

It’s always encouraging to see established researchers from outside the chronic fatigue syndrome (ME/CFS) and fibromyalgia fields converging on them. David Systrom, a pulmonologist at Brigham and Women’s hospital in Boston, has been interested in idiopathic or unexplained exercise intolerance for at least a decade.

A significant number of people who cannot exercise have been a medical mystery to cardiologists and pulmonologists
He and Oldham recently published their magnus opus on exercise intolerance; a study employing over six hundred patients that stretches back nine years.
Unexplained exertional dyspnea caused by low ventricular filling pressures: results from clinical invasivecardiopulmonary exercise testing. William M. Oldham,1,2,3 Gregory D. Lewis,3,4 Alexander R. Opotowsky,2,3,5 Aaron B. Waxman,1,2,3 David M. Systrom1,2,3. Pulm Circ 2016;6(1):55-62. DOI: 10.1086/685054.
In it they proposed that a significant subset of patients with exercise intolerance and heart abnormalities have simply slipped through the cracks. No diagnosis has been able to explain their low energy production (VO2 max) during exercise; they don’t have heart failure arrhythmia cystic fibrosis or known mitochondrial problems. Aside from telling them that they’re deconditioned or depressed the medical profession hasn’t known what to do with these patients.
How a field that gets over $2 billion in funding year in and year out could let any significant group “slip through” the cracks is unclear. Systrom’s use of invasive cardiopulmonary testing techniques apparently has given him a unique insight into these patients.
“In this study, we tested the hypothesis that failure of these mechanisms to increase cardiac preload during exercise….may be the primary limitation….in an undiagnosed population of patients with unexplained exercise intolerance.”
Some of them, perhaps many of them, have ME/CFS/FM or POTS (or would be diagnosed with it if anyone tried) and those that don’t must have something close. (At least three people with ME/CFS/FM have ended up in Systrom’s office, and probably many more were in the study.)
Systrom, though, is ignoring the ME/CFS/FM for the moment – and probably rightly so. He has bigger fish to fry; his goal right now is to enroll his colleagues in the idea that they haven’t been correctly diagnosing a significant subset of their patients.
If my reading of medical history (I highly recommend “The Biography of Cancer” and “The Death of Cancer”) is representative, that conclusion is probably not to going over well.
The Study
In this study, Systrom evaluated people experiencing breathlessness (dyspnea) after exercise (or, as he put it later in the paper, simply exercise intolerance). First, he worked his patients to exhaustion on a bicycle as he gathered every bit of information he could using a procedure called invasive Cardio Pulmonary Exercise Testing (iCPET). It’s clearly not a fun procedure but yields a ton of information.
Systrom placed catheters into the radial and pulmonary arteries of his patients, had them jump on a bike and exercise to exhaustion. Then he allowed them to rest for two minutes, then they cycled without load for three minutes, and then Systrom turned the screws on again by increasing the resistance of the pedals.
Systrom essentially did a quickie repeat exercise study that lasted less than an hour.
These exercise-intolerant mystery patients aren’t a small part of Systrom’s practice and this wasn’t a small study either. Systrom, a pulmonologist, reported that about eight percent of the people who have done invasive CPETS in his lab fit in this group. This study presented the results of no less than 619 iCPET tests done over 9 years at Brigham and Woman’s Hospital in Boston.
Results
Systrom found that these patients had low Qt and ventricular filling; i.e. their hearts were not filling enough with blood during diastole – the part of the heart cycle when the heart fills with blood. (We just saw a similar pattern in ME/CFS in “Chronic Fatigue Syndrome: A Small Heart Disease?” and “A Mestinon Miracle.”) A finding of reduced stroke volume augmentation indicated that the problem probably traced to low preload. Preload is defined by how much the heart muscle cells stretch as they expand to increase the volume of the ventricles during diastole.
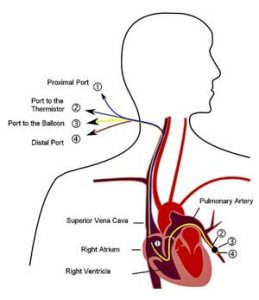
Catheters enabled Oldham and Systrom to gather the data they needed for to correctly diagnose their patients.
(The end-diastolic ventricular pressure and volume measures both measure something similar; they all measure how large the heart gets as it contracts to fill with blood just before it pumps it out.)
A critical part of filling occurs outside the heart. As we begin to exercise our veins vasoconstrict or narrow and the muscle pump in our legs swings into action to push the blood upwards. After the blood takes a trip to the lungs to get rid of waste products and become oxygenated, it moves into both ventricles which expand like a balloon (diastole), and then in a rush pumps the blood out (systole).
Systrom found, though, that the hearts of exercise-intolerant patients do not expand normally when they exercise. This inability to fill with more blood during exercise was why they exhibited low energy production (VO2 max).
Low Blood Volume Not the Primary Problem
When Systrom gave them IV saline to boost their blood volume most improved their Qt max. That suggested that low blood volumes did indeed contribute but here’s the kicker; even with the increased fluid intake, the exercise-intolerant patients still had a reduced response to exercise.
That suggested that reduced blood volume was not the entire problem. Instead, as with Newton, Systrom’s evidence points to problems with what he called impaired “capacitance”, which refers to reduced constriction of the veins during exercise. As noted earlier, once exercise starts the veins should narrow to propel blood back up to the heart where it can be cleansed, oxygenated and sent off to the muscles again. That was not happening normally in these patients.
What appeared at first to be a heart problem was actually a circulatory problem. We recently saw that Newton and Miwa found that blood flows to the heart in chronic fatigue syndrome (ME/CFS) are so reduced as to cause a substantial reduction in the size of ME/CFS patients’ hearts. This wasn’t because the hearts of ME/CFS patients were diseased (in heart failure the size of the heart expands) but because, like any muscle, the size of their heart muscle shrank when it wasn’t being worked enough.
Systrom didn’t diagnose any of the people in the study with chronic fatigue syndrome, but he did note that patients with POTS, autonomic neuropathy and adrenal insufficiency were part of the study. Any of these diseases could cause problems with constriction of the veins, and he noted that reduced heart size has also been found in POTS. POTS, of course, appears to be common in ME/CFS.
A recent study suggesting that autonomic nerve damage may be causing the reduced lung microcirculation in fibromyalgia suggested a similar process may be playing out in FM. Given the low cortisol findings in ME/CFS adrenal insufficiency – probably caused by problems with the HPA axis (not the adrenal gland itself) – is a possibility as well.
Systrom’s catalog of possible issues in POTS; inadequate vasoconstriction, sympathetic dysautonomia, and damage to the autonomic nerves by autoimmune processes makes sense given what we know about ME/CFS and FM as well. Fluge and Mella are exploring the role autoimmune processes may play in effecting blood flows in ME/CFS. Small nerve fiber issues are well known in FM and the reduced lung microcirculation findings in fibromyalgia may be caused by autonomic nerve damage.
Missing the Muscles?
Yet another clue from this complex study came from the decreased oxygen utilization Systrom found. This could be caused by blood flows that get shunted past the capillaries in the muscle fibers to pool in other less metabolically active areas such as the abdominal region. (Increased blood flows to the abdominal region have been found in POTS/ME/CFS). Alternatively, they could be caused by mitochondrial issues.
Not Deconditioning
The study also indicated that neither deconditioning nor a reduced maximal effort – both of which have been suspected in ME/CFS – play a role in the exercise intolerance found. Deconditioned people, ironically, exhibit an opposite finding (increased as opposed to decreased filling pressures) to that found in this study.

