



Several recent blogs have suggested mitochondrial problems may exist in chronic fatigue syndrome and fibromyalgia – but do they look like mitochondrial disorders? That’s the question part I of this blog is tackling.
Chronic fatigue syndrome and fibromyalgia can cause so many symptoms that they can lead themselves to a variety of diagnoses. That’s a problem, but it turns out that the sheer number of symptoms found in these disorders may be a clue. Not many diseases can produce such a rich broth of symptoms.
Those diseases that do, tend to have systemic (body-wide) impacts or effect the brain. They include such disorders as autoimmune diseases, post-viral syndromes, neurodegenerative disorders, the so-called functional syndromes (FM, ME/CFS, etc.) and some mood disorders.
What about mitochondrial disorders? Hundreds of mitochondrial diseases exist, but many do have systemic effects. In fact, the United Mitochondrial Foundation (UMF) recommends that doctors think “mitochondrial disease” when three or more organ systems are affected. The Foundation also lists “CFS-like illnesses’ as possible indicators of a mitochondrial disease.
The UMF’s 40-plus mitochondrial disease symptom list is a long one and ranges from blindness to migraines to fainting. Because so many mitochondrial diseases exist it’s impossible to strictly compare the symptoms of “mitochondrial disease” to those found in ME/CFS and FM. We can, however, look at general symptom patterns – and that’s what this blog will do.
Let’s look at how the symptoms in mitochondrial diseases and ME/CFS and FM compare.
Symptoms
Exercise Intolerance
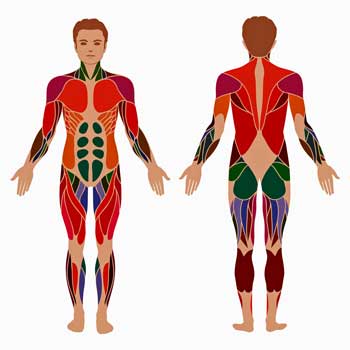
It’s perhaps not surprising that people with mitochondrial diseases often exhibit exercise intolerance. If the mitochondria – the energy producers in our cells – aren’t working well then our muscle cells are not going to be able to produce the energy we need to exercise.
People with mitochondrial disorders tend to be able to exercise only in a limited fashion. Fatigue is not necessarily always present but it and weakness often comes quickly once activity is initiated and rest is needed to build up energy levels again. After rest no clinical evidence of weakness is often present.
Weakness – the inability to generate force – is an important symptom. Weakness is different from fatigue. Fatigue is a sensation associated with pain, weariness, etc. One can feel fatigued without being weak.
I’m unclear on the status of weakness vs fatigue in ME/CFS. Most studies suggest weakness is not present but the two day exercise studies suggest that the inability to generate force after exercise; i.e. weakness is a major issue.
According to MitoAction exercise and physical activity was not recommended for mitochondrial disorders in the past because of concerns about cellular muscle damage. Now, exercise in small amounts is recommended into order to avoid deconditioning – which reduces mitochondrial density – and to increase mitochondrial and blood vessel density, enzymatic activity and improve quality of life.
Post Exertional Malaise (PEM) or Relapse (PER)
Post exertional malaise or relapse is a major problem in ME/CFS and FM and it occurs in people with mitochondrial diseases. Whether they experience the same kind of PEM that people with ME/CFS or FM experience however, is unclear. (It’s not at all suggested that people with ME/CFS and FM all experience the same type of PEM.)
The “global fatigue” people with mitochondrial disorders can experience after exertion, which causes slowed thinking, confusion (and in some “an unmasking of behaviors normally under control”) sounds very much like ME/CFS and FM.
People with mitochondrial diseases are, by definition, low in energy – at least in some parts of their bodies
The muscle symptoms after exercise (pain, cramping and/or muscle spasms with or without tenderness and/or feelings of heaviness (cement legs) particularly in the muscles used) bear some similarities.
