

A Different Kind of Neurological Disorder
Chronic Fatigue Syndrome (ME/CFS) is sometimes described as a neurological disorder – as if that term described something discrete. When people first spoke of ME/CFS as a neurological disorder they probably meant a central nervous system condition – problems with the nerves in the brain or spinal cord. Van Elzakker and others opened up the idea that infections in the vagus nerve and dorsal root ganglia and other nervous system tissues close to the CNS tissues may be present.

Nerves all over the body are being questioned in ME/CFS. Now Dr. Rowe proposes a different kind of nervous system problem is present.
Fibromyalgia studies suggest damage to the small unmyelinated (and perhaps larger myelinated) nerve fibers on the periphery of the body in the skin and perhaps extending inwards may have occurred in some people. Some postural orthostatic tachycardia studies suggest that ‘cardiac denervation’ – damage to the nerves in the heart -may be present.
Now Dr. Peter Rowe – one of the first researchers to study orthostatic intolerance in Chronic Fatigue Syndrome (ME/CFS) – is breaking new ground again with a different kind of nervous system issue. He believes something has gone wrong with the nerves that govern a very basic function – movement.
The breakthrough for him came when he realized that he was able to produce symptoms of pain, fatigue, brain-fog, light-headedness, nausea, sweating and flushing, vision changes, headache, etc. simply by putting pressure on certain parts of the spinal cord or nerves in the body, arms or legs. Conversely, removing the tension in those areas could ease his patient’s fatigue, cognitive problems, light-headedness, nausea, reflux, sweating, and flushing, many types of vision changes, headache, and other symptoms.
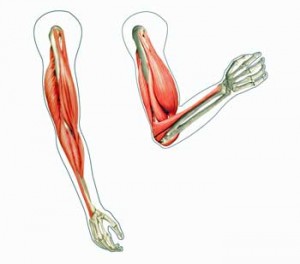
Rowe describes a remarkably fluid body where, as we move, bend, and strain, our bones, joints and muscles and nerves constantly change position to stay in harmony. Our nerves and our spinal cord actually lengthen or shorten – and not just a little bit – as we move. The median nerve in your arm, for instance, elongates 20% as you move your arm from a flexed position (as if you were doing a curl) to an extended position (where your arm is straight).
The spinal cord elongates enough for doctors to be able to use it to test for the central nervous system inflammation seen in spinal meningitis. Raising the legs of a person lying flat causes the spinal cord to come in contact with inflamed tissues at the dural membrane (at the base of the brain?) causing neck pain if you have spinal meningitis.
Nerves that aren’t elongating properly appear to be causing pain and other symptoms in at least some people with ME/CFS.
These nerves contain both motor and sensory fibers, and many contain autonomic nerve fibers as well as connective tissues. As they’re elongating and contracting they’re relaying information on such basic functions as touch, pressure, pain, temperature, position of the body, blood volume, blood flow, etc. back to the brain.
But what if those nerves aren’t moving in tandem in with the muscles? What if inflammation or some other factor has restricted their ability to elongate? Mechanical tension in the nerve will build causing pain and other symptoms. Reduced blood flows, reduced muscle recruitment, improper muscle contractions, etc. may result. Over time the continuous pain signal inputs to the dorsal horn neurons from the damaged nerves could contribute to the central sensitization found.
All that could translate into pain, problems with exercise, muscle fatigue, autonomic problems, and perhaps even orthostatic intolerance.
The Study
Forty-eight consecutive adolescent ME/CFS patients entering Rowe’s Johns Hopkins Clinic and forty-eight healthy controls were assessed for range of motion in eleven areas.
The ME/CFS adolescents were found to have significantly restricted ranges of motion (ROMs) in six of those areas. Restricted ranges of motion were also found in healthy controls, but they were much more common in ME/CFS (p<.001).
Perhaps more importantly, exceeding their range of motion rarely produced symptoms in the healthy controls (4%) but often did in the adolescents with ME/CFS (40%) (p<.001).
The upshot was that restricted motion was much more common in the adolescents with ME/CFS, and when it was exceeded they often experienced pain, fatigue, and other symptoms while the healthy controls rarely did.
Think about it: if every time you exceed your range of motion you experience pain, fatigue and a host of other symptoms – you’re not going to be moving much. Could bollixed ‘neurodynamics’ have put people with ME/CFS in lock-down mode? Is this at least part of what is causing movement to be so difficult at times?
Discussion
How It Starts
Rowe believes the onset of the neurodynamic problems probably preceded ME/CFS or FM. Essentially the system was primed for trouble and simply needed a push — an infection perhaps in combination with prolonged period of inactivity — to freeze into place.
Dr. Rowe believes faulty neurodynamic system probably got exacerbated and then locked into place when ME/CFS patients went down…
During that time a kind of ‘frozen’ muscle/nerve system, the antithesis of the fluid, dynamic system that existed before, became locked into place. Once that happened, nerve elongation became compromised, nerve tension occurred, and movement often became painful and a source of concern.
That spells trouble. Rowe noted that the costs of inactivity are so high that it’s now standard medical practice to get even ‘the sickest hospitalized patients’ mobile in some fashion as early as possible.
He readily acknowledged the difficulty of this, particularly for the most severely ill, in what is, by definition, an activity-challenged illness.
Rowe doesn’t push patients to get more exercise; instead he offers treatments and therapies such as florinef, beta blockers, midrodine, and bodywork that provide more energy first.