Not only was deconditioning not the cause of exercise intolerance but the tests results were opposite to those found in deconditioning
Systrom’s anecdotal report that a severe illness often predated onset of the exercise intolerance presented another possible link to ME/CFS. He suggested that infection/inflammation probably played a major role in the development of the issues he’s found.
Systrom noted how different the people with idiopathic exercise intolerance are than people with heart failure and other problems, and emphasized that this is not a small group. As noted earlier, almost 10% of the patients he’s done CPET testing on have this problem. (It’s possible, in fact, that this is the first time this group has been characterized in the scientific literature.) Despite the lack of attention given to them, Systrom found that their problems were as limiting as those associated with heart failure and pulmonary disease. While their activity was not noted, this was clearly a very functionally limited group.
Treatment
Systrom also pointed to some possible help for people with POTS. Four POTS patients in the small second half of his study improved using B-adrenergic antagonists which reduced sympathetic nervous system functioning and one improved with midrodrine. All of them also increased their fluid intake, used compression stocking and engaged in exercise training.
Systrom found that increasing blood volume in his patients resulted in a smaller-than-expected improvement in their VO2 max. He believed this was probably due to the effects of “dilutional anemia” which makes it more difficult for the red blood cells to pass oxygen to the tissues. This suggested that attempts to increase blood volume may be less effective than therapies that increase vascular tone; i.e. that support blood vessel health.
Systrom believes that circulatory problems, not blood volume, are the biggest issue facing these patients. He suggests that drugs like pyridostigmine (Mestinon) and midodrine (ProAmatine) will be most helpful, in particular, in people with viral onset or autoimmune issues.
This is not to say that increasing blood volume is not helpful; Systrom has his patients increase blood volume but he believes that other therapies will be more effective in this type of patient. See the story of one of his ME/CFS patients who has done very well on Mestinon.
Characterization – Not Cause
If Systrom’s, Newton’s and Miwa’s findings hold sway in ME/CFS then Dr. Cheney must get credit for uncovering the diastolic issues in ME/CFS as well.
We should be clear that Systrom is not getting to the heart of ME/CFS or FM; instead, he’s characterizing an important facet of what may have gone wrong. If problems with diastolic functioning are a key issue in ME/CFS the next question becomes what’s causing it? In the case of his POTS patients, Systrom suggested that an infectious or otherwise significant event tripped off an inflammatory autoimmune response, which, in turn, caused the blood flow problems.
That’s very similar to Fluge and Mella’s proposal that autoimmune issues are causing blood flow and other problems in their ME/CFS patients. They believe that Rituximab’s success may be due to its ability to reduce the levels of autoantibodies present. POTS is more and more being considered an autoimmune disease as well.
Convergence
It’s very good to see a well-published researcher from outside the field converging on it, and coming to similar conclusions as our researchers.
It’s good as well to see the exercise intolerance found in ME/CFS showing up in so many different ways. The Workwell Group and Dr. Keeler have used a repeat, two-day exercise test to demonstrate that energy production is reduced in at least a significant subset of people with ME/CFS. Systrom used a one-day repeat exercise test to demonstrate that exercise intolerance is a significant problem for an important subset of his patients – some of whom must have had ME/CFS (or would meet the criteria for it). Peckerman used (unpublished) a one-day test to show that exercise quickly reduces heart blood flow in people with ME/CFS.
The data from these groups suggests that problems with the blood vessels or mitochondrial issues or both may be the key to these finding. Systrom didn’t get into mitochondrial problems much but he stated mitochondrial problems could also be in play.
Addendum – A Postural Orthostatic Tachycardia Syndrome (POTS) Slant
Postural Tachycardia Syndrome (POTS) Is Not Caused by Deconditioning. Svetlana Blitshteyn1, MD and David Fries2, MD
Systrom and Oldham’s study prompted a rather long letter titled “Postural Tachycardia Syndrome (POTS) Is Not Caused by Deconditioning” to the editor by Svetlana Blitshteyn, MD of the Dysautonomia Clinic at the University at Buffalo School of Medicine and David Fries, MD of the Sands-Constellation Heart Institute at Rochester General Hospital.
They believe that Systrom’s finding are probably applicable to the majority of POTS patients.
The extensive, non-invasive cardiac testing most POTS patients undergo at some point leave them being told that their symptoms are caused by deconditioning. Indeed exercise studies showing that they exhibit low stroke volume and reduced heart mass have attributed both to deconditioning.

Two doctors applauded the study for demonstrating a physiological basis to the exercise problems found in POTS
Systrom and Oldham’s study was the first to show that the hearts in POTS patients don’t appear to be deconditioned at all; in fact, the low ventricular filling pressures found are opposite to the high ventricular filling pressures found in people who are deconditioned.
This is not to say that deconditioning does not occur in POTS. Anyone who undergoes long periods of bed rest will become deconditioned, but the study indicates deconditioning is at most a secondary factor in POTS. The authors also applauded Systrom and Oldham for showing that reduced effort is not contributing to POTS patient’s exercise intolerance.
The authors hoped this study will provide some relief to POTS patients who, despite the fact that they do exercise and are not bedridden, still get blamed by their doctors who believe inactivity is causing their problems.
Key Points
- Idiopathic Exercise Intolerance is not rare in doctors offices but has rarely been diagnosed correctly
- Neither deconditioning nor lack of effort is to blame; in fact, people with unexplained exercise intolerance have the opposite findings to those in deconditioned people
- Low blood volume contributes to, but is probably not the main cause, of unexplained exercise intolerance
- Blood vessel or mitochondrial problems (or both), that prevent sufficient amounts of blood getting to the heart during exercise are probably the main cause of unexplained exercise intolerance
- Treatments that emphasize blood vessel health may be more effective than blood volume enhancers
- The immune system may ultimately be the culprit







The main reason of exercise intolerance is weak cardiac muscle with exercise.primarily this is from the poor microcirculation in the cardiac muscle and increased secretion of TNF-alfa from cardiac
muscle with exercise. This is well documented on the pm.2.5 related articles.
In fact the main CAUSE of CFS/ME is microvaculitis all over the body,heart, brain, kidney.In the brain the microvacular vessel is inside of the nerve itself That neurovasculitis result in neuroinflammation–damage of brain and spinal cord and peripheral nervous system
Thanks Doctor, Very interesting. I’m a fan of the idea that the microcirculation is involved and if it is I would expect it would be everywhere. Would it be the result of an autoimmune process?
NOT exactly autoimmune process,but immune mediated inflammation of microcirculation. There are 3 different kind of cytokine involved in this immune inflammation–TNF-ALFA,IL-1beta,IL-6.
Our heart muscle is in a sense endocrine organ full of TNF-ALFA.
When you do exercise,the amount released from heart(TNF-ALFA) is
increased, this TNF-ALFA REALLY MAKES HEART INFLAMMATION. And also
we know there are potent vascular spasm from microvascular inner line–ENDOTHELINE 1(ET1).THERE ALL MAKES THE POOR CIRCULATION OF HEART MUSCLE,KIDNEY AND BRAINS.IN our country there are so many brain infarct with bleeding in the CFS/ME patient.
I agree. It could be due to dysautonomia (acetylcholine receptors, vagus nerve etc..) as well or infection. I also like the idea of problems with red bloodcell shapes as well.
