




Infectious mononucleosis is a common trigger for ME/CFS in teens. But why do some teens recover while others do not?
Studies indicate that when you ask an adolescent what triggered their Chronic Fatigue Syndrome, up to three-quarters are going to say mononucleosis (or glandular fever) or some other sudden, often vicious mono-like illness. With fully fifty percent of them testing positive for mono, it’s no wonder that Epstein-Barr virus, the pathogen that almost always causes ‘classic mono’, has received more interest than any other virus in ME/CFS.
Infectious Mononucleosis IM) (aka glandular fever) has always been understood to be a serious illness that often requires lengthy recovery periods. As time has gone on, though, a dark underbelly to IM has been exposed: IM is known to cause lengthy disability in about ten percent of its victim.
This study, which was part of a larger effort (which will be covered below), tried to uncover what factors put an adolescent who came down with infectious mononucleosis at risk for Chronic Fatigue Syndrome. Its primary graces were its size (300 plus adolescents in the original sample), its team of experienced ME/CFS researchers and physicians, and its use of a Lenny Jason revised edition of the Fukuda definition to diagnose ME/CFS.
Predictors of post-infectious chronic fatigue syndrome in adolescents. Leonard A. Jasona*, Ben Z. Katzb, Yukiko Shiraishic,Cynthia J. Mearsd, Young Ima & Renee R. Taylore. Health Psychology and Behavioral Medicine: An Open Access Journal. Volume 2, Issue 1, 2014
Given past associations in some studies but not others, it made sense to determine if a very stressful event during the course of IM set patients up for an ME/CFS-like illness. The Dubbo study finding that illness severity was a key factor in progression to ME/CFS prompted the use of an autonomic nervous system symptom questionnaire to determine illness severity. A perceived stress questionnaire focused more on perceived stress, a psychiatric interview determined rates of mood disorders, and a family questionnaire uncovered possible family issues.
Did family issues, stressful events during the illness, mood disorders, perceived stress, or illness severity increase the risk of coming down with ME/CFS? Let’s find out.
Results
That 24% of the adolescents had still not fully recovered six months later confirmed how severe an impact EBV infection can have on adolescents. The fact that almost 80% of the unrecovered adolescents met the criteria for ME/CFS confirmed the major contribution Epstein-Barr virus must be making to the pool of Chronic Fatigue Syndrome patients every year.
Stress of any kind, whether ‘perceived’, in the family or from a major event, did not increase the risk of coming down with ME/CFS
The almost 90% female dominance in the patients that met the CFS criteria was remarkable. The study did not show the gender makeup of the original 300 person cohort, but it was surely more evenly split between females and males given that IM overviews do not mention gender dominance. By 12 and 24 months into the study all the ME/CFS cases were women.
A stepwise-regression analysis indicated that behaviorists will be unable to argue that socio-economic status, family stress, the presence of mood disorders, stressful life events, or even the current presence of stress tip IM patients into Chronic Fatigue Syndrome.
Instead the adolescent’s entry into ME/CFS was advanced, as predicted by the Dubbo study, simply by how severe the initial illness was as measured by the autonomic nervous symptom index and days spent in bed. Essentially, the harder someone got whacked by Epstein-Barr virus in the first place, the less likely they were to recover, and the more likely they were to come down with Chronic Fatigue Syndrome.
That, of course, suggests that the ME/CFS patients-to-be had more difficulty fighting off the virus, a finding that serendipitously a recently published study suggested is true. (A blog on that will be out shortly.)
Other studies have found different results. A Dutch study finding that family stress increased the risk of ME/CFS, however, was confounded both by an inadequate definition and by study referrals to a psychologist which predicted a higher than normal rate of behavioral issues.
This study’s sampling approach ensured that no such biases were present.
Causes
The paper did not suggest why IM illness severity was such a powerful predictor of Chronic Fatigue Syndrome, but we can speculate.
Hormones

Equal numbers of males and females probably come down with infectious mononucleosis, but far more women do not recover from it
This study suggests that females have much more trouble recovering from IM than males. The very high rate of IM diagnoses during a time of major hormonal changes ( 15-17 year old age group) appears to lend credence to Broderick’s hormonal-HPA axis model. This model predicts that hormonal changes, perhaps triggered by an infectious event, are much more likely to push women, and not men, into a low cortisol and immune deficient ME/CFS-like state.
Other studies by this group of the same cohort, however, did not find low cortisol level in the ME/CFS adolescents, nor did they find low natural killer cell functioning or increased rates of orthostatic intolerance. This suggests that, to the extent that they’re present in adolescents with ME/CFS, they may come along later in the disorder.
