It’s great the NIH is doing telebriefings a couple of times a year to inform the chronic fatigue syndrome (ME/CFS) community of their progress. The calls can be more or less interesting. This one was definitely on the more interesting side.
NIH Intramural Study Proceeding on Pace

Good for the NIH for regularly communicating with the ME/CFS community. This was a particularly good call…
Nath reported that the NIH’s intramural study is proceeding on course. The interest in participation in the week-long study has been strong with the group receiving hundreds of inquiries. Eighty people (40 ME/CFS, 40 healthy controls) will go through the study. Thus far 26 people have participated (11 patients, 15 healthy controls).
The pace seems to have picked up a bit. In July Nath reported 10 participants had come through; four months later we’re up to 26, which is about one participant a week. Of the 11 patients, Nath stated that 6 were “adjudicated”, which apparently means passed through to the next phase of the study. (The study is in two parts – a week-long screening stay – followed by another week or so long stay.)
I asked whether the study was proceeding on the timeline and if we would hear anything before it’s over. Nath reported that the study is proceeding as expected – someone is at the hospital being tested every day.
Because patients actually stay at the hospital for two one-week stays, the overall timeline is hard to discern. If everything works perfectly, the 40 patients, given the two week-long stays and the one hospital bed available, would take, if I have it right, 80 weeks. Penciling in a round of one-week stays for the healthy controls brings the total study time to somewhere around 120 weeks.
Of course, nothing works perfectly; several ME/CFS patients didn’t make it to the second round of studies (one became pregnant) and Nath noted that participants have to postpone their stays for one reason or another, etc. Unless I have my numbers wrong, building in some more time would make this approximately a 2 1/2 to 3-year study that’s due to wrap up sometime in 2020. Papers would probably begin flowing in 2021.
Three to four years is actually a typical timeline for a big NIH study and this one is vastly more complicated than most. It’s a great study but it’s also a long time in the life of an ME/CFS patient.
“A Foundational Requisite” Being Established for ME/CFS
Common Data Elements (CDEs) are kind of like a secret weapon the NIH is about to unleash on the ME/CFS research field. Decidedly unsexy but hopefully quite powerful, CDEs could greatly increase the efficiency of ME/CFS research – thus making the limited dollars available for research count for more. The idea is that once CDEs are used, researchers will be able to analyze data across multiple studies, turning them, in effect, into one big study.
Zaher Nahle, the Solve ME/CFS Initiative’s (SMCI) chief scientific officer and a member of the CDE Working Group for ME/CFS, called the ME/CFS CDE project “an important and ambitious” one. He wrote:
“The participation of dozens of disease and community experts as volunteers underscores its importance and anticipated value.”
SMCI states that:
“CDEs are becoming a foundational requisite in biomedical research in any field, and this is especially true for a disease where confusion regarding case definition, inclusion criteria, and study design continue to exist.”
CDEs do what they do by establishing standardized ways to characterize a disease. The 2011 CDE established for multiple sclerosis, for instance, is a massive set of documents containing over 100 recommended data elements which describe everything from how to provide a diagnosis, to how to assess cognitive functioning, to how to do brain scans.
A set of core CDEs, which present essential information that should be present in each study, and supplemental CDEs are provided. A rationale and grade are provided for each CDE. For instance, the multiple sclerosis CDE states that the Berg Balance Scale is a supplemental, but “recommended”, test in MS.
The Common Data Element Working Group for ME/CFS has eleven specialized subgroups/panels covering data elements associated with fatigue, sleep, post-exertional malaise (PEM), autonomic testing, imaging, neuroendocrine test and biomakers and others.
The ME/CFS CDC project was initiated by The National Institute of Neurological Diseases and Disorders and Stroke (NINDS). NINDS appears to have taken a lead role in producing CDEs in the medical research community, and has created 19 thus far. The CDC is collaborating on the study.
The project began in January of this year. The first round of ME/CFS CDEs will be published this month for public comment with the final publication, if my notes are right, early next year.
