



The evidence for central nervous system dysfunction in fibromyalgia is clear: the ascending pain producing pathways are overly activated, while the descending pain inhibitory pathways are under-activated. This results is people with fibromyalgia experiencing pain where no injury or sign of damage exists.
Problems with the peripheral nervous system in the body also exist. The nerve fibers that carry pain signals to the brain are overly activated, and some of the small, unmyelinated nerves in the skin and the eyes that carry sensory information to the spinal cord and brain are damaged in some patients.
The question researchers have been grappling with is whether these damaged nerves are contributing to the pain in fibromyalgia or if they are some sort of side process. The small nerve fiber damage in fibromyalgia is occurring in two ways; first, the small nerve fibers are disappearing, and those that are left are smaller in diameter than usual. The second issue is unusual, and has led researchers to call the small nerve problems in fibromyalgia “small nerve pathology” instead of “small fiber neuropathy”.
The types of symptoms seen in FM may signal differences as well. People with small fiber neuropathy typically experience one kind of symptom while people with neuropathic pain experience another and people with large fiber neuropathy experience yet another kind of symptom.
The Study
Cornea nerve fiber quantification and construction of phenotypes in patients with fibromyalgia. Linda Oudejans1, Xuan He1, Marieke Niesters1, Albert Dahan1, Michael Brines2 & Monique van Velzen1. Scientific Reports | 6:23573 | DOI: 10.1038/srep23573
This study examined the small nerve fibers found in the cornea of the eye, and did extensive pain testing to determine if the small fiber loss in the eye was correlated with pain levels elsewhere.
Pain Tests
The pain tests examined whether FM patients were more sensitive to cold and heat, mechanically induced pain, vibration and pressure, and in the wind-up test, to see if when a painful stimulus was applied (a pin-prick) their pain sensitivity increased over time. Some of these tests were used to determine if “central sensitization” (cold pain threshold, mechanical pain threshold, mechanical pain sensitivity, allodynia and/or windup) was present.
Pain and Stimulus-Response Questionnaires
Pain questionnaires were also given that determined whether symptoms were associated with neuropathic pain (Pain Detect) or small nerve fiber pain (Small Nerve Fiber Screening List (SFNSL)).
Typical indications of neuropathic and small nerve fiber pain include burning and prickling pains (neuropathic) and indigestion, dry eyes, allodynia, tingling sensations, chest pain and others (SNF).
There was no control group: the corneal fiber results were compared to referenced norms.
Results
Corneal Nerve Problems……Check!
The nerve fibers in the corneas of the fibromyalgia patients’ eyes were shorter than normal in 44% of the patients, and nerve fiber density and branching was reduced in 10% and 20% of the patients, respectively. All told, just over 50% of the FM patients displayed one or more indications of small fiber pathology.
Quantitative Sensory Testing (QST)
The QST testing involved exposing FM patients to things like cold, heat, pressure, and pin-pricks. The results indicated that many patients showed signs of allodynia or increased pain sensitivity in one or more tests. In particular, FM patients showed a marked sensitivity to pressure tests.
Allodynia and Increased Sensitivity to Pain (% experiencing) – these tests measured the response to a painful stimuli.
- Mechanical pain – 21%
- WInd-up (increased pain sensitivity as the duration of the pain stimulus increases) – 26%
- Pressure – 69%
Sensitivity to Stimuli – these tests simply introduced a stimuli and then determined at which point FM patients noticed that stimuli. They found that a significant percentage of FM patients were less able to detect some stimuli than normal. This would make sense if they had fewer small nerves in their skin.
Decreased Sensitivity to Stimuli (% experiencing)
- Cold (loss of function) – 38%
- Warm (loss of function) – 21%
- Mechanical (loss of function) – 23%
- Paradoxical heat sensations (loss of function) – 23%
- Vibration (loss of function) – 67%
Increased Sensitivity to Stimuli – a few FM patients, on the other hand, were more sensitive to an allodynia test which measured if they could feel the slightest stimuli.