Immune System
There remains therefore an overwhelming body of evidence reinforcing the link to an infectious etiology in at least a subset of CFS patients, despite the fact that specific viral serology is not required for diagnosing CFS. Broderick et. al.
The Dubbo study’s finding that high cytokine levels and increased symptoms very strongly predicted the appearance of Chronic Fatigue Syndrome suggested that high cytokine levels could alter brain functioning or that EBV infections could have penetrated more deeply into the body, and this group did find cytokine changes.
“Illness-specific differences in the regulation of Th17 response may be a shared component in a significant subset of CFS cases.” Broderick et. al.
An earlier study of this group did find altered levels of cytokines that are associated with a Th17 response. The Th17 response is important in reducing extracellular pathogens (primarily bacteria and fungi) and appears to figure in autoimmune and inflammatory disorders. Because EBV may be able to alter the TH17 response, it’s possible that a more extensive EBV infection altered immune functioning in the unrecovered patients.
Autonomic Nervous System
Another earlier study finding from this group suggested a predisposition to autonomic nervous system dysfunction could explain why some people did not recover. It turned out that the IM patients destined to come down with ME/CFS had higher autonomic nervous system symptoms early in the infection than those who recovered.
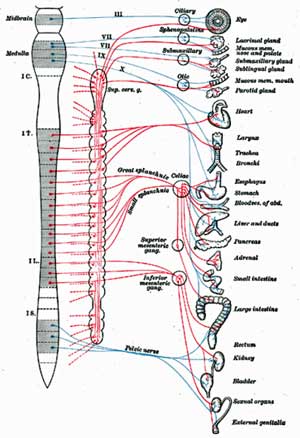
High rates of autonomic nervous system symptoms found early in those who progressed to ME/CFS, suggested the ANS plays a role in who recovers from IM and who does not.
This suggested the infection either affected their ANS more or that a less stable ANS system prevented them from recovering from IM. The ANS is a major immune system regulator, and this finding brings to mind Dr. Klimas’s finding (unpublished) that the ANS dysfunction during exercise appears to trigger immune activation.
Whatever the explanation, this study suggests it’s possible that simply measuring autonomic nervous symptoms early in infectious mononucleosis could pick out adolescents that are likely to come down with ME/CFS.
It also suggests autonomic nervous system dysfunction could be the gateway to ME/CFS. It’s a pity heart rate variability (HRV) measures weren’t done. Would low heart rate variability (sympathetic nervous system dominance) early in the disease have been associated with entry into ME/CFS? Hopefully future studies will answer that question.
Stopping ME/CFS at the Source – Urgent Need For More Studies
None of the psychological or stress factors predisposed adolescents with infectious mononucleosis to come down with ME/CFS. Instead, Illness severity as well as high rates of autonomic nervous symptoms and unusual cytokine patterns possibly associated with a dysfunctional TH17 immune response appeared to be precipitating factors. The fact that two mainstays of adult ME/CFS, low cortisol and reduced natural killer cell functioning, were not found suggested adolescent ME/CFS, at least in the earlier stages, may be fundamentally different from adult ME/CFS.
This was a big, expensive study, the likes of which don’t come around all that often in ME/CFS. The results, however, illuminated more about what we don’t know about pediatric ME/CFS than what we do. With brain imaging findings showing early changes in brain structure and connections in people progressing from acute to chronic pain, perhaps brain imaging would be more enlightening. The autonomic nervous system symptoms suggest that system should be more carefully analyzed.
As time goes on recovery rates continue to improve. By 24 months 4% of the original cohort still met the criteria for ME/CFS. The authors pointed out that that percentage, which doesn’t reflect ill adolescents who do not met the CDC criteria for CFS, is still far too high.
The authors noted the sometimes dire consequences a chronically ill adolescent can have on the family. They urge more studies to determine what happens to turn what is usually a time-limited disorder into what can be a lifetime burden and all that that implies.
“The prevention of the progression from IM to CFS not only saves the patient from the potential of lifelong disability, financial dependency, and the ensuing depression, but may save the family from life-altering care-giving and financial responsibilities; stresses of which alter the family dynamics so drastically and detrimentally that the family unit itself may not survive.”







Who did this study? It’s too bad they didn’t coordinate with Janet Huber at Tufts that has been working along similar lines with Mono and CFS and an endogenous HERV activation possibly causing the link to ME/CFS.