The quick appearance of muscle pain in Mark Vink’s legs after very mild exercise appears to be highly suggestive of mitochondrial problems. My symptoms after too much walking, on the other hand, tend to be less specific and more global. They include fatigue and burning pain sensations across my body but my legs are not particularly affected.
The small muscles can be affected in mitochondrial disorders as well. Too much writing, for instance can cause, penmanship, for instance, to suffer. Tachycardia – rapid heartbeats – can occur. Blurred vision can be caused by eye muscle fatigue. (There’s no mention of the “floaters” often seen in ME/CFS).
Other Symptoms
Signs of significant autonomic dysfunction appear to be often found in both mitochondrial diseases and ME/CFS/FM. They include rapid or slowed heartbeats, problems standing, heat or cold intolerance, unusual sweating, spontaneous pallor or flushing or mottling and gut and bladder problems can occur. Whether these symptoms worsen after exercise was not clear.
Sleep problems including sleep apnea, unrefreshing sleep and daytime fatigue are common in mitochondrial disorders and ME/CFS and FM. Not surprisingly, so is emotional distress.
Breathing problems can be found in both. Dr. Natelson has found that hypoventilation – a short, rapid breathing pattern – is fairly common in adult ME/CFS patients. Breathing problems tend to show up first in mitochondrial disorders during periods of increased oxidative stress (infections, following exercise or emotional distress) but can become more permanent over time.
They appear to be caused by the same problem that’s been suggested by Staci Stevens for ME/CFS – fatigued respiratory muscles in the chest and diaphragm. Staci Stevens has noted that the respiratory muscles are among the most active in the body.
The tendency for infections to cause long term fatigue that remains after the infection has been resolved, occurs in mitochondrial diseases and, is, of course, reminiscent of ME/CFS. It suggests that an autoimmune process affecting the mitochondria could be triggered by an infection, in ME/CFS or FM.
It’s clear then that major symptoms found in ME/CFS – fatigue, post-exertional malaise, sleep and cognitive issues – are also found in mitochondrial disorders. While muscle spasms and pain can occur in mitochondrial disorders they don’t appear – at least from this overview – to achieve the kind of prominence found in fibromyalgia.
Mitochondrial Diseases or Mitochondrial Dysfunction?
Both symptoms and several study findings suggest mitochondrial problems may exist in ME/CFS and FM. If they do it’s not clear if a “mitochondrial disease” is present; i.e., if the mitochondria themselves are defective or if mitochondrial function is being inhibited due to other factors such as insufficient oxygen and blood flows.
Mitochondrial diseases that are genetic in origin usually show up early in life but mitochondrial diseases can also be triggered later in life by infections, autoimmune processes, drugs or “other environmental factors”. Epigenetic processes that affect the expression of mitochondrial genes over time, may play a role as well.
One process that could be occurring in ME/CFS involves the blood vessels. Dr’s Fluge and Mella suggest that autoimmune processes may be reducing blood flows and possibly impairing mitochondrial functioning.
A disease also does not have to be considered a “mitochondrial disease”, for the mitochondria to be affected. The United Mitochondrial Disease Foundation states that evidence of mitochondrial dysfunction can be found in many diseases including Alzheimer’s and Parkinson’s diseases, amyotrophic lateral sclerosis (ALS), multiple sclerosis, Sjogren’s Syndrome, lupus, rheumatoid arthritis, mental retardation, deafness and blindness, diabetes, obesity, cardiovascular disease and stroke.
The CoQ10 Question in Fibromyalgia and ME/CFS
CoQ10 plays a critical role in the generation of aerobic energy (ATP) – the source of about 95% of the energy in our bodies. Two-day exercise studies suggest, however, that aerobic energy production has taken a significant hit in ME/CFS. Several ME/CFS doctors use exercise tests to define safe but usually very low aerobic energy levels for their patients. The collapse of the aerobic energy production system suggests, of course, that the mitochondria are involved.