Derya Unutmaz’s Big Findings
Derya Unutmaz’s story is pretty well known, but it’s still inspiring. Why? Because as everyone knows, if we need anything in this field, it’s new, younger, enthusiastic researchers to jump on board. The whole point of the NIH research center project and the intramural NIH project is not really to solve ME/CFS – they won’t be able to do that by themselves (unless we get lucky!) – but to stimulate this field.
Despite all the advocacy, the growth in donations for research foundations like the Open Medicine Foundation and all the interesting findings, the numbers indicate that where the rubber really meets the road – in the number of grant applications for ME/CFS – this field is still stuck in the mud. The NIH, for those who don’t know, is where the money really is in medical research. Private donations can get us only so far. They’re really great at supporting creative research, but success there almost inevitably ends up in an application for a big, fat NIH grant.
The NIH may be VERY slow. It may lack some creativity (at times). It’s been an incredibly frustrating place for ME/CFS patients to watch over the years, but it’s also where most of the money for medical research is ($31 billion/year). Chronic fatigue syndrome (ME/CFS) simply MUST crack the NIH. Hopefully, the NIH Research Centers project will itself result in a surge of grant applications over the next year.
Back to Unutmaz. Unutmaz, who was really the star of the show on the call, about five years ago got a shout out from Suzanne Vernon (then at the SMCI). She sent him just 20 ME/CFS samples and the rest, as they say, is history. Unutmaz parlayed his initial findings into a nice, big ROI NIH grant that’s going to fund one of the biggest immunological studies (over 200 patients) ever. Plus, Unutmaz, working out of a major lab, is going to be running one of the three NIH ME/CFS Research Centers. What’s not to like about that?
Unutmaz was inspiring on the call – not because he was a good cheerleader but because he’s obviously smart, competent and enthusiastic about studying this disease. We’re clearly in good hands with Unutmaz.
Check out Unutmaz’s resume and you’ll see studies drenched in T-cells. His 100-plus publications feature just about every aspect of T-cells one can imagine. The fact that it took him just 20 ME/CFS samples to detect “profound” differences in ME/CFS patients was exciting in a number of ways.
For one, in response to a great question during the Q&A period, Unutmaz revealed that the most provocative findings found were in the T-cells, and that the findings have proved to be highly reproducible – something we’ve rarely seen outside of NK cells (cousins, it should be pointed out, to T-cells) – in the immune field in ME/CFS.
With the role they play in the humoral branch of the immune system – T-cells are master regulators – any type of T-cell finding could be highly significant. Throw in the preliminary T-cell findings by Mark Davis of Stanford and the energy issues Maureen Hanson is finding in them, and all of the sudden T-cells are becoming a hot topic in ME/CFS.
For those who don’t remember, Mark Davis has found some antigens – immune triggers – that ME/CFS patients appear to be responding to. Another T-cell specialist, Davis reported that T-cells “go clonal”; i.e. start producing replicas of themselves in vast numbers when they meet up with an antigen – a protein nipped off a pathogen or toxin by an immune presenting cell.
The T-cells produced during this process are like honing missiles – they’re designed for one purpose and one purpose only – to search out and destroy anything that presents with that antigenic signature. High numbers of clonally produced T-cells are a sure sign of significant immune activation.
Davis recently found high rates of cytotoxic T-cell clonal expansion in ME/CFS. If his findings hold up, those T-cells should definitively indicate that either an autoimmune process or some sort of foreign antigen (i.e. an infection or toxin) is setting those T-cells in ME/CFS on edge. The most intriguing part, though, is Davis’ ability to search back and determine what’s triggering those T-cells. The Open Medicine Foundation (OMF) recently reported it was funding more of Mark Davis’ potentially ground-breaking work. Plus, Ron Davis is reportedly working with Mark Davis to submit an NIH grant supporting his work.
Because T-cells have hardly been explored in ME/CFS, they’re kind of unknown territory: who knows what surprises might be lurking in them.
