



We don’t generally connect fibromyalgia with skin problems. The skin, though, may present an important window into what’s going on in fibromyalgia.
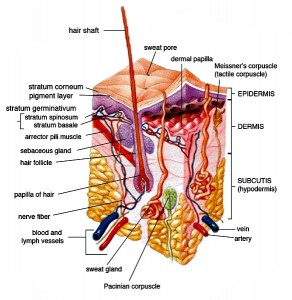
We use the blood vessels and sweat glands in our skin to warm or cool us. Both blood flows and sweat glands are largely controlled by the autonomic nervous system (ANS) – a system of concern in FM. The skin also tells the brain via its sensory nerves what are bodies local environment is like. Aberrant nerve transmission along these nerves could cause pain, numbness for other symptoms. The skin contains unmyelinated nerves that appear to be under attack in some people with FM.
From the autonomic nervous system to blood flows to sensory issues the skin is packed full of possibilities for understanding FM.
Nobody has yet attempted to use skin findings to solve a big problem in FM – how to diagnose it. FM, like ME/CFS, is diagnosed using symptoms.
The Study
This group measured different indices of the sympathetic skin response (SSR). SSR activity reflects “the electrical potential of the skin.” In simpler terms it measures the activity of the sweat glands located in your skin. An electric pulse is applied to the hand or foot and the response – a reflection of how the sympathetic nervous system is doing – is measured.
This test is often used to determine how well the peripheral nervous system is doing in diseases like peripheral neuropathy that knock out the nerves in the skin. If the neuropathy gets really bad as in diabetes no SSR at all will show up; the nerves are apparently dead. Since we have evidence of small fiber neuropathy in fibromyalgia, we would expect some changes to be found.
In total, the Turkish researchers measured a wide range of mostly commonly found lab tests. Then they attempted to determine which combination of tests diagnosed the FM patients and the healthy controls accurately.
- physiological tests -skin temperature, heart and breathing rate
- laboratory tests – rheumatoid factor (RF), c-reactive protein (CRP), white blood cell count (WBC), hemoglobin count, (HB), platelet count (PLT) and sedimentation (sedim)
- skin sympathetic nervous system parameters (latency response time, total time and maximum amplitude values)
If they could pull this off – and if the medical world validates their findings – we could have the first biological test for fibromyalgia ever. That would be a welcome development regarding the naysayers who still believe that FM is not real or is a psychological disease.
Results
The findings suggested that basic, easy to identify aspects of the FM patients physiology had been disturbed. Adding the sympathetic skin response to the mix boosted their accuracy in identifying FM patients correctly to about 98% and the sensitivity to 100%.
Increased latency times seen in the sympathetic skin test FM patients indicated that their systems were responding much more slowly than usual to the electrical impulses. They didn’t manifest the kind of obliterated responses sometimes seen in diabetic patients – where no SSR response is found at all – but the increased response times suggested some damage had occurred.

The researchers were able to identify FM patients with astounding accuracy using mostly simple tests.
Increased latency times have been associated with increased anxiety in another study. That finding brought to mind a recent post on Facebook which asked why even small things now bothered her/him so much? That’s a question I’ve been asking myself for decades. My guess is that a tweaky autonomic nervous system is involved.
Small Fiber Neuropathy and Fibromyalgia – A Short Review
This study and others indicate that is becoming an ever more interesting place in FM. A flurry of findings in 2014 suggested that from 30-40% of FM patients had a condition called small fiber neuropathy (SFN). Small fiber neuropathy refers to damage to the small, unmyelinated nerve fibers found in our skin and elsewhere.
That finding shocked researchers who’d presumed that the damage to FM patients stopped below their heads. Since that time several studies have validated those results. The question now is not whether SFN exists in FM, but how prevalent it is and why it’s occurring. Some work is being done in the both those areas.
Just last year a Spanish study suggested that reduced mitochondrial activity and increased oxidative stress in the skin of FM patients could play a role.
Earlier this year Martinez-Lavin’s findings of decreased corneal nerve thickness suggested that the damage to the peripheral nerves in FM wasn’t confined to the unmyelinated C-nerve fibers in the skin; i.e whatever was happening to FM patients could be happening in other types of nerves. Martinez-Lavin’s study also introduced an easy to use and non-invasive testing methodology. (No skin punches needed.) (The corneal nerve issues found do not affect sight by the way.) Caro and Winter have reported they’ve found evidence of large fiber neuropathy in FM as well.
Besides the skin unmyelinated or “C” nerve fibers are also found in the dorsal of the spinal cord and reach up into brain stem and thalamus.
The most intriguing study, however, popped up just two months. Sommer’s comparison of nerve fiber density the greatest reductions in nerve fiber diameter in the FM patients.
That entirely unexpected finding suggested a different kind of pathology is occurring in FM than in other people with SFN. In fact, Sommers called what she found “small fiber pathology” instead of small fiber neuropathy to distinguish it from the more common forms of small fiber neuropathy.
