



In conclusion, our findings indicate that mifepristone may play a pivotal role in the control of inflammatory responses and suggest a new clinical application for mifepristone — Chen et. al
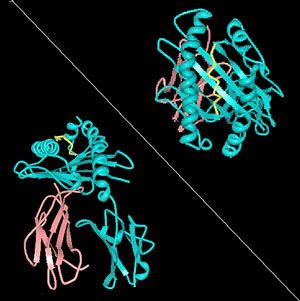
Natural Killer Cells
In the last blog we looked at the potential for an antibiotic called minocycline to be repurposed to reduce neuroinflammation in ME/CFS and or FM. Now we look at an abortion inducing drug, no less, that can enhance natural killer cell functioning.
Natural killer cell functioning is a big deal in Chronic Fatigue Syndrome. No immune factor has been studied more or found to be more consistently abnormal. Several new NK cell studies were reviewed at the IACFS/ME Conference. The CDC is working on a cheaper, more accessible NK cell functioning test, and Dr. Sonya Marshall-Gradisnik of PHANU recently co-authored a dense chapter on natural killer cells and ME/CFS in a medical book.
Doctors report that some people with ME/CFS demonstrate extraordinarily low natural killer levels. Dr. Andreas Kogelnik has said if he had a good natural killer cell booster he would be giving it out like candy to those with this disorder.
NK cells are a big deal.
Drug Repurposing
Drug repurposing has become a big deal as well. The CFIDS Association and the Klimas Research group at Nova Southeastern University are dedicated to finding new drugs for this disorder that have already been FDA approved but have slipped by clinicians, and, of course, Dr. Pridgen is testing combinations of antivirals and anti-inflammatories for use in Fibromyalgia and ME/CFS.
Throw the need to boost NK cell functioning in ME/CFS and drug repurposing together and what do you get? Perhaps you get a drug used to induce abortions that boosts NK cell functioning at the same time. Perhaps you get a drug that does that by affecting a system – the HPA axis – that’s under duress in ME/CFS. Perhaps you get a drug that appears to works effectively (now in combination with another drug) that prompts the autonomic nervous system to boost immune responses. Perhaps you get RU486 – Mifepristone.
Mifepristone increases the cytotoxicity of uterine natural killer cells by acting as a glucocorticoid antagonist via ERK activation. Chen Y, Wang Y, Zhuang Y, Zhou F, Huang L. PLoS One. 2012;7(5):e36413. doi: 10.1371/journal.pone.0036413. Epub 2012 May 1.
Mifepristone’s abortion-inducing properties appear to be due to its ability to increase natural killer cell functioning enough to disturb the attachment of the embryo to the placenta. Natural killer cells serve dual purposes in the placenta: in their latent state they support placental growth, but, if their cytotoxic properties are turned on, they can inhibit it as well. It’s intriguing, given the number of gynecological abnormalities CDC studies have found in women with ME/CFS, that natural killer cells are the most abundant immune cell during embryo implantation and early placental development. Could reduced NK cell functioning be impairing placental growth?
Anti-Glucocorticoid Properties Spell Caution
For years researchers thought progesterone regulated NK cell functioning in the uterus, but recently it’s become clear that high cortisol levels reduce NK cell cytotoxicity in the uterus.
Mifepristone in an anti-glucocorticoid; it actually blocks cortisol’s ability to bind to glucocorticoid receptors on our cells and that could spell trouble for people with ME/CFS or FM with low cortisol levels or a poorly functioning HPA axis.
Another study examing mifepristone’s effects on bi-polar patients with normal HPA axis functioning, however, found that mifepristone increased the “cortisol awakening response” (CAR). The CAR refers to a dramatic increase in cortisol that normally occurs about a half hour we wake. It’s the CAR that’s disturbed in ME/CFS.
Natural Killer Cells
Studies indicate low-dose mifepristone increases NK cell cytotoxicity and perforin expression. Perforin is the substance NK cells uses to ‘drill holes’ into invading cells and studies suggest reduced perforin expression is hampering natural killer cell functioning in ME/CFS.
