



Vitamin D3 has become a big deal in the past couple of years, but the findings in fibromyalgia have not been particularly promising. Several fibromyalgia studies have not found evidence of low Vitamin D3 (calcifediol) levels in fibromyalgia. Noting,though, that other studies suggest low Vit D3 levels are associated with increased pain, and that some studies suggest that increasing D3 may help with pain and other symptoms found in FM, these researchers took another look.
If they were successful they would begin to document a relatively cheap and easy way to help with pain for people with fibromyalgia.
A Look at Vitamin D3
Because humans can synthesize D3 from sunlight, it’s not regarded as an ‘essential nutrient’; i.e. one that needs to be ingested. (Sunblock, by the way, dramatically reduces vitamin D uptake through the skin.) Many claims have been made for D3’s affects on cancer and other disorders, the vast majority of which have not been proven. An IOM overview of D3’s effects stated
“Outcomes related to cancer, cardiovascular disease and hypertension,diabetes and metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsia could not be linked reliably with calcium or vitamin D intake and were often conflicting.” (from Wikipedia).
A recent review article, however, proposed that stress- associated reductions of D3 in chronic fatigue syndrome and autoimmune disorders could result in persistent infections, chronic inflammation and fatigue. Earlier the author (Hoak) proposed that a number of immune and oxidative stress issues in ME/CFS (persistent NF-κB activation, augmented nitrosative-oxidative stress, redox imbalance, chronic inflammation, and concomitant fatigue) could be associated with reduced vitamin D levels. A large 2010 study finding low D3 levels were associated with muscoskeletal pain in men implicated pain.
While no one appears to think Vit D is a cure for fibromyalgia or chronic fatigue syndrome many practitioners appear to recommend trying it. Dr. Lapp finds that almost all his ME/CFS and FM patients are low in vitamin D and puts in his five recommended supplements. He recommends 2,000 IU a day.
Study
In the most rigorous D3 fibromyalgia yet done, these Austrian researchers took FM patients with low blood calcifedol (D3) levels (<32 ng/ml), raised their blood D3 levels to the normal range (between 32 and 48 ng/ml) for a certain amount of time (20 weeks), and then determined if their pain (visual analog scale) or anxiety or other symptoms improved.
Results
“In addition to known therapies, oral substitution of vitamin D may be regarded as a relatively safe and economical treatment for patients with FMS. Vitamin D levels should be monitored regularly in these patients, especially in the winter season, and increased appropriately.” Authors
The study was quite small, but the fact that seventy percent of the fibromyalgia patients had below normal levels of plasma D3 suggested low D3 levels may be common. D3 levels may be low in most people, healthy or unhealthy, but a large 2009 survey found “moderately to severely suboptimal” vitamin D levels in people with chronic fatigue syndrome in the UK. Their D3 levels were much lower than found in the general population.
No improvements were seen in fatigue, fibromyalgia impact score, anxiety, somatization or mental health (SF-36), but significant improvements were seen in the main outcome of the study, pain (visual analog scale), and in ‘physical role functioning’ (SF-36). (I believe physical role refers to the degree to which a person believes physical problems prevent them from functioning normally. ). The fact that the highest reductions in pain were associated with the highest blood D3 levels suggested that the D3 was indeed reducing pain.
The fibro patients were not pain-free by any means; the authors characterized the reduction in pain on the Visual Analog Scale (pain) (20 points on a 0-100) as being ‘relatively low. (A 20 point reduction could easily, however, mean a 25% or more reduction in pain?)
They believe that larger D3 dosing could further reduce pain and pointed out that they’d intentionally chosen a max out blood D3 levels at a lower level.
Reduced D3 levels in the winter when the participants were presumably spending less time outdoors suggested that was a particularly good time to take (and perhaps increase) D3. The fact that after discontinuing D3 the patients blood D3 levels dropped to baseline indicated the drug needs to be taken continuously.
Dosing
Noting that the current ‘optimal’ D3 blood levels are set to prevent rickets, the authors suggested it may be set too low …something Adrienne Delwho of About.com’s Chronic
The questions regarding optimal blood D3 levels suggest hard recommendations on dosing await further study in FM and ME/CFS
Fatigue Syndrome and Fibromyalgia site definitely has something to say about. Her low blood D3 levels after supplementation suggested to her rheumatologist that she needed much more D3 than ‘normal’. A temporary D3 megadose that brought her blood levels up to 60 ng/ml resulted, for the first time, in significant reductions in pain. Her rheumatologist noted that most of her pain patients don’t see significant relief until their blood D3 levels get to over 60 ng/ml.
Adrienne now takes 5,000 IU D3 a day to reduce her pain, a bit higher level than the maximum tolerable amount recommended by the United States Institute of Medicine. (Note that recommendation reflects the lack of information available on the effects of those doses and applies to ‘nearly all persons in the general population”; i.e. it reflects tolerability across a large population and may not apply to people with chronic illnesses. (Adrienne believes the stresses imposed by her chronic illness increase her need for Vitamin D.)
