




Elizabeth Unger reveals first finding from the multi-center CDC study involving top ME/CFS practitioners in the US
(Are different ME/CFS doctors seeing different types of ME/CFS patients. Would closely examining those patients reveal the elusive subsets researcher have been talking about for decades? At the FDA Workshop on April 26, Dr Elizabeth Unger, head of the CDC’s Chronic Fatigue Syndrome programme revealed the initial results of their multi-clinic study assessing ME/CFS patients. Please welcome Simon McGrath to Health Rising as he digs deeper into the first fruits of this fascinating study)
Things are changing at the CDC. Previously known for it’s insularity, the CDC set up a collaboration with the top ME/CFS clinics in the States to look at patients in detail (and even collaborated with the clinics on designing the study protocol ). The goals were to see if and how patients differed between clinics, to gather hard data to help address the issue of case definition, and to find the best ways of measuring this illness.
ME/CFS Physicians Take the Lead in Deciding Who Has ME/CFS
The study set out to capitalize on the expertise of leading clinicians working with ME/CFS patients, including Dan Peterson in Incline Village, Nancy Klimas in Florida and Ben Natelson in New York City (see map). Having chosen clinics run by these top physicians, the CDC left it to them to include the patients that they considered to have “CFS, ME/CFS or anything that fits under this umbrella diagnosis”.
This inclusive approach should help show up any differences between the types of patients that different clinicians consider to have “ME/CFS”. Also, collecting data like this gives a broader population, and any ‘true’ group of patients (eg ICC) should emerge as clusters in deeper analysis.
A Mountain of Data
The study collected a vast amount of data: physical examination results, clinical history, lab test results, immunisation history, demographics. Then patients had a LOT of self-report questionnaires to complete, including mental health, CDC Symptom inventory, DePaul Questionnaire, SF36 health survey and the Mulit-Fatigue Inventory. Also, sleep and pain measures, and a battery of the NIH’s PROMIS questionnaires. Phew! No wonder Beth Unger was keen to thank all the patients patients taking part. Many questionnaires were made available online so that patients could complete them in their own time.
The first results…
The first results are now in, based on an interim analysis of 393 patients (which will ultimately be 450). Starting with the basics:
- Average age: 48.6
- Female: 71%
- BMI: 27.2 (about average for the US)
This is broadly in line with other studies, though the 71% female is a little low, with one clinic having barely over 60%. (77% of patients were women in a recent UK study with a large clinical sample).
It’s also worth noting that this sample isn’t fully representative of all patients: it’s 95% white and 78% college-educated, probably reflecting the fact that 98% were medically-insured. Whether or not this sample is typical of ME/CFS generally, despite this demographic bias, is unclear. Also, like just about every other ME/CFS research study ever done, this one excludes severely affected patients as they are too ill to make it to the clinics.
Burden of Chronic Fatigue Syndrome Laid Bare
The numbers coming out of this large study illustrate the high burden ME/CFS imposes:
- Average time to diagnosis: 4.5 years
- Typical length of illness: 15 years
- Average age at diagnosis: 38 years
- Not working: 75%
- Pain in the last week: 80%
- SF-36 Physical Function mean score: 37 (100 is full-health, 90 is typical for working-age population)
- MFI General Fatigue mean score: 18 ex 20
Take a look at this in the graphic below:
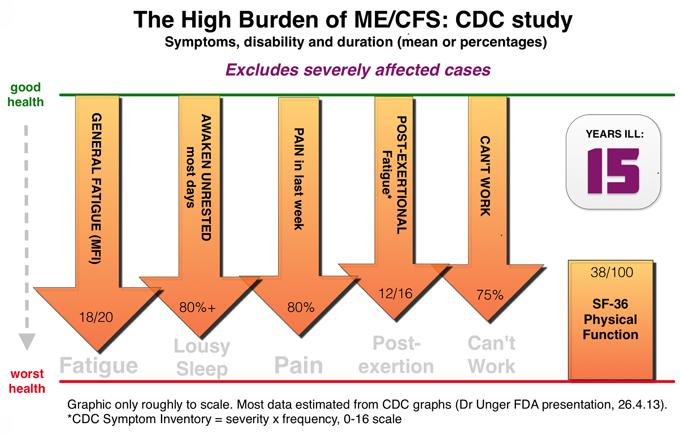
Similar patterns and findings have emerged from other surveys, but none before have used such a comprehensive range of measures, or used the best clinicians in the land – or had the endorsement of the CDC.
Thirty-seven percent of patients scored the maximum possible 20 points for MFI General Fatigue subscale, showing a serious ‘ceiling’ problem where the scale cannot tell the difference between very bad fatigue and even worse fatigue. The same situation applies to the Chalder Fatigue Scale, widely used in the UK. Clearly a more sensitive measure of fatigue is needed.
Fifteen years is a long, long time to be ill, and while those who have recovered obviously aren’t included in this study, those still ill probably have many more years to serve. It’s shocking that it takes an average of nearly five years to get diagnosed – by comparison, the average time for diagnosing Rheumatoid Arthritis is nine months.
All the different sleep questionnaires found severe impairment of sleep, which was also the most disabling symptom reported.
Surprisingly Good Mental Health, and Other Finding s
s
Elizabeth Unger zipped through a lot of results in half an hour, with 27 graphs just for symptom scores. Here are some of the other highlights:
- Unsurprisingly, the top symptoms were poor sleep, post-exertional fatigue and muscle aches and pains.