Gut Connection – That the T-cell abnormalities Unutmaz is finding are associated with the gut probably made Mady Hornig and Ian Lipkin – champions of the role that the gut may play in ME/CFS – smile. It turns out that the problematic T-cells Unutmaz is finding regulate gut functioning. Either something in the guts of ME/CFS patients is messing with the regulatory T-cells or the gut T-cells are simply sitting down on their job. Either way, Unutmaz’ findings appear to put an enhanced focus on the gut in ME/CFS.
The gut is a terribly complex place, but with more and more research focusing on it and new methods being developed to understand it, a central problem in the gut might not be a bad thing at all to find in ME/CFS. Unutmaz echoed that hope when he stated that much is known about the cells he’s finding problems in and many treatments are under development to deal with them. That’s very good news for a disease that’s seemed particularly good at featuring issues with cells about which not much is known.
Unutmaz said he’ll be following up his T-cell study with a deep and rigorous probe of the gut bacteria in ME/CFS. He won’t just determine which bacteria are there – he’ll actually stress ME/CFS patients to see how their gut bacteria react. His studies will generate a lot of data; the challenge with them, as with all “omics” studies, will be to separate the wheat from the chaff.
To deal with that, he’ll be using a topological networks approach developed by Peter Robinson, a rare disease specialist. Robinson developed something called the Human Phenotype Ontology (HPO), which Jackson Labs states has become an international computational standard for studying human disease. Unutmaz stated that he also wanted to use the central data center embedded in the NIH’s ME/CFS research centers project to include data from the research centers in his project.
Unutmaz is also working with Precisely to develop an app to collect clinical data worldwide on ME/CFS patients. We’ve heard of projects like this before, but this may be the first one that has the funding to come to fruition.
So here we are – five years after an immunologist new to this field received 20 samples from the SMCI in the mail – leading an NIH ME/CFS research center. This is the kind of pattern we want to see duplicated again and again. New investigators coming in, bringing their talents and insights to this field and being rewarded for doing so.
Patients Shine
Unutmaz shone during the call, but so did the ME/CFS patients and caregivers during the Q & A period who displayed a depth of knowledge that few other patient groups can probably muster. Denise Lopez-Majano asked why not a research definition now? Koroshetz didn’t to my mind really have an answer to that question, but did report that the research consortium will be asked to characterize ME/CFS patients in all their different phases, including duration of illness.
Koroshetz did point out the need to be flexible – an important stance to take in a disease that is so heterogeneous and about which so little is known. Everybody seems to agree that this disease is astoundingly heterogeneous. Vicky Whittemore rather dramatically remarked on that fact during the last NIH call:
“many of the investigators are coming at this…. from very different directions, which I think is going to all come together to show us that it is heterogeneous disease with potentially many different mechanisms that all lead to very similar symptoms that we’ve been calling ME/CFS but likely have different underlying causes.”
Unutmaz noted that he plans to follow the patients in his study – all short duration patients – over several years to see if their immune systems “turn” as is suspected. Much like Ron Davis, Unutmaz emphasized we’re in the exploratory phase of understanding this disease.
Koroshetz seemed to be genuinely touched when Lopez-Majano reported she had two young sons who’d been sick for 12 years. Koroshetz has been refreshingly honest about the needs of this disease. He’s stated that the disease needs many, many more investigators and much more funding. He acknowledged that the three Research Centers are simply a beginning – an attempt to jump-start the field.
The Centers grant almost doubled NIH research funding for ME/CFS – an unusual outcome in any disease – but the Research Centers are asked to do a lot with little and the disease is still dramatically underfunded. Koroshetz has written blogs on ME/CFS, and even talked up the little NIH program in his talk to top officials at the NIH Advisory Committee. He was blunt about the needs at that meeting:
“Myalgic Encephalomyelitis and Chronic Fatigue Syndrome is an area that’s really been completely under-investigated across the country, and Francis [Collins] was really courageous and went out there and said that NIH is gonna change that.” Koroshetz called ME/CFS a “pathological condition” and stated that “people are completely disabled for decades because of this terrible fatigue and inability to exercise”
Koroshetz, in fact, stated that he believes the field probably needs 20 research centers and 10-20 times its current funding. That was something of a jaw-dropper coming from the head of a large institute at the NIH.
