



Background

Shoulder, neck and head pain are common in fibromyalgia and chronic fatigue syndrome. Could the autonomic nervous system be to blame?
I’ve suffered from upper body pain since I came down with ME/CFS/FM decades ago. I can draw a fairly distinct line from about the middle of my sternum upwards; press a point anywhere above that line and there’s a good chance it’s going to cause pain.
Shoulder, neck and head pain are common in both fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS); in fact, the pain in FM often first shows up in the shoulder, neck and head areas. Dr. Lapp has found that ‘pain, spasms and shortening of the muscles’ in these areas often leads to poor posture, rounded shoulder and shallow breathing in chronic fatigue syndrome and tension headaches may occur in as many 80% of ME/CFS patients.
Myofascial trigger points which trigger local and referred pain are most common in the back, shoulder and neck areas of people with fibromyalgia. If you’re going to try and find a cause of pain in FM and ME/CFS, it’s a good place to start.
The Study
In this study muscle activity, heart rate and heart rate variability were measured during a relaxation period, during isometric stretching, during several mental stress tests (including counting backwards) and when inhaling and then holding ones breath (a sympathetic nervous system enhancer) and eating (another SNS enhancer) in people with fibromyalgia.
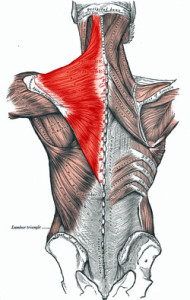
Stretching from the neck to midspine to the shoulder the trapezius muscle is well situated to contribute to the upper body pain in FM and ME/CFS.
They wanted to see if the trapezius, a nice big muscle stretching from the tip of the shoulder to the middle of the spine all the way up to the bottom of the skull, would ‘act up’ when FM patients were exposed to mental stress. The theory was that a dysregulated autonomic nervous system would, in a stressful situation, trigger painful muscle activity in fibromyalgia (no exercise or trauma required..).
There’s no reason it should; a mental stress test after all shouldn’t involve that muscle at all – but there is all this upper body pain in both FM and chronic fatigue syndrome to account for.
Just looking at that muscle with its ability to tighten the screws everywhere from the spine to the shoulder to the neck set me, with my history of pain in that area, a little a quiver. Interestingly this muscle, of all the muscles of the body, is one of the most responsive to stress in FM.
Results
Electromyograph readings indicated the FM patients had significantly more trapezius muscle activity during mental stress tests, breath holding and even during eating (two SNS activators) and instructed rest’ than health controls. There was no difference in muscle activity while watching TV. Pain levels that rose during the mental stress exercises in the shoulder/neck area but not in the lower back indicated the upper body was particularly susceptible to stress induced pain.
A System Primed for Activation
This results displayed a sympathetic nervous system primed to become activated in fibromyalgia. How the muscle activation caused pain is still unclear but the authors suggest one source may be activated trigger points. This is an interesting suggestion given Rowe’s finding that small misalignments in the nerve/muscle interface in ME/CFS adolescents can trigger significant pain. Rowe finds certain types of massage and physical therapy (myofascial release, etc.) that help to put the nerves/muscles back into their proper alignment can reduce pain significantly in his patients. He states they love this kind of body work.
Muscle Problems
To the researchers surprise, muscle activity during isometric exercise was reduced in the FM patients relative to controls. This could be due to problems with muscle metabolism or with poor ‘motor unit’ recruitment. They did suggest that elevated potassium levels -also found in trapezius myalgia – which is similar to FM – could play a role reducing muscle fiber recruitment during exercise. In any case it was remarkable to see muscle activity increased in fibromyalgia when it shouldn’t be (during stressful situations) and then reduced when it should be (during exercise) (!).
Little evidence of muscle issues was present in FM for years and the focus shifted to central nervous system issues but recent studies are beginning to find evidence of muscle problems both in fibromyalgia and chronic fatigue syndrome.
The Catecholamine/Sympathetic Nervous System Paradox Shows Up Again
Just as we saw in an earlier ME/CFS blog, the levels of main drivers of the sympathetic nervous system – the catecholamines – did not correlate with the sympathetic nervous activation that occurred. In fact, catecholamine levels were significantly reduced in the FM patients. In later blogs we’ll be looking in the role the vagus and other nerves may play in the enhanced fight/flight activity in both these disorders.