Greg
Sorry about not providing the link.
Predictors of post-infectious chronic fatigue syndrome in adolescents. Leonard A. Jasona*, Ben Z. Katzb, Yukiko Shiraishic,Cynthia J. Mearsd, Young Ima & Renee R. Taylore. Health Psychology and Behavioral Medicine: An Open Access Journal. Volume 2, Issue 1, 2014
Not only who did the study, but where is it published? Do you have a PubMed link to it? Thanks!
Sorry about that Chris. It hasn’t shown up yet on PubMed. I got the link from Prohealth. (Don’t know how they find these things…:)). It’s open access. You can find it here – http://www.tandfonline.com/doi/full/10.1080/21642850.2013.869176#.UvAExJ5dWSo
The Broderick et al study is linked to in the article. It’s this study:
http://www.ncbi.nlm.nih.gov/pubmed/22973830/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3480896/
I hope this study follows these patients for many years to come. I am hesitant when studies like these deem recovery within a couple years and only follow for 5 years. It was not mentioned how the severity was judged, by symptoms or immune response (i.e. high titers to IgM and IgG antibodies).
I became sick at 15 years old, was told I would recover in 5 years. My EBV titers were so high the specialty lab in California had requested info from my doctor whether I had died. So I would be considered one of the more serious cases based on titer vs. just symptoms. (I had just recovered from GI flu and bacterial pneumonia when the tests were done.)
Was 80% back to normal in 5 years, never got back to 100% but I felt “recovered” although if I did not pace I would have slight flares. If you asked me then I thought I was recovered but slightly broken. Now 25 years later, I can look back and see how my illness progressed. Initial recovery, with relapses every so many years due to a period of severe infections. After each relapse, it took longer to recover and then the recovery was at a lower functionality (75%, 60%, 50%). My last relapse started 5 years ago and has progressively worsened to where I am 15% functional.
This is a very interesting study. It would also be good to evaluate how many developed b cell non-Hodgkins lymphoma later in life. That also happened to me, 22 years after initial CFIDS/ME diagnosis. The B cells (lymphocytes) is where Epstein Barr virus initially infects.
This “I became sick at 15 years old, was told I would recover in 5 years. My EBV titers were so high the specialty lab in California had requested info from my doctor whether I had died.” is amazing.
For some reason EBV can really hit women hard particularly during adolescence.
A blog is coming up shortly that will suggest people with ME/CFS may have a unique inability to protect themselves from this virus. Hopefully it will spur more research.
I have been sick with CFS since 1986, when my CMV Titer was off the charts. As a former athlete and military specialist it took me to my knees.
I have fought back over these 28 years but at my best I get 60% and on my worst 10%!
I have yet to see a study on how the long term illness of CFS affects men. I became ill when I was 28 and I am now 55! It has been a long hard road filled with many land mines, from Divorce, Bankruptcy, and so much more.
Interesting, Bob. I got sick with what was later diagnosed as CFS in 1990, testing positive for CMV in addition to EBV as well. I was 31, have had good medical care and all sorts of holistic and alternative care as well, with similar results: at best I get about 60% on some days, but lead a rather housebound life the majority of the time, with, agreed, about 10% functionality on way too many days after more than 24 years.
A male friend about my age had a similar experience and, to this day, leads a very housebound life full of pressure headaches and pain as well. My heart goes out to you guys, as you brave ME/CFS in the minority.
As a female, I do believe hormones can play a role – when my first daughter was 18 months old I “crashed” with mono, which lasted about 5-6 months. Type A that I was, pushed to get back to “normal” and got pregnant with second child about 3 months after I’d been “cleared” as over the mono. Had second child, then “crashed” with CFS when she was 18 months old, on Nov. 25, 1990. I now believe pregnancy hormones (in addition to the stress of pregnancy on the body and motherhood of babies and toddlers; and lack of sleep and insomnia took its toll). Menopause hasn’t exactly been a cakewalk!
Hang in there! There is still beauty in life, even on those 10% days!
Interesting, wonder if mono has an association with FM, something I never thought of. I had mono at 19, got FM about 25 years later.
I would say yes, Steve, simply because a significant number of people with FM have an infectious onset to their disorder.
My understanding is that infectious mononucleosis not only sets up people for ME/CFS but increases one’s risk of getting multiple sclerosis as well. There’s lots of learn about this bug.