Exercise and Stress
Patients with neural and soft tissue restrictions in the range observed in those with CFS typically experience worse symptoms after exercise. We speculate that this occurs as a consequence of the repetitive mechanical tension exerted on an already less than fully compliant nervous system. Rowe et. al.
These types of neurodynamic issues clearly have the potential to muck up exercise in ME/CFS. If the nerves are compressed or cannot elongate then every movement during exercise will produce mechanical tension; i.e. pain and inflammation. Indeed, post-exertional malaise could simply result from the inflammation and heightened central sensitization that occurs as the brain was slammed with pain signals. (The widespread pain after exercise that can occur in areas that have not been exercised suggests that central sensitization has occurred.)
I don’t know if my range of motion is affected, but Rowe’s work grabbed me because intuitively it fits my experience post-exercise. The range of motion I can go through without producing pain declines dramatically after exercise. Sometimes it seems I can hardly move without pain darting across my body.

With the constant need to elongate the nerves, exercise would be particularly affected in Chronic Fatigue Syndrome
Stress, which for me tends to be accompanied by rapid, short breathing and tightened musculature, has a less dramatic but similar effect.
The short uptakes in breath that I associate with stress appear to lift my body into a painful alignment, whereas breathing from the belly puts it into a less painful position. My guess is that both exercise and stress in my case move the muscles and nerves into more compromised positions thereby causing pain.
Some of the practices Rowe recommends, such as yoga and tai chi, involve both relaxation and movement.
My guess based on my experience is that fluidity of movement declines over time in ME/CFS, and that higher percentages of adults would have restricted ranges of motions. I’ll bet that the same study done in Fibromyalgia would have more ROM and higher levels of distress.
Testing
Rowe determines if patients have altered ‘neurodynamics’ by doing ‘neural provocation’ tests where the limbs are put into positions which require nerve elongation. These strikingly mild tests — which require no muscle exertion — can involve simply have someone slowly raise their leg while lying down to 20 degrees.
When this was done to one young man with particularly neurodynamic issues his fatigue, brain fog, and visual problems skyrocketed over the next twelve minutes. At the end of that short time he was having trouble forming sentences.
Signs and Symptoms
Most obvious is a stiff upper and middle thoracic spine with rounded shoulders and a forward head. Patients find that it is difficult to straighten up and tuck the chin. The rib cage is often very tight, and rotational range of motion is markedly limited. Pressure on the rib cage can give rise to diverse symptoms including vision changes, lightheadedness (to the point of near-fainting), and other autonomic nervous system sensations. Rowe
The muscles near where the nerve cross the joints, in particular, may reflexively shorten and may appear firm, tense, and tender to the deep touch. Even the skin can become affected as it loses its ability to move and glide and adjust temperature accurately, and may begin to sweat. Other indications are reduced range of motion (reduced flexibility), increased resting muscle tone, and pain or other nerve sensations.

This is an exaggeration but physical therapists do find an increased incidence of hunched shoulders in ME/CFS. Could problems with nerve elongation contribute?
Physical therapists associated with Dr. Charles Lapp have noted that the pinched-in chests and rounded shoulders can make it difficult for people with ME/CFS or FM to take deeper breaths.
Rowe finds that stiff upper and middle thoracic spine with rounded shoulders and a pushed-forward head is common in ME/CFS. Straightening up and tucking one’s chin in is often difficult. In my experience exercise significantly exacerbates these problems.
For me, the tightness in my upper body begins around my sternum and then accelerates as you go upwards. I have a very lax abdomen and a very tight chest area. Tucking my chin produces pain in the back of my neck.
Rowe also finds that as many as 2/3 of the adolescents he sees have joint hypermobility, and a group has Ehlers-Danlos Syndrome, a hereditary connective tissue disorder causing the same symptoms. Impaired neurodynamics particularly occur in this group where the nerves pass by hypermobile joints or where lax ligaments anchor the spine.
Treatment
Treatment of areas of diminished soft tissue compliance and adverse neurodynamics … has become an important part of our treatment approach to CFS. – Rowe
The goal of his physical therapy is to enable normal movement by reducing the restricted range of motion present. He noted at a CFSAC presentation that the type of physical therapy done in his office is the one treatment his pediatric patients invariably ask for more of.
Specific types of gentle movement are the key. His team uses methods developed in Australia by Robert Elvey, P.T., David Butler, P.T., Jean-Pierre Barral, D.O., and Alain Croibier, D.O. in France. Anything that asks the tense tissue to stretch is out.
You basically start from where you are – with a ‘frozen’ muscle/ nerve interface – and cajole it to relax and move. Muscle and myofascial stretching, for instance, are no-no’s as are ‘direct joint and neuromobilization’ techniques.
Instead, ‘indirect techniques’ that are applied in a ‘direction opposite to the barrier to movement’ work. The techniques include myofascial release ‘in the direction of ease’, functional technique, and strain and counter-strain and cranio-sacral techniques. Calling these techniques ‘very subtle’, Rowe nonetheless asserts they can provide ‘excellent’ results. He noted that this muscle/nerve work is one treatment his patients always want to return to.
Are neuromuscular problems causing ME/CFS? Even Dr. Rowe probably wouldn’t say that. Are they contributing significant amounts of pain, distress and disability to the disorder? That he would agree with. My guess is that Dr. Rowe has opened up something big. Check out the interview we did with him below.