Ian Lipkin clearly agrees. He warned the NIH (and by implication the patient community) not to expect too much, stating that while the funding for the centers was “helpful”, it was nowhere near “adequate”.
It’s definitely a start, though.
Is Chronic Fatigue Syndrome (ME/CFS) an Autonomic Neuropathy?
I’ve lost my notes, but as I remember, a doctor with ME/CFS asserted that ME/CFS is an autonomic neuropathy and then questioned whether all the money going to molecular studies were going to be much help.
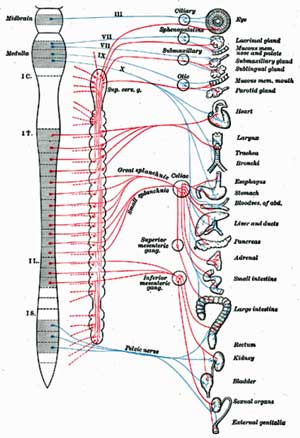
I thought the idea was brilliant – it encapsulated so much – and wondered why it hasn’t seriously been brought up before. I was immediately brought back to Dr. Pocinki’s description of an autonomic nervous system flopping around under stress, and Staci Stevens’ belief that the ANS had lost its setpoint in ME/CFS. Then there was Dr. Wyller’s recent bizarre finding that Clonidine, a sympathetic nervous system inhibitor, actually made many of his adolescent patients worse…something strange is clearly going on in the autonomic nervous systems of people with ME/CFS.
I don’t know if autonomic neuropathies can explain everything in ME/CFS, but they may explain a lot. Autonomic neuropathies involve damage to the autonomic nerves in the body, interrupting the stream of messages to the brain. They’re most often found in diabetes, but the Mayo clinic reports that infections (hmmm…) can also cause them.
Common signs of an autonomic neuropathy include dizziness and fainting, urinary problems, digestive problems including bloating and constipation (IBS), problems with temperature regulation, sexual difficulties, and, get this – exercise intolerance – because of the failure of the heart to beat fast enough to maintain exercise. Many of these symptoms are found in ME/CFS and I’ll bet they are the tip of the iceberg. The heterogeneity in ME/CFS could conceivably be the result of different autonomic nerves being affected in different patients.
We know that small nerve fiber problems occur in POTS, which is commonly found in ME/CFS. What we don’t know is how common they are in ME/CFS. Nor do we know the status of other autonomic nerves in this disease…
If there’s one thing that was missed in the ME/CFS research center grant winners, it was a group focused on the autonomic nervous system. Dr. Unutmaz, however, begged to disagree about the relevance of molecular studies to a possible autonomic neuropathy. It it’s there, he believes, they’ll find evidence of it. The connections between the immune system and the autonomic nervous system – a major regulator of the immune system – are, after all, bountiful.
Donation Drive Update
Thanks to the 33 people who’ve donated about $3300 to Health Rising on the first two days of our fundraising drive, bringing us about 15% of our way to our year end goal. Please contribute! Find out more here or use the donate button below or on the right hand side of this page.







Thanks Cort. My worry is that it’s going to be too late for many of us by the time treatments are eventually found, that we will be the generation lost to tjis disease, it’s pretty heart breaking. If the field is only getting started now, what does that mean for patients locked in their homes now? I know Dr.Davis has said we are in the exploratory phase of this illness but I can’t see him envisioning Whitney bed ridden for another decade, he must want treatments to be found before then. I hope all researchers do.
That’s unfortunately entirely possible. I’m 58, had this since I was 20….Well, if something shows up when I’m 70, I guess I’ll celebrate that.
I would be really surprised, though, if things didn’t show up that didn’t at least significantly help. Ron Davis is lookingd at already approved drugs, Nancy Klimas actually has a tentative drug testing program and I just heard from three people who did VERY well on Dr. Pridgen’s program. I know of a treatment being tested next year that is being kept under wraps. Plus a major finding in the exploratory phase could bring in a lot of research.