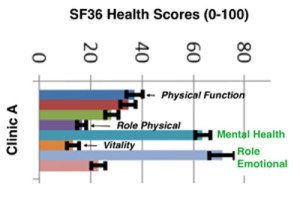
- The comprehensive SF-36 health survey found that pretty well everthing was worse compared to healthy norms, especially Physical Function (no surprise there) and Vitality (or there). But what really stood out were the high mental health scores (see the graph; the data is from a single clinic, but clinics did not differ significantly). This suggests that ME/CFS patients are showing considerable mental resilience in the face of the serious problems they encounter in almost every other area.
- 67% of patients reported sudden onset (individual clinics ranged from 52%-76%).
- Patients said they did mild exercise an average of 3.4 times a week, again varying by clinic, though it’s not clear how ‘mild’ exercise was defined. 80% had pain in the previous week, with 64% taking medication.
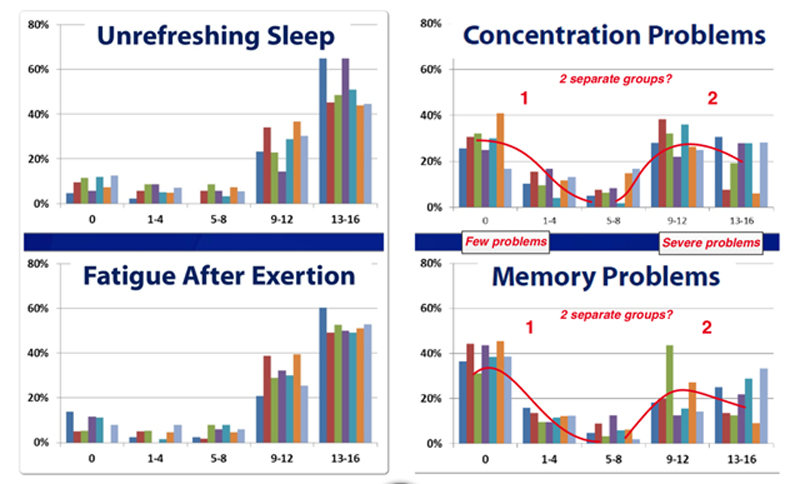
Another intriguing finding is what Elizabeth Unger described as ‘U-shape curves’ for cognitive functions; there appear to be two distinct groups, a larger one with severe cognitive problems and a smaller one with only mild cognitive impairment. It would be interesting to see how these groups map onto different case definitions, eg ICC versus Fukuda.
Illness burden: CFS vs the rest
The final results slide Unger showed compared CFS with other conditions including Multiple Sclerosis, Muscular Dystrophy and Chronic Pelvic Pain. This was done using the NIH’s PROMIS survey that collects standardised data to help contrast different conditions. Pain in ME/CFS was on a par with Chronic Pelvic Pain, but in almost every other case CFS patients had much worse pain, fatigue and sleep scores than comparison illnesses. And of course, Nancy Klimas is on record as saying CFS is worse to have than being HIV positive – and she should know, since she treats both types of patient.
Goals of the study revisited
Do the Clinics have different types of patients?
One goal was to establish: do different Clinics see different types of patients? The answer is Yes and No. Many findings were statistically different between clinics (eg. the average length of fatigue) but generally the differences were not huge – and may not be biologically significant. While there were some differences between clinics, the differences between patients in any clinic was much greater. This is more confirmation of the heterogeneity of ME/CFS patients, and all the clinics seem to be seeing a similarly diverse range of patients – though this is only an interim analysis.
No sign yet of subgroups
So far, said Elizabeth Unger, the existing measures haven’t shown up any robust subgroups (another study goal), but a detailed cluster analysis will probe this in more detail. However, finding subgroups may not be easy, even where there is very good data, as the experience of Parkinson’s Disease shows.
Finding the best ways to measure ME/CFS
The third study goal is to establish the best measures of ME/CFS. The good thing about using so many different measures in one study is that it allows comparison of one measure against another (eg MFI defined fatigue vs PROMIS defined fatigue). Generally, different measures agreed well, which is encouraging. More analysis will be done on this, but the real test may come in the next stage of the study which involves tracking patients over time.
Which measures will best capture changes in ME/CFS is a key question in any clinical trial, but, remarkably, there has been almost no work on this in ME/CFS, or in any other disease. Using an objective measure like Treadmill time – as in the Ampligen study – is a good, perhaps better, alternative to a questionnaire, but where questionnaires are used they need to be shown to reliably measure change.
Networking success
Elizabeth Unger said how valuable she found the networking: “We appreciate our expert clinicians, and one of the things we found most rewarding was our on-site visits with each other, and the clinicians also appreciate the opportunity for networking”. I think this study is probably the largest US clinical collaboration to date, and there seems to be an apetite from all the players to continue with this kind of work.
Bigger Study Underway
What’s great about this study is that it’s established a solid base camp, but much more is planned. A huge amount of data has been captured, showing the scale of problems in ME/CFS and the wide variation between patients. To establish the best measures, and to identify robust subgroups, or even validate a case definition, more data is needed and the CDC have plans to do just that.
First there will be follow-up of patients to see how things change over time. Second, for a subset there will be more and different data gathered: blood to look for biological markers, plus cognitive tests and exercise tests that might yield information that better reveals the true nature of ME/CFS.
