



The Pain Brain
Sometimes you’ve got to ask wonder where is it going to stop with fibromyalgia (FM) and the brain? Reductions in the volume of “gray matter” (the neuronal cell bodies and glial cells as opposed to the long nerve fibers) have been found in the insular, anterior cingulate cortices and the amygdala in the brains of FM patients. Other issues have been found in the thalamus, the basal ganglia, the parahippocampal gyrus, the premotor cortex, motor cortex, the somatosensory cortices and the prefrontal cortex in the brain. Other abnormalities have been found in the connections between various parts of the brain.
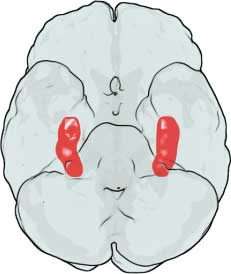
This Florida group was looking to add another brain region to the list: the hippocampus, a part of the limbic system that plays an important role in short-term memory (remember that?), long-term memory (generally thought to be intact) and “spatial navigation”. The hippocampus isn’t directly involved in the production of pain but a breakdown in hippocampal functioning could lead to a “feed-forward” process that ends up disrupting the limbic system and the pain networks in the brain.
Hippocampal problems could then conceivably result in discomfort, severe pain, anxiety and perhaps even the mysterious and disturbing allodynia that some people with FM experience.
Some evidence of hippocampal atrophy exists in FM but this was the first time depression was controlled for in a study. Because hippocampal atrophy is also present in depression and because depression is fairly common in fibromyalgia, the atrophy could have been due to depression.
In this nice-sized (for a brain imaging study) 22 healthy controls and 40 fibromyalgia patients got into an MRI machine and had their hippocampal volumes analyzed. Rates of depression, pain disability, sleep efficiency were assessed as well.
Results
You can another brain abnormality to the growing list. The hippocampus is made up of two hemispheres and hippocampal grey matter volumes were significantly reduced in both of them (p<.o8, p<.02). Because the atrophy was independent of depression, it was coming from or contributing to fibromyalgia not depression.
Earlier studies buttressed the finding of reduced hippocampal volume. Remarkably elevated NAA/Cho ratio’s in a 2008 study suggested that neuron damage had indeed occurred in the hippocampus. A meta-analysis of magnetic resonance spectroscopy findings concluded significant hippocampal NAA reductions are present in FM. A recent study linked cognitive problems in fibromyalgia with hippocampal dysfunction.
The researchers inability to find correlations between levels of pain and sleep efficiency, however, suggested that the smaller hippocampi in the FM patients was not significantly contributing to their symptoms. (Despite the fact that the hippocampus plays a major role in cognition including short-term memory and cognition, they did not examine cognition. )
The fact that hippocampal atrophy was not associated with increased pain, symptom severity or decreased sleep efficiency suggested the atrophy found may have been secondary; i.e. it was the result of having FM rather than being the cause of it. More extensive symptom tests, might, however have found an association and that could change.
Whatever the symptom tests showed, the hippocampus is a major organ in the brain – not exactly something you want to have atrophy a bit. When the authors asked what could be causing the reduced hippocampal grey matter one of the usual suspects in FM showed up: glutamate/GABA imbalance or nervous system burnout.
Glutamate/GABA and Nervous System Burnout
Nervous system “burnout” occurs when the excitatory part of the nervous system triggers so much activity that nervous system cells get killed off. Powered by glutamate and inhibited by GABA, several researchers have proposed that nervous system over excitation could be causing or contributing to the hypersensitive pain state found in FM.
There’s some evidence for this. Increased glutamate levels or ratio’s appear to be widespread in FM having been found in the insula, thalamus and posterior gyrus and have been linked to increased pain in several studies. Increased glutamate ratio’s have also been found in restless leg syndrome, another disorder apparently characterized by “over-excitation”.
Drugs that tamp down glutamate neurotransmission such as Lyrica, sodium oxybate and ketamine can be helpful for some patients. A recent study suggested transcranial direct stimulation (tDS) reduces pain in FM by reducing brain glutamate and increasing brain GABA levels.
Dietary glutamate (MSG), intriguingly, was associated with increased symptom severity in FM in one study. A glutamate-free diet which includes avoid MSG, aspartame, soy, seaweed, yeast and other foods is a key part of Dr. Yasko’s protocol. On more anecdotal note, Marco – who has written several Health Rising blogs on glutamate/GABA – recently received a comment from someone for whom a low FODMAPS/glutamate diet helped. (See Meg’s comment).