First, though, a look at yet another disorder that may have ties to both FM and ME/CFS.
Trapezius Myalgia – a Sister Disorder to Fibromyalgia and Chronic Fatigue Syndrome?
Characterized by chronic neck and shoulder pain, people with ‘trapezius myalgia’ (TM), display the same autonomic nervous system signature (low heart rate variability) found in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome and other so-called allied disorders. Interestingly, given the low HRV findings during sleep in ME/CFS, people with trapezius myalgia experienced their lowest HRV readings during sleep and may experience the same type of ‘micro-arousals’ speculated to occur in ME/CFS.

Trapezius myalgia – a neck and shoulder pain disorder with higher incidences of femailes, shares some similarities with FM and ME/CFS
Dr. Newton’s and others works have suggested circulation may be a huge issue in ME/CFS and this study found ‘micro-circulation’ issues in TM. Micro-circulation tests indicated reduced trapezius blood flows and oxygenation saturation and higher lactate and pyruvate in TM patients during a hour of computer work. (The high rates of ‘hypertrophied muscles fibers and low rates of capillarization which sounds like a recipe for low blood flows.)
I’m not clear if micro-circulation tests have been done in ME/CFS but the low blood volume, reduced blood flows and the paradoxically high rates of pain after exercise in that disorder suggest they may be possible.
Reduced blood flows can cause pain through a inflammatory process called ischemia which results in an explosion of free radicals. Maximum free radical and inflammation production in ischemia, occurs, interestingly enough, when normal blood flows are resumed, not during the period of low blood flows.
Given the advice of exercise physiologists that short bursts of anaerobic activity are the most effective way to exercise in chronic fatigue syndrome, it was interesting to find that ‘specific strength training ‘, not aerobic exercise, is the most effective way to decrease pain in TM. (Anaerobic strength training also appears to increase immune functioning (macrophage content) in TM.)
Wrap Up
In past blogs we’ve seen the autonomic nervous system issues linked with fatigue and sleep issues in ME/CFS; now we see them linked to stress, increased muscle activity and upper body pain in fibromyalgia. As in ME/CFS muscle metabolism or other issues may come into play.






Really interesting blog. If you could be bothered to reference your research articles with web links if you have them that would make them even more useful where readers may wish to follow up. Is TM an accepted new disorder or just a sign of tension in the body? Clarification on the particular types of massage which may be beneficial could also be helpful. Lots of questions raised by this blog. Thanks.
Thanks Linda,
I realized I forgot to link to the actual study (lol). Maybe your browser doesn’t show it but the parts in red in the blog all good to links to studies/papers.
Trapezius Myalgia does appear to be something of an established disorder; it’s never gotten nearly the study of chronic fatigue syndrome or fibromyalgia but it’s referred to in studies dating back 20 years. I imagine that its a subset of FM (ME/CFS?).
I’ll be looking more into the types of massage that are helpful in the future.
FINALLY! I now have possible answers to one of the most painful symptoms I have experienced. I don’t only have pain in this muscle, but spasm that is dreadfully frightening. First discovery was in my car, reaching from the front seat to the floorboard of the second seat…locked this muscle and I could not move for a few minutes. I seriously thought I was not going to be able to loosen it to move and turn back around. Then had burning pain sensation for days if I attempted to reach different ways. Now avoid reaching in the car at all, and combine this with a Ducheynnes’ contracture in the right foot, and something I always enjoyed (driving) is very inhibited. Cyclobenzaprine doesn’t do a bit of good. Still walking and stretching, yet hate being in the car at certain times. This is not me! MC
Oh wow lm the same, l feel a slight ting in my muscle then wham the pain can last for days l thought l was going crazy it’s good to know lm nit alone.