To further understand the abnormalities of ME/CFS, the CDC plan control groups, both of healthy volunteers and ‘ill controls’, groups of patients with other illnesses that will help researchers pinpoint what is unique to ME/CFS. These early, interim results presented at the FDA are just an aperitif for a study that will be delivering a great deal more in the future.
- Graphics, (apart from ‘burden of’) were adapted from Elizabeth Unger’s presentation.
Simon McGrath has been ill with ME/CFS for way too long. He thinks research is finally kicking off after years spent wandering in the desert. He occasionally tweets about ME/CFS research: Follow @sjmnotes. Find more of his blogs on Phoenix Rising.







I think there are ”CFS” patients with POTS and without. SF-36 etc… is not reliable for measuring subgroups. You need objective data. I am happy that the CDC is doing research but there is a long way to go. Fatigue is a very wrong and subjective term. I feel more unwell and weak almost all the time.
Hi Gijs
The next phase of the study will bring in objective data, including bloods, cognitive tests and exercise tests, which should help a lot. As far as I know, this doesn’t include POTS, though the DePaul Symptoms questionnaire does cover some autonomic symptomts.
As for fatigue, I think it’s important to capture this (and not sure of an objective measure of it either) – but it’s clearly not enough on it’s own. That DePaul questionnaire also covered post-exertional fatigue and there were many symptoms covered – worth looking through the video with slides – (think you need to got to at about 90 mins in Panel 3)
http://www.tvworldwide.com/events/fda/130425/default.cfm
Hi Simon
Thanks for another nice blog!
The ‘u-shaped’ distribution for cognitive functions is interesting.
Two sub-groups? Possibly.
It would be interesting to see if cognitive function was correlated with illness duration.
Thanks, Marco!
I thought the U-curve things was one of the most surprising findings. Hopefully the more detailed analysis will show up more correlations, and maybe clusters too, though I suspect they will need more data (inc objective measures) to really find any subgroups.
If you look at much of the objective research done on ME/CFS patients (Shungu’s MRSI, Peckerman’s impedance cardiography, Hollingsworth’s skeletal & cardiac muscle MRSI, etc.) there always tends to be two sub-groups. They typically fall out into 2 groups due to severity – one that has more severe physiologic impairments, and one that is less severe. Why is this the case and it is not a continuum… I really don’t know? Hopefully we will find out soon.
Disease progression may play a role in all this, but when I personally became ill I had fairly severe cognitive dysfunction within a couple days of the acute onset viral-like syndrome that became ME and has been in full force ever since. I am on the “more severe” end of the spectrum. I realize I am n=1 so that doesn’t mean much, but many I know or have talked to who started out with severe disease also had cognitive dysfunction right away.
Marco, what is your hypothesis – that cognitive dysfunction comes early in the disease and fades later, or that is becomes worse as time passes after onset?
See below for the papers I specifically mentioned (there are plenty more, but these are especially good ones):
http://www.ncbi.nlm.nih.gov/pubmed/20497461
http://www.ncbi.nlm.nih.gov/pubmed/12920435
http://www.ncbi.nlm.nih.gov/pubmed/22281935
Thanks for the article Simon – good stuff.
Hi there.
Another anecdote – but in the great scheme of things I guess I’d be classed as gradual onset and I didn’t have any serious cognitive issues until 20 years or so in.
I recently came across a fascinating (and largely overlooked) paper from a few years ago that found two distinct sub-groups using an objective measure of cognitive function. I hope to blog a write-up fairly soon.
The results can be interpreted variously. Different etiologies, a deterioration in cognitive function over time or degrees of severity at onset. There’s insufficient data to determine which.
A viral trigger (as opposed to other potential stressors such as psychological stress or overtraining) could very easily result in initially more severe cognitive function which may potentially resolve over time in some cases in the same way that ‘sickness behaviour’ resolves after the acute phase of a viral infection.
All speculation of course in the absence of evidence but I feel that there is also the potential for cognitive function to deteriorate over time in the absence of treatment whether onset is sudden post-viral or gradual.
That sounds like another example of the need to subset out this illness.. I was just traveling with Corinne, someone who’s severely limited physically but only in the last couple of years (she’s had it 25 years) has the cognitive stuff started to come in. She’s still sharper than me, actually – but now neurological issues – computers wipe her out and she can’t read without getting headaches – are effecting her ability to engage in cognitive activities.
Thanks, MD with ME
You might be interested to know that Julia Newton, who did the ‘impaired cardiovascular response to standing’ study you linked to, has a series of studies underway, including looking at heart functioning in much more detail, and its relationship to orthostatic intolerance.
I was involved in the study and the amount of questions and categories were enormous. Many questions were subjective, which made me a little nervous. I hope the 5-6 hours that myself and other patients spent on this will help to bring about change not just with the CDC but with all agencies that can help make a real difference for us.
Wow – 5-6 hours? That is a lot of work. It’s great that people like you are willing to put in the time. I do think this study is makrs a change from the CDC, with their willingness to collaborate and Beth Unger stressing how important she saw the networking. I suspect the next stage of the study, with follow-ups and objective measures will make a big difference – so watch out, theymay be back for your blood 🙂
It was Dr. Unger who told the CAA ‘We must find a way to capture physician intuition” which lead to the CAA project to do just that (by asking our top physicians what drugs worked with which symptoms’. Why mention that now? Because she was visiting these physicians and I’ll she was impressed enough with them to feel like we must get their knowledge and intuition down. It’s great to have our CDC program leader getting behind ME/CFS physicians…it’s kind of incredible, really.