Corr Johnson, lifelong I have been a competitive female athlete who has not been able to find a specialist who could correlate my shortness of breath with the painful hypoxic type pain in my quadriceps. I could run a marathon and qualify for Boston, but would have not been able to teach a simple aerobics because so short of breath associated with leg pain. After years of trying to figure out why this phenomena happens, I found your article that connects the two. Would there be any advice you could give me, or test trials in which I could participate
Interesting. I don’t know of any trials but the two people I’m most focused on in this regard are David Systrom – several blogs on his work on Health Rising and Ron Tompkins at Harvard who is going to dig into the muscles in ME/CFS.
Dr. Park, where are you located? If it is not possible to see you I would like to take this information to my doctor. Would a print out of the comment be the best source of information or do you suggest a website?
I have always felt that there is an issue in my heart contributing to my CFS.
What do you suggest or know of to remedy the microvaculitis?
I have a Bemer mat which is supposed to help with cellular oxygenation and microcirculation. Do you know anything about the Bemer?
we are at the SEOUL,KOREA. MAIN TX OF micorvaculitis is
IVIG.LOW DOSE once per wk for 6 months
Dr Tae Park,
How does one diagnose the microvaculitis? Is there a specific type of Dr I should see? Blood testing? Heart test? I have a pacemaker due to a 20 second pause that I relate to nerve issues. My EKG and Echocardiogram are clear. I have been disabled for 7 years. I am in Southern California and have fairly severe fatigue and muscle weakness.
I have never said the heart was damaged in CFS. What is happening is an energy linked (aka mitochondrial dysfunction linked) pure cardiac diastolic dysfunction with compensatory increases in systolic action called increased LV ad RV strain or torsion and both recently confirmed by MRSI of the heart by Hollingsworth et al 2012. The combination of poor diastolic filling and compensatory increased LV and RV strain or torsion produces the small heart in CFS described by the Japanese. The underlying problem is poor redox buffer control confirmed by the 100% finding of oxygen toxicity by cardiac IVRT response criteria in all CFS cases. If redox buffer is impaired, then there is a compensatory feedback inhibition of the mitochondria to help control the redox state so the mitochondrial dysfunction is a solution and not the main problem. Viruses that need DNA integration into the human DNA need to suppress redox buffer in order to increase methylation block so they can integrate into human DNA and survive. Neuroinflammation is a side show of the cytokine response effects to human DNA integrated viruses such as HHV-6A which is harbored in the oligodendrocytes of the brain and elsewhere. Increased LV strain with C-fiber firing along with low cardiac output seen in all CFS cases is responsible for POTS, NMH and OI as well as poor exercise tolerance. Another factor in poor exercise tolerance in CFS is poor hypothalamic driving of the HPA axis published by Demitrack out of the NIH in the mid 1990’s. The average cardiac index in my practice of over 2,000 cases examined is 1.8 (range 1.04-2.8, normal 3.0-3.5). Nothing is more disabling that a low cardiac output state. 500 consecutive measurements using 3-D volumetric which is as accurate as MRI confirms these numbers. 1.8 is at the cardiogenic shock threshold. The reason CFS cases are not in cardiogenic shock is because they do not have cardiac disease and very good and even increased systolic action as described above.
Thanks for clearing that up 🙂
I tried IVIG for 6 months. I was exhausted for 2 days after treatment and then had one good day. In the end I found that it made me itch like crazy and I stopped treatment.
For what it’s worth, I have had at least two echocardiograms which showed mild diastolic dysfunction – meaning the ventricles showed stiffening when they were supposed to be filling. For the ventricles to expand to accept blood from the atria, it actually takes energy. This is a particularly interesting study and I will have to go back and try to figure out when my echoes were done in relation to when I got sick. I think one was actually before I got sick. Thanks again for a great report!
My echocardiagram showed stage 2 diastolic dysfunction.
I have the same problems 🙂
Dear Professor Davis,
I have working on this problem for a long time. I agree with you that POTS might well be one of the most important sources of disability in ME/CFS.
There are a number of curiosities that I might bring to your attention. I also agree with you that blood volume is relevant but not causal of POTS. Certainly, exacerbations of circulating volume, as in the dehydration from vomiting or poor fluid intake, create severe weakness and poor cerebral blood flow, especially if there is a concomitant loss of sodium ion. Poor brain circulation (insufficient to cause fainting but enough to lead to suboptimal fuel supplies over time), is one important cause of head fog.
Using Paul Cheney’s method of Tilt Table Testing (which includes echocardiography in both the supine and 70 degrees tilt positions) there are indeed problems with left atrial filling and left atrial pressure, with demonstrable reductions in left atrial dimensions (what Dr Cheney calls ‘left atrial cavitation’). Stroke volume and the cardiac index are nearly always reduced (unless the tachycardia is vigorous enough to maintain the cardiac output).
These left atrial parameters strongly imply pooling of blood, either in the legs and/or abdomen as a result of orthostasis (standing AND not moving). Left atrial issues may be seen in the supine position as well, and this finding supports the likelihood of a concomitant blood volume depletion problem.
To fix hydration issues is quite complex. A combination of glucose and salt (NaCl) as a hydration solution instead of plain water, can provide substantial functional and symptomatic benefits and may reduce the severity of the tachycardia, and has an important palliative management effects far superior to the use of fludrocortisone (Flurinef) for example.
At presentation, nearly all patients have decreased 24 hour urinary sodium outputs, more so in the more severely affected patients. The glucose/salt fluid intake strategy (which aids salt absorption in the SMALL bowel), unlike fludrocortisone (which at best is responsible for only 20% of normal salt absorption – all in the LARGE bowel) is the most effective way of restoring 24 hour urinary sodium values to normal. Having achieved normality in urinary sodium however, hyponatraemia (low serum sodiums) may still persist or occur sporadically.
This is where a small amount of Flurinef may assist (by helping tubular reabsorption of sodium), but one then runs the risk of tissue fluid retention – not a desirable side effect for most people.
Another problem in ME/CFS is polyuria. Polyuria can be caused by drinking too much plain water without electrolyte in a vain effort to self hydrate (thirst mechanisms may sometimes fail, so self hydration, especially on waking in the mornings, has to be deliberate).
The concept of ‘drink to thirst’ does not apply here.
The other problem is diabetes insipidis, and vasopressin in low dose may help to limit polyuria (urine volumes can be excessive on occasion), but should only be used when sodium status is adequate. Otherwise, dangerous hyponatraemia may ensue.
Having done all this, the body still seems to be unable to retain fluids, and without adequate self discipline, this is what happens. It may become necessary to weigh oneself daily, as a more accurate guide to hydration status (1kg of body weight = 1000 mls. of water), all else being equal). To do this, one should determine what is one’s best body weight: even one kilogram of body weight too low (1 Litre) may sometime render oneself bed bound.
What is also strange is that Hb (haemoglobin) levels remain normal, even when there is an unequivocal iron deficiency, as defined by extremely low ferritin levels, and despite the presence of chronic inflammation, which normally would produce a condition called the ‘anaemia of chronic disease’. Something unknown is maintaining Hb status despite these factors. Hb has a role in blood volume, but only if red cell mass is taken into account. Accurate testing for this is not always available, but some studies suggest that red cell mass is also reduced, and if one is also dehydrated, the expected anaemia will presumably be masked.
I agree with you and Dr Park that there is likely to be a small vessel disease or anomaly at the heart of the matter, and while the above considerations are very important, they are not the whole story.