I think these are the psychobabblers, in disguise, actually. I think this is a sneaky way for them to say it’s just that we’re tensing up and causing our own pain because we don’t know how to relax. It totally ignores primary causes for hyperirritability of the upper trapezius, specifically, which might be presume to be the case in persons with physiologically based pain syndromes which then have lead to typical dyskinese of the shoulder force-couples (a flaw in the system of the different parts of the trapezius muscle working synergistically with other muscles to cause rotatory motions of the scapula for dynamic stability during shoulder motion) which occurs during many clearly physically based conditions, such as torn labrum, rotator cuff tear, chronic bursitis, etc.
It’s a study using EMG’s, so it’s made to look as if it’s a biomiedical study, but in fact, it’s just an attempt to find some way to attempt to quantify to the old argument that it’s all in our heads.
Hey, was my brain working for a minute? Ii’m not going to edit. Hope I don’t regret putting this out there. Waaay to late for me to be near a mode of communication.
🙂
It seemed pretty coherent to me…The mental stress element is certainly there but it involved simply doing a math test – not a psychological stressor at all – simply doing mental work..They also looked at eating – which is another sympathetic nervous system inducer and found the same pattern. The changes in muscle activity were small but evident and pain levels did increase although they weren’t completely sure why..They do note the possibility of muscle metabolism problems and they do suggest that myofascial trigger points may be involved.
I would agree that there’s more tenseness there – that’s at least been my experience since I got ME/CFS but I don’t think its because I don’t know how to relax I think its just been really difficult to relax and this shows up in poor sleep and the heart rate variability patterns seem to go along with that. I don’t think the inability to relax is in my head…I think it’s in my body and these and other studies are showing physiologically why that might be so…..I didn’t have to worry about relaxing pre-ME/CFS…
Cort Johnson I agree with everything you wrote above, with exception to massage being helpful. I had massage on those muscles and it activated trigger points that to this day I suffer on going pain from it in places I didn’t have pain in before I went.
It’s probably no surprise to you that this article resonates with me given my thoughts as per my recent article.
But Kim I feel you may be taking offense where none is intended. For years we have all fought to have our illness recognised as being real, and I can think of nothing more offensive than someone suggesting it is “all in your head”, as in; you are making it up, you are overreacting or even something as offensive as “you are causing this to get attention” or anything of the like.
CFS/ME and Fibromyalgia are clearly real illnesses with real physical symptoms. Just because some (like I) are saying that the root cause of the illness is in the head (that is where the largest part of the nervous system resides), should be no reason for offense.
Think about it, when people have Parkinsons or Alzheimers or Epilepsy, no-one says, “it’s all in your head”. The nervous system like any other part of the body can have dysfunction or disease.
The Vagus Nerve interact directly with macrophages and Lymphocytes. It works both ways. If the problem is in the immunesystem the parasympathetic nervous system will not work correctly and can also explain the ANS dysfunction. It is difficult. Or the overdrive can be a reaction for compensation the lack of energy. The ANS is not disfunctional because of stimuli. That is Bullshit, sorry for my language.
Perhaps I am misreading your comments.
You said: “Or the overdrive can be a reaction for compensation the lack of energy. The ANS is not disfunctional because of stimuli.
So isn’t the “reaction for compensation the lack of energy” the stimuli?
Cort,
Dr. Les Simpson’s recent book and ebook on Ramsay’s Disease posits that our some of red blood cells can become significantly deformed so they are the wrong shape to fit into capillaries. When fixed immediately at blood draw, the cells show up well. No cause is noted, but apparently use of Evening Primrose Oil, Fish Oils and Vitamin B12 can be helpful in improving the situation.
Hence our lower oxygenation and ability to perform much physical activity. These findings have been ignored by CFS researchers.
I wonder if this intermittent red blood cell deformation may influence the muscle spasms symptom?
Ramsay’s Disease – Myalgic Encephalomyelitis (ME) and the Unfortunate Creation of ‘CFS’ by Leslie O. Simpson PhD and Nancy Blake BA CQSW (May 28, 2012)
Suella
If its there, it fits right in with these findings – the rbc’s are getting there but they’re not offloading their oxygen as readily because they’re deformed – which leads to different conclusions.
Thank you for publishing this, Cort! I started out reading and thinking, “Hmmm. Interesting even though I don’t have upper body pain.” And then I realized, “Oh my gosh, this is describing my migraines and their shoulder, neck and back pain!” These headaches – well, I thought they were just headaches – started when I developed dysautonomia and CFS/ME and are excruciating. I always thought of them simply as migraines. This is a whole new perspective. They travel the path you’ve mapped. Exactly.
