(Marco digs into a controversial subject in this second of two blogs on Stiff Person Syndrome and ME/CFS – “Is the depression/anxiety present in Stiff Person Syndrome and, possibly by reflection, chronic fatigue syndrome (ME/CFS), a consequence of having a difficult disease or is it an inherent part of the illness itself? This debate – what belongs to the mind and what belongs to the body – is being played out in many other diseases, including, of course, ME/CFS. Let’s see what’s happening with it in Stiff Person Syndrome)

Is the depression and anxiety in SPS and ME/CFS a function of the disease itself or simply the result of having a chronic illness?
Are ‘Co-morbid’ Anxiety and Depression An Essential Part of Stiff Person Syndrome ?
Like chronic fatigue syndrome there are questions whether the anxiety (arousal) or depression found in SPS is an inherent part of it or whether they are simply normal reactions to having a chronic illness .
No one believes chronic fatigue syndrome is major depression or generalized anxiety disorder; the question is whether the two, in some places, share some common ground with ME/CFS and if they do, is it due to the illness or the consequences of having a chronic illness?
For instance, while some studies find differences between major depression and ME/CFS (cortisol (Cleare et. al. 1995), EEG (Duffy et. al, 2011), Beta endorphins (Panerai et al,2002), cognitive patterns (Moss-Morris et al, 2001) others have had difficulty separating the two; brain glutathione levels (Shungu et al, 2012) ventricular lactate (Murrough et. al. 2010), cerebral hypoperfusion (MacHale et al, 2000, (motor evoked potentials (Samii 1996), SPECT scans (Schwartz et. al, 1995).
In her Nova Southeastern University (NSU) talk Dr. Hornig noted that some of the same brain structures are found in both ME/CFS and Dr. Maes (Maes et al, 2012) believes a similar inflammatory context underlies both disorders. Significantly increased immune factors in ME/CFS and people with major depression versus controls suggested similar immune processes were at work in both disorders. Significantly higher immune factors in ME/CFS patients vs depressed patients suggested increased immune dysfunction was present in ME/CFS but that immune dysfunction played a role in both (Maes, Mihaylova et al 2012, Maes, Twisk et al,2012).
“ This study has detected a shared ‘pathway phenotype’, i.e. disorders in inflammatory and CMI pathways, which underpins both ME/CFS and depression and, therefore, may explain the co-occurrence of both disorders. “ Maes et al.
Maes, a psychiatrist with a pathophysiological bent, takes the concept even further in another study stating that ‘co-ordinated and interacting biological pathways’ involving pro-inflammatory cytokines, tryptophan and other factors drive the symptoms found in ME/CFS, depression and ‘somatization disorder’. (Anderson et al, 2012).
Maes and Hornig combine both body and mind in their conception of ME/CFS but others do not. In her ME/CFS treatment manual, “Let The Light Shine Through”, Dr. Eleanor Stein, an ME/CFS patient herself, has this to say about the general vibe in the medical community around ME/CFS.
“In spite of the thousands of published peer reviewed papers since the 1980’s reporting abnormal biological findings in ME/CFS, FM and MCS that are different from findings in depression or any other psychiatric disorder, the ‘primary psychiatric’ view continues to have influence. In the absence of valid diagnostic tests, the fallback position seems to be that these conditions are essentially psychological.”
Back to the question SPS researchers are facing. Is the anxiety/depression found in SPS a reaction to the stresses of the disease or are anxiety and depression also manifestations of the underlying autoimmune disease? Maes believes immune findings help explain both chronic fatigue syndrome and depression. What about Stiff Person Syndrome?
Fear of Falling?
Like ME/CFS, SPS appears to be accompanied by high levels of ‘co-morbid’ anxiety and depression which are assumed to arise in response to a much reduced quality of life and the real risk of serious injury (Rodrigues de Cerqueira et al, 2010 – correspondence). It appears that there are frequent anecdotal and case study reports of co-morbid anxiety which may be either a context specific phobia related to movement difficulties or more of a generalised anxiety disorder.