I’ve been told that CFS and FM are like “sister illnesses” – each on the far ends of the spectrum, with most patients falling somewhere in between with some symptoms of both. Interestly, my issues (beyond fatigue and post exertional malaise whenever I exercised) were more mental/cognitive “brain fog” in the early years, more like CFS. But as time has gone on (24+ years now) the “fog” has lifted gradually, but the body aches and FM “tender points” have gotten worse every year.
As for MS, I was given that diagnosis by a neurologist a couple of years ago based on brain lesions that showed up on MRI’s when they were diagnosing migraines. I HAD NO OTHER SYMPTOMS OF MS and this doc wanted me to start daily Copaxone shots! My CFS doc (love him – Dr. Charles Lapp) says that 80-90% of ME/CFS patients would show brain lesions in certain areas of the brain that come and go IF they were to have brain MRI’s. Since the other MS tests showed up normal for me neurologically, I’ve declined treatments for MS. Still, if ME/CFS is considered a type of autoimmune illness, I understand the likelihood increases to later get more autoimmune diseases.
Hi, Steve, if your wondering if there’s an association between ME/CFS and FM, I think the answer is yes. There’s very high overlap between the two conditions. At least one study showed that 70% of people with ME/CFS also have FMS (or it might have been the other way around, i.e., 70% of people with FMS also have ME/CFS — remembering details isn’t my strong suit these days).
I had IM when I was 14, then came down with FMS 37 years later. I kept working for about 3 years until I was in a near total state of collapse. By then full blown ME/CFS had ended any prospect of my being able to work.
I believe that first bout of IM did have an impact on my having FMS, and I definitely think it set the stage for my developing ME/CFS.
Deficient EBV-Specific B- and T-Cell Response in Patients with Chronic Fatigue Syndrome http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0085387
Maybe this is the cause for a subgroup. It sounds very good.
It is…A blog is coming up shortly. I ran it by some experts to make sure it was right – so it should be right! 🙂
I found this study very interesting.
I was diagnosed with glandular fever when I was 17, and recovered after a few months. Then, much to my doctors surprise, tested positive again in my early twenties when I was so ill she thought I may have something as serious as leukaemia. After several negative blood tests, as a last resort, she thought she might as well test for EBV and the results were positive. She thought it was only possible to have EBV once, but wondered if I’d ever truly recovered from the first bout. Who knows – that was over 35 years ago.
It took me a couple of years to recover and then 14 years later was diagnosed with M.E.
I’ll be very interested to see where this research leads.
You will find this study also interesting. I hope this mistake was not the case with you.
Epstein-barr virus infection masquerading as acute leukemia: a report of two cases and review of literature. http://www.ncbi.nlm.nih.gov/pubmed/24554817
From a 2006 study- http://www.biomedcentral.com/1471-2334/6/15
A small proportion of people that develop infectious mononucleosis following EBV infection remain sick with chronic fatigue syndrome. Gene expression profiling was used to determine whether failure to recover reflected altered gene expression. The subjects who did not recover from infectious mononucleosis had altered gene expression response during the early phase of EBV infection compared to those who subsequently recovered uneventfully. There were several differentially expressed genes identified including gene involved in the immune response, apoptosis and the cell cycle. A comparison of gene expression profiles early and late following EBV infection revealed that those who did not recover had differentially expressed genes implicating mitochondrial perturbations with fatty acid metabolism, mitochondrial function and apoptosis pathways.
Thanks Chris
Cort,
I’m interested in your EBV/CFS blog. I got mono at 29 and then CFS at 44! But I noticed after my initial illness I couldn’t bounce back from colds very well. The CFS progressed quite a bit since the onset.
I’ve had CFS since contracting a flu at age 4. My mother the same, as my mothers mother. In fact, every member of family from my maternal side has CFS.
EBV is NOT the cause. It is merely one of the many triggers.
I finally found the cause earlier this year. But I am researching
on what I can do. Everyone will be happy to know that CFS
can and will be fully reversible by way of remission/cure.
Lipkin’s study will prove this if it every receives enough funding for lift-off.
hi:
can u pls write me…….i am desperate for hope even if it is just words at this point. i have been severely ill for 9 years and have no life at all. i really am reaching the end of the line here….if lipkin’s study really will provide as with actionable answers perhaps i can fortify myself once again to wait. right now there just seems to be no new treatments and therefore no help re: improvement. i am sad and need a boost of confidence.
pls help if u can
lgrasso_hawaii@yahoo.com
thanks so much!!!