For example, Venous Blood Gas (VBG) analysis is usually abnormal in ME/CFS and results may vary between a slow capillary circulation (causing increased venous pCO2 and possible low venous pO2), and AV shunting though arteriolar AV shunts (regulated locally by various mediators, including nitrous oxide)(causing high venous oxygen saturation levels), or both phenomena may occur together.
I have not seen any evidence that would indicate an overt vasculitis, but inflammatory mediators perhaps TNF-alpha, or more specifically, NFkB, might be involved in some or even most cases nevertheless.
We must not forget previous work showing that there is a role of stiff Red Blood Cell membranes in poor microcirulatory states. Such RBC’s are unable to reshape fluidly in order to freely fit through the diameter limited capillary networks. Thus microcirulatory standstill may occur.
Speaking of capillary networks, in normal resting muscle, only 30% of such capillaries are in free flow state at any given time. This percentage changes with exercise and other manoeuvres, so a regulatory defect in the degree of blood flow distribution may be operating as well in ME/CFS.
I have NOT found mestinon to be of use in many patients, but there are some patients who really do benefit from this intervention.
Finally, and anti-intuitively, ACE-inhibitors may help improve the cardiac index and peripheral circulation. Cold feet and cramps, for example, may benefit. More importantly, however, is that some patients with severe POTS have evidence of left ventricular hypertrophy, and paradoxically, may ultimately develop HYPERtension. ACE inhibitors will reduce this over time and also improve the efficiency of myocardial contractility and efficiency.
My colleague, Dr Neil McGregor, is identifying metabolic anomalies, and matching them to genetic anomalies, symptoms and stool biochemistry. The various phenomena may have seperate origins. One wonders how so many genetic factors can come together in one patient. Perhaps population migrations and interactions between populations may allow “incidental’ anomalies in each population to converge?
In summary, many factors operating in tandem, together seem to come into play, making the management of what appears to be an irreversible disorder, a very challenging one that many of today’s doctors do not know what to do about, let alone know that POTS exists! It looks as though such a situation may one day change.
Sincerely
Dr John L Whiting
Infectious Diseases and General Medicine Consultant
Brisbane, Queensland, Australia
I have had Fibromyalgia for 25 years. Fluid control problems were implicated right from the start. I was extremely fit and a competitive cyclist. Excessive need to urinate interrupted my riding regime before I started to experience the FM pain and tension, but they followed eventually. I was having to experiment with electrolytes to keep cramp at bay, Magnesium and Potassium were as important as sodium or more so. Eventually I discovered Hair Mineral Analysis testing as a guide to where the deficiencies might be; but these have always been volatile. My weight has fluctuated wildly all along, obviously with fluid content. Besides this I have an appalling tendency to gain fat while eating no more than a normal person, I need to be dieting extremely strictly, and exercising regularly, to remain merely “somewhat overweight”.
The Hair Mineral Analysis Testing eventually started to show Cadmium toxicity, which is disturbing, as Cadmium only starts to show up in the hair once the internal organs are saturated. I have a theory where the Cadmium came from, and have been dieting and supplementing in ways that have reduced it. Maybe the fluid control problems are related to the body attempting to remove a toxic substance?
I kept fighting to exercise in spite of FM, which kept me more functional than otherwise all these years. But 3 years ago I formed a hypothesis and put it to effect – by exercising strictly at low intensity and avoiding higher intensity (and relatively “high” intensity is easy to hit when you have FM), and following a Paleo diet, and a number of other initiatives, I have slowly reduced pain and tension, and gained muscle mobility. I have been commenting regularly on this blog as I have made progress.
My hypothesis is that the cardiovascular system was somehow adversely affected by the malfunction in muscle tissue and fascia; and my ability to recover from “anaerobic” exercise or exertion above a certain level was impaired to the point that post-exertion damage (oxidation, lactic acid?) was ongoing for a long time rather than for a short recovery period. What I have done, is build a kind of aerobic capacity, and gained the benefit of exercise (flushing etc) without triggering the previous dis-benefit.
I also was forever frustrated that I had a large frame and large, strong muscles, and in some gym routines I was able to exert considerable power – in a seated leg-press for example; yet in certain postures my entire system simply rebelled – I was unable to squat, for example. It was not POTs as it is usually defined, but something like it – as soon as I went into certain postures, including extension of the arms to perform a routine function like hanging washing, I would go into cardiovascular overload. I have slowly been re-gaining the ability to to some of these things without the overload.
I have read a hypothesis that makes sense, that the cardiovascular problem is related to small blood vessels trapped in tight fascia tissue and constricted, especially so when certain postures are adopted. Trigger points in the muscles are also present, I believe due to loss of lubrication of muscle fibre and fascia, which leads to fibres sticking together and forming clumps. All this is gradually diminishing in me, and response to specialist massage is now happening (for years massage was just a waste of time and money, the underlying condition meant the muscle dysfunctions persisted).
Glad to correspond further.
Thanks again Phil,
Have you ever tried the valsalva maneuver? The valsalva maneuver actually reduces preload to the heart.
Interestingly, it’s also used to “believed to be the optimal breathing pattern for producing maximal force and is frequently used in powerlifting to stabilize the trunk during exercises such as the squat, deadlift, and bench press, and in both lifts of Olympic weightlifting.”
I wonder if during those squating situations you’re reducing blood flows to the heart. If you get dizzy during the valsalva maneuver I wonder if that might suggest that that is happening.
I also wonder if during squatting blood is preferentially flowing to your abdominal area or if you’re just putting too much pressure – for you – on the muscle pump in the legs?
I used to be really into body building. Now blow drying my hair or anything with my arms up brings on POTS. I can do horizontal exercise and seem to do okay with a leg sled. But a squat -forget it. I think it has to do with whether or not we are taking blood away from our head. And the fast up, down motion of a squat doesn’t allow our body to adjust the level of our blood fast enough.
My hubby says the larger muscle groups require more blood and it goes into those muscles and away from our head. The support of sitting on a sled doesn’t cause it so bad because your head is on the same level as your legs.
Issie
hi philip have you had your thyroid tested by a doc who knows to test for all thyroid markers? if you have not it might explain your weight problems.
Marta, I have been trying for YEARS to get my doctor to get a full thyroid blood test done. I will keep trying!
Cort, I never heard of the Valsalva maneuver before. I just tried it for the first time. I think I might be vulnerable to passing out if I try too hard, I will have to be careful! Got horribly “overloaded” immediately, felt ghastly; then on release, just about passed out! Had to collapse onto a chair which I had strategically placed just in case. But I feel better for it afterwards, like after a good stretching session – including that squatting felt easier.
Another angle is that I became aware recently that I have always had lazy abs and lats, and these are what are used in the Valsalva maneuver if you work out how to do it properly, to produce the compression of the body core. I do wonder if there is a lack in autonomous muscle control in some of us, that has left us predisposed to more serious conditions later in life. Do normal people’s abs and lats activate automatically a lot of the time, in appropriate ways to the way the body is being used? And mine never did? Having become aware of this, I have been working on activating them. So the Valsalva maneuver is a fascinating further step in my experimentation with self-treatment. Watch this space!
Issie; I agree, and add that trigger points and knotted tissue in the muscles at certain points are highly like to introduce a greater-than-normal constriction on blood flow. Especially at the back of the knee, for example. I have been getting my massage therapists to work on this and it seems to be helping. Because of stretching and crunching routines called “Body Mechanics” that I have been learning, I have become aware of trigger points that restrict my flexibility, and get massage therapists to work on them (particularly someone trained in trigger point therapy). I have recently got rid of the tendency for cramps in the arches of my feet (on attempting certain stretches and crunches), after getting trigger points in the feet and lower legs repeatedly worked over.