- Dynamic mechanical allodynia (gain of function) – 13%
Small Nerve Fiber Loss and Pain
The cornea testing found evidence of small fiber pathology in 51% of patients, and Small Nerve Fiber Screening List (SNFSL) questionnaires suggested that a small nerve pathology was highly likely in 56% of patients. The loss of small nerve fibers in the cornea of the eye was not, however, associated with pain levels in general, symptoms overall, or problems with central sensitization.
This suggests that the amount of pain the small fiber problems are causing is probably minimal compared to the other types of pain found in FM.
Different Flavors of Fibromyalgia
The QTEST detected intriguing patterns. Many people with FM experienced more pain than usual when confronted with a painful sensation, but a significant number of patients were less likely than normal to feel other kinds of sensations. Most notably, many FM patients exhibited a reduced ability to detect vibration. The reduced ability to detect all sorts of stimuli (most prominently vibration) found in a subset of FM patients, however, points to the presence of large fiber neuropathy.
A subgroup analysis suggested that fibromyalgia comes in all sorts of different flavors. For example, it indicated that “central sensitization” is not necessary to have in order to be in considerable pain.
- One group of FM patients exhibited neither small fiber problems nor evidence of central sensitization. Their pain apparently derives from central nervous system dysfunction without the added layer of central sensitization. These patients did not, for instance, exhibit “wind-up” – a process taking place at the spinal cord, where repeated pain signals result in increased pain sensitivity. Nor were they more sensitive to pain evoked by cold, heat or pressure. These patients’ pain presumably derives from central nervous system processes that keep them in pain but do not render them more sensitive to outside painful stimuli; i.e. knocking one’s elbow or something does not cause them unusual amounts of pain.
- Another group that had the worst of all worlds had small nerve fiber problems, central nervous system dysfunction and central sensitization; they were more sensitive to painful stimuli, may have had allodynia, experienced sensations associated with small fiber problems, and also experienced ongoing central nervous system induced pain.
- Another group with small fiber pathology and no central sensitization probably experience pain symptoms related to their small fiber problems but do not experience increased pain when they knock something or injure themselves slightly.
- Another group with no small fiber pathology and central sensitization probably don’t have small fiber symptoms but probably experience increased levels of pain when they have a small injury.
If the authors had added neuropathic pain to the mix, more combinations would have sprung up.
This study, then, suggests that fibromyalgia is not a pain disorder but is a collection of pain disorders perhaps overlain by a common central nervous system dysfunction. This dysfunction, they suggested, probably causes problems with pain in general, as well as fatigue, sleep, anxiety and cognitive problems in FM and in diseases like chronic fatigue syndrome (ME/CFS).
Different FM patients also experience pain associated with a) central sensitization produced at the spinal cord level, b) peripheral neuropathic problems, c) small nerve pathology and/or d) large nerve pathology.
Promising Drug on the Horizon?
FM patients with small nerve pathology might benefit from immune agents, while those without small nerve problems might benefit from central nervous system acting drugs such as Lyrica. The authors noted that a drug they’ve used with success in patients with sarcoidosis and small fiber neuropathy called ARA 290 which restores peripheral nerve architecture could be helpful in FM patients with peripheral nerve problems. ARA 290 is the first drug focused totally on small fiber neuropathy.
A new class of drug, ARA 290 activates “innate repair receptors” and turns off cytokines, protects tissues in inflammatory environments from damage, and even promotes small nerve fiber repair. It may be able to help with both the pain and autonomic symptoms associated with SFN. In laboratory studies it’s been able to reduce microglia activity, neuropathic pain, and allodynia. It’s been given fast-track status for the treatment of SFN associated with sarcoidosis. The orphan drug designation it recently received for the treatment of sarcoidosis should reduce the cost of Phase III trials.
Despite the finding that small nerve pathology does not increase central sensitization, the authors acknowledged that it’s still possible that an ongoing stream of pain signals emanating from the body to the brain is responsible for, or contributes to, the central nervous system problems found.