This is hardly surprising given the risk of falling present in this disorder. It also explains why many SPS sufferers are originally diagnosed (sic) as suffering from a psychogenic movement disorder.
Or Low GABA?
The fact that high levels of anxiety/specific phobia correlate with GAD antibody levels and reduced locomotor function (Henningsen and Meinck, 2002) is usually taken as merely indicative of phobic avoidance due to increased morbidity and thus likelihood of injury – e.g. going into spasm while crossing a road.
Anxiety and depression might also be expected with low GABA levels. Indeed, initial misdiagnoses made when there are few objective medical findings suggest that high levels of anxiety may be a result of the underlying pathology and not a maladaptive phobic response to the risk of injury which occurs later in the disease. It bears noting that SPS patients originally misdiagnosed with a ‘kinesiophobia’, do not respond to cognitive therapies, nor do those therapies reduce the anxiety of those correctly diagnosed with SPS. Something else appears to be causing the anxiety….
Enter the GAD antibody/GABA connection…
GAD antibodies in Psychiatry
Experimentally injecting rats with SPS antibodies results in the rats displaying high levels of anxiety like behaviour (Geis et al, 2011). Yarlagadda et al (2007) believe GABAergic neurotransmission issues play a key role in epilepsy, anxiety disorders, schizophrenia, premenstrual dysphoric disorder and bipolar disorder.
Could an autoimmune reaction be contributing to a GABA/Glutamate imbalance in Stiff Person Syndrome?
A small pilot study examining GAD antibody levels in chronic psychotic disorders led them to conclude :
“Antibodies to GAD65 (an isoform of GAD) are peripherally present in patients with chronic psychotic disorders (schizophrenia/schizoaffective disorders) and may potentially be used as a tool to screen for these disorders. The presence of such antibodies also suggests a possible role for autoimmune mechanism in the pathogenesis of these disorders.”
At Dr. Klimas’ recent NSU Conference, Dr. Hornig included these disorders (plus ADHD, Fibromyalgia and ME/CFS) in a list of ‘neuropsychiatric disorders’ that may have immune causes. You may also recognize this list from the discussion of sensory gating deficits in Part I of the Neuroinflammation Seriess: Not Fatigue After All:).
You can parse out the term ‘neuropsychiatric’ in various ways but it bears mentioning that a disorder causing cognitive difficulties can fall into the ‘neuropsychiatric’ camp.
Remember also that we are looking at disorders like schizophrenia in the context of neuroinflammation and a sensory gating disorder and the evidence indicates that sensory gating issues could show up as schizophrenia in one way and fibromyalgia or CFS in another. The fact that similar pathological issues can manifest in very different ways was recently borne out in a study that found that the same genetic makeup could result in vastly different disorders. (Cross-Disorder Group of the Psychiatric Genomics Consortium, 2013). It’s also reflected in the fact that, as discussed in Part I, the same drug can impact a wide range of disorders.
One possible mechanism to explain the attacks of extreme muscle rigidity in SPS involves GABA mediated inhibition from the cortex, brain stem, and cerebellum of motor neurons. If GAD levels are raised, the levels of GABA required to be inhibit it are decreased and the muscles become continuously stimulated by the motor neurons (Rodgers-Neame, Medscape Reference).
Intriguingly, recent research (Cort will be blogging on this soon) suggests that the muscles of those with fibromyalgia also appear to be continuously ‘firing’; ie they’ve become locked in a contracted state. It’s no surprise that fibromyalgia patients often complain of muscle stiffness (Klaver-Król et al, 2012).
Infectious Onset?
The exact aetiology of SPS has yet to be found. However Yarlagadda et al also report that GAD antibodies in diabetes (as previously seen, high rates of metabolic syndrome and diabetes are found in a number of neuroinflammatory conditions) have been associated with entero and coxsackie infection :
“In the context of diabetes, GAD65 antibodies have been associated with an infectious etiology, especially entero and coxsackie viruses. However, GAD65 antibodies interestingly bear a striking similarity with P2-C protein of coxsackie virus suggesting a cross-reactivity and interference with neuronal development.”