At least one other study is underway. Anne Oaklander hypothesizes that the present SFN testing regimens misdiagnose over half the adults under the age of 35 experiencing widespread pain. She’s in the midst of a multi-million dollar NIH-funded study to see if that’s so.
She’ll be examining a wide variety of tests (including corneal tests) to determine which tests best identify SFN in people with widespread pain. She’ll also attempt to figure out what’s causing SFN using blood tests and a close examination of the skin. Finally, she’ll assess how effective several treatments are.
The $3 million or so study began last year, and it’s slated to end (ouch) in 2020. I imagine, though, that it’s proceeding step by step, and we’ll find out if the rates for SFN will double in younger adults soon. That result would surely focus more interest on SFN.
- Check out the next blog in the SFN series: Diagnosing Fibromyalgia The Small Nerve Fiber Way
- For more on SFN and Fibromyalgia –Small Fiber Neuropathy (SFN) Resource Page for Fibromyalgia







We go round and round…..always searching…..so many symptoms that flip flop……more symptoms appearing…..always a surprise and a feeling of “OH, NO, NOT SOMETHING ELSE”…WE HAVE TO GET $$$$ FOR DR. LIPKIN. I THINK HE WILL FIND THE ANSWER. LOVE YOU, CORT. LOVE, JAVEN
Absolutely, maybe it will get to my goosebumps oddity that spring up on my body for no reason. Then I could sleep soundly with one less quirk one the list. But with all the forward I am going and I am going forward, with my CBD oil, vitamins, supplements,and vagal treatments, I still can’t stand up in place, like at the stove or my cutting board without pain. Or waiting in line, I have left before. Some one do so real research on the pain. Better yet, Medical Marijuana cream and pain.
Does anyone live in Montana, there’s a man that makes a marijuana salve that doesn’t affect your system or functions it’s called Original Relief by Vaughn Hirschkorn. I heard about in an article that athletes are using it. But it’s such a genuine blessing in nursing homes and hospices. And they said you get a good can of it for $40. I am told a little goes a long way. I really don’t understand why a cream or salve, that would not enter the system and give relief better than opium in targeted areas can’t be approved, standardized and legalized.
We’re on his bucket list! 🙂
But did not the ME study with Rituximab also cure fibromyalgia?
I don’t know of the ME patients also had FM but I would guess, since there’s so much overlap, that some of them did.
It makes sense because of the sensitivity levels. It hurts to lean up against anything, pick up anything, my hair and my scalp hurt, along with all of the major skin and body pain. I’ve tried SOOO many things, nothing works except cannabis..even in NY state where MMJ has been approved, the condition hasn’t….this sucks. I am ready to completely check out…this is no way to live.
I’m with you, I can’t bear the thought of waiting til 2020–I’ll be 65 & have been suffering since I was 50 (with the sleep deprivation since I was 20). I’m tired of looking for a billboard that justifies what most of us have been waiting for that will prove to ‘normal’ people who are able to have a life that we’re not psychiatric whiners (mostly family are guilty of this). I’m hanging on at least until my 10-year-old doggie (who like me, suffers from OA) has to leave this earth, then I won’t feel like I’m leaving anyone behind who really needs me.
I think the answers will start showing up before 2020. Bear in mind this is a pretty hot topic and I’m sure other studies by other researchers are underway.
I’ve had chronic fatigue since 2006 and just last year was diagnosed by Oaklander with SFN. She’s been treating me with IVIG and I’ve seen steady improvement in all my symptoms. Between these studies and the Rituximab studies, we’re seeing the immune system be the major cause for our systems. The next question is what caused our immune systems to go astray.
That’s big, Bob. Thanks for sharing that. You mentioned you have chronic fatigue. Did you have symptoms of numbness, burning, cold, prickling, pins and needles?
The only symptom I have is burning sensations particularly after I exercise too much.
I had some numbness and occasional feelings of what felt like ice water running through my veins. But it was far down on my list of symptoms; complete lack of energy, brain fog, exercise intolerance (all the standards) were much more an issue for me. Frankly I never gave the numbness/cold much thought. I had days laying in bed wherein if I had an itch on my head, I wouldn’t have the energy to raise my arm to scratch it.
I had both a skin biopsy and the a foot nerve biopsy to confirm SFN. I was in less than the 1st percentile in relation to nerve count. I also had positive ANA and Voltage Gate Potassium Antibodies.
I’ve had IVIG for a year (once a month infusions) and its made a big difference. I am not 100% but have been steadily making progress.
who is oaklander and how can i reach him?
Dr. Anne Louise Oaklander at Mass General in Boston
To the above commenters, Sally and Debby. I read your comments and I can relate to how difficult chronic pain is. I just wanted to write to let you know help and support is out there and if you are feeling like you need more support I encourage you to reach out for resources if needed. As difficult as it is to live with this, support can have a huge impact. Support may come in the form of a professional skilled in helping people living with the stress of living with chronic disease and/or pain. I was concerned about the above commenters and just wanted to reach out and offer compassion.