I remember asking Dr. Peterson in the Reeves era if the CDC ever visited him and the the answer was, after that first outbreak, no….I asked Staci Stevens if the CDC ever asked her about the exercise test and she laughed in my face….Now the next study will include the results of VO2 max tests (and blood samples.). This is a very different CDC we’re seeing.
Thanks for taking part, Cheryl.
Simon, thank you for an excellent summary of Dr. Unger’s presentation.
You noted: “Like just about every other ME/CFS study ever done, this one excludes severely affected patients as they are too ill to make it to the clinics.” Key point.
Severely affected patients are too ill to participate in research studies like this one; to participate in treatment trials; to get to physicians/clinics for ongoing care; and to appear at public meetings to represent their subgroup and put a face on it.
At the meeting Dr. Lily Chu offered ideas for overcoming some of these barriers. Hope to hear more from her on this.
Thanks, Gemini
Would love to hear those ideas from Lily Chu.
There was on large trial in the UK, called FINE, that used ‘rehabilitative therapy’ (based on deconditioning) and was home-based and included severely affected patients. It didn’t produce any gain on either primary endpoint (Fatigue and function) at 12 months, though reanalysis did find a small fatigue gain using an alternative scoring method…
http://www.biomedcentral.com/1741-7015/4/9
Still, credit to the authors for including the severely-affected.
Ultimately, to include the severely-affected, researchers must go to them, or bring them into hospital for assessment.
I just drove Corrine up to Dr. Peterson’s. She’s mostly housebound (she was bedbound when she first saw him -and came in in a wheelchair). She goes to bed around 5pm every day – can’t stay up later than that – walks very little – and has worrying neurological issues.
She’s not bedbound but I think she’s probably ill enough to more or less represent a class of severely ill patients and Dr. Peterson has a quite a few patients like her in his practice. Corinne is in the CDC study. My guess is that he purposely included more severely ill patients in the study and that there may be more than we think. If I was a physician I would get my ‘illest’ patients, the ones with the most abnormal findings, into this study.
I imagine that at the end of the day Unger will be able to separate out more severely ill patients and see what kinds of unique issues they have.
If there are people like Corinne in the study then I think we’re in pretty good shape even if they aren’t bedbound..(and Corinne was before she saw Dr. Peterson.) I would also guess that the group of people who see the top ME/CFS physicians tend to be sicker than your ordinary patient. They’ve probably been around – seen scores of physicians – and finally ended up at Peterson, Lapp et .al. I think we’ll see, though, as more study results come out, just how sick they are.
It’s great that people like Corinne are in the study – what’s needed is a way to include enough of such people so that they can be properly examined in a study like this. (There’s a case of excluding them until later stages of the study where researchers are clearer about what they need to look for, to minimise the burden on these patients).
I suspect, though, that Corinne isn’t typical of the CDC study. The mean SF36 Physical Function score was 38, just the same as the large PACE trial (n=640). We know that for PACE, patients had to be able to attend weekly, one-hour sessions of therapy to be able to be treated, and to be able to take part in graded exercise. So if levels of Physical Function are similar in both studies (as the SF36 scores indicate), then there probably aren’t too many severely-affected patients in the CDC study.
But I do think that people like Corinne – and worse (though maybe not fully bedbound) should be seen as a major research asset and priority.
When the MRC produced a Strategy report in 2003, one of their main recommendations was that researchers should prioritise including severely-affected patients because of their research value. Unfortunately, that hasn’t happened yet.
As someone who is now too ill to see any of these physicians or participate in any studies, I want to second Gemini’s comments. What has Dr. Lily Chu suggested so far? I am barely able to get to my internist who is ten minutes from my home. He requires me to visit every three months to get my meds renewed. Is there any way we can have input?
Thanks to Simon for an excellent summary.
Thanks, Theresa
Sorry to hear of your problems re your meds. In theory, in the UK doctors will come to see housebound patients at home, though consultants almost always will not (I have been very luck on that front myself).
You could always try contacting Elizabeth Unger at the FDA, pointing out how you are unable to reach such clinics. http://www.cdc.gov/media/subtopic/sme/unger.html
In other illnesses, the most severely-affected are sought out by researchers as thebest place to look for abnormalities etc. I suspect they are a negelected goldmine in ME/CFS too.
To me after reading for years and experiencing a lot. I think it starts with the stress bank account being depleted, the immune system goes down and then the cascade,,some have different symptoms but I see very much the same in the people I know..I got sick after the most stressful year of my life. I did eveything I read to do and saw several experts all with a little different versions but I learned from them all and had an 8 year remission. I went back to my old habits of being and doing everything. I crashed and seem to be coming out again after a lot of work on my part and life style change. Dr. Klimas knew the right tests to do, those never where done..huge immune testing.. Epsten Barr was very high no one would check for that. Killer cells were very low but high normal last May and I will be checked again…sent blood so test results will be ready on the 22. Wish me luck! I still had EVB activation last year. I know the doctors that do the right immune testing always find our killer cells to be low. I got mine back with LDN, Imunivor, Equilibrant and last May Acyclovir was added.