Several studies suggest low CoQ10 levels could be contributing to the symptoms found in fibromyalgia as well. A Spanish trial resulted in significant reductions in pain, fatigue and morning tiredness as well as reduced inflammation and increased mitochondrial activity. Similar findings were reported in a Japanese trial of adolescents with FM and CoQ10 reduced pain and headache in FM patients in a third. Finally a small study found evidence of both mitochondrial dysfunction and CoQ10 depletion in the tissues of FM patients.
The Mendus/Health Rising Placebo-controlled MitoQ Chronic Fatigue Syndrome and Fibromyalgia Trial
Background
Saying that MitoQ is a mitochondrial supplement is not really doing it justice. MitoQ is a mitochondria supplement that’s been featured in 180 research papers i.e. it’s a serious mitochondrial supplement. MitoQ says their product – patented by New Zealand researchers to deliver CoQ10 to the mitochondria at very high levels – is 847 times more effective than other CoQ10 formulations. Read more about the difference between ordinary CoQ10 and MitoQ here.
When MitoQ approached me some time ago about offering our ME/CFS/FM members their product in exchange for some feedback I immediately thought of MENDUS. MENDUS is a website created by a researcher and ME/CFS patient, Joshua Grant, that allows health communities to create their own online clinical trials.
Josh was interested in using MENDUS to assess the results of a MitoQ trial but we both thought MitoQ would be leery of such a public assessment of their product’s effectiveness.
We were wrong. MitoQ was fine with a public MENDUS trial. When Joshua suggested that a placebo component be introduced, MitoQ agreed to that as well.
So now we have a twelve week, 100 person (50 ME/CFS and 50 FM), double-blind, placebo-controlled MitoQ trial underway on MENDUS.
The Trial
The first fifty people with each disease to sign up for the trial and complete their registration with MENDUS will get two bottles of MitoQ; a placebo and the MitoQ. They will take each bottle for six weeks and complete a set of measurements 5 times over that period including a variety of symptoms and cognitive tests on MENDUS.
Others who want to participate in the trial can purchase the supplement at a reduced price on MENDUS. Because the more people entered into the trial the better we hope some people who can’t make it into the free trial will take advantage of this offer. (The purchasers of MitoQ will not receive a placebo bottle).
Some things to note
If you want to be in the free trial you should
- First, send an email to MitoQ at this address (study@mitoq.com) with the subject heading “Study Enrollment CFS” or “Study Enrollment FM” depending on which condition you have. (If you have both pick the predominant one). MitoQ will send you an email with information about the study and how to proceed, including the links to register with MENDUS and to the study.
- If you haven’t registered with MENDUS, immediately register for MENDUS. Then send your name, your MENDUS ID and your shipping address to MitoQ in the reply email to them.
- MitoQ will send two bottles to you; the MitoQ bottle and the placebo bottle. These will be marked Bottle 1 and Bottle 2. You should begin with Bottle 1. But, you will not know which is MitoQ and which is placebo.
- Be sure to read the Project Information Form, the Detailed Study Instructions and sign the Consent Form on the MENDUS website, otherwise you will not be able to participate.
- If the 100 places have already been filled you’ll be informed of that when you initially contact MitoQ. In their reply they’ll include a 1-time use 50% discount code you can use to purchase the product and register in the trial.
- Anyone anywhere in the world can be in the trial.
- Please note that because MitoQ is putting more pills than usual into the bottles the bottles will not be sealed as they usually are. Instead MitoQ is putting tamper-proof tops on the bottles.
- If you’re currently taking CoQ10 you agree to stop taking it for a week before you start the MitoQ trial.
- Please note that the low doses of MitoQ (20 mgs/day) in the study translate into higher doses of other kinds of CoQ10.
- Questions about MitoQ itself should be directed to MitoQ (customerservice@mitoq.com). Questions about the study can be sent to Joshua (Mendus.org@gmail.com).











Sent out a request to be included in the CFS trial – I’d love to try CoQ10, and see if it does anything for me.
Thanks, Cort.