Do you know if it’s common for them to change sides? Like I can have one of these “migraines” for days and one day it will be traveling the right side, the next, the left. They’re rarely on both sides at once. Always accompanied by severe wooziness and poor light and sound tolerance. So are they related to migraines or is the accompanying head pain not considered a migraine or perhaps the TM is a migraine trigger? I also think there is a hormonal connection as they are much worse during … well, you know … I also find them triggered if I push beyond my physical limit or go too many hours without eating.
Thanks for shedding light once again!
Really interesting Tee
I hope to do a blog on migraines. Baraniuk did a study which found that migraines are much more common in ME/CFS than believed except that they were different kinds of migraines than usual…I’ll have to look it up…(There’s so much research they could do on this disease…that they haven’t done.)
Maybe TM is a migraine trigger…why not? So many things can…Migraines seem like another of this central sensitivity, sensory over stimulation aspect that Marco’s been blogging on.
I’ve never suffered physical pain as the result of this disease, so I’m bait out of place here and what I have to comment on might seem a bit off topic. However the significance of what I’ve learned from this article means a lot to me and is perhaps worth sharing.
I’ve always thought of eating as more of a parasympathetic stimulator, yet I agree there would have to be some sympathetic involvement, especially as blood is shunted from the periphery to the gut. This neurological response is of particular interest to me as I’ve long believed there was something in the act of eating that perpetuates this disease. The reaction I speak of occurs very soon after chewing and swallowing. I always thought it was due to LPS translocation, but I suppose it could be some manifestation of dysautonomia.
The following study references the bizarre phenomenon of fibromyalgia sufferers receiving relief after gastric bypass surgery. ‘Stone’ over at PR described a complete remission from ME/CFS and fibro symptoms only a few days after this surgery. The doctor said it was very common in these diseases but not to get too excited as the symptoms would very likely return several months down the road, which they did. However, this is an example of the type of thing the docs should be looking into but don’t.
http://www.ncbi.nlm.nih.gov/pubmed/18401670
Could it be this surgery changes the autonomic response to eating, that a stomach one-tenth the size doesn’t require the same sort of neurological involvement? I’ve no idea. Just putting the question out there.
The second thing that got me going in this article is the following:
“Maximum free radical and inflammation production in ischemia, occurs, interestingly enough, when normal blood flows are resumed, not during the period of low blood flows.”
Could this fact bring together two seemingly disparate ways of thinking about our disease? Dr Cheney talks about ‘oxygen toxicity’ being the main problem, and how our systems will do whatever it takes to keep oxygen out of the cells. He shows how we become overwhelmed by oxidative stress when given extra oxygen. Dr Shoemaker on the other hand claims the cellular energy problem is the result of ischemia and the concomitant GABA/glutamate imbalance and oxidative stress. Both can’t be right, can they? What if Cheney’s ETM readings concerning oxygen and commonly used supplements are merely gauging the short-term explosion of free radicals following resumption of normal levels of oxygen? Perhaps as long as problems with micro-circulation are present various treatments you would expect to be helpful in a condition like ours can’t be used. By these I mean oxygen, CoQ10, methylcobalamin, etc. So what’s causing the ischemia then?
I’m really loving this site! Absolutely what I was needing. Thanks so much.
Interesting article! Thanks, Cort. I certainly have major problems in that area. Sometimes it tenses up so much it feels like stone. Sort of happy knowing I’m not alone in that problem.
None of us like to have our condition dismissed as an emotional/mental one and we certainly don’t want to be told that it’s all in our head! I’m sure the majority of us have run into more than one person who’s accused or inferred that to us. However, it also bothers me a bit when PWC’s et al automatically get defensive and immediately dismiss any use of the word “stress” without taking a minute to remember that stress means more than just an emotional state. One can have stress from physical things like heat, weather, pain etc and things other than just situations. Perhaps by doing so sometimes the baby is getting tossed out with the bathwater and important clues may go missing??