- 0–6 months of age: 1,000 IU (25 µg/day)
- 6–12 months of age: 1,500 IU (37.5 µg/day)
- 1–3 years of age: 2,500 IU (62.5 µg/day)
- 4–8 years of age: 3,000 IU (75 µg/day)
- 9–71+ years of age: 4,000 IU (100 µg/day)
- Pregnant/lactating: 4,000 IU[7]:5(100 µg/day)
Conclusion
Vitamin D appears to present a mostly safe and cheap way to reduce pain (and possibly other symptoms) for some people with fibromyalgia and chronic fatigue syndrome. Larger studies are needed to identify optimal doses and to validate and enlarge on this studies findings.
We should know more about the effects of Vit D on ME/CFS soon. ME Research UK funded a study, “The effects of oral vitamin D supplementation on cardiovascular disease risk in patients with ME/CFS” that should wrap up this year. (Thanks to Tom Kindlon for the info.)
If you’ve tried Vitamin D what are your experiences?
Please consider supporting our sponsor, Prohealth, when you buy your supplements







initially my D3 was extremely low, I started out with 70,000 weekly, then reduced after 9 months to 40,000. I had a reading of 90 in Dec about 16 months to get to this. In Dec my Vit d was doubled from 40,000 to 80,000 weekly. On reading this I just realised that yes my intermittent randomised pain has reduced in both severity and reguarity, and perhaps this is why.
Smiling
Indeed, D3. I have significant reduction in pain after quitting all pain Rx and staying on D3 4000IU/day and a couple of natural supplements for inflammation. Power to the People.
Power to the people indeed :). Glad it works for you…
My last blood-work showed low vitamin D levels, so at my doctor’s suggestion I started taking vitamin D3. I’ve been taking it for about 5 weeks now. So far I haven’t noticed a difference, one way or the other. Of course, it’s impossible to know what my pain levels would have been had I not been taking it.
Vitamin D3 makes me feel much much worse although it helps with infections. Anything that has helped with infections has made me more ill and anything that has made me feel a little better has made infections worse. Now that I am severe I can pick up on these things very quickly. I took D3 before I was severe and didn’t notice any effect.
When the question of vitamin D and fibro first came up about 6 years ago I was found to be low in vitamin D and was put on a dose of 5000 IU a day that was later decreased to 2000 a day as my levels rose and then I was told that the amount in a multivitamin should suffice. There were two doctor changes between then and now and at one point I dropped the multivitamin because I was trying different supplements and did not want to accidentally overdose on anything. In the meantime other illnesses and injuries have caused other health problems but in general my pain levels are high again. Several months back I re-instituted the multivitamin and have been feeling somewhat better. When new information about a vitamin D and fibro connection came out again I started considering increasing my dosage starting the first of this month. After researching to make sure I would not be endangering myself I decided to just leave the multivitamin in place and added 2000 IU of D3 which brings me up to 3000 IU a day. I haven’t seen a lot of change but it is only a week and on top of that it has truly been the winter from h*ll for me. I set up all my pills on Sunday for the coming week and will probably add an extra 2000 a day and see how that goes.
Researchers talk about “necessary and sufficient.”
What they mean is that sometimes just one thing is needed (for instance, to cause the enzymatic reaction they are looking for) or sometimes it’s two, three or more.
When just one single thing will work, they say it is necessary — necessary for function. And sufficient, meaning that no additional protein, co-enzyme, co-factor, linker, etc. etc. is needed.
It seems obvious that in the case of Vitamin D, it is necessary. That is, people with inadequate levels of Vitamin D improve — SOME of them improve — when those levels are increased.
However, even though it is necessary, it is not sufficient. That is, low Vitamin D is obviously not the one and only problem here.
But when I read stories about people who are “bedbound” (and I assume staying indoors for weeks or months at a time) it seems obviously they are not getting any Vitamin D from sun exposure. Therefore it seems logical to assume that anyone — with CFS or with Alzheimer’s or any other limiting illness — might want to consider how much sun exposure they are not getting.
If the answer is “basically none” then the first step should be obvious.
– – – – –
“Anon, good nurse, anon! Sweet Montague, be true. Stay but a little, I will come again
I don’t have fibromyalgia, but I do have ME/CFS. I feel lucky not to have a lot of pain. But I do find that vitamin D helps. I get this really strange feeling in my arms when I get a crash and when my vitamin D is higher I don’t get that sensation – it’s quite uncomfortable. Like Adrienne, I feel best when it is around 60. Started at 17! I take 3000mg/day to keep it there. Good stuff.