Dear Lisa,
Hang in there! I, too, have had many days when I’d just rather not have to live if it was going to continue that way, but with appropriate self care, attention to nutrition, and mental, emotional, spiritual health focus, I have always slowly come out of a flare to have at least a few “good” weeks or months before the next “crash.” We are all different, so my advice is to look for opportunities in your area for more holistic healing modalities and give the one(s) you resonate with a try. There is no magic pill, but I believe “healing” can happen even without a “cure.” And know you are NOT ALONE! Sending healing love and light your way!
I got mono at 12 & the fatigue has stayed with me since … 22 yrs later. I am much sicker since getting pregnant with my 1st child (5 yrs ago). Something about my 1st pregnancy & 2nd delivery really effected my body for the worse. I feel like they were both mini tramas & created worsening of my fatigue & many more symptoms.
Thanks for the info Cort!
I am curious… has anyone gotten any better from long term anti-viral treatment?
Cort, have you thought about maybe doing a survey about what we have done to help heal our different symptoms? Similar to what you did with people who took the B1?
I have worked very hard for the last 5 yrs to heal myself & have had a lot of success with healing several of my symptoms & I am curious if other people have too. I figured we could share this information some how…?
Just a thought…:-)
I second that thought.
Methylcobalamin shots twice a week. Methylfolate daily. Vitamin D3 daily. Cut out artificial sweeteners. Eat a more whole food diet and juicing vegetables and fruits have helped me considerably.
My doctor put me on the Whole30 diet. I’m also committing to all organic. I’ve been shocked by the improvement in my energy and lessening of my depression. I’ve been losing weight, but she refers to it as losing inflammation. She’s a Fundamental Medical doctor.
Thanks Cort …. I feel a combination of all 3, but 1st and foremost is Fungal mycotoxicosis, which then opens the door for Bacteria and Virus – Start with the Fungus, the root of the cause! and IMO it falls on NASA and the DOD’s deep space Gemini and Apollo experiments. They brought back some dangerous stuff and had no way to harness it. Fungus has since been denied for many a year in Courts with Media playing along to negate illness and deaths. Learn about the HUGE now world wide FRAUD against the PEOPLE – Please see details at: http://katysexposure.wordpress.com/2014/01/03/update-on-rico-lawsuit-against-san-diego-judges-et-al/
I am working on repairing the gut conditions first, by taking daily sauerkraut. That way, any tablets, etc I swallow, will then have a better chance of being assimilated. Sauerkraut is loaded with bio available vitamins, enzymes etc, and is best looked up for further information.
It has been used for centuries in Europe and Russia, for aiding optimal health through the harsh and frugal conditions of winters.
So far. the repetitive irritable bowel syndrome, experienced by so many ME people, has in me reduced, and now stopped.
I figure that any helpful hints that might crop up , will be better employed now, with some improved possibility of success?
My CFS started with mono at the age of 36 & it is as if it never went away. I am now 58.
I too had a bad case of IM at 18. It took me a year to fully recover. 17 years later Hashimoto’s and a downward spiral. What’s interesting is that when I’m in a flare-up, EBV is reactivated. I worry about MS because my brother was diagnosed with it 5 years ago and Dr. Klimas said that people with CFS can get MS also.
I thought the EBV connection was no longer valid. I had mono when I was 18. I got ME
at about 25. I was in great shape, a runner. It progressively got worse. I was misdiagnosed with depression. I’m 51, now. Recovery from flares is more difficult and I
don’t recover to my original state.
I was completely bedridden for 4 years. It took many more
years to recover from that “flare”.
It is very difficult for me to maintain my life. Cooking, cleaning, laundry are nearly impossible for me to do without causing relapse.
I also remember reading that childhood trauma DID contribute to the likelihood of contracting
ME.
I moved to Chicago and have never found a doctor even slightly knowledgable (and therefore willing to treat) ME. Anyone out there have a great doctor?
My daughter at age 12 had IM that was quite mild other than intense fatigue. She was a competitive athlete, working out 20 hours per week. After recovering, we didn’t notice CF symptoms until almost a year later, when the load on her increased (workout schedule plus school schedule). She could hardly function and her sport suffered. Somehow she maintained her grades despite missing a great deal of school, due to fatigue and frequent illness. All testing (ID, Allergy and Immune, etc.) was normal, showing history of EBV but none currently active. We have seen various specialists in our area, but no one who can seem to diagnose her or offer symptom relief. She had to give up her sport because her lack of endurance risked her safety. She seems to have bouts of almost normalcy then will have a week or two of unrelenting, overwhelming fatigue. She has learned to live a strict sleep routine (hard for a teenager to explain to friends) and give up activities on weekends to have time to “recover” from the week. She is also being looked at for potentially having cyclic vomiting syndrome. It has been so discouraging to not have answers and have doctors look at you like you are making this up because the tests show nothing. I cannot seem to find anyone whose history is quite like hers as everyone’s illness seems so much more severe. But I am so thankful for the information that is provided here.