Tee, your reply could be mine! I too didn’t think this was relevant to me, but then made the connection with my neck and shoulder pain and migraines. Mine too go n for days, 48 hours on one side, then 48 hours on the other.
I have found only one helpful treatment, Greater Occipital nerve injections on both sides, it gives two weeks or more pain free time.
There is also a major link between the migraines and ME/CFS for me.
Thank you Cort for your paper, very very helpful
The first information I got about my illness was from a post-polio conference. A neighbor purchased 6 or so tapes and loaned them to me. This was in about 1985. A few points that may show similarity with FM/Myalgic Encephalomyelitis.
One speaker gave a long presentation on scoliosis. This is an S curve in the spine, but I did not realize that the spine’s curvature was caused by a constant signal from the brain that shortened the trapezius. This may be closely related to Trapezius Myalgic or even cause it.
I believe the Conference was held a the Shriner’s Children’s Hospital in San Francisco.
I had an interesting note when I was feeling discouraged. It was from a British member of the virology group. He read the patient groups and felt that I would be happier in a post polio group. ME was closely tied to polio caregivers and nurses–a spin off from polio hospitals. Some people did not get polio-myelitis but were observed for it because they often showed similar symptom.
The Behan/Behan Glascow medical epidemic was found to be caused by a milder enterovirus called Cox Sakke according to a 1985 paper by the 1st Behan. He married a researcher.
He thought that my ME was causing me grief because I was much more ill than most PME’s at that time and older than most support group members. He seemed to feel that the viruses blamed for ME (or Post ME) and the Chronic illnesses that reactivated after a polio remission were so similar that I might simply switch diagnoses with the help of a compassionate doctor to get into a more supportive community.
This did not mean that I did not have ME, but the collateral viruses were similar. Some polio survivors relapsed into a ME like condition in middle age.
ME is not caused by any one virus. Geography, local genetics, climate, all play their role and run their course. Comorbidity will become a rich source of understanding.
The Science budget has been slashed by 55 million dollars.
Much ME and virulent viral research is outside the Federal budget, but largely underground. My source for this information is impeccable. Operation White-coat has just ended, Information about it is in Wiki.
This involved injecting Seventh Day Adventists with the pathogens that were expected to cause the post war chronic illness. Wiki included a consent form for each injection. A form for each virus may have been included. The men then worked for the Post Office.
What we know does not hold a candle to what we don’t yet know.
I was looking at my Aunt’s death certificate, she died of Encephalitis, Pharnxgitis and Necrosis of the pons. She may have been exposed to an unannounced “Safety” shot. The town doctor had diagnosed her with sciatic rheumatism. She collapsed a few days after a picnic “out in the valley”.
Her death certificate, I noticed, had been reviewed at the Federal level and included a signature verifying that it matched the original certificate. The upper left corner said
“Federal Security Agency.” it said there had been 345x antecedent cases. Of what? Sudden and enigmatic deaths in nubile young girls?
There are numerous other copies of her death certificate. And then of the 375x antecedent cases. Her cousin Carolee died the same year, before her namesake niece was born.
This might be of interest – particularly for those with a post-viral onset.
I’ve been digging around lately on the autonomic nervous system and how it might relate to immune and inflammatory parameters.
This is nice little summary (can’t vouch for the accuracy of the reporting of the science I’m afraid) that describes how the sympathetic nervous system stimulates the production of pro-inflammatory cytokines including IL1b, IL6, TNF-a and c-reactive protein (which should be familiar as those inflammatory markers consistently found in ME/CFS and described by Danzer in Part I of my ‘blog’ as ‘reliable markers of inflammation in medically ill patients’ – which result in “non-specific symptoms that are similar in all these conditions and include depressed mood, altered cognition, fatigue, and sleep disorders.”
A clear mechanism by which ‘stress’ can lead to or exacerbate heart disease :
Nervous system regulation of inflammation, cytokines, and heart rate variability
http://www.lapislight.com/wp/2010/05/27/nervous-system-regulation-of-inflammation-cytokines-and-heart-rate-variability/#.UWbQKbWBHJY
I also came across another paper (not referenced in the above) that describes how ‘sympathetic dominance’ of the ANS can exacerbate the inflammatory response to common respiratory infections. Rats infected with the influenza A virus that have had their sympathetic nervous system ‘chemically disconnected’ have a much greater survival rate than those that don’t :
Cutting Edge: Sympathetic Nervous System Increases Proinflammatory Cytokines and Exacerbates Influenza A Virus Pathogenesis
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941093/
Could this explain why common viruses barely effect some while others seem to never recover?