Good luck Marg…I was actually doing pretty darn good – not alot of stress- when I got ill…but after that I my stress response was thrown for a loop… Congratulations on getting better and good luck with those EBV tests 🙂
Great article, Simon! Thanks!
Thanks, John!
Simon, you have touched on an extremely important subject. I particularly like these two statements:
1) “Also, like just about every other ME/CFS research study ever done, this one excludes severely affected patients as they are too ill to make it to the clinics.”
2) In other illnesses, the most severely-affected are sought out by researchers as the best place to look for abnormalities etc. I suspect they are a negelected goldmine in ME/CFS too.
I sent a query to Dr. Dikoma Shungu, who has a $2 million NIMH research grant to study CFS. I wanted to know if they were going to include bedbound and housebound patients in his study.
I included my telephone number in my query, and was amazed when Dr. Shungu called me at home. I believe he was sincere when he told me that his team is committed to getting to the root of the illness.
He also said they desperately want to test the sickest patients. His exact words to me were: “People who are the sickest would have the strongest markers.”
And yet, this study–like almost all CFS studies–is *designed* to exclude bedbound and housebound patients.
I’m going to present an opposing viewpoint. I’ve long been wary of the need to include bedbound patients in studies. Yes, I agree that you can probably find out alot from them but, if you have an illness that stops 75% percent of the study participants from working – you’ve already got a really sick population. People can have heart attacks and still remain upright, they can have diabetes without effecting their functioning like that. These patients had worse sleep, fatigue and pain scores than people with muscular dystrophy and multiple sclerosis. By any standards these are very ill people.
I do recognize the fear that with all the difficulty pinning ME/CFS down, that excluding bedbound patients (which I don’t think necessarily happened; I think bedbound patients like Corinne do end up seeing doctors) might mean it’s easier to miss something. I’m sure that’s true.
On the other hand, people who are bedbound have a host of other problems that result from being bedbound; their heart rates, blood volume, blood flows and others which I can’t remember at the moment are disturbed simply from being bedbound – so with bedbound patients you have the additional obstacle of teasing out what was due to their not being able to move from ME/CFS. For that reason alone alot of researchers might poo-poo any studies focused on bedbound patients.
The optimum patient in an research study might just be someone who can get around enough to avoid the effects of deconditioning but who’s still very limited otherwise; someone perhaps like Corinne (?)
There’s definitely something in what you say about the problems of severe deconditioning confounding any results, but it’s something clinicians deal with in many other diseases. Lots of people with MS, muscular dystrophy and other neurological disorders are wheelchair-bound (and spend a good deal of time in bed) and may have less fatigue and pain with us, but are severely impaired in many other ways. Yet they are often selected for studies because of the severity of their condition. Probably many trials of such patients have almost all patients unable to work.
Clearly the issue of whether or not deconditioning could explain the result has to be addressed, but one way could be to included controls who have another illness, rather than are healthy.
It may well prove impractical to include the most extreme cases in research studies. However, including specific sub-groups of severely-affected patients in studies would show show whether these patients are a treasure-trove of markers (signal) or a major source of confounders (noise).
And in the UK, bed bound patients sadly get almost no proper treatment (just a GP visit if lucky)- it’s a big problem here.
I’m very encouraged to hear that about Doc Shungu. I do realise it is difficult and expensive to include severely-affected patients, but would like to see researchers making more effort to include these as a specific group within their studies: I think they would glean a lot of extra-information.
Either this “This suggests that ME/CFS patients are showing considerable mental resilience in the face of the serious problems they encounter in almost every other area.” or the patients have learnt to no speak about these symptoms for fear ME/CFS will be labelled psychogenic.
Hadn’t thought of that – an interesting point, esp as these patients had been ill for an average of 15 years so willl know the score. However, I doubt it would be a big enough factor to explain all the difference.
It seems from the account that the trial did not make use of actometers. Or are they activometers? In any case, with the burgeoning of cheap digital measuring instruments for a range of phenomena such as heart rate, footsteps, et al, it would be good to see use of these in research. Better to gather data of which some is later thrown out than never to have gathered at all.
It is astonishing that no one treats or measures severely ill patients. Can you imagine that in cancer?
Surely CDC needs to start gathering data on the severely ill person by person — and then of course randomizing the names to number codes.
I think actinometers, actinmeters whatever they are are a great idea and look forward to some news from the OMI on that front. I hope the CDC can include them in the study. That would take the CDC or the doctors buying acti—blah, blah, blahs 0 – I have no idea how expensive they are but I hope somebody can get them in there.
“It is astonishing that no one treats or measures severely ill patients. Can you imagine that in cancer?”
Could not agree more. “Actometer” is right.
I think Dr. Peterson, Dr. Klimas, Dr. Lapp and Dr. Cheney would disagree with the idea that they’re not treating severely ill patients. (They might agree with the idea that they’re not treating the illest patients) As I noted earlier Corinne was bedbound and wheelchair bound when she first saw Dr. Peterson.
I hope researchers can get access to the extremely ill and I think by the time this is all done, and all the blood samples and exercise tests have been done its going to provide alot of very useful information.
Maybe if this study sparks alot of interest the next study can focus on the most severely ill.
Hi Cort
Should have said I was talking from UK experience – the only NHS inpatient treatment centre closed when the consultant in charge retired.
But do any of the above clinicians treat inpatients? Sadly, many patients are just too ill to make it to a clinic – these are just the kind of patients who for any other illness would be getting the most attention, but in ME/CFS get the least.
