

Tina Tidmore is an “Independent/Freelance Communications Specialist” who has assisted several ME/CFS organizations including the Open Medicine Foundation, Jarred Younger’s Neuroinflammation and Fatigue Lab, and PANDORA. During her seven years as the editor of the Clay News newspaper in Alabama, she successfully (and courageously) fought three First Amendment battle and uncovered and reported on a $4.5 million Ponzi scheme in her city. She also has a long-standing case of ME/CFS. Thanks very much to Tina for allowing Health Rising to run her blog originally titled “Introducing Victor Darley-Usmar, PhD, an Alabama Researcher Now Helping in a SEID Study“
…………………………………………………………………..
Day after day, from my bed, I watch my social media newsfeeds for some news on my disease, especially for anything happening locally in Alabama. But news, by nature, often comes when not expected. And this happened in October, while I was watching a video from Open Medicine Foundation of a presentation at the International Association of CFS/ME conference.
Dr. Jon Kaiser was speaking – and he said:
“There’s a researcher named Victor Darley-Usmar at the University of Alabama, who works with the Seahorse company” and I think he’s a genius. He is developing an equation to take all the data that the Seahorse tests provides and distill it down into a single number – he calls it the ‘BHI,’ the bioenergetic health index. So, you know, it would be like getting a PSA or [inaudible]. You get a bioenergetic health index from a blood sample, looking at white blood cell mitochondrial energy production. So I think that’s the cutting edge of this field, and once we start sending our patients who present with ME/CFS, just as an example, we can start [inaudible] whether their disease severity winds up with the severity in their mitochondrial [inaudible].”
Who is Victor Darley-Usmar, PhD?
Living in a major metropolitan city that has always been absent expert clinical care for my disease and, from 2003 to 2014, no research in the disease, I get excited when the name of a researcher or doctor in my part of Alabama is connected to systemic exertion intolerance disease (aka “SEID” or “ME/CFS”). I wondered just who this “genius” is right here in Birmingham and what has he done that may help people with my disease.
My Google search took me to Wikipedia, which tells me Victor Darley-Usmar, PhD, was born in England and that he is a “free radical biologist and biochemist” and the UAB endowed professor in Mitochondrial Medicine and Pathology. (Note: “UAB” stands for the University of Alabama at Birmingham, which is different from the University of Alabama. UAB is well-known, even internationally, for medical care -especially cardiac and AIDS – and medical research.)
Darley-Usmar’s career journey included stops at the University of Oregon for a postdoctoral fellowship from 1980-1983, appointment as assistant professor at Japan’s Tsukuba Medical School for 2 years, then to Kent, England, to work as a senior biochemist at Wellcome Research Laboratories for 10 years. Then UAB recruited him to the Heart of Dixie, the land of fried chicken and sweet tea, right here in sweet home Alabama. He’s been here for over 20 years.
He has a profile on UAB’s website, but he said it needs updating, so he prefers the information in a bio he sent me. It says he’s in the Department of Pathology. He has received “multiple awards for training and mentoring and served as the Associate Dean for Post-Doctoral Education and the Pathology Graduate Program Director”. It says “He established the UAB Center for Free Radical Biology from 2006-2015 as an international center for research in redox biology.” And, it further says: “In his own research program he has been instrumental in defining how redox biology modifies mitochondrial function in pathology and in recognition of these achievements was awarded a Lifetime Achievement Award by the Society for Free Radical Biology and Medicine in 2012…. He was a recent recipient of the prestigious ‘Creativity is a Decision’ and ‘Blue Sky’ awards from UAB for the Bioenergetic Health Index concept. He has been continuously funded by NIH for 20 years and has published over 300 articles with an H factor of 92.”
For a recent interview, I found Darley-Usmar in the 5th floor of a Birmingham brick building, part of the UAB campus, which takes up about a third to half of the downtown grid. His office has the standard elements of desk, computer, and chair, but it is rectangular to include a small conference table and a white board attached to the wall opposite his desk. Sitting on the table are a projector and the connected laptop to show charts for explaining the science, which he was glad to have the opportunity to do for this unlearned interviewer.