In the meantime FM just got a bit more complex. It’s clearly a central pain disorder than can collect other types of pain disorders as well. Determining what kinds of pain you experience could give you a shot at finding better treatments.







I’ve been tested for SFN by Dr. Englander at MGH and am positive for SFN. I don’t quite get the difference between neuropathy and pathology. And I definitely have symptoms related to CNS. I have other symptoms which other folks don’t seem to have, exercise exhaustion, which is best described by a feeling that oxygen is not being delivered to the muscles. The heart races far beyond normal exertion level, and the muscles feel starved and burning. I attend an FM support group and haven’t heard anyone complain of those symptoms.
It’s pretty subtle really, in neuropathy they just disappear I think, in pathology they both disappear and they get smaller in diameter.
You really sound ME/CFS’ey to me. I have the same symptoms. I get the muscles feeling starved and burning feeling with too much exercise. In fact, those are really key symptoms for me. I had thought they were small nerve fiber symptoms but now I’m thinking they may be more neuropathic pain symptoms. I must confess I don’t know the difference between the two – both after all involve the nerves but I guess in different ways…(???)
Lynn,
This Sancar, have you had relief from your SFN from Dr. Englander’s proocol? I was diagnosed with SFN at Cleveland Clinic in 2010. Not treatment protocol. I’ve just b come worse and worse.
Thank you,
I had seen rheumatologists and neurologists prior to Dr. Englander and the SFN biopsy. My pain was effectively addressed prior to seeing her, by medication. Amitripilene helped alot. Also sleep was impossible, for years, and imo contributed greatly to developing FM. So I’m on several meds now to treat pain and help sleep. All those years without any sleep, my system was on overdrive and could no longer kick down ever. Now I take nortripilene 60 mg., Gabapentin 400 mg., hydrocloroquine 200 mg., LDN 4.5 mg, and for tyroid 2.25 gr. It’s a lot of medication, though not high doses, and really has given me a semblance of my life back. Different things work for some, not for others. Trial and error, but I don’t believe my symptoms could be addressed in a homeopathic way. So I am grateful for the meds.
Is it possible some of the symptoms you describe are from other disorders entirely? While it’s common for doctors and patients alike to attribute all symptoms on fibro, that isn’t a fair representation of the syndrome and self reports by patients of uncommon symptoms in correlation to the syndrome are misleading.
What makes fibro a syndrome (at this time, I’m not saying it isn’t also a disease) is the characteristics that have been repeated and observed and correlated to one another in a pattern. That is not to say we don’t experience these symptoms, just that there is a tendancy for people to blame a new or long term symptom on the one diagnosis they have.
If you are encountering a symptom and a specialist has “never heard of that” it isn’t because its necessarily a rare presentation of a symptom within a disorder, but it could instead be a symptom of another problem or a stand alone feature. Exercise intolerance/orthostatic intolerance are common in ME/CFS and POTS/dysautonomia, but probably occur in other disorders and I have heard others with fibro describe similar issues. I certainly have this symptom but correlate it to my ME/CFS.
The heart also could be caused by POTS/dysautonomia. Unfortunately, ME/CFS and POTS/dysautonomia appear to have very few specialists or doctors interested in learning about them for practice because they fully believe these are rare illnesses.
Well even if you do not qualify clinically for a diagnosis, treatments used can still help you so it may benefit you to try to get to the bottom of these symptoms not attributing them to any one cause until you’ve had the chance to see other docs and tests about them. Illness/symptom complacency and false attribution are what lands many people with cancer for example diagnosed with fibro to not get treatment or explore it as soon as they could or should- this isn’t really their fault the pain seems normal to them or they are used to being shrugged off.
But doctors are complicent in allowing things to slip by because a fibro diagnosis popped up at some point. I imagine this will become a major health crisis in the coming years unless attention is paid to this very issue.