Thanks Phil – very interesting! Besides walking the one exercise I am doing is trying to strengthen my abdominal core. I was going to ask you if you were doing Pilates or anything in that area. That is an area where blood can settle. Looking forward to future posts.
Hi Philip, in response to:
“I have read a hypothesis that makes sense, that the cardiovascular problem is related to small blood vessels trapped in tight fascia tissue and constricted, especially so when certain postures are adopted.”
-> I find remarkable and consistent improvement in my OI-related symptoms by doiing several times a day gentle neck and shoulder exercises.
This makes sense to me as follows: the veins in the neck are (if I understand correct) veins that can vary more in diameter than any other veins in the body and are in healthy persons quite often in the “middle posistion”. This seems to allow to better change the blood flow to the head in accordance to the quickly varying (positional) needs compared to other body parts.
Tight neck and upper shoulder muscles close these veins off by default and disallow good variation, leaving blood flow to the head poorly regulated.
Strong movements like squads can possibly thighten (or rebalance tension) muscle all over your body including neck and shoulder ones.
People with ME/fibro are quite vulnarable to this in my opinion as:
* they have often adrenaline/epiphrene problems; adrenaline thigtens muscles. Plenty of us have been told “learn to relax your muscles!”
* our expression “to shrink of pain” makes quite a lot of sense to me: I learned that continuously/quickly thigting ones muscles (espescially neck!) is an effective way to decrease pain sensitiviness (but has huge drawbacks!!!). I learned this pain control method unconsciously and had to dislearn it in order to reduce its damaging effets. (note: just taking pain killers does not remove this bad tendancy).
Dr Whiting,
Thank you so much for your detailed and informative comment. My daughter was diagnosed with POTS about two years ago. It’s been a non stop journey of bouncing from one dr to another to treat different symptoms that keep popping up. Unfortunately, each dr has a different treatment plan. It feels as though we are on a runaway train.
I most certainly will bring up this article to my daughter’s POTS dr, especially some of the points that you made in reference to the affect in POTS patients.
Thank you again.
Stay tuned for a really kind of wild POTS recovery story…
Having POTS myself, I know how complex and complicated it is. And there are so many different approaches to treatment. (Many of which I question.) But, if you don’t know what subset type of POTS you are trying to treat….you could be making things worse. I have HyperPOTS with high upright NE levels and more Hyper blood pressure with a drop more into normal ranges. I also have extremely low aldosterone levels. Adding more salt was wrong for me and most of the “normal” meds tried for POTS was a diaster. The higher NE levels that brings on tachycardia turns out to be a protection response of my body to keep my blood flowing and get blood and oxygen to my head and heart. Stopping that response is not good for me. My body is trying to “save me”, by increasing heart action to move blood up. Yes, as uncomfortable as it is – I prefer it over not having the response. My having kidney involvement – I was at 3rd stage CKD – now normal – was a key point. Taking the load off my kidneys by not having animal proteins helped this to become normal and also helped my over zealous autoimmune system to balance out better. I’m still working on things, but better than I have been.
Issie
Did he respond?
What an interesting study! The findings and assumptions taken from these clinical exercise trials aren’t really surprising. I have a cardiologist among “my specialists.” All my EKG’s for the last several years since I’ve been on Medicare have been normal. I get one for my annual physical at my primary care doctor’s, and one at my infrequent visits to my cardiologist. I take a beta-blocker for my tachycardia. My tilt table test three years ago was negative. (Had a previous one long ago in Houston that showed significant neurally mediated hypotension.) My recent EKG at the cardiologist’s showed mild mitral valve prolapse, which was rather alarming. The cardiologist said “It’s really mild, so let’s just keep that in the back of our minds. You may not require any treatment until you’re in your 80’s.” I laughed to myself and thought “Nice try doctor!” I’m 71 now, so we’ll see. I’m not aware that anyone in my family had this, so I’m not sure why it just popped up at this stage in my life. I will do some research. Makes me wonder if the CFS/ME could be contributing to it. I gather that it’s not an uncommon diagnosis and some people apparently go through their lives with it undiagnosed, unless it presents obvious side-effects.
In addition to auto-immune and viral causation one might consider a compounded MCAD issue causing unknown vasodilation or lack of construction. Moreover, in ME/CFS patients w elevated TNFa levels effecting micro circulation w concomitant MCAD might well benefit from a TNFa antagonist as therapy per Dr Lawrence Afrin’s comment that MCAD is almost always implicated in elevated TNFa per his book. Just a hypothesis. Yet one worthy of looking into in a specific subset of ME/CFS (MCAD) or subset cluster MCAD,Viral onset, auto-immune).
In addition the strong link between MCAD and POTs?
I went down the whole MCAD route after getting a elevated tryptase back, I tried all the mast cell stabilizer meds Rx and over the counter didn’t feel anything. i have no skin issues, any ideas?
Dr Goodman, at Mayo – I was told – is going up on how much GastroCrom his difficult cases use. Are you using all three histamine blockers and GastroCrom and ketotifen?
Some also find they can use a small dose of aspirin to cause a small release instead of a dump. (I cant.) Others also find quercetin and rutin to help. (Again, I dont.) And still others find luteolin to help. (I haven’t tried.) There is also DOA enzymes. (I haven’t tried.)
Issie
Correction – DAO enzyme. Ha! Could be a DOA (dead on arrival) response if not corrected/managed well enough.
Issie
I am glad to see Dr. Whiting’s acknowledgement of the role of ‘stiffened’ red blood cells – hopefully he is referring to the work of Dr. L. O. Simpson’s studies in the hemorrheology issues in chronic diseases, including ME/CFS. The non-deformable erythrocytes cannot traverse the microcirculation, causing the oxidative and nitrosative stress referred to in so many studied. If this affects muscles, as it does, as well as the brain and the endocrine system, it easily accounts for the range of symptoms found in ME/CFS. Exercise intolerance following failure of the aerobic metabolism…the heart is a muscle, effective muscular activity is essential in the gut; muscles in the eye must work effectively to allow the eyes to focus….wherever the microcirculation is impaired because non-deformable RBCs are blocking delivery of oxygen and removal of metabolites, there is going to be damage and malfunction. There are currently efforts to reprint Dr. Simpson’s book, ‘Blood Viscocity Factors – The Missing Factor in Modern Medicine, which is available from the Mumford Foundation. In the meantime, a detailed account of his researches is given in “Ramsay’s Disease’, of which I am co-author. Readers can gain immediate access to his thoughts via his article in the e-journal ‘Positive Health’, via http://www.positivehealth.com/article/cfs-me/the-importance-of-blood-flow-and-evening-primrose-oil-in-me
The blood flow problems can be alleviated in a proportion of ME sufferers by taking 6 g per day of fish oil, or 4 g per day of genuine EPO, or injections of B12 as hydroxocobalamin, or pentoxyfilline. These recommendations should be included in any discussion of blood flow problems in ME/CFS/FM, as they are relatively easily available (except the last), inexpensive relative to complex medical interventions, and they have proved helpful to many ME patients.