His First Experience with a “Fatigue Syndrome” Patient
His first connection to what he calls “fatigue syndromes” was as a post-doc in Oregon in 1980, when his boss was asked to help figure out the cause of a patient’s fatigue, suspected to be a mitochondrial dysfunction. They found a deficiency in one of the mitochondrial proteins in that patient. “So I always had the point of view that these were real things because I had one straight off that was real,” he said. And he said there are documented genetic mitochondrial dysfunctions that cause “fatigue syndromes,” and drugs that alter the mitochondria behavior that cause “fatigue syndromes” so he figured there could be other mitochondrial-based malfunctions leading to fatigue-causing diseases. “Fatigue, in the end, is a disease of metabolism, isn’t it?” said Darley-Usmar. “And there’s a limit to how many things can go wrong; it’s not infinite.” In some cases, it could be metabolism dysfunction is not the driver of a person’s symptoms but is a result of something else, he said.
(Personal comment: Just imagine what could have happened if he went into studying our disease back then!)
After that experience in Oregon, for about 3 decades, his research was mostly in cells and mice. Then, “About 5 or 6 years ago, I said I want to do research in patients,” he said. He felt the testing was good enough to be “translated” into human experiments. This led him to studying bioenergy health in HIV patients at UAB’s well-known HIV clinic. Those patients, who have seen much progress in treatments preventing death, are still experiencing fatigue and premature aging, he was told. And since he is at UAB, his research has been in patients who are already being cared for through UAB’s clinical care services. He’s also studied bioenergetics in alcoholic liver disease, diabetes, and kidney disease.
(Note from me: This shows how clinical care can help spur more SEID research.)
And he was also told of other “fatigue syndromes” using the test created at Seahorse, such as a post-cancer-treatment fatigue syndrome. “It told me there is an unmet need for a clinical test” of bioenergetic health, he said, in addition to its research usefulness. And that led to his working with Seahorse to create a test to measure it.
About the Test
The Seahorse XFE24 Analyzer
Seahorse Bioenergetics, now Agilent, has created three machines. The company’s website says: “Seahorse XF Analyzers measure the oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) of live cells in a multi-well plate to interrogate key cellular functions such as mitochondrial respiration and glycolysis. The instruments perform compound addition and mixing, label-free detection, and automatic calculation of OCR and ECAR in real time.” Darley-Usmar said it more plainly: “It measures oxygen and protons.” He said it is a “break-through technology.”
According to Darley-Usmar, this bioenergetic health reading shows the cell’s ability to respond to an ATP (adenosine triphosphate, an energy molecule) demand. So it is measuring the cellular energy production capacity, the cell’s ability to produce energy molecules as needed. And there are so many things that can diminish this capacity, which is why he believes the “fatigue syndromes” likely have many different causes.
The test is not clinically useful, yet, but he and Agilent and UAB and the Foundation for Mitochondrial Medicine, a charity, are working toward that. As Kaiser said, the goal is to take the Seahorse machine readings of multiple factors and have it translated into a one-figure score that says what the cell’s energy production capacity is.
This reminded me of the cardiopulmonary exercise test (CPET), which has been used to show SEID patients are unable to normally use the aerobic system (using oxygen to create energy) a day (or two or three) after they were put under a high-energy demand. In other words, their oxygen-based energy-producing capacity is reduced because of exercising the day before, so they go into a predominant anaerobic (not using oxygen) energy-production system quicker. Anaerobic energy production produces damaging ethanol and lactic acid, which is why you cannot last long in an activity if the energy you’re using is mostly from the anaerobic system.
It sounded to me like this bioenergy health index may measure the same thing on a cellular and chemical level in the blood rather than from the gases in the breath and the heart rate, as the CPET does.
Darley-Usmar showed me a chart with a sliding scale of cellular energy-producing capacity (aka bioenergetic health). The top level, he said, may correlate to aerobic energy mode whereas a person with low bioenergetic health, according to the blood test, is more in the anaerobic mode, cellularly speaking. The CPET shows a person has an energy-production problem, but testing the capacity of the cells may give clues as to the reason why, he said.