If your autonomic nervous system is already switched to a sympathetic dominant state a common virus could hit you like a ton of bricks!
Errata: the note was not from a Behan.
In POTS (and maybe in other types of orthostatic intolerance as well, one would have to look this up) there’s often a form of pain they call “coathanger pain”. It could be helpful to also look at this in order to try to understand how this all fits together.
I think that elevated glutamate may be a common denominator between trapezius myalgia, fibromyalgia, and migraines. Here is a study on elevated glutamate in trapezius myalgia.
http://www.ncbi.nlm.nih.gov/pubmed/15561388
Here is a excerpt from my new fibromyalgia book on glutamate in fibromyalgia and migraines.
Elevated Glutamate
While GABA is the major inhibitory neurotransmitter in the brain, glutamate is the major excitatory neurotransmitter. As our next study confirms, fibromyalgia patients have significantly higher levels of glutamate in their cerebrospinal fluid. Glutamate mediates central sensitization (Gudin, 2004). Central sensitization is a condition of the nervous system that is associated with the development and maintenance of chronic pain. The following study discusses the association between central sensitization and the “tender points” found in fibromyalgia, due to the increase in glutamate levels. Central sensitization can lead to heightened sensitivities across all senses, not just the sense of touch. Fibromyalgia patients often report other sensitivities, such as those to light and odors.
Research shows that central sensitization is also associated with chronic low back pain (O’Neill, 2007) and chronic neck pain (Chua, 2011), both of which are associated with fibromyalgia. A recent study found 28 per cent of women with chronic low back pain also met the criteria for fibromyalgia (Nordeman, 2012).
The following study also discusses the association between elevated glutamate and migraines. The significantly higher levels of glutamate, along with the damaging effects of homocysteine on the blood vessels, would clearly explain the comorbidity of chronic migraine with fibromyalgia.
Cerebrospinal fluid glutamate levels in chronic migraine.
Peres, M.F., E. Zukerman, C.A. Senne Soares, E.O. Alonso, B.F. Santos, M.H. Faulhaber. 2004. Cephalalgia 24(9):735-9.
“Both preclinical and clinical data link glutamate to the migraine pathophysiology. Altered plasma, platelets and cerebrospinal (CSF) glutamate levels have been reported in migraine patients. Chronic migraine is comorbid with several conditions. It has been recently shown chronic migraine comorbidity with fibromyalgia…CSF glutamate demonstrated significantly higher levels in patients with fibromyalgia compared to those without fibromyalgia…Tender points, the hallmark of fibromyalgia… is probably mediated by central sensitization, with increase in CSF glutamate levels.”
This would also explain the connection to PMS and why these symptoms worsen.( More book info:)
“Many patients with fibromyalgia also suffer with severe premenstrual syndrome (PMS) (Amital, 2010). Premenstrual syndrome occurs when there is a drop in progesterone levels just prior to the start of the menstrual period. Common symptoms of PMS are anxiety, depression, and irritability. In the following study the researchers found that patients with premenstrual dysphoric disorder, or severe PMS, had low levels of GABA.
GABA (gamma-aminobutyric acid) is the major inhibitory neurotransmitter in the brain. Excitation in the brain must be balanced with inhibition.
Low plasma gamma-aminobutyric acid levels during the late luteal phase of women with
premenstrual dysphoric disorder.
Halbreich, U., F. Petty, K. Yonkers, G.L. Kramer, A.J. Rush, K.W. Bibi. 1996. Am J Psychiatry. 153(5):718-20.
“In women with premenstrual dysphoric disorder… plasma GABA levels decreased from the nonsymptomatic, mid-follicular phase to the symptomatic, late luteal phase.”
The declining levels of progesterone just prior to the onset of the menstrual cycle are responsible for the low levels of GABA and resulting symptoms found in PMS. The progesterone metabolite allopregnanolone is a potent modulator of GABA receptors.