- Unrestrained: An Interview with Dr. Peter Rowe
- Find out more about Dr. Rowe’s approach and his Solve ME/CFS Association neuromuscular study








Such a huge problem,…mid back/sternum – and up, fighting that curve. Trying to explain to a doctor that your shoulders, areas of your neck, jaw, and hairline,…are, or have been frozen. It’s taken me almost a decade, to be able to have impact on those muscles with stretching and exercise. Being bedridden and constantly hospitalized in the 90’s, didn’t help. Wouldn’t most practitioners consider this CMP? Fascinating and explains so much for me. Thanks Cort!
Seemed to fit me too! That upper body problem is really something…
Yes mines there’s constant are you hypermobile
Thanks for the great articles.
I have no obvious muscle or joint pain with my ME/CFS, but my fatigue and intra-cranial pressure (along with the brain fog) are worse after exercise. I feel a sense of pressure/pain in the center of my head, right where the vagus nerve is supposed to terminate. I don’t know why other people have much more muscle and joint pain, but I’ve read that Van Elzakker thinks it may have to do with the virus affecting different regions of the vagus. The virus (or whatever) must irritate the nerves; Rowe’s exercise routine must handle those nerves gingerly. I exercise regularly, the same amount, but take a day or so off once a week. I just don’t want to get deconditioned, despite the price paid. I’d do the Rowe method, but I’m too set in my ways.
Re: the vagus nerve and infections. Thanks for the opportunity to post this article I found the other day:
World J Cardiol. 2014 Jun 26;6(6):502-6. doi: 10.4330/wjc.v6.i6.502.
Respiratory modulation of cardiac vagal tone in Lyme disease.
Puri BK, Shah M, Monro JA, Kingston MC, Julu PO.
Abstract
AIM:
To conduct the first systematic test of the hypothesis that modulation of cardiac vagal tone is impaired in Lyme disease.
METHODS:
The response of cardiac vagal tone to respiratory modulation was measured in 18 serologically positive Lyme disease patients and in 18 controls.
RESULTS:
The two groups were matched in respect of age, sex, body mass, mean arterial blood pressure, mean resting heart rate and mean resting cardiac vagal tone. The mean maximum cardiac vagal tone during deep breathing in the Lyme disease patients [11.2 (standard error 1.3)] was lower than in the matched controls [16.5 (standard error 1.7); P = 0.02].
CONCLUSION:
Respiratory modulation of cardiac vagal tone is impaired in Lyme disease, which suggests that Lyme disease may directly affect the vagus nerve or the brainstem.
Full article at: http://www.wjgnet.com/1949-8462/full/v6/i6/502.htm
Some people the vagus nerve gets ‘trapped’ by the surrounding structures. I don’t know what wouldn’t make sense as well. There’s the chiari malformation problem some people have. I imagine a percentage of the population has structural problems that contribute to all this.
I doubt it’s structural as the symptoms occur after an illness and change in intensity with the illness. That’s also why I’m skeptical of the mold explanation.
The illness could have tipped structural problems over the edge, exacerbating and creating more trigger points and also mould is a perpetuating factor for trigger points.
I’m at a loss trying to come up with some notion of how this “scientist” came to the “conclusion” that “neurodynamic” symptoms precede ME/CFS. So much BS out there it’s no small wonder in 35 years no progress has been made.
Lets see, I was in training, had just finished a hike in the desolation wilderness- clearly out of shape and “primed” for ME/CFS!
Wait, I think we all tire easily and that precedes our onset of ME/CFS- that works for me, a new theory!
Some day we’ll find some research you like Greg..:)
This “scientist” has co-authored dozens of research studies and was fundamental in proving orthostatic intolerance is present in ME/CFS.
I don’t understand that idea either but based on what he’s done I’m going to give him the benefit of doubt on it; not that it’s true, but that there’s some good reasoning behind it.
I too, do not have much muscle and joint pain on average but I do have tendonitis, a lot of inflammation.
My primary provider and other specialists don’t seem to have any knowledge of “low blood volume” which I believe most of us deal with. As I grow older, all these issues are exacerbated, of course.
I’m sure it’s the primary cause of “air hunger” especially at the end of the day and early in the morning because a tired heart muscle and diaphragm coupled with low blood volume result in less oxygenated blood to the brain.
I think we all are aware the body does it’s best to compensate for whatever physical issues we deal with and not the least is “low blood volume”. Low blood volume, in my experience results in “dehydration” although, I rarely get thirsty. So, I know to drink water regardless.
Why, low blood volume to begin with? Lower blood volume is easier for the heart to pump all through the body. I have chronic high blood pressure (I believe) due to vasoconstriction, to get the blood up to the brain, especially when my gut is highly inflamed and there is less blood to go around.
I drink at least two or three liters of water per day and only a small amount comes out during the day, I don’t have edema but I retain most all liquids while awake but as soon as I fall asleep I’m up 5 or 6 times during the night to easily urinate out at least 2 liters, or more, no problem, as the body knows low blood volume is not as much an issue as when one is up and awake!! Few physicians seem to be aware of this. None, that I know of, because, when I asked why so little urination during the day and so much at bed time, they have no idea.
Plus, that explains the reason for scary air hunger in the morning, unless I get up and drink a couple of glasses of water, as I’m dehydrated by morning. RP
I really wish there was more focus on blood volume…I don’t know why there isn’t since it’s a pretty rare condition that can explain a lot – although certainly not everything.