Good luck Shawn
Make sure she continues not to overdue and hopefully she’ll work her way out of this. I do know of one person with ME/CFS who had cyclic vomiting problems that resolved. I think they were tied to his gall bladder.
I know my CFS is EBV related but I was 42 when I came down with EBV, not a teen or kid so I was part of the small population that is just never exposed then, and I just never got better. My job & family obligations were high-stress but I also have co-morbid genetics that are auto-immune related. I function at around 50% of the 110% I used to be, some times better, sometimes worse. Thank you for this article!
It really appears Cynthia that the earlier you get exposed to EBV the better. Children usually blow through it, teenagers can get infectious mononucleosis and I imagine that many adults who are exposed for the first time may get ME/CFS.
Agreed. My son was 4 1/2 at the time & we came down with a “cold” the same day. He bounced back in a few days but I could hardly lift my head for two weeks so I went to the doc & got the mono diagnosis. He’s almost 14 and fine now. 🙂
I have a question if someone can answer it please.
My initial illness in 1986 was caused by an EBV infection which my doctor documented by following my EBV titers. It culminated in ten months according to the titers and I experienced the worst pain in my 28 years of ME/CFS. I remember alternating between different pain relievers every two hours and still being in unbearable pain. But at the same time I tested negative on the mono spot test. I’m don’t understand how this could be?
When the name Chronic Fatigue Syndrome came into usage, my doctor said he didn’t care what they called it now but that what I had was a Chronic EBV Infection. He also asked whether I had been in Tahoe in the previous year; I had. Since EBV is ubiquitous, I can’t help but wonder if some environmental toxin there triggered that outbreak. Something that prevented our immune systems from fighting off EBV.
Also, I was in the third trimester of my pregnancy while visiting Tahoe and became ill when my son was 8 months old. I wonder if there are parallels between adolescents, pregnant women and menopausal women in terms of how hormones impact the length and severity of illness?
Finally, does anyone know of any doctor in Nashville, TN who knows anything about ME/CFS? Thanks Cort for all you do. May we all be well in spirit.
My partner got so ill with Mono in 1980 that she missed a semester of college (couldn’t even walk up and down the stairs more than once per day). She was an all star athlete, but never recovered fully. It was tough to get a diagnosis in those days, however, we figured out that she had CFS. I came down with CFS a few years later. (Contagious??? I wish there were more research being done on that!) I’ve always been on the lookout for research connecting the two illnesses.
Another athlete bites the dust! Interesting question. I assume that she was shedding virus particles like mad for awhile. If you’d already been infected with EBV – as most people are by the that time, then theoretically I wouldn’t think it would matter. However, Lerner and Williams do believe a defective form of EBV is present in some ME/CFS patients and I wonder if she had another strain or form if that would matter. (????)
I just found this article and find it helpful. I got a pretty severe case of mono when I was in college. I don’t know what the exact blood results were, but the ER doctor told me I was VERY POSITIVE for mono. When I saw a doctor for follow up I was told I was in the clear. That doctor LIED! Since I had mono 24 years ago I’ve been suffering from CFS which has given me severe depression, a lack of concentration, I feel like I have brain darts ALL the time, and I turned into an introvert. Mono screwed me up ALOT!
I had a severe EBV infection in 1986 at 20, have been ill ever since.
I had a lumbar puncture 4 years ago, which showed high EBV in the CSF, but no comments were ever made about it.
Surely it’s not normal to have viruses in your CSF?
Re:contagion, my former partner contraced ME after me, and both my adult children meet the criteria.
I think it is definitely contagious, I was iller during both pregnancies and breastfed both longterm.
My son succumbed at age 19, almost the same as me, after an EBV like illness that didn’t show EBV, strange!
I happened upon this site accidentally but am so glad I did. My story is so like everyone else’s here.
I was very athletic;playing football,hockey and track in high school and through two years of college. At the end of my sophomore year in college I came down with mono and my life was never the same. Went to dr. after dr. and was basically told I was suffering from depression. Anyone feeling this exhausted day after day after day for years would be depressed. I am now 63 yrs. old but feel that my life has been just surviving from day to day and living a flat line existence.