Of course, other factors could come into play. For instance the low muscle oxygenation found in patients with fibromyalgia.Patients with fibromyalgia are unable to properly metabolize iron. A molecule of iron is needed to make hemoglobin, so this would explain the low muscle oxygenation.
Muscle tissue oxygen pressure in primary
fibromyalgia.
Lund, N. A. Bengtsson, P. Thorborg. 1986. Scand J Rheumatol 15(2):165-73.
“The conclusion is that in patients with primary fibromyalgia, the muscle oxygenation is abnormal or low…”
Fascia inflammation and the abnormal collagen metabolism found in fibromyalgia would also most likely be involved in shoulder pain.
Collagen cross-links in fibromyalgia syndrome.
Sprott, H. A. Müller, H. Heine. 1998. Z Rheumatol. 57 Suppl 2:52-5.
“To determine whether abnormal collagen metabolism is a characteristic of fibromyalgia, we have analyzed collagen metabolites in the urine and serum of patients with fibromyalgia…Decreased levels of collagen cross-linking may contribute to remodeling of the extracellular matrix…”
Also, fibromyalgia patients have significantly lower levels of ATP in their muscles which may be involved.
Use of P-31 magnetic resonance spectroscopy to detect metabolic abnormalities in muscles of patients with fibromyalgia.
Park, J.H., P. Phothimat, C.T. Oates, M. Hernanz-Schulman, N.J. Olsen. 1998. Arthritis Rheum 41(3):406-13.
“patients had significantly lower than normal…ATP levels…in the quadriceps muscles during rest.”
I can think of a few more things, but with all of this going on there is no wonder fibromyalgia patients have shoulder pain.
How to diagnose brain fog in patients with FM/CFS/ME: challenge them to read through the comments to these articles!! 😮 My eyes were glazing over after the first few, but by the time I reached the last two, I had a meltdown. LOL! 🙂 BTW, I have both FMS and CFS/ME.
Seriously, many of these studies are great in the sense that they can shine a light on various clinical outcomes and conclusions based on them. At the same time, and maybe this is just ME, it also adds another “could be/maybe it’s related” to an ever growing, very long list of possible underlying causes of our symptoms that can be really confusing.
I have a medical background, so I am able to read fairly complex medical papers and understand rather scientifically detailed comments like Annesse’s above. However, not to discount the intelligence of the majority of people with these illnesses, I wonder how many can truly relate to all this influx of information. Just saying… 😉 The question often hangs in the air, “fine, but what in the hell can I DO about it!” As you stated Cort, it may be years before we see any effective drug treatments for these illnesses.
That being said, I can subjectively relate some of this to my own symptoms; some symptoms I’ve not understood how or why they develop. For example, whenever I go out to eat, or when I have to sit in a chair at a table, I get nagging pain between my shoulder blades and down my back. When I’m at home, I eat in my chair, leaning back on a pillow and my feet on my footstool, and don’t suffer from that pain. When I try and work on my jewelry-making, a few minutes of barely leaning over my work, even with a good chair and arm/back support, causes the same pain symptoms. Bending my head back, especially for longer than a few seconds, can result in a headache and burning nerve pain the next day that may last from 1- 3 days. The information above may explain some of the causes of these symptoms.
The findings regarding strength training vs. anaerobic exercises is interesting. I have taped on my office wall an article titled “End Neck Pain in Three Moves” from Prevention magazine (don’t have the date). I admit it – I haven’t tried the easy exercises I’m about to describe because I am a terrible procrastinator. I just need to get weights! The study was conducted in Denmark “which studied 42 women ages 36 to 52.” It involves only three strength training sessions per week, and only three simple exercises using weights from 2- to 5-pounds. After only three months, the women in the study had reduced their neck pain by 80%. The researchers believed that this type of strength training “may help generate new muscle in place of injured tissue.” There may be other factors at play, as well. These women were not diagnosed with FM, only “chronic neck pain.” So, I have no idea if it would help in FMS, but it very well could.
As always, Cort, thank you for this most interesting article about this study’s findings! Hopefully, these many puzzle pieces will eventually come together to form a truly clear picture of the complete puzzle.