How do you find out your Vit D levels? What is the name of the test and who can prescribe it? The physicians in the clinic in my area are not familiar with ME/CFS. I am basically on my own with keeping up with the latest information on treating aspects of this disease. The rheumatologist that visits the area once a month is a joke. Said he didn’t know what was causing my symptoms and left it at that. I recently started Vit D3 supplementation on my own but it would be nice to monitor the effects over time.
Well this is well timed.
A week ago I was at my Dr’s for dry and cracking skin (on one hand only strangely) and he prescribed a single megadose (200,000 UI) of D3.
Which of course I had to google and it appears that D3 is involved in regulating hundreds (thousands?) of genes and D3 deficiency is linked to all sorts of non-skeletal conditions from depression to diabetes to autism. Whether deficiency is linked causally or as a consequence of chronic illness is another matter.
One thing to mention is that D3 requires various co-factors (magnesium, zinc and others I can’t recall).
I can’t honestly say I’ve noticed much difference to date (pain isn’t a big problem for me) apart from feeling a little more ‘purposeful’ but its early days and I’m sure maintaining an optimal level of D3 can’t be a bad thing – especially this time of year.
What I have noticed over the years is that any downturns in my health have come just at the end of winter so who knows?
Ha! Good timing indeed. Good luck with it 🙂
my D3 levels (t.i. 25(OH)vit D as in most blood tests) is very low and did not increase even when I took 10.000 UI. daily for months.
Recently I learned from a video seminar (on U tube) from dr K. De Meirleir, a belgian dokter who treated many fibromyalgia and CVS patients (he works in the US also now) that he is not positive for giving vit D3 to fibro patiënts: normally only a small quantity of the 0,25 hydroxyvitD available is transferred in 1,25 (OH)D (the hormone); But infection or damage of the body transfers 0,25D in 1,25D. Low 25D and high 1,25 D seem to result in chronic inflammation;
we don’t need that I suppose.
I recently stopped taking vit D3 and will have the ratio 0,25/1,25 D tested .
ME Research UK funded a study, “The effects of oral vitamin D supplementation on cardiovascular disease risk in patients with ME/CFS”. I think we should expect the results reasonably soon e.g. in 2014.
http://www.meresearch.org.uk/our-research/ongoing-studies/vitd-suppl/
http://www.controlled-trials.com/ISRCTN59927814/59927814
Thanks Tom. Didn’t know that. I’ll put it in the blog 🙂
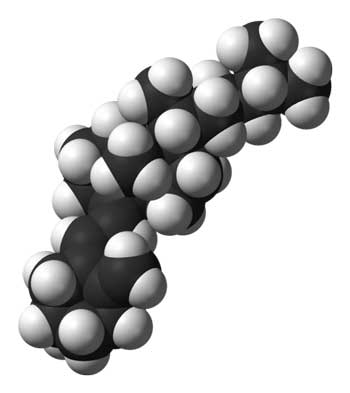
http://en.wikipedia.org/wiki/Vitamin_d
In the liver, cholecalciferol (vitamin D3) is converted to calcidiol, which is also known as calcifediol (INN), 25-hydroxycholecalciferol, or 25-hydroxyvitamin D3 — abbreviated 25(OH)D3. Ergocalciferol (vitamin D2) is converted in the liver to 25-hydroxyergocalciferol, also known as 25-hydroxyvitamin D2 — abbreviated 25(OH)D2. These are the two specific vitamin D metabolites that are measured in serum to determine a person’s vitamin D status.[10][11] Part of the calcidiol is converted by the kidneys to calcitriol, the biologically active form of vitamin D.[12] Calcitriol circulates as a hormone in the blood, regulating the concentration of calcium and phosphate in the bloodstream and promoting the healthy growth and remodeling of bone. *****Calcitriol also affects neuromuscular and immune function.*****[13]
( emphasis as ***** is mine)
http://en.wikipedia.org/wiki/Mitochondria#Storage_of_calcium_ions
( but what do I know? )
Was found to be well below normal in D3. Started taking a supplement, but within a day or two it looked like I had black eyes. I also had bleeding gums and bruising on arms and later, had very tender feet when out walking.
Does it also increase photosensitivity? My husband, late 50s, started D3 and immediately had to wear sunglasses – first time ever.
Found that D3 needs to be balanced with Vitamin K2. Am trying to eat a lot more leafy greens, but have dropped the D3.
I did ask to be tested for D2 because we have sarcoidosis in the family. Offered to pay for the test, but it wasn’t done.
I’ve had bad reactions from Vit D also, as well as cod liver oil and flax seed oil. All the same problem (rectal bleeding). Stopping the capsules stops the bleeding. I can only tolerate one small vit D capsule a week.
Has anyone else had this reaction?
(I have to be very careful of the supplements/foods/pharmaceuticals I take due to over-reacting. I understand that goes with type O blood.)