I wrote one of the doctors in the study recently about using some of the newer exercise watches in some of the studies. The Basis watch (just one example) tests how many steps you take, continuous heart rate, how much you sleep, and even how much you sweat, and can upload the data over the internet. It seems like a treasure trove of data for much less than the cost of one doctor’s visit, and you could re-use the watch for multiple study participants. And it doesn’t require any work on the patient’s side, other than plugging in the watch to your computer every few days, so could even be used by the bed-bound.
Love it B! Thanks for the info…I’ll check it out.
Cool, please feel free to ping me if you have any questions. I just did an informal sleep study for a friend who works there and the watch data matched up really well with the EEG, which made me think that it could be used for much simpler sleep studies for people with CFS since you don’t need to go into an office/try to sleep while stuck with a million wires. I am sure in-office sleep studies can provide more detail but it isn’t very useful if people can’t actually sleep and/or can’t afford an expensive study…
I agree, that could provide a treasure trove of info to combine with the clinical and self-report measures. Dr Snell mentioned this type of thing too, think it could be the future.
Doctors will see housebound patients at their own home in the UK?
That is amazing.
In my own life in the US, that practice ended in my early childhood, making life hard for my mother — six small children, and there was no car at her disposal.
Makes life hard for me now, as one visit per year takes it all out of me. And that is not enough to get decent medical care.
More to the point of the article and all its data, it is a good way to learn something about patients and the specialist doctors. But I will be happy when someone pays enough money to visit the homebound ready to draw blood, and get a few questions answered about them.
Sarah
2 observations:
1. I am a bit blown away that the CDC was actually involved in a study that really seems impressive, that went to the real CFS experts & trusted them, & that actually concedes the pt that we are not only not mentally ill, but in fact actually pretty darn resilient! (yes there are certainly limitations in this study, as have been pointed out, but no study is going to be perfect, & this is definitely a step in the rt direction)
2. There are a lot more cognitive impairments associated with CFS than just memory & concentration
Things are changing at the CDC!
UNGER ON IMMUNIZATION/INFECTION HISTORY – COULD BE IMPORTANT
Just been watching the Q&A after Beth Unger’s talk where she was asked about the data they hold on infection and immunisation history – and whether that correlated with symptoms etc. She said that as this info was collected from patient clinical notes it isn’t in a standardised format, so they are having to do a lot of work cleaning up the data into a useable format. BUT, she added:
“At a first look there are interesting differences in numbers of infections and immunizations. We think this will be an important data point but are only at the beginning of looking at it”.
Wouldn’t that be something – having the CDC document that would really wake up the medical world. That’s the power of a study like this 🙂
We are very pleased to see the fruits from the letter PANDORA sent to Dr. Unger upon her appointment. That letter urged the CDC to have ongoing collaborations with ME/CFS experts, change the diagnostic criteria (which is what this study aims to do) and use patients for studies from experts who know best how to recognize the disease. http://pandoraorg.net/uploads/Welcome_Unger___Urge_Change.pdf
Now, one of the requests in that letter is to change the name. With a new definition and with the power the CDC has, this is the optimal time to address the name issue.
Thanks Tina – I think the PANDORA letter probably touched off quite a bit. That was a great idea and a great advocacy effort and I hope PANDORA/CFS Solutions and other groups continue to bring the orgs together like that.
Thank God that the CDC is finally helping. Really taking the reins.
One thought came to mind about this study from the perspective of a Canadian – does financial resources skew the demographics of the study. I took note that most participants were well educated and of course had the resources to access these clinics. What happens to those who do not have the wealth and/or the insurance to access the specialized care of these clinics? Are people who are the sickest also be the most likely to liquidate their assets and have family members liquidate their assets to receive care?
While the study is a positive step forward. I think it has to be seen as a first step rather than the definite step. I think it is quite possible that the numbers would be a lot different if the study were done where their was a single tier medical system.
“does financial resources skew the demographics of the study”
Definitely. Beth Unger commented on the finding that 95.4% of the study particpants were white, saying “we think this is a really good sign of access to care that we have to address in a concerted effort.”.
“Are people who are the sickest also be the most likely to liquidate their assets and have family members liquidate their assets to receive care?”
In terms of severtity, I’m not sure it makes much difference, at least judging by a couple of very large clinic-based studies in the UK: both were similar to the CDC sample in terms of fatigue and function. And of course the UK has a universal health-care system, like Canada (though provides no specialist care for MECFS patients too ill to attend outpatient clinics).
I’m in the severe 25% group. Bedridden, housebound, high viral load, forgotten and almost hope-less. I tried to make appointments by a few high profiled physicians and found that a lot do not accept severely ill patients. From a few docs I had the impression they rather treat younger patients who have been ill a max of 5 years. This increases their success rate and looks good for their records and practice and papers that they publish.
They were not really enthusiastic about a 58 year old ill for 30 years and were rather negative in their response. I felt like they just signed my death certificate.
It’s not the question if the researchers will get access to the severely ill, they only have to reach to them to get them involved. But so far no one has wanted to go that extra mile. People might point out that the severely ill are not included, fact is no one gives a hoot, at least not enough to reach out to them at home and get them involved.
Am I bitter and sarcastic? Yes a bit. In those 30 years I spend many years advocating, now I’m too ill to do much more than participating in questionnaires, surveys, sign petitions and write to congress. I am forgotten and left to rot. All those years advocating did not help me in the end. Cause that’s how it feels, the end.