Regarding the disparity between daytime and nighttime urinary frequency: here’s what my mother’s urologist told me about her similar situation. “She drinks during the day, does not urinate much during the day, but does at night. All of that nighttime urine has to be coming from somewhere. So the question is where is where is it coming from? The fluids that she is drinking are collecting in the so called ‘third space’, then at night when she lays down in bed she elevates her legs and it leaves the third space. It has to go somewhere, so it goes to the bladder, and then comes out.” He told me to have her elevate her legs for 2-3 hours before going to bed at night. When she does, the problem goes away. She has never had any visible signs of edema. Hope this helps you sleep better.
You might also want to get checked for sleep apnea syndrome.
It is very sad that a person in such an important position as Dr Rowe’s fails to mention or is ignorant of the presence of trigger points (knots) in the muscles. Trigger points cause a restricted ROM and obstruct nerves causing pain, weakness and autonomic symptoms by shortening and widening the muscles. They can cause interference to the peripheral circulation resulting in allodynia, neuropathy and an overproduction of mast cells. Widespread trigger points can be caused by over activation of the sympathetic nervous system and are exacerbated by exercise, poor nutrition, metabolic imbalances, infections and weather extremes. Trigger point activity can vary from latent which causes weakness through to a high level of activity resulting in severe pain and severely restricted ROM. Direct manual application to the trigger points using a variety of simple tools can relieve enough tension to immediately reduce or even eliminate symptoms and the level of overall trigger point activity can be reduced by taking pregnenolone which helps to normalise cortisol levels. Inceased trigger point activity in one area distorts posture resulting in increased trigger point activity in other areas of the body which is why exercise can cause widespread pain and post-exertional malaise. I have fibromyalgia and before I started doing my own trigger point therapy and taking pregnenolone, I could be so immobilised by trigger points that I couldn’t move enough to get out of bed and when I could walk, it was only with support as I was so bent over and weak. When I get short of breath, massage to various trigger points in respiratory muscles relieves it immediately. Please refer to Myofascial Pain and Dysfunction, The Trigger Point Manuals Vol. 1 and 2 by Travell and Simons or The Trigger Point Therapy Workbook by Clair Davies.
Rowe doesn’t mention trigger points or myofascial pain but I asked him about that in the interview and you’ll see something on it there. It’s hard for me to imagine that they’re not connected with what Rowe is finding.
Thanks for info. I definitely want to learn more about trigger points. I didn’t know that SNS activation was involved!
Agreed – I was lucky enough to access a very talented clinician who treated the trigger points in my occipital area. I did not have enough range of motion in my neck to do a shoulder check while driving but that has now been completely resolved. I do still have multiple trigger points and they all restrict movement. Deactivating an active trigger point results in immediate increases in range of motion.
With all due respect to Dr Rowe, osteopaths, massage therapists, physiotherapists and pain management clinics have been noting and treating these restricted movements in the ME/CFS and FM population for decades.
A point of interest – the fascia which surrounds muscles is deeply innervated with sensory nerves and communicates directly with the CNS. My anaesthesiologist explained that FM trigger points are almost always bilateral for this reason – they are spinal cord mediated.
Great point. This is why both sides of the body should be treated at the same time. It is interesting to note that for a diagnosis of FM, there must be tender points in all four quadrants of the body. It is now believed in some parts of the world that tender points are actually trigger points.
They certainly have in FM and I’m sure some have in ME/CFS, but there’s a HUGE difference between practitioners working on these problems and a scientific research paper which actually proves they are there. Rowe in an email to me acknowledged all the work others have done – but it takes a scientific study to get researchers to dig into these problems and why they exist. That hasn’t happened in ME/CFS before. It’s interesting how the muscle studies of all sorts are bringing ME/CFS and FM closer together.
Very interesting about the fascia, Chris! There’s so much to learn in this area.
I believe that because ME/CFS is most often activated by an infection that the studies have tended to focus more on the immune system whereas FM is more endocrine focused but of course both infections and endocrine imbalance can perpetuate trigger points which is just one of the things we both have in common.
I would agree that Dr. Rowe is the first to make such a direct connection between neuromuscular dysfunction and cfs/me but I think he is contributing to a larger body of published evidence that has been researching this relationship for a long time. – perhaps not specific to ME but certainly around the periphery of the issue.
I would not diminish his work – I just wish it was a little more exacting. I would be curious to understand in more detail the “why” of what is happening because at the moment it sounds a bit vague.
For example – TMJ dysfunction is found in a huge percentage of FM’ers and research was published back in June showing how the massester muscle can be sensitized to mimic TMJ by injecting nerve growth factor in to the muscle. The increase in NGF upregulates the expression of peripheral NDMA receptors which leads to an enhanced response of muscle nociceptors to endogenous glutamate.
Would it surprise anyone to know that FM’ers have 3-4 times the normal amount of NGF in the CSF ?? If nerve growth factor can elicit this dysfunction in the masseter muscle what would whole body circulating levels of increases NGF do to the body ??
Any Dr who does research in this field deserves a medal including Dr. Rowe – I just want more from him ! I think this is such an exciting line of research that can actually be translated in to real treatments.
I knew we had huge amounts of Substance P in the CSF but did not know about huge increases of NGF. I haven’t seen that study. It seems logical to me that in order to bring trigger points to the attention of the cerebral cortex that this would be one of the mechanisms involved.
This is very interesting. I find I can identify with the descriptions here.
There are a couple of medicines that really help me. Not to be controversial, but my go-to choice for pain is legal medical marijuana (MMJ). It provides relief for just the symptoms mentioned here.