Nancy, it’s nice to see mention of Dr. Les Simpson’s work and research here. Back when I lived in Houston, TX…oh, gosh, it must have been around 2000, Dr. Simpson came to one of the Houston CFIDS Support Group’s meetings. Dr. Patricia Salvato, who was also my doctor at the time, introduced him. He talked about his findings and his hypothesis about deformed RBCs. He took blood samples from all who wanted it done to take back to New Zealand with him. Quite awhile later, we all received an individual report explaining our results. According to what I recall, I tested positive for the deformed RBCs, and was advised to take the evening primrose oil (EPO). I do recall that the report was rather confusing! However, I was still quite sick at that time and neurally mediated hypotension was one of my symptoms. The EPO lowered my BP even more, and I couldn’t continue taking it since I was still working. Therefore, I do not know if it would have helped my illness had I taken it for an extended period of time. I no longer have that report, unfortunately, since I was rather aggressive in clearing things out when I moved here to NY. I see that Dr. Simpson is still living and apparently still doing his work; he has a web site. He was quite up in years when he visited Houston, but then I’m quite “up in years,” whatever that even means any more! I will read the article at the link you shared, and even consider possible B12 injections. I’m quite sure I could tolerate that. Thank you for sharing this information, Nancy! Judith
Oh, yes, I forgot! This appears to be Dr. Les Simpson’s web site: http://www.blood-flow.net/ Also, Cort, I know that you’ve had an article on this blog referring to Dr. Simpson’s findings because I ran across a link to it yesterday, so wanted to mention that as well (but now I can’t find it!). 😛
Judith
Has there been any research into a possible connection between the C677T mthfr variant and exercise intolerance? Would the inability to methylate some of the b vitamins cause some of the symptoms of cf/me/fm etc.?
I have ‘ME/CFS’ triggered by a viral infection over 5 years ago. Last year, after a frustrating assessment at CFS Specialist Services (I’m in the UK, the apparent victim-blaming approach to medicine came as a bit of a shock) I sought out and paid privately to see a specialist in a condition that I’d come across online. I was subsequently diagnosed with the Hypermobility variant of Ehlers Danlos Syndrome. A hereditary connective tissue disorder characterised by generalised tissue laxity that apparently has less awareness, or sometimes even belief, among medical professionals than PoTS or ME/CFS/FM.
I have since been diagnosed with both POTS and possible MCAS (a non-proliferative mast cell disorder). Both of which are common comorbidities with EDS. I believe that there is no published data to support the latter, just recent observation among specialists. However, the link between EDS and POTS is well established, with the overwhelming majority of EDS patients having POTS. It is believed that one of the main reasons for the prevalence of POTS in this population is blood vessel laxity.
As such, the above article seems very relevant to me (as do the comments from Dr Park if the inflammatory mediators mentioned are released from mast cells). So much so that it seems surprising that there is no consideration of EDS or other connective tissue disorders within this patient group. Hypermobility EDS is considered massively underdiagnosed and is considered by some to be present in the majority of the CFS/ME and particularly FM populations (though I’m sure mast cell issues and POTS can occur independently), yet there seems so little awareness of it among professionals dealing with these conditions.
Just a side note to Judith F – mitral valve prolapse has also been linked to EDS (and is usually benign). I would be curious to know whether you, or anyone in your immediate family is (or was) hypermobile.
Thanks Helena, the idea that EDS is causing blood vessel laxity in ME/CFS is really interesting. Did you have classic signs of EDS as described by the Beighton test?
Yes. My Beighton score was 6/9 and I have hypermobility in pretty much every other joint that was checked. I probably would have scored 9/9 had that test been done 10 years ago though. These days tight muscles won’t let me touch the floor!
It’s an interesting question as my niece shows signs of EDS, yet my sister would not score high enough to be diagnosed under the Beighton criteria (though I think there is some allowance for that under Brighton criteria). She does exhibit other signs of it (e.g. skin fragility, flat feet under loading), but doesn’t have the severity of health issues that I do. I’ve also heard from health professionals that they’ve come across patients with close relatives with EDS who don’t exhibit any obvious hypermobility, yet seem to have all the internal issues such as POTS, digestive problems etc. I don’t know whether there’s been any reliable research on that though.
Thank you, Helena, for pointing out the link between mitral valve prolapse and EDS. I’m definitely not hypermobile, quite the opposite. As far as any family members who were/are, none in my immediate family. Thank you also for sharing your story and your thoughts regarding the lack of awareness about all these various and potential contributing disorders. So many puzzle pieces that have yet to be put together.
Like Judith F, I definitely do not have hypermobility. When discussing FM with others (I have FM, not CFS) I have always assumed that we all suffered from muscles going tight, immobile, foreshortened, and knotted. Myofascial stickiness and pain, and trigger points, seem to also be common. So now I am wondering whether “Fibromyalgia” is really more like a symptom than a condition in its own right, seeing there are such widely disparate morbidities affecting different people who have it. After all, the diagnosis is based on “tender points” – but what if these tender points are simply a symptom of many different conditions?
Perhaps a diagnosis of “Fibromyalgia” is about as helpful as a diagnosis of “nausea” or “cramp”? Some people actually have EDS, others have myofascial pain syndrome and trigger points, others have POTS, others have thyroid malfunctions, others have an infection, and so on. By diagnosing “Fibromyalgia”, possibly the medical profession is being lazy and not going far enough in diagnosing the real problem that each person has, who manifests the tender points.
Absolutely! Not getting to core issues. My first DX was FMS and then came all the other stuff.
Issie
Yes, Philip, what you say makes a lot of sense to me! I think I have myofascial pain/trigger points along w/other symptoms (which are primarily my CFS). Dr. David Brady, who hosted the recent Fibro Fix Summit of alternative practitioners, believes that MANY patients are mis-diagnosed with FMS when they really have other disorders. His book is titled “The Fibro Fix.” I haven’t bought it yet, but after considering your comments, Dr. Brady’s comments and my own thoughts, I’ve decided to get his book. Best of luck as you go forward on your journey! Judith
I also have joint hypermobility. I have POTS, svt, IBS, reflux, TMJ, fibro, chronic fatigue, and I am wanting to get tested for mast cell issues as my allergies are horrible and I cannot tolerate any medications, caffeine or alcohol. My life is pretty dull and scary, now, where I used to be happy and full of energy. I was a ballet dancer and worked out with trainers and ran. Now, I have severe exercise intolerance, but not from a lack of trying! My Drs all day I’m deconditioned, but I’m not! I get very heavy in my body during most workouts that have exertion and I feel like I’m going to fall over. My bp never drops too low, though. Lately, I actually get bp spikes. I’m on 25 mg beta blocker. My loose joints cause severe muscle tightness and pain. Some days are ok and other days are horrible. I’m 41, and my quality of life is poor. I get dizzy a lot and just read that it might be from my loose neck joints. I have several specialists, but I’m just not getting anywhere at this time. I know that strengthening the muscles around my joints is the best thing to do, but when I have exercise intolerance, I get frustrated. I was in physical therapy, but my insurance doesn’t cover it and it was $600 per session! My son has loose joints, and now I’m terrified that he will end up this way. He seems healthy, but so did I until my thirties. We’ve both had heart echoes that show that everything is ok. I have a loop recorder implanted in my chest which shows PVCs PACs and mild infrequent svt. I’m just at a loss here. I need to get my normal life back since I have my son and three stepchildren to raise!
Really hard times Marna!
Has anyone said anything that would help you understand why this popped up in your thirties? Could it be due to an autoimmune problem?
Good luck with everything..