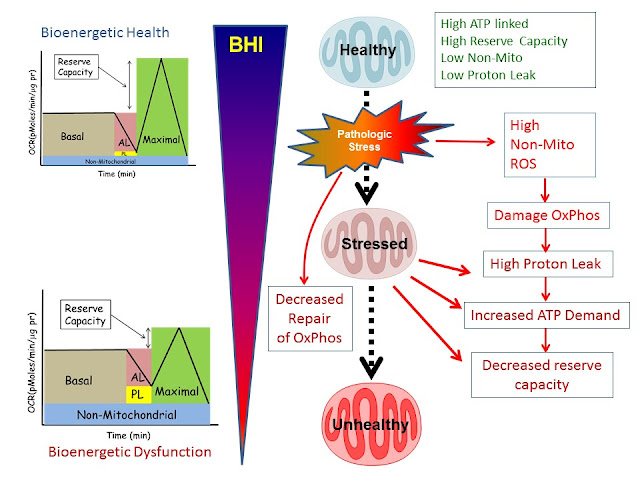 |
| BHI as a dynamic measure of the response of the body to stress. In this scheme, healthy subjects have a high BHI with a high bioenergetic reserve capacity, high ATP-linked respiration and low proton leak. The population of mitochondria is maintained by regenerative biogenesis. During normal metabolism, a sub-healthy mitochondrial population, still capable of meeting the energetic demand of the cell, accumulates functional defects, which can be repaired or turned over by mitophagy.Chronic metabolic stress induces damage in the mitochondrial respiratory machinery by progressively decreasing mitochondrial function. This manifests as low ATP linked respiration, low reserve capacity and high non-mitochondrial (e.g. ROS generation) respiration. These bioenergetically inefficient, damaged mitochondria exhibit increased proton leak and require higher levels of ATP for maintaining organelle integrity, which increases the basal oxygen consumption. In addition, chronic metabolic stress also promotes mitochondrial superoxide generation leading to increased oxidative stress, which can amplify mitochondrial damage, the population of unhealthy mitochondria and basal cellular energy requirements. The persistence of unhealthy mitochondria damages the mitochondrial DNA (mtDNA), which impairs the integrity of the biogenesis program, leading to a progressive deterioration in bioenergetic function, which we propose can be identified by changes in different parameters of the bioenergetics profile and decreasing BHI. |
How He Got Involved in SEID Research
Recent discoveries in our disease have brought our scientists to Darley-Usmar and to mitochondrial function testing, more so than his coming to our field.
I have heard of some theories over the decades in relation to SEID and mitochondria function and the NO/ONOO cycle (increase in nitric oxide and peroxynitrite, causing oxidative stress). But mitochondria-related studies have taken over much of the research interest of our disease in the last two years. This matches the interest of mitochondrial research in general, in other diseases.
His first contact from someone from the SEID field was Dr. Jon Kaiser, with K Pax, who just called him up one day. But then, researchers from Nevada, Ruben Dagda, Phd, and Isabel Silvestre, Phd, asked him to help set up a study they want to do on bioenergetic health in natural killer cells in SEID patients. He plans to visit the research team there this summer.
This networking and camaraderie is often how joint projects come about; it’s word of mouth. “They took the time and effort to try to understand what I was saying about the bionergetic health index, he said. And they explained their theory to him.
The Nevada-based study, titled “The Bioenergetic Health Index of NK Cells as a Diagnostic Test for Chronic Fatigue Syndrome,” has been funded by the Solve ME/CFS Initiative Ramsey Awards. The abstract points out, “Mitochondrial dysfunction has been reported in CFS. However, the extent by which the metabolic profiles of lymphocytes [natural killer cells] is associated with immune dysfunction remains to be elucidated.”
Previous research, going back to the late 1980s, has revealed that NK cells don’t function well in this disease and seem to die before reaching maturity.
The potential impact of this study is that it may lead to a clinically useful test and may contribute to the knowledge of the disease that may point to a target for a treatment clinical trial.
How Useful Could a Blood Test for BHI Be?