When I find the right MMJ strain (a combo of high CBD and THC), I can feel my muscles relax and elongate. I actually become taller, to the point where I have a parallax problem until I can get used to seeing the world from a “new angle”. The fog in my head clears. I have tons of energy, because my muscles are not in a constant state of contraction.
Yes, my concentration improves when I smoke pot. It was really weird at first, but now I expect it, crave it.
I know, too, that I am hypovolemic (low blood volume). I wonder if that would cause more tension in the nerves, since the neurons themselves would dry out without a constant, rich bath of blood to provide water to the cells. Dry nerves = “tense” nerves, maybe?
This is a very interesting study, in light of my MMJ experience. Thanks for sharing it with us.
Your MMJ is so interesting. I was walking into a conference and I was doing better and Nancy Klimas walks up to me and says something like “You’re doing better, I can tell – you’re taller. All my patients that do better get taller!”
Leaving aside the amazing fact that Dr. Klimas, whom I see very briefly maybe once or twice a year could actually tell I was taller (what does that say about a doctor’s powers of observation?) – I’ve noticed that myself. When I’m doing better I’m actually more ‘elongated’….
On the other hand when I take things that help my muscle relax sometimes I feel better and then fall apart; it’s as if they’re tense for a reason.
I would disagree with Dr Rowe on inactivity causing or increasing the problem in PWME.
After a serious road traffic accident I began to move around and even went back to work early. The more I moved the more pain I was in and the range of movement became even more restricted.
It was not until I gave up, rested and stopped working, travelling in a car, doing stretching exercise that i slowly began to recover but I am not there yet.
When I first had (ME) as an acute viral illness I was also encouraged not to rest and I was one of the early survivors of a graded exercise program. A terrible effect that had on me.
If we are in “locked down” mode there is going to be a good reason for it.
Time after time, ME and CFS patients have had to prove that it is not inactivity that causes their symptoms – unless doctors understand it is exactly the opposite they are of no use to us.
Rowe does not actually say that and I did a poor job of presenting what he said. He says – according to my understanding – that the infection or some other issue causes the system to be susceptible to kind of freezing in place when activity goes down.
In no way does he prescribe graded exercise for patients who cannot exercise and I was careful to note that so please don’t ascribe that to him.
I recognize that it may seem like a subtle point but he does not believe inactivity is the cause and he’s very clear that simply being more active doesn’t work. – so please don’t ascribe those ideas to him either.
He proposes that something that occurs during the initial illness creates problems with nerve elongation and the system get’s stuck in that mode. How you can tell it get’s stuck in that mode is that he can actually relieve it by using bodywork to remove the stuckness.
I assume with your problem, if Rowe’s hypothesis applies to it, that your ROM and your neuromuscular system got ‘stuck’ very quickly. It may be that he’s wrong as well about that early period.
I don’t think that part of the paper is all that important actually; what’s important to me are his findings of impaired neurodynamics and his abilty to set off symptoms simply moving a limb or pressure on nerves – and also to be able to relieve those constrictions with bodywork.
It’s going to be a complicated situation that involves the nerves, connective tissues and myofascial fibers…as well as inflammation and the central nervous system.
Two other facts about trigger points are that you cannot strengthen trigger pointed muscles as the trigger points intensify with exercise but also trigger points intensify with inactivity as well. The latter is the reason for morning stiffness in fibromyalgia – once you get moving, the muscles loosen up. It is also the reason why you feel stiff after sitting for a long time and have trouble getting up but once you get moving, you straighten up. It depends on many factors how active your trigger points are at any one time and some areas of the body may be worse than others. It’s at least 30 years ago that gentle exercise only was advocated for FM so these facts have been known for a long time.
Thanks Tricia for pointing out the delicate nature of this problem – triggers points worsen with inactivity and worsen with too much activity – that fits me perfectly – and indicates how easily the situation can be misinterpreted.
I really do so much better in the afternoon than in the morning when I feel so stiff.
I don’t see anyone quantifying the kind of exercise that causes them problems. There is a picture of a woman who appears to have been jogging. What I know about my version of ME is that all the muscles seem tense in the sense that they are unable biochemically to complete their contraction/relaxation cycle and have a high rate of resting tone. I know that Magnesium is involved in helping them relax. I know that its like having a flat internal battery which never recharges properly and that I cant do anything which uses energy at faster than a certain rate. Walking is the most I can do, then only in the afternoon or evening. 5 to 20 minutes on a flat soft surface. It takes half a day to get used to being upright before things get working after sleep.
For me its an energy supply problem to the muscle and I cant see how Dr Rowe’s ideas apply to my situation. I have had trigger therapy stuff done on the muscles and it mellows the worst of the knots, but does nothing for the energy supply. Marijuana is out of the question for me. There may be a subgroup for whom his approach is the key, or a key, and I am happy for you. We are a varied group.
I don’t think you would necessarily quantify the kind of exercise that is problematic – I think Rowe would point to the types of movement which exceed your range of motion and which cause pain, fatigue, etc.
I do think Rowe’s theory could help explain your problems (which are similar to mine by the way) because they could explain why muscles are tense and contracted and I assume eating up magnesium like it was candy. Rowe is describing a neuromuscular state that I think would lead to muscles being unable to relax properly.
I think it’s one piece of the puzzle for some people. The energy problem in the muscles is another piece – hopefully they will all fit together at some point and I’m encouraged that they will. A variety of possible muscle problems are now showing up in ME/CFS and FM studies. That’s very encouraging to me.