Marna, if there is MCAS – Then beta blockers can trigger more problems. Most of us have to stay away from them. The first thing most of us did when trying to determine if MCAS was an issue is start on H1 and H2 blockers. I use Allegra and 1/2 Zantac. Some have to add an H3 blocker (Singulair) and then add a mast cell stabilizer like GastroCrom or Ketotifen. Until I added GastroCrom, things weren’t as effective. Exercise can trigger a mast cell degranulation and all sorts of problems come with that.
Issie
Great article!!
Having POTS, MCAS and EDS alot of all the above comments – I agree with. I too have diastolic dysfunction. I have found that Gastrocrom which is a mast cell stabilizer and is also a mild calcium channel blocker is of great benefit for me. Helps with not only the MCAS issues but my POTS symptoms too. Having MCAS we are not to use beta blockers as they cause a mast cell degranulation. But for me the help with more Hyper presentation of POTS (Which includes more hyper-blood pressues) that the GastroCrom gives, is of great benefit. I too have autoimmune issues and hypogamaglobulinemia. The GastroCrom seems to help with my autoimmune issues too. For sure there is a circulation issue with me. Having EDS I also have issues with vein function. But…..I’m overly constrcited. Probably due to Lyme and Protomyzoa Rehumatica and the biofilms they cause in my veins. (The vasoconstrictive drugs were some of the worst things I tried.) However, a very light external compression helps. I find more help with abdominal binders than on my legs. But, flying or riding a long time, they are on my legs. Helps with pooling and edema. (Too strong compression caused more neuropathy.)
So great that more docs are looking into our issues. Lots of trial and error. More error than not. But, we are slowly finding answers.
Issie
Judith, thank you for noting the multiplicity of factors that need to put together like a puzzle, necessary not only for understanding the condition but also in treating it.
This multiplicity is an ‘odd’ aberattion for the average medical doctor’s way of thinking and training, and leads to patient condemnation for taking ‘too many’ medications. This so called ‘polypharmacy’ is frowned upon as if it is a sign of an over self conscious or self indulgent mind. Professor Peter Rowe, however, refers to this as ‘rational polypharmacy’, and hence, he and I both see this as no different from the management of other complex disorders such as HIV, Lyme disease, and the like.
Nancy, you are absolutely right – I am indeed referring to Dr L. O. Simpson’s ground breaking work. This highly skilled doctor was a true expert in the field of hemorrheology and it is sad that this field of enquiry has not received continuing attention. I agree with you that this work needs further evaluation.
Sally, as far as TNF-alpha blockers are concerned, the most widely available and cheapest TNF-alpha blocking agent is Vitamin D (and is extremely effective when therapeutic doses are used – eg 600,000 IU of 25 OH Vitamin D intramuscularly in oil by intramuscular injection every 6 months). Therapeutic doses of course mean doses that achieve therapeutic levels, but remember, normal ranges on blood tests can include levels that are sub therapeutic.
Oddly, some of my very sun exposed patients are still Vitamin D deficient despite such excessive Queensland sun exposure (I wonder why – skin disease in ME/CFS? or, a metabolic defect of genetic original?), whilst others are unable to absorb even 50,000 IU when taken orally. This malabsorption may be isolated, or part of a more generalised fat malabsorption from the gut.
The goal of such treatment, of course, is to reduce NFkB (by blocking TNF-alpha), but Vitamin D has an influence on many many other genomic Vitamin D sensitive sites, and so many other good (or bad) effects may perhaps occur. I certainly do not see any signs of hypercalcaemia on such doses. Remember that magnesium homeostasis is also regulated by Vitamin D, and that Magnesium is an ATP cofactor. Total body magnesium levels may be reduced as a consequence of inadequate Vitamin D status and a letter in the Lancet in the mid 1990’s regarding intramuscular Mg was one of the first accepted by the Lancet as a treatment for ME/CFS.
It should be recognised that DHEA also is a TNF-alpha blocker, so expensive new compounds do not necessarily have to replace these natural agents. Medications like these need to be applied when the clinical situation calls for them, and not simply be a blanket treatment for all. The negative responses occurring in some patients to medications such as DHEA can obscure the real benefits experienced by the remainder. Therefore, one needs to know EXACTLY what one is doing and what one is trying to achieve with any given medication, so research studies definitely need to take these issues (treatment goals) into account, so that they do not throw the baby out with the bath water.
Back to topic: the problem of loss of pulmonary blood volume is from poor venous return of blood from the peripheries. The extent of pulmonary arterial, pulmonary venous and pulmonary capillary blood loss may be quite considerable, relatively speaking, and would, besides their effect on cardiac function, have important effects on gas exchange in the lungs and/or lead to the experience of unexplained shortness of breath.
I have wondered if pulmonary blood volume depletion might account for the finding amongst many ME/CFS patients of elevated ACE (Angiotensin Converting Enzyme) levels. Blood ACE is derived only from the pulmonary microcirculation and exist on the luminal surface of pulmonary capillary endothelium, especially those at lung bases. (The high ACE levels in sarcoidosis is due to a completely different mechanism and is not chest blood volume related). The role of TNF-alpha acting on an enzyme called sheddase, that allows the release of membrane bound ACE to be released into the blood, cannot be ruled out. However, increased blood levels of ACE are much more likely to be a consequence of diminished blood flow through pulmonary capillaries in this setting, and are raised in order to affect increased renal sodium absorption through the renin-angiotensin-aldosterone system.
For Issie: Where blood pools in the upright position in any given patient is difficult to say. It is said to amount to only about 500mls of blood not returning to the heart as it should. This ‘small’ amount of not returning blood is nevertheless sufficient to compromise cardiac output. Just as in your case, one patient of mine found tight binding around her abdomen with strapping, added to the benefits of compression leg stockings, and may even have been more important to this patient’s functionality.
The problem with leg bindings is that it does seem to accentuate certain neuropathic symptoms in some people, with can induce more numbness and parasthesia experiences. As the capacitance veins of the legs do not appear to be constricting adequately to prevent venous pooling, apart from the fact that there may also be concurrent Ehrlers Danlos Syndrome in many, a neurogenic or myopathic anomaly affecting the smooth muscle of these vessels, I believe, MUST be present here. I have no idea as to the effects of the compression stockings on these 50 cms long, 1.2 micrometer diameter post ganglionic unmyelinated sympathetic axons that enervate these blood vessels might be, but it would be nice to know. For example, the actually physical volume of these axons could be reduced by such stockings, if they are too tight or worn for too long and this could adversely affect nerve axon function.
Finally, it is clear that a few 15 minute appointments to doctors to talk about these problems is predictably insufficient, given all that needs to be considered and taken into account in each and every patient. Furthermore, given the widespread nature of this complaint, it is clear that more doctors adequately trained in this field, are required. I am not aware of anyone calculating exactly HOW MANY doctors of this kind is needed, but this definitely needs to be done, and presented to relevant medical authorities. It is not enough for patients being more qualified than their doctors in such complexities. It is no wonder that what Health Authorities expected of Dr Bested in Vancouver were so unrealistic.
The above reported research was very invasive, and I commend Dr Systrom and Dr Oldham for their long term commitment to the research they performed. They did not specifically study ME/CFS patients, and were thus able to find the necessary funding for work that otherwise might have been shelved as inappropriate and not given funding, were they to have selected ME/CFS patients to study in particular.
Sincerely,
John
Here may be something to think about as to low Vit D levels. This is just my hypothesis. I did have someone send me a paper that supports it. I’d have to find it.
This is another comment on another thread – I just copied it.