Alicia
Good luck! Be sure that you’re signed up with Mendus.
Ehlers Danlos Syndrome ‘undiagnosed’ type(s) Genetic Born mutations Protein Collagen deficiencies…
Interesting article Cort.
I have had ME/CFS for 19 years. Within the past few months I have noticed breathing problems. I get winded doing just about anything. I hope the CoQ10 might be able to help with that and other symptoms.
I’ve sent my info in for the trial.
Lynn
I’m sure the breathing problems can be caused by quite a few things but the possible mitochondrial connection is intriguing…Good luck with the MitoQ
We need to be careful not to confuse the MitoQ trial with our CoEnzyme Q10 study. We have both now. This article is introducing the MitoQ, which is of course amped up Q10.
mendus.org/q10-study-home.html
mendus.org/mitoq-study-home.html
Joshua
Thank you Cort!
Your friend from Sweden
Mats
Thanks Mats. Good luck!
I am happy that my wife is now included in the study
I signed up for the MitoQ study. Thanks for the information.
We have had people send their information into MitoQ, sign up on Mendus for the study, get the OK from MitoQ and then promptly unregister themselves from Mendus….
That’s not going to work. We request that everyone honor the terms of their agreement. The agreement is that MitoQ will give you a free product if you participate in the Mendus study, take the supplement as promised and provide your results every week as promised.
Everyone in the study has a responsibility to the rest of the community to do the study as requested. Why? Because the study will get done and some people will use it as a basis to decide whether or not to try this treatment. They deserve that we do our best.
This is also the first study of its type and if it’s successful it could lay the groundwork for more patient produced studies. If compliance is poor, though, it will demonstrate that the patient community can’t be trusted to do this on its own. For sure this kind of study is harder to comply with because there’s no doctor or researcher to see – we’re doing this on our own. Let’s make it a success..
It was only a few people but they popped up right away and I thought I would mention it.
that’s really disappointing. they will actually miss out on heaps of information as a result of that (somewhat selfish) move. they won’t know which period of time they had placebo for and they won’t have a record of exactly how they were going that will be directly comparible to the others in the study. so they will be left guessing if any benefit was their own imagination or is shared by others during the non placebo part of their regime.
Im happy that Im part of the additional group that dont have blinding applied but can trial mitoQ at a discount. I have never felt the effects of CoQ10 so periodically drop it due to expense but then hear testimonials and go back on it . this could well tell me if CoQ10 derivatives will help by giving me a MUCH more effective dose.
Agreed Tim. To be fair though, our turnout thus far has been pretty good and I’m impressed with how serious folks are taking it.
One thing I’d like to add. The group that you’re in is incredibly important so I hope people don’t feel like joining that way is a waste. With your group we’re going to be able to make claims about how dosage influences potential effects as well as how long you take it. I’ll be increasing the number of measurement time points for Group 3 to allow you to keep measuring for 3 months instead of 6 weeks as Group 1 and 2 do. They have the placebo so are going 3 months as well.
Joshua
Thank you, Cort, for the reminder that we have to help make science happen!!!
Thanks Marilee.
This is the kind of study. I think, where one might give oneself the freedom to not be as rigorous as they might be otherwise. I think we have to guard against that.
This study is not an NIH approved study, the patients are not age, sex, weight and etc. matched. We’re relying that everyone who says they do has ME/CFS/FM etc. This type of study, as I see it, is probably more difficult to achieve results than others in which many of the patients are picked by doctors who think they will do well in the trial. Accuracy in reporting and as full compliance as possible is important..
Can we as a community do this well? I’ll be the first to admit that my supplement “regimen” is pretty darn sloppy. I’m going to have to up the ante a little bit and make sure I do this right..
Well, I can say that so far on Mendus we’ve had truly dedicated people who have even managed to design their own placebos… and trick themselves!
A relatively rigorous study is definitely possible. I can ‘fix’ a lot of the variability statistically, as long as I have the information and we have an extensive questionnaire for everyone to fill out which will help.