- When you have an intervention to test, this bioenergetic health index can measure whether that intervention is causing a molecular change, thus reducing any fatigue treatment placebo effect corrupting study results. “Lots and lots of people take supplements [for energy], which may or may not have any effect on our biology,” said Darley-Usmar. So it can be measured molecularly whether any of these supplements actually enhance the cellular energy-production capacity.
- If you know the particular mechanism of the diminished cellular energy production in a certain condition, then you can possibly figure out what intervention might improve it. So the test may point to what treatments ought to be tried for different conditions.
- It may be used to predict the outcome of a treatment for some diseases. “If your metabolism is stronger before you have a clinical procedure or therapeutic or intervention, then the chance of your outcome being better goes up,” said Darley-Usmar. Bioenergetic health testing may reveal why some do better on treatments, while others don’t do as well.
- It can be used to see the differing bioenergy health of different cells within one body. For example, a person could have high muscle energy capacity and not feel fatigue, but the immune system energy capacity could be diminished, contributing to a disease. Darley-Usmar already did this with heart valve replacement patients. The cells around the heart were diminished in their bioenergetic health, but the cells in the blood taken from the arm were not.
- In a clinical setting, it can validate the patient complaint of fatigue as being real and objectively measurable and may replace the more painful test of muscle biopsies.
- It may identify those with “fatigue syndromes” that have mitochondrial dysfunction and separate them from those who may have another cause for their fatigue. To achieve this, mitochondrial studies with many SEID subjects are needed.
Recognition of Role of Mitochondrial Dysfunctions in Diseases
There are a few mitochondrial disease clinicians. But the problem is having clinical tests, Darley-Usmar said. But that is improving. “We now know the mitochondria can change the genes in the nucleus pretty dramatically,” he said. “The idea that mitochondria are part of the problem in cardiovascular disease, in diabetes, in neurodegenerative disease is completely accepted at the research level." But all of this will only get into clinical care when there is a test and a treatment for these mitochondrial dysfunctions. He said there are some interesting drugs “coming into the mitochondrial space.”
Not Yet Connected to Other SEID Researchers at UAB
Darley-Usmar has not yet connected with the two other SEID researchers at UAB: Kevin Fontaine, PhD, who is working with Dr. Peter Rowe; and Jarred Younger, PhD, who is researching SEID and fibromyalgia from the neuroinflammation angle.
But, Darley-Usmar is collaborating with the UAB Undiagnosed Disease Program, and they have people that come in with “fatigue syndromes.” However, to do a study on SEID, he would need to have a clinical connection to patients with SEID.
He is open to helping other researchers of this disease. He described the post-exertional malaise (activity-induced symptom exacerbation) as a “powerful paradigm” for doing a study. He said the patient can be her own baseline for comparison of BHI on good days and bad days.






Thank you for your blog, Tina! I recently moved to Nashville and I wonder if you know of anyone doing research or clinical work here? Also, until I heard you use SEID, I haven’t heard anyone else use it. I know the IOM report tried to rename ME/CFS but the patient community seems to have rejected the name. Has the name caught on in the South? Thanks, Esther
With the increasing focus on energy production (or the lack of it) in ME/CFS I wonder if SEID would not be received better now (????) although the deeper researchers get into this illness the better the name we will get.
Esther, no, it’s not caught on. But it won’t unless people start using it. And I have written about how upsetting it was that so many patients rejected the term. But I won’t go into the reasons why. But since there are so many names, and I have seen SEID in news articles, I guess we can choose. So I made my choice. Change won’t happen from the status quo on the name unless we change what name we use.
Sorry, I am not aware of any research in Nashville.
I didn’t know you had written that you were upset when so many patients rejected the name SEID. I, too, was upset. It also upsets me that so many people blithely choose a psychiatric term–PEM–to describe how they are affected by exertion. If what they suffer from is malaise, they must have a disease that is very different from SEID.