Sorry to hear that Christine. I don’t know physicians but I imagine Dr. Peterson would see you if you could get to him. From what I’ve seen his patients range from young to quite old. I was encouraged by Dr. Peterson’s results with Vistide; those patients weren’t a huge part of his population but I have the feeling that age didn’t necessarily make a difference.
For me, I think you did the right thing – you answered the call – a call you must have felt very strongly – you had a yearning to make a difference…and I salute you for that. Hopefully we’ll all see success at some point.
All I can say is we’re in your debt. I was thinking just today about ‘failure’ and I realized that every venture, no matter how good, has the possibility of ending in failure or at least not complete success. All you can do is step forward and I applaud you for doing that…
That’s really tough, Christine, and I understand why you feel like that. I hope that things will improve for you, and that researchers will start reaching out to people like you. And thanks for the advocacy you do.
Cort , yours and other prominent activists view re the bedbound unsettles me. I hate to say it as you do very good work.:)
IMO The bedbound like me deserve research In our own right. We are the sickest – it’s bad not being able to work? imagine not being able to sit, speak or see family for yrs. It’s precisely because of all the complications / extra damage of getting severe that standard ME research won’t be enough to get us really better i don’t think. We need our complexities examined and attempts made to help us through, with the evolving knowledge coming through from general ME research.
It’s debatable who are best to research for general ME research – I’m not intersted in broader CFS – I would say people who clearly meet good criteria ICC etc (without co morbid MH , screened if possible for purity).
But the arguers to exclude the severely affected for mainstream research aren’t also advocating for special severe ME research instead, it Seems to be just do nothing at all with that group which i can’t countenance.
Maybe I’m wrong, but I think the severely affected have a higher profile in the UK, with one charity, “The 25% ME Group” dedicated to the most severely affected patients, http://www.25megroup.org/. Though still very little research on the severely-affected here.
Perhaps the answer is to start research on those able to make it to clinics but then roll promising research to take in severely-affected patients. This would need to be specified at the start of studies, and included in funding bids, with a tranche of money held back to be used to recruit severely affected patients if the intial results justify it. As I said before, in any other illness the most severe cases are of great interest to researchers. Sure, it isn’t easy to include severely-affected cases in studies, but I agree that more effort should be made to gather data on a very important group.
Turns out that Sonia Marshall-Gradisnik IS studying severely-affected (bedridden) patients in Australia:
http://news.ninemsn.com.au/health/2013/05/15/15/04/aust-bid-to-solve-chronic-fatigue-riddle
“She is delighted the university and the Gold Coast Hospital and Health Service have set up a world-leading National Centre for Neuroimmunology and Emerging Diseases, which facilitates efficient communication between researchers, doctors, nurses and and patients.
She says the close proximity of the centre to the hospital is the only model internationally where researchers have direct access to severely ill bedridden patients.”
UNGER ON INCLUDING PATIENTS, CFSAC MEET:
[from PR article http://forums.phoenixrising.me/index.php?threads/the-bar-has-been-raised-cfsac-spring-2013-day-one.23422/#post-358327%5D
“Nancy Lee asked whether any bedbound patients are included in the CDC’s study.
No, said Unger: they talked to physicians to try to do that, but by definition the patients in the study are able to get to their doctor’s office.
They’d discussed what to do about this problem, and felt they should complete the study even so, but they’re aware that there is this house-bound group that we’re not reaching and they’re discussing what to do about that.”
Good to hear they have at least recognised the study and I hope the CDC and participating clinics will take action to include more severely-affected patients.
I was on Ampligen for a year and felt 60% better. Two years later I’m in the lazyboy or bed. Two months off Ampligen I lost my much improved health. If I had the money I would have moved to Charlotte and get back on Ampligen. I was disappointed like many when Unger shut down the approval and yes she is responsible. Had she voted yes it would have went through and I could walk my dogs, no more IBS, carry on a conversation, less pain and fatigue. Sorry if I’m unable to jump on the Unger’s helping us bandwagon lol. I pray every night for a FDA treatment, cure or for GOD to take me in my sleep and end the suffering. You can only go on so long in this condition but for the people who have taken their life I admire their courage. It’s not a normal thought process like going into a burning building. These people couldn’t wait another thirty years of inhumane treatment by the government. My life is worthless without ampligen and Unger and her Masters don’t care. Shouldn’t compassionate care apply if you’re a responder to Ampligen? We spent 50K for me to move to Charlotte for Ampligen and it looks like it was a huge mistake! Even though Hemespherix and Dr. Lapp no how much better I was after a year of Ampligen. I’m a Veteran and worked for 27 years paying into the system until almost four years ago. I waited 27 months for my disability hearing in Charlotte which cost a grand and turned out I didn’t need to go! Two hours before the hearing the ALJ read my file and cancelled my hearing. I was approved for disability but my lawyer got 6 grand of my back pay lol. 80% are approved once in front of ALJ ! Oh but he threw in a mandatory CDR in 24 months and said I’m expected to improve with appropriate treatment! There isn’t a FDA treatment much less appropriate so I guess he’s a Doctor too…. I’m done……
Simon, just wondering are the slides publicly available somewhere?
You can reply off-list, as it were, if you prefer.
Thanks.