The picture is definitely not intended to be illustrative of people with ME/CFS 🙂
Trigger points tie up energy as they are highly electrified areas in the muscle fibres which obstruct the blood supply going into and out of the muscle. You can have therapy done on your trigger points and relieve pain but unless they are completely eliminated, they will continue to cause weakness. It is believed that at least in FM ( and I suspect it is the same for ME/CFS) that the disease is a perpetuating factor for trigger points so that you will never be rid of them completely. The dysfunctional HPA axis is the metabolic imbalance we have which perpetuates them.
“Most obvious is a stiff upper and middle thoracic spine with rounded shoulders and a forward head. Patients find that it is difficult to straighten up and tuck the chin. The rib cage is often very tight, and rotational range of motion is markedly limited.”
And what`s about the former athletes, dancers and yoga teachers?
Did we have a stiff upper, rounded shoulders etc before falling ill? No, never ever!
What`s about the ME patients exercising yoga or dancing or those who practiced Pilates BEFORE falling ill?
Rowe will cure them with … what?
That seems to me to be a very shaky hypothesis.
In my opinion ROM may be a RESULT of ME, and not the cause.
A predisposition to something does not mean that it evidences itself physically.
People who have risk factors for autoimmune disorders and then finally get one are healthy before they get sick and it usually takes that risk factor and some other event to cause their system to fail.
If you have a predisposition to neuromuscular problems you could very well be an athlete or yoga teacher or whatever if some event – an infection or whatever – hadn’t manifested that weakness. Most people who have a predisposition to something never get it – because they never bumped into the situation that caused it to manifest itself.
Since Rowe’s neurodynamic hypothesis suggests the problems with nerve elongation, etc. only come with ME/CFS it does not suggest that you should have rounded shoulders, stiff upper bodies before you get ME/CFS.
Think of it like a herpesvirus infection; it’s sitting there latent – not doing anything at all in most people. I assume the situation is similar with Rowe’s hypothesis.
I honestly wish I had not included that paragraph because I’m afraid it’s detracting from the pain point of the study – that for the first time someone has documented negative responses not to exercise, but simply to movement. That a big step forward for me.
To be able to demonstrate that simple movements themselves can provoke problems is an amazing step forward I believe. The fact they’re probably exacerbated by exercise is another step forward. The fact that they can be at least somewhat resolved by particular kinds of bodywork is intriguing as well.
My experience tells me the muscles are involved in a major way. I’m glad to see that experienced validated.
I share your experience that the muscles are involved in a major way.
But I cant recognize why demonstrating that simple movements themselves can provoke problems should be an “amazing step forward”.
Every single day I see the difficulty or impossibility of my most severely affected elderly daughter to hold even a glass in her hand or any other nearly weightless object.
I practised Modern Dance, Ballet, Yoga etc for many many years. So did my younger severely affected daughter. But although we are both very ill we are able to walk upright and to sit upright without rounded shoulders, stiff upper and a forward head. We can keep this position for about half an hour respectively 10 minutes before we have to rest and lay down.
I`m sure every former trained person is able to do so. (Beside the most severely affected patients who are not able to sit up etc)
So I cant understand why rounded shoulders etc should be symptomatic for people with ME.
But I think it is symptomatic for adolescents in general.
I would really like to know more about Rowe`s patient cohort. Which criterias he used in his study? Fukuda? CCC? ICC?
I guess I look at this in a kind of historical way. Researchers have shown that exercise has negative effects, but showing that simply moving couild have negative effects is an enormous step forward in the scientifically. It’s about explaining ME/CFS scientifically on entirely different level. I don’t think it’s amazing that people with ME/CFS can’t do much; but proving that mere movement can produce strong symptoms is amazing – it’s a big step forward scientifically. . That’s what I meant by that.
Anyone who practiced modern dance, ballet and yoga for years is quite an outlier in the area of posture you know:)
I think you’re trying to put your ‘understanding’ on top of science which often doesn’t work. If Rowe and Dr. Lapp are finding increased incidences of rounded shoulders, etc. then it’s there whether you or I understand it or not. It may not be there in everybody but it’s present in general. Given that next thing to do is try and figure what it means and why its there.
From a historical point of view you might be right.
But even though I’m not a scientist, just a lousy lay person who tries to understand some studies I take the liberty to think that scientists often find what they PREFER to find.
And this study appears to be kind of this – in my unprofessional view! :))
Court, I’d just like to take this opportunity to complement you on the amazing job that you do with this site. I’ve been following your work since the earlier days of your previous site. I am constantly impressed with your ability to take in such a variety of technical information and break it down for the rest of us. And somehow you maintain your appetite for this task despite your own personal challenges with the condition(s). But perhaps most impressive of all is your tolerance for the huge variety of opinions that come back at you. Even when your work comes under direct (sometimes even personal) fire, you somehow always maintain a cool and level head. That ability is vital to making any headway through such a contentious set of subjects…making it a truly amazing gift. So, I just want to thank you for all that you do for the CFS, ME, FM, etc. communities, as well as what you have done for me personally, by providing this balanced and unwavering service.
On the subject at hand – I’ve been sick for 14 years and over that time have instituted changes into (what feels like!) every aspect of my being. But about a year ago, I got really interested in the spine, itself, and the surrounding tissues, and since have been concentrating the bulk of my new efforts on my physicality (with yoga, self-applied trigger point massage, Epsom salt baths, therapeutic massage). I’m not all there, but I’ve had more concentrated success in the last year than I had in the previous 13 combined, so I finally feel like I’m narrowing in on the right track (for me). With all these efforts, my back has gradually released its brick-like rigidity, my sleep has much improved, and many other systems have come to operate more normally.