I too was stunned when the name SEID was rejected, the name describes the core of the disease I have. Well rested I have far less ICC symptoms than on bad days. Symptom load is directly related to exertion. It doesnt make any sense to me to stick with criteria that rely on not resting to get well. Severely ill yet low symptom load if stay in bed …We were offered a line in the sand a move away from the CFS and ME confusion and rejected it!!! Wessley and White et al must of been so so happy.
Well, maybe we three need to get together. I sent an email to CDC months ago about a conversation I had where the “systemic exertion intolerance disease” and a 1-sentence description based on that name helped someone understand the disease more than anything else I had tried. Dr. Unger’s response was to just thank me for sharing.
I too don’t like “PEM.” Best I came up with is “activity-induced sickness symptoms.” Most people understand what you mean when you say, “I feel sick.”
Connect with me at tina@tidcom.net if you want to try to do something about this. I can’t drive an effort, though.
It would be great to elucidate exactly what cells are experiencing mitochondrial dysfunction. It is appreciated that hypoxia or ischemia to the brain and spinal cord cause changes in oxidative metabolism in affected nerve cells.
Shokei Yamada and colleagues discuss much of this in their publications on the pathophysiology of tethered cord syndrome. They found that when oxygenation of the brain or spinal cord was decreased, cytochrome a1 a3 was increasingly reduced, and energy production decreased. They measured these redox shifts with noninvasive reflection spectrophotometry.
So mitochondria dysfunction may be as “simple” as inadequate oxygen supply.
Thanks. I wouldn’t be surprised at all if an inadequate oxygen supply due to blood vessel problems isn’t a major issue. That’s what Shungu believes is happening in the brains of ME/CFS patients.
Cort
I totally agree with you..
I am so short of breath due to what I prefer to call myalgic encephalomyelitis…what my internist diagnosed me with in 1994.
Better name than CFS or CFIDs and fibromyalgia..
Husband also…has all the above … too.
We both have mcs illness also..
He was diagnosed by the same internist in 1996..
I have chest tightness and so short of breath I rarely talk on the phone. Even bending over to pick up a pencil
when I stand back up ..shortness of breath..for all these years..
I do think as you do that is is inadequate oxygen due to blood vessel problems…
I was glad to see the article from the person in alabama I have been to the same center they have been to at UAB to infectious disease specialists 24 years ago and there was nothing they could do
at that time they were skeptical of the disease
however since my internist had diagnosed me in 1994 and I had taken with me a copy of his diagnosis on paper
they would acknowledge it but barely when I requested a copy of that days office visit notes..from the infectious disease young doctor..
I was disappointed..in the infectious disease doctors notes..but he was polite.
If I had not been diagnosed already I would not have gotten a diagnosis from the infectious disease doctor that day…and had traveled a long distance…
I would like to be able to breathe and to stand up without leaning on something ..
if I keep moving fast that is the only way I can walk in a store or outside or inside..
once I slow down I have to sit down or lean on something like the door frame…I can never stand in a long line
or stand still and talk to someone..
Sheri in Alabama
Very interesting blog. Lack of oxygen was suggested in the 1980’s so sad it was not followed up. SEID does not describe the reality of ME/CFS, only one of its symptoms. It is a Multi-system illness which is only adequately described by the Myalgic Encephalomyelitis International Consensus Primer -2012-11-26. My personal reaction and prolonged crash when accidenally exposed to synthetically produced fragrances and chemicals is very frightening, living a life trying to avoid these chemicals verges on the impossible. How many of us are virtually trying to do just that? Has anyone dared to propose that our bodies are producing a natural and correct response when subjected to the increasing poisoning of our environment?
I would flip it on its head and propose that our bodies are producing an unnatural response to chemicals that the vast majority of people have absolutely no problem with – not that our environment is not being poisoned to some degree, I believe it is – but that the main problem is with our systems.
I have MCS as well, by the way.
Cort,
I like your comment, ” an unnatural response to chemicals.” This is exactly what porphyria is. As I mentioned ( somewhere) I had 2 very deep red brown urines just a few weeks ago. Went to my doc. He re- did urinalysis/ blood work and there was no blood in urine, no gout chemicals, all was fine. However, the original dark urine was not tested.