Thanks for your thoughts. I used ‘exercise’ but just climbing a couple sets of stairs on some days is near impossible due to the stress on the muscles. While I can use the crosstrainer for 20 minutes w/o a problem. So hopefully not heart-related. It’s bursts of activity. And there are no relapse effects or backlash other than the pain/intolerance at the time. I don’t expect to go to the gym and workout like I used to 😉 It’s just small tasks in everyday life, like carrying laundry up and down stairs.
Yes, I have wondered for a while whether the standard test for “FM”, merely confirms the existence of one particular symptom that is actually common to several different underlying conditions. That is, you have X number of especially tender and painful points around your body. There are so many hypotheses about what FM “is” or what “causes” it – what if all the hypotheses are correct and there are in fact several different underlying problems that all have one common symptom, the tender and painful points?
Toxic element poisoning could cause this symptom; infections could cause it; Ehlers Danlos Syndrome is known to cause it; Myofascia dysfunction syndrome certainly causes it.
By constantly trying to find “a cure for fibromyalgia”, the medical system seems to be dodging the need to diagnose underlying problem conditions like infections, toxic element poisoning, thyroid problems, sleep apnoea, etc. This is like having “a cure for headaches” – aspirin – and never bothering to diagnose when it is a brain tumour causing it.
“…This study, then, suggests that fibromyalgia is not a pain disorder but is a collection of pain disorders perhaps overlain by a common central nervous system dysfunction…”
And I still believe that there IS a “physical” cause – muscles being in a permanent state of at least partial tension, which is the case with most people with FM, is an obvious cause of real pain, and if there is CNS dysfunction, why assume that this preceded, and was the cause of, “pain” that therefore might not be “real”?
Maybe there is some subset of people diagnosed with FM, who do not have the permanently tense muscles (itself usually accompanied by myofascia dysfunction); it is glaringly obvious that the underlying cause is different for these contrasting groups. A “cause” and a “cure” is extremely unlikely to be found in “the same place” for both or all.
Lynne Thompson.. you are not alone in your symptoms of exercise exhaustion.
Not only do I experience extreme fatigue I also experience extreme pain after doing most anything. My symptoms are heavy,weak,burning painful muscles for doing the slightest normal activity. Yet, there are times these very same symptoms are not present at the same time for the same level el of activity. It’s very frustrating since I can do something on each day yet do the same at another time and I experience flare which last week’s or months.
I think that means there’s hope….just very ill-defined hope.
I notice that burning painful muscles also come when I’m stressed or working hard mentally – the acting of working hard and concentrating seems to cause them to go into contraction mode.
“I notice that burning painful muscles also come when I’m stressed or working hard mentally – the acting of working hard and concentrating seems to cause them to go into contraction mode.”
-> This year I improved a lot upon my observations. I detected that I have 3 phases off FM pain currently:
Fase 1: overtiring my brains; can be exercising, reading to long, watching TV, talk with multiple persons simultaneously. Trying to do any 2 things simultaneously works “like a charm”. When my brains go to jelly quickly, I get near instant contraction in my legs. Most often, it is only part of a muscle (like for example the upper half calf muscle) and more than once it is asymmetric (for example combining previous example with lower half of thigh muscle). When exercising only my arms, it still is my legs that are victims.
Fase 2: happens if fase 1 happened too long or too strong like for example 5 times fase 1 in 2 weeks. I get cold and sore rheuma like pain. Part of some muscles are very hard like concrete.
Fase 3: happens if I reduce physical stress a lot and a long time when in fase 2 and do not overexert my brain. The muscles get warm/hot, feel acid and burning. That is the healing inflammation fase with me. After it, things get better.
The 3 fases appeared in this exact order time and again since I noticed this first about 4 months ago. Note: I could notice this only after very strict pacing so that pain levels decreased for prolonged periods. Before I noticed parts of this, but the 3 fases sometimes existed concurrently in the same or other muscles making clear observations near impossible.