However, as I continue to release the tension in my muscles, I have become more aware of the soreness and weakness of my spine. Almost as though the muscle rigidity were a compensatory method, rather than a primary one.
Just last week I became aware of yet another avenue to explore…namely, the NUCCA chiropractic technique, which is an adjustment of the very first two vertebrae of your spine.
http://www.nucca.org/
When misaligned, those two vertebrae are thought to put pressure directly on your brainstem, disrupting nerve impulses, causing chronic sympathetic nervous system activation (with muscle rigidity) and central sensitization, and impeding blood flow to the brain by pinching the main blood vessels that pass through them. Extreme fatigue is said to be the main symptom of this impaired blood flow. (I’m wondering if that could also be contributing to my POTS, which comes with a very particular sense of “impingement” or “pressure” at the base of my skull.) And then, your whole back/spine can apparently get involved, tensing up and pulling taught in various directions at multiple points, as it tries to compensate for the crooked “top floor” and take pressure off of your brainstem.
This site has good illustrations: http://www.uppercervicalillustrations.com/illustrations.htm#
I am scheduled to get some imaging done this week to see if that particular treatment might be helpful for me. Theoretically, it seems to make sense. In any case, and weather the cause or the result (at this point, I hardly care!), I think the role of the spine itself (and surrounding soft tissues) is one of the more neglected subjects in the discussion of conditions that involve the nervous system. (After all, it is the main conduit!) Perhaps this is mostly due to the ancient battle between traditional medicine and the chiropractic field?
So I’m glad to see that you are gradually taking this general line of thought on, and I look forward to any future posts around this subject. I always learn so much from your articles, as well as all the comments that follow.
Thanks! Martha.
By the way, anyone who is interested in the role that structural issues can play in CFS and ME should check out Dr. Raymond Perrin’s book, The Perrin Technique. His approach, while certainly maintaining some differences from Dr. Rowe’s, is also clearly related to this discussion. He also focuses on the importance of the thoracic spine, its tendency to be flattened, and the importance of bodywork to free up normal (blood and lymph) circulation, and, perhaps most importantly, to regulate nervous system function. Also similar to Dr. Rowe, he believes that issues affecting the spine/nervous system often pre-date the illness onset. He believes that pre-existing structural/postural abnormalities may make certain sections of the spine more susceptible to viral/microbial attack, inflammation, etc. His explanation is on Pg. 29-32.
Sorry Cort…I just saw that I mis-spelled your name in my post! Maybe spellcheck, or maybe just me!
No problem 🙂
Thanks Martha! I think that has to be involved for some people and Rowe has found that working with those areas can be VERY helpful for some people. Good luck with your appointment.
This rings true for me. However, I don’t find the core problem to be the muscles but the fascia. My skin is “frozen”, particularly along the spine and in the neck. There is restriction that affects breathing and most certainly movement. In my case, I do not characterize this as pain. But massage does seem to help get the blood flow better providing some relief.
My exact thoughts and feelings too, Martha Lauren. I also thank you Cort for your perseverance, and I appreciate all the information you bring to us. I have been sick since the age of 20, I am now 58 and have finally found others who share the same lingo and understanding.
I thought this was a facinating Idea that I haven’t heard of before and the fact that he can provoke symptoms by applying pressure is very interesting and could be important. I think more research looking into this is needed. I think his approach to helping people is good.
I think there are some elements of truth in it but like other commenters I don’t see how deconditioning can have any part to play as like my family, people are knocked down in there prime of youth and fitness.
I recognise the body posture item but not the cause. It’s taken over a quarter of a century for myself and family members with ME to be able to straighten up but the cause we have always thought was muscle weakness. Muscles so weak we couldn’t hold our heads up without support, arms so heavy that shoulders slumped downwards and chests sunk inward. We were stiff as boards for the first very acute years of ME but later became unnaturally loose but our other ME symptoms remained unchanged.
A major question this article throws up is; how can structural abnormalities as described in ‘How It Starts’ be a cause when ME can come in epidemics. This is the bigger picture that researchers like Rowe and Perrin never seem to take into account.
Hmm. I wonder if this is one of the reasons why people with Ehlers-Danlos Syndrome are so prone to developing CFS/FM.
I think it’s got to be in there….
“an infection perhaps in combination with prolonged period of inactivity — to freeze into place.”
I also have to take issue with his above comment. Most of us, including myself, did not become ill following a “prolonged period of inactivity”, quite the contrary many of us have been very physically active up to the day of becoming ill. So this is a very misleading characterization of the disease whether or not its his or your words. Since we as patients have been going to such lengths to have an accurate picture of ME portrayed to health care workers, DHHS or new patients, seeing this is troubling and discredits Dr. Rowe’s understanding.
However there are parts of this that do ring true for me, the stiffening of the spine, feels more like “crushing”, increasing when I overdo or have a flare up. (It is helped by isoquercitrin or antihistamines as well as rest) as though the “virus” or infection is in my spine. Its frustrating that most research articles seem to see only some parts of the disease and not all, like the old elephant and blind men story. Hopefully there is someone out there who can put it all together someday.
The word ‘perhaps’ means that long periods of inactivity may have in some cases – contributed to the problem. It doesn’t say that people didn’t work their butts off until they finally collapsed (and then couldn’t move.)