But it comes down to making an honest effort. I second Cort, you owe it to the community and yourself, to only participate if you’re going to hold up your end of the arrangement. Not sure if you all realize the cost and reputation of MitoQ.
This is a really great opportunity!
Joshua
Now that’s a good placebo 🙂
But check how who we’re dealing with here. Josh is the real deal; he’s a researcher with ME/CFS – he can handle the variability, he can make adjustments. His expertise is not to be missed….It’s a real opportunity and I hope Mendus – be sure to check out the other studies – grows and grows.
Joshua,
You are doing a wonderful job.
According to me a placebo and actual drug should be given to the same person at different times not to different persons at the same time.
This is the best way to understand if the medicine or drug or protocol is really working on the individual or not.
If you can design a study like this, it will be great.
Please see how much the modern medicine is missing or misleading itself under the constraints of finance.
Have fun,
Hari
“According to me a placebo and actual drug should be given to the same person at different times not to different persons at the same time.
This is the best way to understand if the medicine or drug or protocol is really working on the individual or not.”
After I got a reply asking for more detail to be part of FMS group, I saw you already designed the study like this.
Kudos to you Joshua.
Have fun,
Hari
I’m shocked people have done that! So much human collaboration and goodwill and preparation… and to mess them around just so you can get a free bottle of something?
Anyway Cort I was moved to write by your last sentence about your ‘regimen’. I am exactly the same. With medicine I seem to be able to remember to take things at the right time and right amount (mostly), but can’t seem to do the same with supplements. It made me think – why try so hard and spend so much money on them and then be so sloppy and all over the place about taking them? I am resolved as of tomorrow to write down everything I am currently taking and at what time I should take them and record the results.
Also to say that I read about MitoQ last year – esp the face cream which got rave reviews on anti-aging and skin-care sites. I took both for about four months and the results were pretty positive – the only problem was the price point. Way out of reach for something more permanent. Hopefully if the study yields good results it might lead to a way of reducing it? No idea how that would work, but fingers crossed. Very exciting stuff.
I’m glad I’m not alone 🙂
We had a few glitches in the beginning but all is good now.
Cort,
On the approach of clinical trails by the professional community, I completely disagree. Please see my other post for depth analysis.
http://www.cortjohnson.org/forums/posts/7705/
The essence of the post is: So called professionals, scientific and medical community conduct study in a controlled manner, by excluding vast majority of the groups. If the results are satisfactory then they prescribe the medicine to everyone, including those who are excluded in the study.
I am not sure, why, and how any one would accept this kind of social behavior. Personally, I believe it is immoral and injustice to the humanity.
Let me take an example: A person who do not have digestive problem, is included in the study. The result is good. Is it acceptable to give the same drug to the person who has digestive issue also?
**** ***
On the contrary, I completely acknowledge MendUs approach – to include every sub group in the study and see the result.
I would appreciate if the study group is bigger, say about 500 and purposely include as many sub groups as possible, and see the result for each sub group and compare with other sub groups. This is the holistic approach to understand holistic outcome.
I see, this approach will create new trend in the future of clinical trains.
I congratulate Joshua Grant, and acknowledge both of you for making it big.
In summary, this is how any clinical trail should be. Sometime in the future NIH and any other related authority will endorse your activity.
Have fun,
Hari
I would love 500 person studies and I agree they would tell us soooo much! They seem crucial to me to really understanding what is going on in these disorders.
🙂 Thanks for all the kind words Hari.
If the NIH ever endorses us for this study I’ll buy you a… a… bottle of MitoQ!
It is possible that we could get to 500 people but only 100 will do both placebo and active MitoQ. The others could join by buying MitoQ at 1/2 price. This will still be very informative and allow us to assess dosage effects as well.
Take care,
Joshua
I’ve just requested to be part of this study, I hope I’m not too late.
I hope so Annie. The folks at MitoQ will probably get back to you tomorrow.
Great article. I have been taking Mito Q for a while now, and it has totally given me my life back.