When I have jumping to bubbling “things” in my muscles like frogs or little imploding cavities kind of jerky feeling, that is actually a healing sign to me. Before, I thought it was a bad spasm thing, but I noticed for about nearly half a year it helps pain retracting AND it goes hand in hand with my brain relaxing so I happily allow it now. It’s like Champagne: the smaller the bubbles, the better the effect.
All that lets me believe: this type of FM is for me in fact pure ME/CFS. In line with my thoughts that much of our symptoms are side effects of our bodies trying to protect/heal ourselves, I believe it is a “over-exertion-prevention” mechanism. It sometimes contracts part of my muscles so hard I can barely contract that part any further. This makes it near impossible to move or stand (so I go lie down). Making only parts of a single muscle contract makes it very hard to adjust to it and still go on. Making it asymmetrical makes it even harder and makes keeping balanced a real challenge. I call it my “leg clamp” referring to a wheel clamp on a car: inhibits any will to move. As such, it does not only reduce muscular effort to movement but also more importantly it reduces the very high computational effort movement costs (letting a robot go up the stairs smoothly is near impossible due to complexity) and it nearly forces me to lie down. I see clamping only some parts of my muscles as reducing the cost of this “strong-stop-advice” compared to fully clamping all muscles.
My situation sounds very much like yours, Lynne. A times my brain would feel like it was shutting down, and my weakness and disorientation seemed overwhelming along with bursts of tachycardia. In the last two weeks, however, I have been started on a calcium channel blocker (Diltiazem, 120 mg. ER) and it has definitely helped my brain!
Thanks for passing that on Gary :). That’s an interesting drug. I guess they gave this to you for the arrhythmia and its helped your weakness as well?
Diltiazem is a nondihydropyridines calcium channel blocker used in the treatment of hypertension, angina pectoris, and some types of arrhythmia. It relaxes the smooth muscles in the walls of arteries, which opens the arteries, allows blood to flow more easily, and lowers blood pressure. Additionally, it lowers blood pressure by acting on the heart itself to reduce the rate, strength, and conduction speed of each beat.
I have along with fms and me/cfs ADD. I have thoght for a long time that trying to focus and concentrate on something contributed greatly to my muscle fatigue.
Gary and Cort – Thanks for your reply and explanation. Very interesting.
When I was tested over 20 years ago, they said that when I exercise, my body only produces the amount of oxygen that most people get when they are resting. The term is hypoxia.
Ouch!
Laura – Thank you, I’ll check out more info on hypoxia. That’s exactly how it feels – during exertion, the muscles literally feel like they’re starving.
Exactly how I describe it…. just like there’s a lack of oxygen getting thru to my muscles. Very similar to when I used to exercise a lot & how that made my body feel. Overdid the rowing once & literally couldn’t stand up afterward as my legs just gave out, just like what happens to runners!
Sorry to hear from others that you have similar symptoms; however, it’s good to be validated since I haven’t heard this complaint from other FM sufferers.
Same problem here, either terrible burning or just weakness and risk of falling after just walking up stairs or for no reason. I use a cane like reported 25% of FM sufferers.
I just wanted to let you know that I also get that type of exercise fatigue so you are not alone, but you’re the first person I know of that feels it too.
Hi I do feel the same, especially the muscle burning feeling that gives me a lot of pain, not to talk about my heart rate
Court,
As usual, Thank you for presenting this information. It explains a lot about the “chronic” sistemic pain suffers with Fibromyalgia/ME/CFS suffer with. No report or update on current medications and or therapy for those suffering right now?
Sancar
Thanks. I plan to look at what’s going on in clinical trials sometime over the next couple of months. FM may not be getting a lot of research but efforts are certainly being made to produce treatments for chronic pain….It should be interesting.
You might check out this though on some FM drugs under way – Top Fibromyalgia Drug Tanks: One Down – Four Other Drugs On the Way
I’ve never had tests performed beyond the silly fibro point test (which I have discovered actually is typically done wrong more than it is done correctly! And I say silly because the test is really pittiable compared to other tests for diagnoses- not because our pain and symptoms are silly.) for any of my pain, except one time they let me get a chest xray. Well I’m fairly sure I will turn up positive if I am ever given a SFN test (they take punch biopsies typically of your muscles don’t they?)