This was a great post, Simon. When I read this initially I was thrilled to see the CDC finally do what they should have done a quarter of a century ago — even as I agree about the unfortunate lack of housebound patients, as well as poor and patients of color. But after reading Jennie Spotila’s post reviewing the recent CFSAC meeting in which Dr. Unger said that 2-day CPET will NOT be used in this multi-center study, I’m now quite concerned. Do we have any idea what kind of “stressing” of these (clearly heroic!) patients will be included beyond the stress of filling out 5 hours worth questionnaires? What I would think has become quite clear since Snell et. al. published their initial finding a decade ago is that some form of stress/cardiopulmonary exercise is essential for finding abnormalities. True, there are abnormalities that will pop up without stressing the patient (or do they? given how inconsistent even the most consistent findings are, who knows?). But given the centrality of exercise-induced exacerbation of the entire global symptom complex in this disease, the lack of an exercise test in developing what appears to be the definition-to-end-all-other-definitions is concerning in the extreme.
Hi Michelle, and thanks for the kind feedback.
During the FDA talk Beth Unger said that for a subset there will be more and different data gathered: blood to look for biological markers, plus cognitive tests and exercise tests
So I assumed there would be exercise testing of some sort.
And I’m actually not sure what the best exercise test would be at this stage. At the FDA meet, where Jennifer Spotilla pointed out Chris Snell presented about his exercise testing (just before Unger spoke!), he put up a slide showing a decline in maximal oxygen used on the repeat testing for patients but not controls. I think this is the work that has been mentioned so often before. However, he also said that was based on a sample size of just 6, and that’s no basis to define a test as ‘definitive’. They have recently repeated the study on a larger sample (51 patients) and this time found NO statistically significant difference between the inital test and repeat test for CFS patients. In some ways this is quite shocking, though perhaps not surprising given the tiny initial study.
The results have apparently been accepted for publication, and include an interesting finding that although peak oxygen use doesn’t decline, EFFICIENCY at anaerobic threshold does decline dramatically. These new findings could be very relevant, although they really need replicating in an independent sample. I’d like to think that Chris Snell would use the new results, once published, to engage Beth Unger about how best to do the planned CDC exercise testing. Though if the physicians don’t want to do a 2-day test, that is going to be tricky.
Incidentally, the Lights found significant differences in gene expression using a single sub-maximal (‘moderate’) exercise regime and I wonder if a moderate stress test would be more appropriate, since for many of us that would be enough to provoke symptoms (I couldn’t do 1 max test, let alone 2 on successive days).
Hi Simon,
Thanks for your response. I haven’t actually been able to watch the FDA meetings (indeed I think I’ve been more proactive online — i.e commenting — in the last two weeks than I have been in the last two years!) so I should note that all of my thoughts regarding them are based solely on the summaries of others.
Yes the paper everyone refers to, VanNess, et al. “Diminished Cardiopulmonary Capacity During Post-Exertional Malaise” Journal of CFS 2007, is an n=6 study, though it is indeed shocking if their larger study of 51 patients shows no difference after all the years of hearing otherwise (and I may yet slog through the FDA presentations to hear this). In reviewing the rest of their research, I can see that it’s been more ambivalent, sometimes with well over 100 patients and controls but not the two day testing, or with a similar number of patients and two day testing but no controls. My understanding is that over the years they’ve actually tested far more patients for insurance purposes but without that work being published, it’s not very helpful with regard to review — though maybe it is with regard to answering CDC’s current question of how do providers decide what ME/CFS looks like (perhaps Peterson is answering this question for the PFL/Workwell group?). I’ve also heard/read Ms Stevens mention in the past that about 50% of ME/CFS patients have the abnormal response to the second day of testing, but, again, it looks like their upcoming published data may say something else. Their work has been replicated by Vermeulen et. al. in 2010 but still with only n=15 (which I had confused w/the VanNess paper above causing me hours of trying to find where this n=6 study was until I finally just called up my copy of VanNess from my hard drive…brain fog is so effing fun!). I keep thinking there was a Spanish study that came out just after the PACE study that used a similar protocol, but perhaps it was just submaximal?
As you point out, the Lights were able to get their findings with a submaximal test, and Nijs and De Meirleir as well as Natelson’s group have been successfully using one-day CPET (indeed his group has been using elements of CPET since the late 90s),* and thus I’m not necessarily opposed to submaximal testing (especially as I know I’d need a gurney and ambulance to get to a second day of testing!). And I agree with you that insisting on the test-retest protocol may not be warranted at this time given such conflicting research (though I hope it’s not off the table because it would cost too much to, say, just admit patients to hospital during the testing). But I do want to make certain that there is some exercise testing in this multi-center CDC study. Blood work without stressing the patient first seems, if not completely pointless, at least not as helpful as it could be.
And can I just say that at this point in the game I am weary to death of ME/CFS studies that are anything less than n=100 (sorry to sound so melodramatic but…seriously, it’s craziness!). Had NIH just funded the PFL/Workwell group years ago, we might well have already had our much larger studies of the test-retest protocol and had a clearer idea of what sort of testing would be best. And I might well have not just spent several hours of my precious online time/energy hunting down a mini-bibliography of CPET and ME/CFS. 😉 I do hope CDC is spending at least as much time on this question — for all our sakes.
*To me, this study, which found a five-day delay in PEM after exercise using what looks like a tripped-out HR monitor, was really interesting given that my crashes often take about that long to happen after overdoing it. But, as always with this disease, it’s a very small study (n=9).