An additional single case report (Hassin-Baer et al, 2004) describes the onset of SPS following acute West Nile virus infection and describes a stretch of 12 amino acids in the NS1 protein of West Nile virus with a high degree of homology to the GAD65 region :
“Cross-reactivity between antibodies directed against West Nile virus and GAD may have contributed to the development of stiff-person syndrome in this patient.”
The previously discussed Anti-NMDA receptor encephalitis (an autoimmune encephalitis) has also been associated with Mycoplasma pneumoniae infection (Gable et al, 2009).
Conclusions
An imbalance in the excitatory and inhibitory neurotransmitters glutamate and GABA is implicated in a wide range of neuropsychiatric (ASD, schizophrenia, bipolar disorder, major depressive disorder, OCD etc) and in pain (fibromyalgia, interstitial cystitis, IBS) and movement disorders (Parkinson’s, Huntington’s).
Stiff Person Syndrome is one rare but extreme example of a condition combining a movement disorder with neuropsychiatric symptoms (anxiety, depression) where a glutamate/GABA imbalance is clearly central to the pathology, is likely of autoimmune origin and which may have an infectious etiology.
Current research provides hints that a similar etiology may underlie a range of ‘neuroinflammatory’ conditions including ME/CFS.
C
>







Hi, Marco,
I’m following your posts with great interest. Thanks for going to all the trouble of keeping up with the research and drawing it out for us.
I’m curious about something (that I’m thinking may be obvious to most people, but not to me, so I’m asking): When you mention “GAD antibody levels,” is that antibodies to Generalized Anxiety Disorder? Or does GAD stand for something else in this context? I just didn’t know that there were antibodies to an anxiety disorder. If you can enlighten me, I’d appreciate it.
Thanks again!
Sarah
Hi Sarah
Too many acronyms.
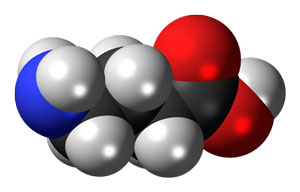
In this case, GAD isn’t referring to generalised anxiety disorder but an enzyme called glutamic acid decarboxylase (GAD) that converts glutamate to GABA and where antibodies to GAD result in low GABA levels.
http://en.wikipedia.org/wiki/Glutamate_decarboxylase
Not that (in my view) the two are not related. If you recall Part II – Glutamate another piece in the puzzle – Baclofen – a GABA promoting drug apparently not only helps cure alcoholism (and is used to treat SPS) but also appears to cure alcoholics of their life long anxiety.
Glad you’re enjoying these posts.
Much more to come where I’ll be hoping to ‘put it all together’!
I just looked up Baclofen…It’s an interesting drug; its a derivative of GABA – the neurotransmitter that regulates neuronal excitation…Interestingly enough it was developed to treat epilepsy and is now used to spastic muscles and as a muscle relaxant in topical creams…plus it’s helpful as Mark mentioned in alcohol withdrawl of all things.
This all sounds pretty good. I wonder why it’s not more used in ME/CFS?
Baclofen is a muscle relaxer and was prescribed to me for spinal stenosis pain.
I’d been taking Zanaflex exclusively, (another muscle relaxer) as it’s been exceptionally helpful to me for a couple of years with a lot of CFS symptoms.
A pain management doctor suggested I take Baclofen during the day, and Zanaflex at night.
I’ve not noticed any special benefit from Baclofen, other than it seems to be a milder muscle relaxer than Zanaflex. Don’t get a ‘dopey’ feeling from it which is a plus, so can drive while taking it. I might try taking higher doses and taking notes and see if I can ascertain any difference with CFS symptoms.
Fascinating information though, I had no knowledge that it was approved in 2012 for use with alcohol withdrawal.
Thanks for this article Cort.
Best,
Questus
Thanks to Marco…..Thanks for the info on Baclofen – I’ll create a resource page for it.