My heart goes out to you all. I have had FM for seventeen years since I crashed down onto a concrete floor from the level above, and amidst sustaining several broken bones etc., smashed my skull. I now have a 7 1/2″ plate in my head and sixty four nuts, bolts, screws etc., holding the whole lot together. (No pain from that! The pain is all from the FM and CF!). But, my points are two fold. After the accident it was discovered that I also had Klippel-Feil syndrome, ie. born with two vertebrae fused together. Also, I have a skin condition called Dermographia, in which I can write on my skin and leave legible words in the form of raised weals which take about an hour to fade. This is apparently caused by excess histamine in my skin. Ignoring the accident damage which I just get on with now, I am itrigued that both the K-F and the Dermographia which I have had life long, could be associated with FM. Incidentally I had symptoms of FM decades before I was diagnosed. The accident unfoubtedly brought it on, but even as a young child I remember “crashing” for two or three days at a time.
To end, Cort you are wonderful. Thank you for being there, and for your website. Keep smiling everyone. If you keep smiling you’ll win in the end! Love and hugs to all.
Virginia
I to hv the same syndrome and to discovered after a car accident. I guess it’s rare.
https://www.facebook.com/speakingthetruthaboutfibromyalgia
After more than 30 years with Fibromyalgia I totally welcome every study out there that will bring more attention and legitimacy to our condition. The more education that reaches the medical world the better.
One of our common phrases on our Facebook page: We look for the day that anyone can say “I have fibromyalgia” without the fear of not being believed”
Kathy Carre
Admin for Speaking the truth about Fibromyaliga
“Anne Oaklander hypothesizes that the present SFN testing regimens misdiagnose over half the adults under the age of 35 experiencing widespread pain. She’s in the midst of a multi-million dollar NIH-funded study to see if that’s so.”
This boils my blood. When my oldest was 6, he developed peripheral small fiber neuropathy. We were sent by a specialist at one hospital to another hospital per Dr. Oaklander’s request. We saw her once in the ER where she performed a punch biopsy on his right lower leg, and I think she may have come once more during our week from hell at that hospital. My son has PTSD from his experience with her staff and the complete failure to address his pain. He was discharged when he should have been transferred. He then saw Dr. Berde at Children’s and was in the MICU within 2 hours with his pain knocked down with lidocaine. He spent two weeks there. I would NEVER suggest Dr. Oaklander or her affiliated hospital to anyone.
Iam a single mom of 3, Iam 39 yrs.old. I have had Fibro since 2006. My mother has it as well. Dr.s now think my 14 yr. Old daughter has it. All 3 of us have the severe dry skin and bumps all over. ( Dr. Called it “chicken skin”. I have the needle pain but not constant. Usually when I have had too much stimulation or done too much. No medication works at that level, just a hot shower or bath. My hearing is so sensitive, I wear ear plugs alot. My pain can triple from something as simple as vacuuming or moping. I took my son to the park and just did light swinging on the park swing and hurt so very bad for a good 3 days. I can’t bare the thought of my daughter or kids having this same disease.
I just found this site today. I’ve had pain since I was a child. After many Drs. & tests, I found my family dr now who said I have fibromyalgia, I told him the first time I saw him .i thought everybody had pain all the time. Now 50 years later I still have pain, have tried PT, many meds I’m allergic to. I found Dr. Thomas Jach DO. He is a kinesiologist ,chiropractor, acpuncture ,laser,ultra sound and much much more. He is a brilliant man. After so many years his treatment s are the only ones that give any relief. I have OA,RA,neuropathy,pretty bad,daily headaches. & more.The kinesiology makes the pain much less. And a combination of supplements. I would suggest you find a good kinesiologist.(one who studied under Dr.Goodheart in Mich”) he has passed away in the last few years. Really it’s not a cure all but it works. I’m on maintenance now. My family Dr approves and will work with Dr Jach. And I’m 75 yrs old. That’s a lot of years in pain. I thank God for Dr Jach.He is in Flossmoor Illinois.
Hello, I live in the UK.
For 15 years I’ve had an Underactive Thyroid M.E./CFS and FM. and many more ailments.
Here in the UK Dr’s still don’t believe M.E/CFS,FM. They think it’s all in your mind.
One Dr commented “that thing, you feel a bit tired once in a while” another “just try to forget about it and get to the gym and get lots of exercise”
Not to be believed about the excruciating pain, chronic fatigue, brain fog and all the other extreme ailments is crushing – to say the least – Just thrown on the rubbish dump!
If I had a car accident resulting in amputation the reason for the amputation wouldn’t be the accident but because I have M.E.FM.
It’s a complete waste of time seeing the Dr for any additional ailment as you know before you even get to see them the diagnosis will be “It’s the M.E.FM” – Once you have one of these “labels” you are on a road to nowhere – Totally Soul Destroying! Kind Regards,LXX
I am in a fibromyalgis flare and i would be me than willing to be a test subject to help Dr’s find out more. Dr Reynolds of Toronto in 2006 said to me I was the worse case he had seen. So if you are interested , I am willing sincerely teresa sheflin