It could also be something that happens in ME/CFS but does not cause it; i.e. you got ME/CFS – you struggled on as long as you could – then you fell apart – and had to stop. When you stopped this neuromuscular problem really settled in – causing you more pain and problems. That makes the most sense for me.
I know I struggled along for quite a while and then I was pretty down for awhile. I don’t know if some sort of system reset occurred during that period. I think it’s a legitimate possibility and I don’t blame myself for it at all. I was in alot of pain. Prolonged inactivity does after all appear to be associated with worsened trigger points. Anything that restricts blood flows (such as prolonged inactivity) could cause problems for the muscles. It’s definitely a complicated subject.
In any case, the most significant part of the blog is the fact that Rowe is documenting movement restrictions in ME/CFS and suggesting a physiological reason for them. I’m surprised that people are choosing to focus on the hypothesis instead of focusing on the potential significance of this finding. He’s offering a physiological reason why movement and exercise is so difficult – your nerves are kind of stuck…
“Its frustrating that most research articles seem to see only some parts of the disease and not all, like the old elephant and blind men story.” – it’s frustrating but true, actually of ALL research studies. ME/CFS is too complex – has too many components – for even a quarter of them to be referenced in a scientific study. For one – the journals won’t allow it. This finding just added another component to the mix; now movement restriction is something that needs to be incorporated into our understanding of ME/CFS.
Even review articles tend to stick to a single subject like the immune system…I hope there are some people out there who are putting it all together. I imagine there are actually….
Actually Cort, you are one of those people who is putting it all together through your site – your contribution to advancing this field has been without a doubt a game changer – and we are all indebted to you.
Actually Cort , there is someone who puts all things together. I came upon the book of Dr Bodo Kuklinski who claims that instability of the cervical spine can lead to several chronic diseases, so
FM is not in our head… it’s just below;
Dr Kuklinski claims that many chronic diseases are due to instability of the
cervical region of the spine .This occurs not only after a trauma of the head : any trauma to the vertebral column will extend to the cervical region.Morphological damage results in disturbed information given by proprioceptors about the position of the head and causes a lack of information or – chaos.Because of the cross-links with the cervical nerves of the cranial nerves numerous symptoms can occur according to their sensory and motor supply areas.Since the vagus and sympaticus are included in the cross-links vegetatieve symptoms will develop with significant consequences for further health. Especially dangerous is a chronic overactivity of the nervus sympaticus. This ultimately affects all organ systems.Irritation of the sympaticus in the cervical region can cause a loss in circulation of the brain up to 80 %. Neuroendocrine dysfunctions are preprogrammed in that way.
Sympaticus stress can also open or damage the blood-brain barrier.
The effects of such irregular nerve irritations on the human organism are multiple.
Enzymes and thus entire metabolic pathways are blocked. Intermediate products reach to pathologic amounts.The organism looks for alternative pathways to break those down and produces thus non-physiological conditions. Proteins are changed, this results in continuous inflammation and later in severe organic damage.
The ischemia in the brain region -as mentioned above -leads to release of oxygen radicals and thus to real brain damage.The clinical consequences are severe: multi-system diseases develop
.
In his book there are many case reports, he describes extensively the diagnostics of the Cervical Spine Instability, he writes about progressive brain and nerve barrier disorders, neurogenic inflammation through activation of C nerve fibers with increased NO synthesis and Histadelia and so on., he also gives many references to the litterature.
He gives examples of chronic deseases induced by CSI: multiple sclerosis,multiple chemical sensitivity,, CVS,FM..
He proposes his CSP-complextherapy;
1)amelioration of sleepquality by use of pillows, good beds
2)osteopatic treatment and strenghtening of skeltal muscles
3)special behavioral therapies to improve the plasticity of the brain
4)nutrition ,
5)micronutrients and supplements
all explained in a scientific way
All you have to do is buy the book on Amazon.com and read it … in German
Or is there someone out there who fluently reads and writes german and can help Cort to translate and make a summary?
Dr. Bodo Kuklinski; Das HWS-trauma.Ursachen, Diagnose und therapie.(2012)
ISBN 978-3-89901-068-8
In German! 🙂 But I am not surprised that instability of the spine is in the mix. I don’t know if Dr. Rowe referred to that but he does find instability of the spine particularly in his EDS patients. I can’t imagine but that problems in the cervical area are not an issue for a subset at least. Rowe has found and treated cervical problems with good success.
It’s so interesting how so many are hovering around this area “.Since the vagus and sympaticus are included in the cross-links vegetatieve symptoms will develop with significant consequences for further health.”.
Thanks for passing it on:)
So many of the points mentioned not only in the article and study, but also the comments, are so true for me. Hypermobility my whole life to a sub-clinical EDS extent, cervical instability (nearly broke my neck in an injury at age 6 and had a 3 level ACDF 3 years ago and looking at another one soon), illness triggering worsening symptoms, vagus nerve infection, and on and on. It’s like a checklist for me! So far I have only been officially diagnosed with FM, but my GP has also suggested CFS as something to look into further. At 44, I mourn the erosion of vitality and independence that accompanies these issues.
Thank you for sharing so articulately this research. The implications of the research of the effects of simple motion, not even entering an exercise level of exertion, are fascinating to me. Looking at my own family, my grandmother, my mother and my sister all had/have similar symptoms (only I have been officially diagnosed), the predisposition rings true as well.
This was my first visit to your blog, but it certainly will not be my last (and I’ll be introducing my doctor to it as well).