Wow. Ok. Suddenly I need to check out Baclofen. I am super sensitive to meds, don’t metabolize many in anything approximating a normal fashion. So I am at a standstill right now. Its great to have a new idea. Wonder if it would have a synergistic effect with clonazepam. Gotta have my clonazepam. Long story. Iatrongenic injury.
Once I wanted to be a doctor. Gotta be cold as ice to do the stuff they do to people. ( Hope none of you reading
this are physicians, lol..ok, yeah,I really don’t care. Not impressed here. ). lol
Of all Things. I was looking up Baclofen…
Baclofen and Stiff Person Syndrome
Reg Anesth Pain Med. 2013 Mar 20. [Epub ahead of print]
Trialing of Intrathecal Baclofen Therapy for Refractory Stiff-Person Syndrome.
Newton JC, Harned ME, Sloan PA, Salles SS.
OBJECTIVE:
Stiff-person syndrome (SPS) is a rare disorder of the central nervous system characterized by stiffness and muscle spasms that may be progressive in nature. When oral medication is inadequate to control muscle spasticity, intrathecal baclofen may be used. We report a patient with severe SPS and glutamate decarboxylase negative [GAD(-)] (note: GAD(-) indicates the patient has no antibodies to GAD), refractory to oral standard therapies. The patient was effectively trialed with an intrathecal catheter and subsequently treated with chronic intrathecal baclofen, which provided significant relief of spasticity symptoms.
CASE REPORT:
A 48-year-old white man with a history consistent with SPS presented to the clinic. His previous history showed that he met several diagnostic criteria for GAD(-) SPS and had a muscle biopsy positive for myositis. Oral medications were unable to control his muscle spasticity, preventing him from working. The patient received an intrathecal trial using a lumbar approach for placement of a thoracic catheter with an initial baclofen dose of 50 μg/d. Gradual titration to symptom relief was performed up to 150 μg/d. Functional evaluation by our physical therapist showed improved motor function, the temporary catheter was removed, and a permanent intrathecal pump placed for intrathecal baclofen infusion. The patient reported excellent symptom relief over the next 6 months and improved activity.
CONCLUSIONS:
Refractory SPS is difficult to treat and has few therapeutic options. We report a GAD(-) patient with SPS and resulting debilitating spasticity that was refractory to oral medications who underwent successful continuous intrathecal catheter trial of baclofen over 4 days and subsequently went on to implantation of intrathecal pump.
Plus
In a rodent study focusing on IBS Baclofen is effective pain reducer
Scand J Gastroenterol. 2011 Jun;46(6):652-62. doi: 10.3109/00365521.2011.560677. Epub 2011 Mar 28.
Oral baclofen reduces visceral pain-related pseudo-affective responses to colorectal distension in rats: relation between plasma exposure and efficacy.
Lindström E, Brusberg M, Ravnefjord A, Kakol-Palm D, Påhlman I, Novén A, Larsson H, Martinez V.
Source
AstraZeneca R&D, Mölndal, Sweden. Erik.Lindstrom@medivir.se
Abstract
OBJECTIVE:
We previously showed that activation of GABA(B) receptors by intravenous baclofen reduces pseudo-affective responses to colorectal distension in rats. Here we evaluate the potential clinical significance of these observations.
MATERIAL AND METHODS:
Clinically relevant colorectal distension protocols were used to assess the effects of oral baclofen on visceromotor and autonomic cardiovascular responses in conscious rats.
CONCLUSIONS:
Oral baclofen, at plasma levels similar to those reported safe and within a therapeutic range in humans, produced significant visceral anti-nociceptive effects in rats.
I just want to add a note of caution that Baclofen is a prescription drug and self-medication or experimenting with dosage is definitely NOT a good idea.
Bear in mind that this is all hypothetical and as discussed in Part II – GABAergic drugs including benzodiazepines and alcohol can lead to neurological kindling – not a good thing if ME/CFS already involves kindling.
Also in SPS Baclofen pump failure can have very serious consequences.
Definitely worth considering in a research context though!