I was not able to walk far, but since taking this I have had a lot more energy. I wake up with a clearer head, and have more energy than I have had for years.
I totally recommend this supplement.
That’s good news. Thanks for passing that on Anita 🙂
Hi Anita, really great to hear it has helped you.
What were your symptoms/diagnoses prior to starting the mitoQ? Have you surrendered other supplements in exchange for this one?
I have ME/CFS and FM. I had really bad brain fog, lack of energy, bad headaches, pain, severe fatigue etc. My pharmacist suggested taking Mito Q, and I noticed a difference the very first day I took it.
I woke up the next day with a clearer head and the brain fog has not been as bad as it was.
I gave up taking COQ10 as the Mito Q is the new generation COQ10, just 100 times stronger.
I still have to pace myself as I can still crash easily, but I can do a lot more than I could 2 Years ago. I make sure I go for a walk every day to build up my strength, and have added a lot of super food to my meals.
Best of luck to those on the trial, hopefully you will notice a difference.
Hey when your pharmacist recommends MitoQ – we’re really getting somewhere. Glad it’s helped and thanks for passing that on 🙂
Hi Anita, really great to hear it has helped you.
What were your symptoms/diagnoses prior to starting the mitoQ? Have you surrendered other supplements in exchange for this one?
Cort,
Thanks for the reminder and for the study. I am late to send the request for the study. I got the reply saying the study is full.
I acknowledge you for being honest about your regime.
Please see if the following helps you motivate to manage on your regime well:
Higher Energy levels = good health.
If any activity that improves energy levels will gradually build health through healing, not by managing symptoms. The only condition is that the activity should not be side effect prone and one should able to manage the same for long enough. How long? – I am not sure.
If MitoQ gives energy, please ensure you manage your regime well. I read few people did not get the intended or desired energy initially, they took time.
Also stay as much possible with organic diet and regular timings. Since I started 16:8 diet / fasting, I see good results. But when I step back on organic food and timings and pacing, I see relapse.
For all of you who are on the study, please ensure you follow the regime well.
All the best.
Have fun,
Hari
Good advice not to forget pacing if energy goes up. 🙂
What is 16:8 diet/fasting? 16 hours eating with 8 hours fasting a day?
Cort,
It is 16 hours fasting, 8 hours eating.
Even in that 8 hours, I eat only if I am hungry.
I started the same on Oct 1st. First I read from one of your posts, then dug deep. I had a minor set back in my second week, after I ate more even when I was not hungry with the intention to keep up with weight.
I am studying long term fasting. Will start 21 days water only fast after preparing the ground. Will share more.
Thanks for writing little about the fasting.
COQ10 is something I tried years ago and did not regard as beneficial; however, I understand how MitoQ may be significantly superior. I have registered with Mendus and signed up with MitoQ. Not sure yet whether I made the cut for the first group.
Hopefully I’m not too late to be part of the trial.
Cort, alt least a subgroup of CFS patiënts have mito problems. Look at the study of Julia Newton http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0122982
This also puts pressure on vascular, brain and immunological hypotheses. It is very plausible.
I have classic post-viral ME/CFS and was recently diagnosed with mitochondrial dysfunction. There is no doubt in my mind that mitochondrial issues are one of the main drivers of fatigue/exhaustion in ME/CFS. The problem is that there are so few mitochondrial doctors out there & it is a hard thing to test for but some day we will get there!
The company emailed me to tell me the CFS study is closed. They told me I could buy MitoQ at half price, but I have to resend them my Mendus registration number. But they did not give me a Mendus registration number!
Anyone know where I’m supposed to get a Mendus registration number?
Hi Pam,
Here is where you register for Mendus in order to get your ID to send to MitoQ:
http://www.mendus.org/cfs-register.html
I hope you’ll join us with the discounted MitoQ. The more we get the more accurate our results will be.
Joshua
After hearing from you, I immediately registered with Mendus & received an ID. I emailed and asked if I would get a 50% off code. You said I woyld received one soon. It’s been 5 days and I haven’t gotten a discound code.