————
Or could low Vit D be a compensatory response of the body? I recently found out I have calcification in soft tissue. I have low Vit D levels. Research says it can be caused by either not using Vit K along with Vit D to keep calcium in the bones or it can be the bodies way of lowering Vit D as a response for too high calcium for whatever cause. Having MCAS (mast cell activation syndrome), I use GastroCrom, one of my best meds for both my MCAS and POTS). It is a very mild calcium channel blocker along with being a mast cell stablizer. Having been trying to up my Vit D with 10,000 a day of Vit D and it barely budging, makes one wonder if my body doesn’t need extra Vit D after all. It could be trying to keep my calcium in check by staying low. I have recently lowered my Vit D and added Vit K a few times a week. Being summer I get in the sun more now. We will see how it goes.
Issie
Issie,
Check this :Low Vitamin D Levels, and Low Blood Vitamin D. There are two reasons for having low vitamin D. If your doctor put you on high doses of vitamin D, then you must know why your vitamin D is low. If your doctor said the words “secondary hyperparathyroidism” to you and put you on high doses of vitamin D because your calcium is not normal then you need to read this page and watch the video.
http://www.parathyroid.com/low-vitamin-d.htm
Thanks Sam, I read this awhile back but didn’t pursue it like I should have. With 10,000 Vit D a day for over a year my levels of D have gone from being in the 20s to 40. You’d think with that much Vit D, I would have reached the goal levels of at least 50. My calcium is 9.5. So on high side. I don’t suppliment calcium and don’t injest things with added calcium. I am mostly Vegan, so whatever there is in fruits and vegetables. I do have to keep a watch on a meningioma and a thyroid tumor so will have them pay closer attention to parathyroid and see if they see anything. Thanks for the link. Something else to check.
Issie
I just had a friend send this to me. Having to low magnesium can cause calcification problems too. Good article here – worth a read.
http://drsircus.com/medicine/magnesium/calcification-and-its-treatment-with-magnesium-and-sodium-thiosulfate
Issie
Issie,
25(OH)D Is Not a Specific Marker of Vitamin D Status according to Chris Masterjohn, Ph.D.
(He is another “source” I closely follow. He now has live facebook podcasts) HIs next one “Ask me anything” is on July 12th. https://www.facebook.com/chrismasterjohn/
I have not read this article yet and can’t comment on it. http://www.westonaprice.org/our-blogs/cmasterjohn/an-ancestral-perspective-on-vitamin-d-status-part-2-why-low-25ohd-could-indicate-a-deficiency-of-calcium-instead-of-vitamin-d/
Also, I think your calcium level is not high.
SAM, I Agree, I’m still within range on calcium. I do however take things to moderate it. Not sure where I’d be without my tweaking. Thanks for all the info. I will look into it more. I love learning.
Whole point of comment, initially, is some of us can’t get our Vit D levels up even with high supplements – there may be a reason for this. Could be a compensatory response or as mentioned an issue with VDR genetic mutations.
Issie
I do, however, also have a VDR genetic mutation.
https://ghr.nlm.nih.gov/gene/VDR
Issie
John L Whiting
Check this out : Low Vitamin D Levels, and Low Blood Vitamin D. There are two reasons for having low vitamin D.
http://www.parathyroid.com/low-vitamin-d.htm
I find this article very interesting. Maybe a new wave of testing for patients with symptoms. If insurance will cover. I have FM four years now. I work and stay pretty active but also have exercise induced dyspnea and exercise intolerance.
Nicotinamide riboside and NMN both improve circulation and cellular energy production. I wonder if they would help in this regard.
Ribose has zero effect on my energy. The same goes for pqq, coq10, ubiquinol, ginseng, b12 and everything else that is out there. That makes me think that something else is going on. May be my cells produce enough energy but something happens after that . I have no clue.
If I understand him right, Bob Naviaux believes that the problem is not that the mitochondria are broken; i.e. that they’re damaged but that something is turning them off. He would agree that none of the mitochondrial enhancers typically tried in ME/CFS are the answer. They might work for classical mitochondrial problems but not for ME/CFS.
Recent research I’ve been doing can point to issues caused by too much glutamate and increased need for heatshock proteins. If there is too much glutamate (can be due to neurotoxins ie. MSG etc) there is a problem with a release of too much calcium and that can trigger death of cells which directly affect mitochondria. I don’t completely understand it – but find it fascinating. I’ve always felt the over response of the autonomic nervous system in POTS has some connection to glutamate and dopamine dysfunction.
Issie
Is anyone aware of any studies on ME cardiopulmonary physiology compared with high altitude physiological challenges? I had ME in 1990 and worked out how to rehabilitate myself back to a normal life over a period of 6 years. When I went to Machu Picchu in 2008 the symptoms I experienced during the 2 days of high altitude adaptation in the city of Cusco was eerily similar to my ME days. Fortunately I was able to adapt and hike around at high altitude with my family. Could ME be a failure or weakness of central processing systems such that patients are stuck struggling to function as if they had climbed half way up Mount Everest. It may not matter what the cause was (infection, trauma, head injury, extreme stress etc) if the end result is a neurological disabilty. If this is the case then working out a rehabilitation treatment program should be the priority of researchers in the field.
I have POTS,since 3 years ago. And with NUUN( electrolytes and salts) added to my water,compression socks and being on my feet as much as I tolerate every singel day have my standing/walking time improved very slowly from 5 min.(3 years ago) to the whole day now. But I need a betablocker to slow down my tachycardia.
If I use Tramadol(50 mg.) for pain have I noticed that I can stand up for longer time without getting dizzy,and my brain fog disappear for a while too.Wonder why..But it is a hug improvement!
I live in Norway..
Hege, for me, Tramadol moderates neurotransmitters and NMDA. Calms down the sympathetic system. Adding Bentyl – a mild muscle relaxer works even better than Tramadol by itself. And then put GastroCrom with it and things stay pretty level. I do use H1 and H2 meds, supplements and other herbals. But for RX meds, those have been my best.
Issie
Here is a good link regarding AV shunts and how the peripheral circulation could readily be severely disrupting central circulation
http://www.livingwithfibromyalgia.ca/interesting-study-finds-possible-cause-of-fibromyalgia/
Regarding brain hypoxia and tolerance, this is an important paper:
Acute and chronic hypoxia: implications for cerebral function and
exercise tolerance
Stuart Goodalla*, Rosie Twomeyb and Markus Amannc
aFaculty of Health and Life Sciences, Northumbria University, Newcastle, UK; bSchool of Sportand Service Management, University of Brighton, Eastbourne, UK; cDepartment of Medicine,University of Utah, Salt Lake City, USA
Purpose: To outline how hypoxia profoundly affects neuronal functionality and thus compromises exercise performance. Methods: Investigations were reviewed and evaluated that used electroencephalography (EEG) and transcranial magnetic stimulation (TMS) to detect neuronal changes at rest and those studying fatiguing effects on whole-body exercise performance in acute (AH) and chronic hypoxia (CH).
That’s interesting. I know I don’t regulate body temp correctly – in either direction.
I do find that MCAS triggers some mighty hot flashes. And MCAS can be triggered by getting over hot.
Thanks for the info. Something to research.
Issie
Really exciting research on Natto kinase to address the CFS/ME and Covid related blood clotting issues with no side effects is very promising. I have started taking 4,000 FU per day of Natto kinase and have seen very quick results in energy and pain and cognition. There are numerous studies published at the NIH and the implications for viral disease, leaky gut, Alzheimers, cardiac care etc. are enormous. I would really like to hear if anyone else with CFS/ME has had positive response from Natto kinase and what dosage was used.