What a pity that symptoms continue to be studied instead of causes. If a person has the genetics (HLA DR) then chronic toxic mold exposure in water damaged buildings will set the immune system on a path of releasing inflammatory cytokines which wreak all kinds of havoc in the immune system, resulting in a plethora of malfunctions that will present as many classes of “disorders.” Minutely studying the consequences of mold exposure in the susceptible is a silly way to proceed when simple removal of exposure would alleviate the majority of the symptoms, allowing the needed action (extreme avoidance) to take place. However, removal is rarely “simple” because it is so incredibly difficult to achieve, with the sufferers who figure it out often needing to live outside of buildings altogether. However, a life of wellness lived outdoors is infinitely preferable to a life of chronic illness lived indoors.
Depression, anxiety etc inherent in the illness – rather caused by I suggest Marco from personal experience. Much in the same way “fatigue” has been applied to ME. We know it is not “fatigue” as commonly used. In the same way depression (a loose description if ever there was). I do not recall depression as a part of ME (OK so fed up now and again) but clinical – bod functioning at disasterously low levels including endocrine dysfunction and autonomic NS. Actually the “black holes” experienced early on which lead to passings out were clearly not due to being “depressed” about my illness – I recall being very proactive with my Docs. I a similar way I think “anxiety” – loose one too was very related to a situation we describe as “wired and tired” as if the adrenals have suddenly jumped in for no apparent reason, well there weren’t functioning before it seems.
Hi Enid
As per my biography I did experience depression which I do believe is part and parcel of ‘my’ ME/CFS as is the anxiety I still experience.
But, as will become clear later, I don’t expect us all to experience the same mix of symptoms – quite the opposite.
But I would expect that the ‘symptoms’ of depression and anxiety are likely to be part and parcel of most neurological disorders. The problem is that these symptoms are either explained as separate ‘co-morbid’ conditions (what’s the likelihood that you would simultaneously develop two or more completely unrelated conditions) or that ME/CFS is a ‘type of’ depression or anxiety.
Next up I’m hoping to give a fuller explanation of how this neuroinflammatory model can account for all of our symptoms.
I must add a very good experience with Gabapentin (added to another HR article), when in such pain and sleepless. Levels up to Epilepsy dosage over a short period of time (mostly sleeping) relieved sleep, pain and being constantly “wired”.
I also had to take Gabapentin when I was living in my water-damaged house with hidden toxic mold. After I got out of the house and into a mold-free environment, I no longer needed the Gabapentin. 20 doctors over 10 years did not diagnose the cause of my problems; all they did was offer drugs and shrugs.
I have tried reading through this article but my brain wont engage. 🙁
I at one time wondered whether have SPS. I have a very bad startle reflex plus myoclonic like movements that look like I’ve been startled when I haven’t. I had posted a number of videos on youtube, including ones of me having these movements. Added to that the muscles in my leg become very stiff after walking short distances. Someone who suffered from SPS contacted me via Youtube http://www.youtube.com/kaazoom saying my symptoms looked a lot like theirs. I had my GAD antibodies checked but they were normal. I have since gone on to develop type 2 diabetes.
One thing I found out about SPS when I was looking into it is there are a number of subtypes. Some people have a type that is primary myoclonic type movements, others only have part of their body affected.
I did meet one person online who had originally had a ME/CFS diagnosis who eventually was diagnosed with SPS, so there does seem to be some similarities
Thanks for the comments Paul.
I wasn’t suggesting ME/CFS folks have SPS but I used SPS as an extreme example of how a GABA/glut imbalance can cause both ‘psychiatric’ symptoms plus severe physical ones.
Having said that, there may be a similar underlying etiology and I’ve seen a few comments that suggest PWME/CFS have ‘marginal’ GAD65 levels when tested.
Interesting reaction you had with benzos (despite the side effects etc you are aware of). You may be interested that a new drug Arbaclofen is currently being trialed for ASD with claimed much better efficacy and reduced side effects.
Type II diabetes does seem to go with the territory as outlined in part II of this blog :
http://www.cortjohnson.org/blog/2013/02/15/glutamate-one-more-piece-in-the-chronic-fatigue-syndrome-mecfs-puzzle-the-neuroinflammatory-series-pt-ii/