Gulf War Syndrome Connection
The authors concluded mifepristone should be explored further in other diseases, and it is indeed — in Gulf War Syndrome. A 2008 GWS study — still listed as recruiting patients according to Clinicaltrials.gov — is giving low dose mifepristone (200 mg/day, about half of what’s used to treat Cushing’s disease and a third of what’s used to induce abortions) to GWS patients to see if their overall health and cognitive function improved and if it relieved their depression and PTSD.
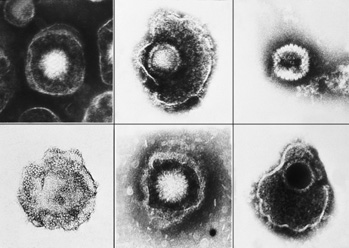
Herpesvirus Connection
Another indirect connection to ME/CFS also exists. About 20 years ago, a study led by ME/CFS and herpesvirus researcher Ron Glaser infected mice with herpes simplex viruses, put them into restraints (as a way to stress them) and then watched their immune systems tumble.
Specifically, the stressed-out herpesvirus-infected mice weren’t able to mount normal cytokine and cytotoxic T-cell responses, their immune cells were not able to penetrate the infected areas, and their herpes simplex levels went up. The mice also became more susceptible to further infections.
The Glaser team then used mifepristone to restore (by blocking glucocorticoid receptors) the cytokine responses, but the T-cell cytotoxic activity remained inhibited. They restored full T-cell cytotoxic activity by using a beta blocker called nadolol. The intersection of a herpes virus infection, natural killer cells, and autonomic nervous system functioning in this study is intriguing.
Mifepristone also appears to have neuroprotective properties – particularly with regard to the hippocampus.
Conclusions
With studies underway examining its effectiveness in GWS as well as prostate, brain, and nervous system cancers, ‘stress sensitivity’, Cushing’s disease, depression, and its ‘original’ use for abortion, mifepristone is getting a good workout at the clinical level.
Mifepristone’s anti-glucocorticoid properties suggest it may not be appropriate for HPA axis suppressed ME/CFS patients but it’s cortisol enhancing properties suggest that it might be. However the mifepristone saga ends up, it and minocycline provide examples of the surprises that await as researchers dig deeper into how drugs work, and this provides hope that better drugs for ME/CFS and Fibromyalgia are already, without our knowing it, among us.







“The CDC is working on a cheaper, more accessible NK cell functioning test.”
I hadn’t heard about this before. Do you have more info on that? Did they announce this publicly? Is there a timeline?
You’ll see this in an upcoming blog. They talked about it at the Immunology Workshop.
Mifepristone has a long and extremely “checkered” past to say the least. As well it has some very serious side effects in women, I personally wouldn’t put much hope in this drug for ME/CFS.
I agree the drug has issues. However, the authors of the article suggested using it in low-doses for inflammatory disorders, and other drugs with checkered pasts (thalidomide) if used differently can be helpful. Not saying this drug is appropriate for ME/CFS but it may be a possibility for some people at some point.
It does raise NK cell functioning, it was helpful (with a beta blocker) in reducing herpesviruses in one study. It does appear to have neuroprotective properties. It’s interesting…:)
Cort your article grabbed my attention when I got to the end and beta blockers were mentioned. I have wondered if that class of drugs would be useful if ME/CFS involves inappropriate messaging in the nervous system. A friend of mine suffered from rheumatoid arthritis for years until they tried treating him with beta blockers. After treatment his pain subsided and he was able to get back to cycling and other activities. Do you know of any other research with beta blockers and ME/CFS?
How did they treat with beta blockers? I am very interested, I have RA.
But understanding how these drugs do what they do – their mode of action – can still be beneficial. Potential clinical trials using various dosages and learning what subsets of patients with ME/CFS could safely take this drug might lead to one choice of treatment, among others.
I was diagnosed with ME/CFS in 1998 by Dr. Patricia Salvato in Houston, TX. Before I finally saw her, I had been through the proverbial doctor ringer for over a year. One of her main tests to help her diagnose ME/CFS was NK cell count (and later on, NK cell function). Not surprisingly, mine was way below normal. Of course, she used patient symptoms and history to diagnose, as well. At that time, she said in a large number of her patients, when NK cell count went up, they felt better. In those years, Dr. Salvato was trying various methods to raise NK cell counts, as well as running small clinical trials on her own patients.