I could have easily missed this. It never occurred previously or since – that I know of. I understand that porphyria can be sporadic and hard to diagnose. Porphyrins are neurotoxic, and can “gum up” metabolic pathways. It is known to be induced by various fumes.
What about exposing people to an offending chemical and then running their urine/ blood through complete analysis – like a spectrophotometric analysis.
This may not be porphyria, but something similar???
My commiserataions Cort on you being another ‘canary down the mine’. Insecticdes, biocides, fungicides,neurotoxins are all chemicals designed to interfere with LIFE. DDT, from which I suffered 20 months of exposure, Agent Orange etc. The dose used to kill small living creatures will obviously affect similar systems in larger creatures to a certain degree. The more frequent the exposure the more sensitive you can become. I (& you?) are now in that proportion of humanity who are pathologically sensitised to chemicals, including fragrances in perfumes, soaps, cleaning agents, paint, cigarette smoke…..
I suggest an increasing proportion of those not severely affected to the point of disability ARE affected to the degree of unreasonable and uncontrollable flashes of anger which lead to domestic violence, road rage etc. Head and neckaches, the feeling on being on fast forward, that you are disintegrating from the inside out, being sensitive to food and chemicals is undermining humanities very being.
Paper Published by Team at McMaster University in Hamilton, Ontario, Canada which is saying CFIDS is radiation injuries they have also put out
now a Book with one full complete Chapter on how CFIDS is tied to Radiation Sickness I know there is Positive urine samples on Uranium or Plutonium found these are Government tests.The work was funded by The
National CFIDS Foundation the Paper & Book links can be found on their site or contact Gail Kansky…Me, I want the truth not lies or false hopes no matter who is right & I still feel countless have been
Poisoned by Antibiotics & there is n doubts now that the Spinal Brain Dura is Leaking spinal fluids & has nothing to do with a POTS diagnosis at all that is a false Assumption http://www.floxiehope.com
Well, Aiden, as was said in the Seahorse article, there are probably many causes of ME/CFS/SEID including radiation exposure and also poisoning from such things as certain antibiotics. I can corroborate the problems with Fluoroquinolones as I experienced nastigmus (uncontrolled eye movements) when I was once prescribed Cipro. Years later, it finally has a black box warning that it can also affect the eyes.
As far as radiation exposure goes, depleted uranium usage is something that most people don’t know about. It has been used in the Middle Eastern conflicts for over a decade but only recently has received much media attention–and is probably still being employed despite military efforts to downplay its use. http://foreignpolicy.com/2017/02/14/the-united-states-used-depleted-uranium-in-syria/
That could be the cause of mitochondrial malfunction (for veterans)–along with the hundreds of other man made chemicals (that are commonly carried in most of us from ‘developed nations’) not usually found in the natural environment.
Just a thought of mine…..did anyone ever do a study with Fibromyalgia and/or CFS patients with Hyperbaric Chamber treatments? This would definitely increase oxygen to all the cells in the body. And if a virus or bacteria is causing this that lives in an anaerobic environment, you would think the high oxygen levels introduced to the patient, may kill off the virus/bacteria and if it did, we would be cured. I would love to do this if I had the money for it, cause it’s not FDA approved for this and insurance companies won’t cover it.
I do HBOT and have gotten some benefit. It is covered by my insurance for wound healing but not for CFS or killing bacteria and viruses.
Your analysis of the theory is correct – oxygen therapies can be used against viruses and bacteria. Ozone has been successfully used to kill Ebola.
As for HBOT and CFS, here’s one small study showing promise:
https://www.ncbi.nlm.nih.gov/pubmed/23682549
There are other oxygen modalities as well… ozone IVs, rectal ozone, ultraviolet blood irradiation, and major auto hemp ozone therapy. It has been used in Cuba, Germany, Russia, and Italy, with good results.
As for oxidative stress, it is possible, but they’ve found the oxygen actually does good things for tissues.
Sorry, I hit submit too soon…
This article describes how oxygen therapies work and the author, Bocci, has 2 detailed books out on the topic.
Drs. Frank Schallenberger and Robert Rowan use it extensively in the US and have publications as well.