- Glutamate – One More Piece in the Chronic Fatigue Syndrome (ME/CFS) Puzzle? The Neuroinflammatory Series Pt. II
- A Neuroinflammatory View of Chronic Fatigue Syndrome
- Cooling the Flames: Possible Approaches to Reducing Neuroinflammation in Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia
Prolonged Stress
Secondary or Primary Factor?
Because prolonged stress has been associated with hippocampal atrophy, the atrophy could simply result from the prolonged stress of having a painful illness. An a acute infection or otherwise stressful event could also kick off an atrophy in the hippocampus that helps to trigger FM. It’s also possible that people with FM are predisposed to having small hippocampi. A twin study found having a smaller hippocampus predisposed twins to come down with post-traumatic stress disorder after being exposed to a severe stressor.
The association between reduced hippocampus volume and prolonged stress suggests that interventions that impact the stress response and/or glutamate neurotransmission could be helpful. These could include behavioral modifications (mindfulness/meditation/yoga/CBT) and/or glutamate reducing drugs – some of which have been found useful in FM. A reduced glutamate diet is another, mostly untried, option.
The authors called the “neuroplasticity” of the hippocampus; e.g. it’s ability to respond to treatment an “unknown and exciting area”.
The hippocampus is now one of several brain regions implicated in fibromyalgia. How it will shake out in the end is unclear but it’s clear that the brain is heavily involved in producing the pain in FM. Whether that brain dysregulation is being driven by problems with the nerves or the immune system or pathogens or other factors in the body is a big question.







Thanks as usual for the great articles. I’ve been watching development of this small companies drug trial for some time. I didn’t think of it helping me but you never know.
It may be able to help regrow the hippocampus.
NSI-189 is an experimental drug being studied by Neuralstem, Inc.[1] Research into NSI-189 has been funded by the Defense Advanced Research Projects Agency (DARPA) and the National Institutes of Health (NIH) for the treatment of major depressive disorder.[2]
Contents [hide]
1 Pharmacology
2 Clinical trials
3 See also
4 References
Pharmacology[edit]
NSI-189 has been shown to increase the hippocampal volume of adult mice by 20%,[3][verification needed][medical citation needed] and has been shown to stimulate neurogenesis of human hippocampal stem cells in vitro and in vivo. The hippocampus is responsible for the consolidation of information from short-term memory to long-term memory, along with spatial navigation, and is also involved in regulation of mood.[2][4][5]
Clinical trials[edit]
NSI-189 successfully completed a phase 1 clinical trial in 2011 where it was administered to 41 healthy volunteers.[6]
A phase 1b clinical trial for treating major depressive disorder in 24 patients started in 2012 and completed in July 2014.[7][8] The study suggests that there were improvements in the patients’ condition when the doses were 40/80 mg per day, but no significant improvements were seen for a higher dosage of 120 mg/day.
Neuralstem intends to pursue further clinical trials for a variety of neurological conditions, including major depressive disorder, traumatic brain injury, Alzheimer’s disease, post-traumatic stress disorder,[2] stroke, and natural cognitive and memory decline in aging.[3]
Thanks Tim
Interesting – thanks Tim 🙂
Interesting Cort. If anyone is interested I. Jon Russell is doing a module on Fibromyalgia this week on Coursera’s “Preventing Chronic Pain” course. I haven’t listened yet but I did just listen to an NPR program “On Point” talking about Chronic Fatigue and the recent IOM report. The chairman of that, Ellen Clayton was on along with Jennifer Brea ( she got quite passionate) Dr. Inlander and another doc from the Cleveland clinic. The program is from today and about 30 minutes.
Thanks Betsy. I went and had a look, and immediately had to lambast “Brian” politely. He was expressing the usual attitude.
Thanks for the info.
I’m so thankful you are out there, Cort, to digest and share all this budding information. Reading your posts is often like looking in the mirror.
One partial discrepancy: While I don’t take Lyrica, Duloxetine has helped my pain measurably. But my neurologist (who is skilled, informed, and interested) predicted that the Duloxetine would NOT help my restless legs — and, sure enough, the restless legs are now worse than ever. (At least it’s better than all-over burning pain.)
I also relate to the sense that prolonged stress eventually broke something in the nervous system, but of course it’s hard to tell what’s cause and what’s effect.
Interesting. Did he say why he thought that would happen?
