of you, I’ve been coping with ME/CFS for the majority of my life and for the vast majority of my adult years. I’ve also been fortunate enough that for 20 of those 27 years with ME/CFS I have been able to attend university (gaining a first degree in Psychology and master’s degree in Computing) and work full time. The onset of illness for me was sudden and gradual. By that I mean there was a clear demarcation between being fully physically well and then unwell.

I currently live in rural France with my wife of the last 21 years and three cats.
None of this confers on me any biomedical expertise at all and certainly nothing that would merit suggesting any course of treatment. All I can offer is my own insights into my illness and a certain skewed way of looking at the world.
I should add that, since the onset of ME/CFS, I have been variously diagnosed with depression, obsessive compulsive disorder (OCD), IBS, fibromyalgia, ME and then CFS. None of these ‘labels’ I believe carries any more significance than being merely facets of the same underlying pathology.
General ‘fatigue’ has never been a major problem for me. Rather I tend to view my various symptoms as falling under the ‘wired and tired’ type.
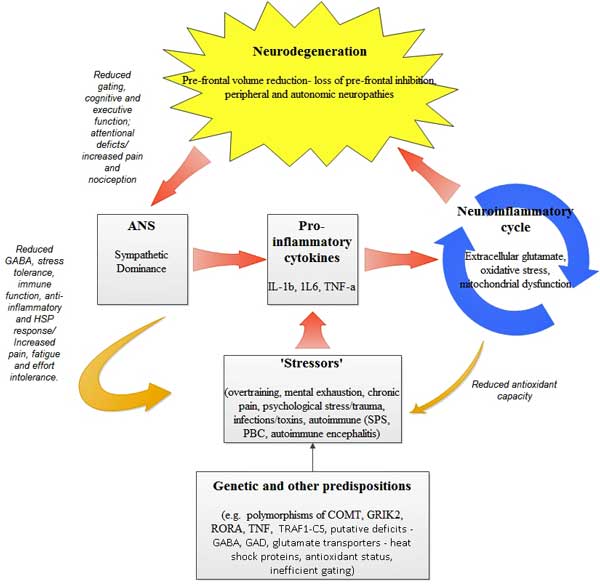
Marco’s Neuroinflammatory Model of ME/CFS
I have written this in ‘blog’ format rather than in the more traditional format of a scientific paper for two reasons. Firstly, it was always my intention to put together a ‘short’ paper that I could open up for discussion amongst ourselves. Every hypothesis must be critically tested and who better to do this than those who live with ME/CFS on a daily basis.
Secondly, this material has evolved over the course of just over a year. The initial impetus came from several threads on Phoenix Rising where I and others were discussing several ‘atypical’ symptoms we experienced including various types of ‘sensory defensiveness’ or ADHD or ASD like behaviours or symptoms that are rarely if ever mentioned in the ME/CFS literature and which seemed more appropriate to an alternative ‘diagnosis’.
Comparing conditions in which various forms of ‘sensory overload’ featured brought up some startling commonalities and led to neuroinflammation as a potential common pathophysiology.
The Chronic Fatigue Syndrome (ME/CFS) Neuroinflammatory Series
- Not Fatigue After All? New Model Suggests Other Symptoms Better Explain Chronic Fatigue Syndrome (ME/CFS)
- Glutamate – One More Piece in the Chronic Fatigue Syndrome (ME/CFS) Puzzle? The Neuroinflammatory Series Pt. II
- Does A Rare Neurological Disorder Provide Clues to ME/CFS and FM? The Neuroinflammation Series Pt 3a
- Scared Stiff? Exploring Anxiety, Autoimmunity and Infection in Stiff Person Syndrome – A Possible Model For Chronic Fatigue Syndrome
- When Definitions Obscure: A Neuroinflammatory View of Chronic Fatigue Syndrome Pt. IV
- From Mood Disorders to MCS: A Neuroinflammatory Model Takes on the Symptoms in Chronic Fatigue Syndrome (ME/CFS)
- The Immune System and Neuroinflammation: Part IV of the Neuroinflammatory Series in ME/CFS Continues
- Cooling the Flames: Possible Approaches to Reducing Neuroinflammation in Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia
- From Chronic Regional Pain Syndrome to Fibromyalgia to ME/CFS? The ‘Spreading Neuroinflammation’ Model
- Neuroinflammation: Putting the ‘itis’ back into Myalgic Encephalomyelitis – Back to the Future For Chronic Fatigue Syndrome?
- Japanese Sensory Gating Study Reveals Profound Cognitive Deficits Present in Chronic Fatigue Syndrome
- Sensory Overload: Study Suggests Brains in Fibromyalgia Are Being Pummeled With Too Much Information
- The Energy Disorders: Diabetes, ME/CFS and FM – Can Diabetes Tell Us Anything About Chronic Fatigue Syndrome and Fibromyalgia?
- Could Cancer Research Improve the Treatment of Widespread pain in Fibromyalgia and ME/CFS?
My many thanks to Cort Johnson who has worked with me on this over a period of many months in the capacity of ‘contributing editor’ and who has now kindly agreed to host this material here as one of what will hopefully become a growing list of ‘guest bloggers’.
I hope this ‘hypothesis’ resonates with at least some of you.