It’s hard to get a typical doctor to prescribe such a test though since so much of the data on it is fairly small (under 100) controls/patients involved last I looked. Still the symptoms seem more complex than otherwise and I have many of the described types of pain related to multiple sources.
In expanding on the “fibro syndrome” view- this actually makes sense. In the syndrome view a syndrome is simply an observed set of traits, symptoms, characteristics, and test results with no known specific pinpointed cause(s) yet. (Fibro in this case fits the medical, non-genetic syndrome definition.) It makes sense when no one cause is found and your only clues for the condition you are researching are a collection of related symptoms that the chances the cause will be one specific thing versus many things overlaping are nearly equal (depending on presentation). I’m not doctor or researcher of course, but that’s just my common 2 cents.
Yes its just a quick punch test. I went to Dr. Oaklander because she was pioneering studies in SFN. While I never met Dr. O, her research assistant, when I requested a script for LDN, willingly gave it to me – so for that reason alone it was worthwhile! I don’t have a diagnosis of Fibro, so the SFN was appealing just to firmly document my problems are not psychosomatic.
My experience is very similar. I was diagnosed with FM more than 20 years ago with that simple tender-point test.
I do have a thyroid gland with part of it lost to a cancer a few years before that, and thyroid issues are one potential contributor to having “FM”. Yet I cannot get a full panel thyroid function test done. They do the quick cheap one and say it is enough if that shows “normal”.
I also discovered years later via Hair Mineral Analysis testing, that I have pathological levels of cadmium in my system, which is another obvious possible cause of the FM symptoms. But mainstream medicine is absolutely not bothering to look for toxic element imbalances in FM sufferers.
I’ve had the same experience. The doc never wants to run the full panel. WE don’t need it Philip because we’re ‘normal’. The thyroid is definitely a player in the bigger picture…
I too have been diagnosed with SFN. This brings me back to the genetic SNPs. My theory is that since a lot of us have methylation SNPs (e.g. MTHFR etc) we have a virtual B12 deficiency. Low B12 is a cause of neuropathy. Our levels are in the normal range but the B12 is unable to function at full capacity because of the SNPs and the “folate” problems.The active form of folate must be able to interact with the B12 so that B12 can function. Maybe others have said this, but I’m unaware. That’s my 2 cents.
Regarding B12 and Folate. I was tested positive for both gene mutations of MTHFR. I’ve been fortunate to have avalibity to B12 shot for 30 years. Now since I found out that I also have MTHFR I take a supplement for Folate. I’m not sure it’s working. I’ve not found any solid information regarding the taking of Folate suppilments that will attualy help with the problem of methylation deficiency. I’ve modified my diet even more so.
Has anyone had any success with this problem?
Grateful for any information regarding this probematic condition. Thank you~
The complexity of this disorder is discouraging. Every pain I’ve experienced, as disparate, widespread, and weird as they are, except an acute injury has proven to be FM. From your description, I have ” the worst of all worlds”, which makes sense since every treatment thus far has failed. A new pain management specialist this week wants me to try Baclofen or Methadone as Tramadol stopped doing whatever months ago.Today I took a carefully dosed but probably incorrectly compounded commercial 1:1 cbd/THC edible, I thought 10 mg of each, legal in my state, finally available. This was my third dosing attempt with these, very carefully weighed and calculated by me from enclosed analyses, but first dose was ineffective, followed by second and also today’s horrible couch lock experience for many hours but with 70% less pain. Bad trade off, need more consistent edible composition.
Porsha wrote
“I have nerve pain .Back and neck pain .All over pain , migraines,Ibs..”