I have classic post-viral ME/CFS and was recently diagnosed with mitochondrial dysfunction. There is no doubt in my mind that mitochondrial issues are one of the main drivers of fatigue/exhaustion in ME/CFS. The problem is that there are so few mitochondrial doctors out there & it is a hard thing to test for but I hope some day more doctors will be interested in specializing in it.
Hi Anne, just wanted to know, how were you diagnosed with mitochondrial disorder?
I’d also like to know how you were diagnosed, Anne.
Hi, I sent an email re. the trial, and got an email back saying that I missed out.
I am wanting to do the third study, but have not received a Mendus link.
Can you please help?
(I’m pretty devastated at missing out on the original study as I’ve been sick 28+ years)
Hi Isabelle,
You need to go here to get your Mendus ID:
http://www.mendus.org/cfs-register.html
We’ve experienced some delays simply due to the massive time differences. Cort in the US, I’m in Germany and MitoQ is in New Zealand. We all have different work days. So have patience with us. The MitoQ folks have to go through all the emails manually and so it may take a day or even two to get back to everyone. But we’ll do everything we can to get you into the third group.
Good luck,
Joshua
I didn’t make the first cut but I am supposed to be getting a coupon via email for 50% off!!
I’m very excited!
I only have to pay half price and I don’t have to take the placebo and waste my time with
it!
Yes, I am very concerned about the cost once my coupon is gone. I don’t know how much more of my necessities I can cut out of an already threadbare budget.
The more I read about the mitochondria though, the more I have to try!
Joshua from Mendus was a great help and got right back to me on email when I got a little confused on the site. He emailed me back twice in the same day.
I think they are very proud of their product and I’m looking forward to getting some for myself!
Meg.
Did you get your 50% off coupon? I never got mine 🙁
Hi Pam,
I’m really sorry. I’m not sure what’s happened but I’d like to try to straighten it out. If you see this post can you email me through the site?
http://www.mendus.org/contact.html
aww Ive just sent my request away but by the looks of the comments Im too late. 🙁 I was so looking forward to possibly trying it and seeing some results. Cant afford it myself. Oh well!
Sorry to hear that Hannah. You can get a 50% discount on it if you can afford that. (?)
According to what they just emailed me, they won’t give 50% off anymore. I signed up with them and got a code #, and they still won’t give me 50% off.
Hi everyone,
I want to thank Cort for publishing the information about the MitoQ trial. I signed up and just received my 2 bottles of pills so I will be starting the trial tomorrow. I have had personal experience with mitochondrial dysfunction due to a “primary carnitine disorder” (there is a blood test for carnitine levels). I was having a horrible time with frequent migraine headaches but was looking into carnitine metabolism due to some advice that it might be related to chronic muscle pain. My neurologist got me on prescription levocarnitine and within a couple of weeks I had my last migraine – since about 10 years now. I have had ME for 18 years now and levocarnitine has been one of the best things ever.
I think there is a real chance that this MitoQ could prove to be a beneficial therapy so I am very happy to be in this study.
Cort, you are amazing man – I don’t know how you manage to keep up with all the activity but I have come to rely on your blog and forums for information. I cant thank you enough, but I realized I can support your work more reliably than the occasional donations I have sent your way, so I took the plunge and became a monthly subscriber. What you do is truly worth a lot.
Everyone has something to be grateful for. I wish you all the best.
Greg
Thanks so much for your generous contributions in the past and your generous support now Gregory. Your contributions are what all me to do this (instead of working at McDonald’s – which I couldn’t do anyway (lol).
Good luck with the MitoQ and thanks for passing on the carnitine information…
I had problems with the MitoQ company. Never got a 50% coupon.
Cort, do you know if I can try MitoQ at full price, and how much it costs?
Pam, I think you may be having issues with your email inbox. I sent you an email several days ago proposing a potential solution and you never responded.
Joshua