I wanted to try low dose naltrexone (LDN) last year, but my rheumatologist flat out refused to even consider it. However, she treats my FM. Up here in NY, I don’t have a doctor who treats my ME/CFS. Since I get along fairly well and can rest when I wish (I’m retired), and I use affordable supplements and pain meds for moderate symptom management, I am no longer concerned about running around trying to find a suitable doctor. I turn 70 in December. Aging will throw in its own set of challenges.
Let’s hope that all these various findings and conclusions will take a more refined shape not too long into the future, rather than these mountains of information remaining an amorphous, shapeless blob of “possible” ME/CFS treatments!
Thank you, as always, Cort, for your continuing mission to gather and share the latest ‘scoops’ in the world of ME/CFS. I know I wouldn’t be aware of or have read a fraction of what you bring to us on this magnificent blog. (No, I’m not being paid for this endorsement!!) 😉
Cheers! Judith in NY
Check is in the mail 🙂
This is really fascinating – I looked into mifepristone years ago as potentially a way to reset the HPAA, and wrote to one of the authors of the “Model-Based Therapeutic Correction of Hypothalamic-Pituitary-Adrenal Axis Dysfunction” paper to ask for an opinion on using RU486 for that purpose. I went so far as to buy some from Israel but was too nervous to try it as anything but a last resort. It’s been sitting in my refrigerator ever since. I didn’t know about the NK boosting function then, only the anti-glutocorticoid effects, so now it looks even more interesting. I tried other milder anti-glc agents (herbals), and some definite changes in HPAA function appeared to take place that led to positive long-term results. Now I’m more intrigued than ever to try the RU486, at *extremely,* extremely low doses. Eventually, as the HPAA hopefully resets and becomes more robust, it might be possible to increase the mifepristone dose accordingly and thereby “stair step” the HPPA back up into more normal functioning. That is the theory, at least. Thanks for posting this article.
I was thinking of that article too when I read that mifepristone increased morning cortisol (instead of doing the opposite). Did it reset the axis..?
Interesting that milder anti-glucocorticoid agents helped. If it wasn’t Broderick you talked to you might want to talk to him. He’s gone much further with the HPA axis/immune modeling now….I would love to hear what he thinks of this.
(A blog is coming up on his work :)).
Thank you for the reports on drug research, Cort!
When I hear about studies like the one trying low dose mifepristone on GWS patients, I always think “What would happen if they tried 5 mg/day of it?”
Medical researchers have their idea of “low dose” but some of us CFS patients have our own idea of low dose.
That’s for sure. 🙂 It’s amazing what some people can do if they start out really, really low.
I’ve been searching the web for info on healthy amounts of NK cells. Mine are low according to lab results ordered by Dr Kaufman of the OMI. I forgot to ask him what a normal range would be. I’ve had ME/CFS for 18 years & am currently stuck in a 2 year severe relapse.
I’m not convinced by the natural killer cell theory. They are low in many disorders and that is often a result of stress/depression induced by the disease.
Since, I never get colds or flues and over-react to anything and everything my body deems foreign (eg chemicals etc), I doubt very much that the reason for my ME/CFS symptoms are caused by a lack of NK cells. I believe my ME/CFS is caused by just the opposite; an immune system in overdrive, that just doesn’t know when to quit. When, I discovered how to calm “my” hyper-immune response; “my” case of ME/CFS greatly improved. No lack of natural killer cells here!
FOR RACHEL”
how did you calm your overactive immune system. this is my problem also. any advice/insight appreciated.
cort can you pass this on to rachel.
thanks
lgrasso_hawaii@yahoo.com
How did you do this Rachel?
Thank you for this information. Who is using the treatment that you described in this article? Are they still using Minocycline as well? I tried low dose naltrexone but after several days, it caused a major headache. Thanks for keeping us all informed Cort!! So grateful to you!