I get HBOT treatments for about $45 at a small local center run by a doctor from Russia.
Here’s a blog on a fibromyalgia HBOT study that got good results – https://www.healthrising.org/forums/threads/new-age-fluff-or-real-treatment-fibromyalgia-hyperbaric-oxygen-therapy-study-opens-eyes.2688/
I just talked to researcher whose studies (not yet published) are finding major problems with oxygen utilization in ME/CFS, FM and similar diseases. A blog is coming up.
The article:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3231820/
Thanks for the blog, Tina. Did you mean to say that humans produce ethanol as part of the cellular respiration process? I thought only anaerobic micro-organisms do.
The research happening on AIDS patients in the 80s is the kind that Dr. Klimas was involved in – psychoneuroimmunology. I’ve just discovered it to my dismay. The idea that our thinking will make us physically sick. What psychoneuroimmunology does not consider is that the tissue repair system and the immune system are one and the same systems. White blood cells are small and like amoebas; some act as garbage cleaners, some act as immune system sentinels and yet some act to dissolve/maintenance/construction connective tissue. Dr. Peter Rowe has found that puberty and menopause can cause great symptom flares in ME/CFS/EDS. (In fact, Dr. Rowe’s specialties include ME/CFS as well as a connective tissue disorder, Ehlers Danlos Syndrome.) During puberty and menopause there is much increased cell signalling for tissue building and dissolving. If our adipose tissues, which is connective tissue and hold ATP cells in storage for cell respiration when needed, is degraded due to connective tissue disease, then maybe this is why we can’t produce energy like we used to or like everyone else.
Would just like to add that everyone uses anaerobic energy when needed for maximal effort. Though it does not produce ATP cells as prolifically, the process is apparently 100 times faster than aerobic energy production. Excess lactate goes to the liver to be reused.
Aerobic energy production is not without it’s downside: we do not efficiently process about 2% of the oxygen we take into our bodies. So 2% of the oxygen we take in ends up poisoning us. It’s called the oxygen paradox. “Oxidative stress” has been widely misused by researchers and clinicians so that stupid and innappropriate therapies have been recommended for some. According to Dr. Charles Cantor, Molecular Geneticist, OXYGEN WILL AGGRAVATE central nervous system disorders, including dementia and blindness. If we have POTS, we may fall into this category of conditions which oxygen supplementation will aggravate. https://www.ncbi.nlm.nih.gov/pubmed/27095211
https://www.facebook.com/ideacityonline/videos/667197896753633
Tina, I would urge Dr. D-U to look into connective tissue disorders as the cause of the physical illness of ME/CFS/FM/MCS. Interestingly, blood plasma is connective tissue. Muscle is not. Wouldn’t it be interesting if the reason that the heart valve replacement tests came out differently is because of inherent connective tissue disorder? Dr. Ron Davis says that the mitochondria IN THE PLASMA is wonky; out of the plasma it is not. Worth looking into.
Laura, I did mean to say that. But it is an error, evidently. Thank you for bringing it to my attention.
Genetic testing will determine if one has more fast twitch muscle fibre, common in elite atheletes. If one does, and one has connective tissue disease, perhaps the body, being failed by connective tissue, is powering the fast twitch muscles through anaerobic respiration which is the only choice to keep the body going at the moment. Perhaps this is another difference between those who are mainly bedridden – they don’t have as much fast twitch muscle, so take longer to develop their anaerobic respiration capability in the face of connective tissue being degraded by fungus, bacteria, virus, drugs or injury, etc?
I wonder will this effectively automate the work done by Myhill, Bell et al?
In their earlier research that produced a similar single figure index that gave an indication of functional health.
This research appears largely similar, but their ealier efforts involved a fair bit of manual intervention to peform the test making it clinically expensive.
In a cfs/fm group I once belonged to, it was revealed MANY of us had engaged in endurance type athletics. (slow twitch muscle)
Always wondered if that was a clue.
I did! That would be an interesting survey….
It would be an interesting survey, but only if it’s determined what type of muscle is predominant in each person. Having more fast twitch muscle doesn’t preclude engaging in endurance athletics.