Cheers! Judith
I pasted a picture of my grandmother with two herpes sores
just above her cheek bone that eventually blinded her and took her wealth of wisdom and history, her ability to think and orient herself to her family and few remaining friends.
Christmas dinner was out to her childhood friend Annie who had married my grandfather’s Brother Rass and farmed farmed out in the valley. I called at Christmas a few years later and though she remembered a great deal, her brain, seemed to reject death Aunt Annie and Rass were there again. I wondered how long it would be before she joined them. She was very afraid of her life ending as it did.
Gancyclovere might have prevented it, according to Virologists I talked to on the web. I hope something will be there for me. So far I’m fine if I get enough sleep, but really, ME is far less than anyone deserves.
Since she was the last to become frail she shoveled snow until noon of the walks of her friends. Then she might go chop wood for my grandfathers sister, stoke her old school friends’ wood stove. She had met my grandfather through his sisters.
I’ve had fibromyalgia since I was 23.. I am now 42. I am not sure if I am supposed to call these a migraine or not. Imitrex spray helps to make it go away and doesn’t leave me with the migraine hangover..(sensitivity where the pain was, feeling drained and the feeling of it coming back any minute). Is the trapezius myalgia not considered a migraine?
As someone who has had fibroymyalgia since they were 27(im 39 now) I can really appreciate to find other people who suffer like I do. I also have interest in Kay’s question if you wouldn’t mind answering it.
Fibromyalgia can be one of the many causes of lower back pain in women. That’s why it isn’t important not to ignore symptoms but rather consult a medical professional when discomfort persists.
Good point. Thanks.
I agree with Cort it was a coherent article and it really explains a lot. When those muscles are activated, they go into spasm and began to burn exactly where the picture points out on both sides up to my head. Math questions are an excellent example…when I went to see my M.E. / Fibro specialist she did a test requiring me to do simple math while walking a straight line on the floor. I couldn’t do it with out loosing my balance and escalating burning pain right across my trap muscles and shoulder down to under my shoulder blades. They are on the right track…ppl just aren’t reading the article correctly..this on the right track!
One year ago, I had to have reconstructive shoulder surgery: cracked labrum. Interestingly enough, I did NOTHING to crack my labrum; it just happened. Six months ago, my jaw started to dislocate and spasm to one side of my face. Stress, they say. The new specialist did say that the jaw and the shoulder are connected issues. During all of that time, I had horrible tension headaches, which I first thought were migraines. This article REALLY speaks to me. It makes complete sense, as does the fact that I’ve been told that my central nervous system has flipped out. I will be discussing this with any doctor, who will listen. I was first diagnosed at either 15 or 17, and I’m now 37; I’m too young for this.
Wow….Good luck with all that Ananada. I would just keep seeing experts, if you can, until you get some answers.
Good post…..Back pain, and with it sciatica, is one of the most common forms of pain affecting our society today and Headaches are an extremely common complaint in our society. Pain is an unpleasant conscious experience that emerges from the brain when the sum of all the available information suggests that you need to protect a particular part of your body. When a health illness or condition is chronic it means it is long-lasting. visit our site for good tertments for Back Pain, Diabetes, Fibromyalgia, Thyroid. http://www.drbastomski.com/
Hi Cort, I remember when you started this blog. What an excellent blog it has become, congratulations. An incorrect bite causes heaps of problems in FMS suffers, but I find it hard to find a dentist who understands the sensitivity in my bite. The above blog is an excellent example of how sensitive we are.
Why I am writing you is that about two weeks ago I was diagnosed with a Genetic Disorder called Pyrroles Disorder. It is a blood disorder. We need Pyrroles but in this disorder they become too high and cause all sorts of havoc, both mental and physical including a lot of MFS/CFS symptoms. Only 10% of the population have it, so it is rarely tested for or diagnosed. The test is a special urine test. I started seeing an Integrative Doctor a month ago who tested me and gave me the diagnoses. There is no medical treatment for it, the treatment is diet and supplements advised by a naturopath. Just wanted to let you know of this. If you do some research you may find a whole lot of interesting things to put on this your blog, for fellow sufferers who don’t know they have it. Thank you for all you excellent work.