No, just that the RLS would have to be addressed separately. He’s a one-step-at-a-time guy. He also predicted the symptoms of generalized neuropathy (numbness, weakness, cramping, etc) would not improve either, and that’s also been the case (same with chronic fatigue). But, for me, the thing that rendered me most incapacitated was when all of the above were combined with the sense that molten lava was flowing under my skin throughout the body. That’s pretty much the only symptom that duloxetine alleviated — but it’s a biggie.
There were studies done years ago that showed dysfunctional lay down of emotional long- term memories in the hippocampus in fibromyalgia. This is the reason why I always took a lot of photographs during my lifetime (my father did the same). We needed the visual reminder to help us remember, which we did especially if we referred to them often. This is how I ended up remembering more things than the rest of the family, despite me being the only one with fibromyalgia. I put this dysfunction down to the emotional stress, with resulting over excitation of the nervous system, having a severe impact on the hippocampus and the resulting lay down of these memories.
I suffered from increasing chronic stress that was reaching an unendurable maximum during the approximate period 1995 – 2000; I was basically just going through the motions of life during this period.
Now I periodically find that I have no memory at all for events during that time; friends and family might be talking about things, and I am a complete blank. Including a trip overseas and the places we went and saw and the people we met. Even meeting the same people again since, I do not remember them.
I recently accompanied a visiting friend on a tour of our nation’s Parliament Buildings, and there was a photo gallery devoted to a major rebuild project that took place in the late 1990’s. The buildings and grounds were covered in scaffolding and sheds and ditches with shelters erected over them, for a couple of years – and a major fire occurred during the work, which left the roof burned out and set the work back months.
I would have been passing this almost daily on my commute to the highly stressful job I had, and I have NO recollection of it at all….!
I have recovered a lot of my capacity to remember since then, but I believe that I have a totally different capacity for memory for different THINGS – I have become permanently terrible with people’s names and putting names to faces, yet I have good memory for academic matters that I make a focus of study.
The more I learn about what has happened to me, the more angry I am at the moral monsters who claimed to be my “friends” in advising me that it was “all in my mind”, I needed to pull myself together, etc etc. Part of closure and getting on with life, is letting “friends” like this go. If nothing you can say will make them back down about what they have done to you, then they settle their own case about what they actually are, and they might as well belong to the KKK or ISIS, for all the regard I have for their humanity now. You can feel back in charge of your life again if you bust up totally with people like these, tell them exactly what they are and let them go away on their high horse “because YOU wouldn’t listen to THEM”…..
Any health professional who has been like this to you, tell them they are in breach of their Hippocratic Oath and should be deregistered. Tell them they are incompetent and as arrogant as only an incompetent person who covers their incompetence with bullying, can be.
Phil,
Face recognition happens in a specific small part of the human brain. Something called “face blindness” is not as uncommon as it might seem — although like everything else, it occurs as a spectrum problem.
The longer more technical name is prosopagnosia. There is a page with a test for it, here:
http://www.faceblind.org/facetests/
I can still recognize faces of famous people, and faces of people who I’ve known for quite a while. But I have trouble with new people — it’s that thing about laying down new memories, I guess.
Being faceblind is famous, or notorious, as being frequently a part of autism.
People who have been seriously faceblind — not like me, where if I work on it, I can manage — learn to recognize people by their haircut, or the clothes they commonly wear. Or whatever.
Further about faceblindness.
I looked up the anatomical area that I was trying to remember — and Wikipedia says “. Brain imaging studies typically show a great deal of activity in an area of the temporal lobe known as the fusiform gyrus . . . ”
It’s a more complicated process that just that one little area. But if that area becomes dysfunctional somehow, that’s enough to interfere with the ability to recognize a face. Or faces.
Hi Cort,
Stress and infection have brought me right down. I had infection in my upper gum (undiagnosed and not treated by my then dentist) from March to December last year. I am alone and quite socially isolated, many days I was so ill I would live on biscuits as that was all I could manage. I was in solitude for most of the time (no friends or family) with only the carer visiting Mon to Fri to shower me.
The pain was more than unbearable as was the hunger at times and I ended up malnourished (supplements was my main form of nutrition but they don’t take the place of real food). Medical care here is abominable to say the least. I actually thought I was going to die.
Before I got the infection I wasn’t doing too bad. I used Lumosity Brain training exercises and that really kept my brain going well. Now after all that has happened my body has become weakened and tired, as has my immune system. I now have Ross River Virus just to top things off.
However, I have today started doing Lumosity brain training again and am pleased to say my brain looks OK, just tires extremely fast. So what I am trying to say is that even though our brains (I don’t type brian for brain anymore:)) are affected, they can be helped with brain training exercises. Initially, I was amazed at how well and how fast they work and now I will continue to do them for as long as I am able. Sorry this is so long.