I too have horible “pain all over”. The constant head pain 24/7 along with relentless tinnitus is maddening. I also have tremors and shake badly at times. CTS as well. I’ve not found any relief for it. I have not been able to see a specialist. I live in Idaho. Doctors here, (I’ve been to 20+) will not accept the disease or treat it. Only ‘popular drugs, Lyrica, Cymbalta, Gabapentine. All good drugs, “if” they work for you. Unfortunately none of those drugs have. I just suffer. I’ve been on my sofa, home bound for 2 years. When I do have a better day and can push myself I take my mutts for a short walk. It makes me feel good while walking. However as many of you say, I pay dearly for it afterward.
I used to walk 2 miles a day:( I miss that and exercise so much…
“I also have tremors and shake badly at times.”
-> Do you keep track of your body temperature, especially in the morning? My shaking and tremors went together with very low body temperature. Trying to get body temperature up by doing a lot of small warm-ups, drinking hot drinks and using IR triggered hot burning inflammation like pain, so that didn’t work for me.
When I did a small (less than a minute) warm up after getting out of bed and before “exercising”, it improved. I believe that getting my temperature up all day has undesirable effects to my body, but moving with cold muscle is bad too. So warming up only before moving does get the best of both worlds for me.
Anytime there is a questionnaire to fill out describing the symptoms I feel like it is not going to be an accurate description. I have had fibromyalgia since I was about 3 – of course we didn’t know what it was then. I am 58 now. What I would describe as a pain of 8 now is probably a 5 now. I have been shown as it gets worse that I can handle more pain. One day I can get a big beautiful hug from my grandson that literally puts me to my knees and the next day the same hug barely hurts. I just don’t know how you can get accurate study findings when things change so much so fast. I am convinced it is dietary some how. I would love to see someone go on a complete fast for about a week and then eat only purified water and food grown with pesticides, etc, grass fed meat, etc. Then after a year see how they feel. See if the pain is gone. Maybe some day I will try this – if you knew me you’d know what a joke that is!
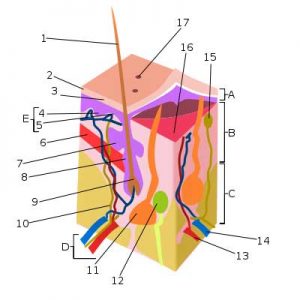
I have some serious fibrofog going on ATM. Am I missing the description that identifies the numbered areas on the picture at the beginning? And it doesn’t show in the pdf for printing. I am having a host of new neurologic issues on top of EMG/NCS confirmed bilateral chronic L5 radiculopathy which predates any nerve root impingement in my back. Now have hypersenstivity type peripheral neuropathy symptoms in a stocking pattern in both feet and legs almost up to my knees. And I think I may have had a small stroke in the last 6 weeks. WAy to compliated to go into but smile is asymmetrical and tongue deviates to right. See neurologist on Oct 27. THanks for your help. LOts of info to digest. I appreciate it and hope my docs do as well.
Excellent thread on FM subtypes. I am trying yo get a clearer understanding of my “type” or suggestions from others about other tests for possible conditions that may be happening?
My symptoms include spasms..in gut..neck, back..which are brought on by cold air. Sometimes gut spasms then the back and ribs follow. I cannot exercise with free weights anymore. If I overexert with activity I feel very sore after and I experience hyperacusis…and my nervous system goes haywire..much anxiety. I cannot do yoga anymore either. The day after exertion I feel fatigue and brain fog. Some depression at those times. I felt like I had no oxygen getting to my brain. Also very dry eyes, tired vision and dry mouth.
Interesting find: Live blood cell analysis indicated much fibrin accumulation and cells were clumping together. Naturopath tried giving me serrapeptase enzymes. Fatigue disappeared and brain fog lifted. I also use fish oils. I included pregnenolone for low testosterone which slso helps brain fog but spasms still come.
Do any of you experience this combo of symptoms? I was diagnosed with FM last year and SSRI’S just make me zombie like. Benzodiazepenes help settle nervous jumpiness, antispasmodic herbal teas..castor oil packs on gut help…codeine helps somewhat for migratory pain.
Is this a type of fibro or done thing else? Any suggestions would be most appreciated.
Thank you