At one stage I feared being bedbound. I date a very slow recovery from when I persuaded my doctors to do a vit D test, discovered it was suboptimal and took supplements. So yes – necessary but not sufficient. I’ve now added other things and they’ve made more difference.
A couple of things not yet mentioned – Dr Gominak (an American neurologist) has found vitamin D helps her patients sleep better. http://drgominak.com/vitamin-d-3/ With improved sleep the body is better able to heal itself and I suspect that’s what happened to me. In the UK, not famous for its sun, many ME sufferers report improvements on holiday in sunnier places. Could be relaxation but could also be improved vitamin D levels.
A liver specialist told me that vitamin D deficiency can affect liver tests. I’m afraid I didn’t think to follow up on this and ask how. Certainly low liver function is associated with low vitamin D levels but it’s not clear if poor liver function causes low D levels or the other way round. http://www.medscape.com/viewarticle/807726 I’d certainly recommend anyone with low D to try and arrange a fibroscan.
For those unable to tolerate supplements there are UVB narrowband lamps like this for the UK http://www.amazon.co.uk/Dermfix-3000-UV-B-Lamp-Vitamin/dp/B004NOPC9S but in America you may only have these http://www.amazon.com/UV-B-Phototherapy-Psoriasis-Vitiligo-Eczema/dp/B00CJHS572/ref=sr_1_1?ie=UTF8&qid=1392029205&sr=8-1&keywords=uvb+lamp+narrowband
I too wonder about the 25 D/ 1,25D ratio as purported in the Marshall protocol. That is why his protocol reduces sunlight and all D sources and gets the D levels very low. The idea I understand is that because of the mis-conversion of D converting to D 1,25 in these diseases, and in an unhealthy way, inflammation is increased and there is a bad overall outcome until that pathway is fixed through other means. It is true that my ratio of 25 to 1,25D is abnormal. Low D and high 1,25 D. (I hope I have got this right) I think the Marshall site and Dr. DeMeirleire are exploring this. I always wonder if it will be attached to the RNaseL pathways somehow: The good RNaseL being converted to the low molecular weight RNaseL which is causing inflammation and cell death. My rates on this was extremely abnormal as well.One day these may all be tied together.
This is my first reply on this site, so I hope I’m doing this right! Anyway, I can say that Vitamin D3 is definitely something that has helped my fibro pain. I have had fibro/CFS for about the last 20 years, and for the first many years my symptoms were pretty evenly divided between the pain of fibro and the fatigue of CFS (besides all the other symptoms like brain fog, etc). Anyway, about 5 years ago my doc checked my D3 level and it was very low. He started me on 100,000 units – yes you read that correctly – 100,000 units a week of D3. It was split into two doses of 50,000 per week. My pain initially got much worse and I could tell it was from the D3. He thought I was nuts, but switched me to Vitamin D2, and I did not get the intense achiness that I had gotten with the D3.
When I was at Mayo clinic the following year, I asked a rheumatologist if she had ever heard of someone getting achy from D3, and she said with a dose of 50,000IU she wasn’t surprised. I do not have a medical background so cannot remember the specific reason, but it was because it put too much D3 into my system compared to the other things it interacts with, such as calcium, and was causing an imbalance. She suggested I go back to the D3 at a lesser dose each day to add up to 100,000 units a week. That is what I did, and it took me a good year to finally get my D3 levels to midrange.
I presently take 50,000 units a week, taking 5,000 some days and 10,000 on the others. I cannot think of anything else I have tried that has gotten rid of my fibro pain like D3. It has been amazing!
I also want to thank you for this site Cort. I can’t believe all the wonderful information you put out!
That’s great to hear Mary. It’s a reminder to me to be sure to tinker around with the doses and don’t give up right away.
I take 2,000 IU’s per day and have for six years, not the high levels recommended in the study but my blood levels are normal with this. I haven’t noticed a difference in pain one way or the other, but my bone density scores which had been dropping each test turned around and started going back up after adding this supplement. That’s good news.
I have Osteoporosis of the lower spine which was diagnosed around 2 years ago. Almost in the same year I was diagnosed with Fibromyalgia.
I’m also having Zoldronic acid infusions for my Osteoporosis, I have had 2 infusions so far( an infusion once a year for 3 years) and 1 more next year and then another bone density scan.
I was prescribed Adcal D3 by my GP. I used to forget to take them in the evenings, so I was only taking the morning dose of Adcal.
Probably in the last few months I have been regularly taking Adcal at night and wow……my Fibromyalgia is under control.
I used to think the pain I was experiencing was related to my Osteoporosis and that my lower spine was crumbling (every Fibro flair is located in my lower spine then spreads to my entire body)
Since taking the correct dosage of Adcal D3 my flairs are so much better and less frequent.
After reading this article I now understand why my flairs have been better and less frequent.
I’m due to see my Rheumatologist early next year so I will be keen to talk about my experience.