Jazel
That’s great to hear Jazel – thanks for sharing that. Congratulations….
Luminosity is great!
If you cannot afford a subscription, regular computer games will work, I increased my capacity for short memory with matching games, like solitare, mahjong, candy crush, etc. They were hard at first but I believe it retrains the brain.
I start my mornings now with a sudoku game that tells me how many mistakes I made, so I can tell how hard I will have to concentrate and double check myself that day!
I try to search out games with feedback, undo capacity, scoring in different areas etc. If it is too hard I start with one with lots of ‘hints’ available, or a childs version, and just follow along until it starts to make sense.
Next up, hidden object for observation skills
Sorry, really getting off topic here!
Great stuff – thanks. Hey, anything that helps 🙂
Re Luminosity. I love the brain games. Fun but challenging. I was almost consistently gaining points until I went on a holiday. Had a nice relaxing time in the sun but even relaxing holidays, for me, can take a month to recover from the exhaustion. Why go you may say, well it’s cold here in Canada in the winter and I’ll do most anything to be warm and in the sunshine.
Back to luminosity. Since I’ve returned home my points on each game has drastically gone down. I’ve had years and years of high stress, until the last year and half but ME/SEID settled in 15 years ago and won’t let go.
My STML is certainly embarrassing at times, like forgetting my best friend’s name when introducing her to someone!
Hi Cort,
Only the first page of this article is set up to be printed; can you fix it? Thanks!!
Oh man…how did that happen – I don’t know why that’s happening. I did just make it so that the images are not included in the print job – perhaps that will help?
Hi again Cort,
No, whatever you did made it worse! Only the first paragraph now comes up to print.
Mary
Lordy…..
How about downloading it as a Pdf (next to the print button) and then printing it?
Hi again Cort,
No, using the PDF button brings up the same, short, one paragraph of the article that the print button does. Hey! Don’t stress over this. I have not tried to print any other articles after this one, so I don’t know if this problem is only with this article, or others.
Thanks for your efforts,
Mary
I really appreciate these articles. This one really spoke to what has been going on with me. I have been trying to think of some ways, just this week, to help with memory and concentration loss. I think I’m going to audit a piano class at a nearby college. My short term memory is terrible, but I seem to be able to build on things in my long term memory, and I have a lot of musical training. Beginning music lessons might be a good way for people to build some new connections.
I just want to add my voice to the chorus of ‘thank you Cort’ – and all those who know enough and take the time to comment.
Since I have been reading your ‘blog’ I feel I have hope. I could probably find the info you write about elsewhere if I had the energy to search but as I don’t, finding it all in one place is wonderful.
I’m in the UK and having a GP (family doctor) whose attitude is extremely negative e.g. ‘there is no point in referring you to anybody because there is nothing they can do about fibro and CFS.’ is the attitude. What I hear is that there is no hope for me and my fellow sufferers. To live with no hope is not to live – one way or another – for me.
Thank you, thank you, thank you!
Christine
I feel the exact same way Christine!!
Great post! Thanks court. I started hoping after reading your article.
Hi….there was a paper published over 12 years ago that spoke to this exact thing….problem was, it was written by a fellow in psychopharmacology so the big guys in research didn’t pay much attention. You can look it up on Pubmed but I pretty sure that the group in Florida cited the work pretty heavily in their finished paper and I believe the NIH awarded the researchers an award…unfortunately, big Pharma had no chance of making money on this news…..so that was that.
Thank you all for this information on the brain pain. I was diagnosed with FM after struggling for over 4 years with pain even while doing therapy. Now I am in Grad school and is struggling as my brain feels like there is a heavy pressure there. I am unable to be critical and analytical and find simple information that is normally easy, difficult to understand. Additionally, I can hardly remember anything at all as my short-term memory is at its worst ever. The brain struggle causes me to become depressed.
I was wondering what could be done about it but I now understand that I can retrain the brain. I will share this information with my therapist so that we can work on a plan.
Again thanks.
Nadine D
Fascinating! My mom was recently diagnosed with fibromyalgia so I am trying to help by doing all the research I can.
She has reported some success when taking magnesium malate, but based on this I will let her know about the glutamate-free diet.
Thank you!
Fibromyalgia has central nervous system origins
Date:May 17, 2015 Source:American Pain Society
http://www.sciencedaily.com/releases/2015/05/150517071813.htm
Hyperbaric hope for fibromyalgia sufferers
http://www.sciencedaily.com/releases/2015/06/150602153528.htm