In the meantime I’m working on being satisfied now – no matter what. We’ll see what the future brings….
And don’t overlook all the things that you can do to help your gut in the meantime.
Functional medicine is big on testing for gut problems. Genova Diagnistics among other labs has a good series of tests.
Maybe keep an eye on fecal implants too.
Also it’s good to remind ourselves that a lot of the technology for analysis was never around 20 years ago, findings will be accelerated many times faster than ever before. My hope as Cort already mentioned is the search for already approved drugs that most probably are out there, yet we just don’t know yet until all the new technology can weed which ones work best
Emer, as long as patients advocate for funding for molecular studies rather than funding for more studies of the autonomic nervous system, researchers at least have a chance of finding an answer. The autonomic nervous system studies to date do not examine what it is that are affecting our cells. They simply observe that the nervous system is out of whack. No kidding. This is the meaning of molecular studies and it’s the kind that Ron Davis is doing:
“Molecular genetics is the field of biology that studies the structure and function of genes at a molecular level and thus employs methods of both molecular biology and genetics. The study of chromosomes and gene expression of an organism can give insight into heredity, genetic variation, and mutations. This is useful in the study of developmental biology and in understanding and treating genetic diseases.”
Whitney Dafoe was sick, but not bedridden, mute and unable to ingest food by mouth when Dr. Kogelnik of the Open Medicine Institute at Stanford took on his case. If I were Ron Davis I would be looking for a cure for poisoning caused by that experimental drug.
I’m not surprised about the Autonomic Nervous system stuff, Because that’s what ANNIE HOOPER, ASHOK GUPTA, DAN NEUFFLER, with all their brain retraining stuff work on, with CFS/MCS.
Have tired it , but , couldn’t get it to work for me. Had this thing for 20yrs.
And what about the breakthrough research, the Griffith University here in Australia, has recently released. Identified that patients with CFS/ME were far more likely to have single nucleotide polymorphisms – DNA typos- in the genetic code for certain cell receptor. this cell receptor is known as transient receptor potential melastatin 3(TRPM3), and in healthy cells, it plays a crucial role – transferring calcium from outside the cell to the inside, where it helps regulate gene expression and protein production. In several peer-reviewed papers published by the Griffith team last year, showed that in CFS/ME patients, something seemed to be going wrong withTRPM3. As a result , calcium ions weren’t making it inside the cell like they should be, meaning cell function was impaired. And what makes matters worse is that TRPM3, the receptor is found on every single cell in the body, not just the immune cells. Which explains why it is so difficult to diagnose , but also why it’s so severe. These TRPM3 receptors are also known as the ‘THREAT RECEPTORS’ , because they’re upregulated when the body is under any kind of threat, such as infection, trauma, or even childbirth.
Now , doesn’t that RING A BELL, sound like the AUTONOMIC NERVOUS SYSTEM, again????????
Having POTS and autoimmune dysfunction/illness I’m certain there is a connection. We may have the WHY (autoimmune and inflammation) figured out. But we still don’t have a solution to the WHY. Still no great “fixes”, only “bandaids” for the symptoms.
Issie
For the why, personally from everything I’ve read, my money is on gut bacteria/gut permeability. Either through antibiotic use, pathogens in the gut, chemicals/additives/pesticides or modern diet affecting the gut bacteria/gut permeability or all of the above in combination. There are some interesting studies that pwME may not be able to convert carbs into energy. Dr Myhill work focuses on the mitochondria and using ketogenic diet for example to bypass not being able to convert carbs into energy, by switching to ketosis and gaining energy from fat. Though it’s not as simple as diet unfortunately, it’s fixing why the system has broken down and why the mitochondria are broken and if the gut isn’t working properly we may be lacking essential vitamins and minerals. So I think it’s a cumalative thing that may need a multi-pronged approach to fix and fixing neurological damage may be a lot more complicated too. If it’s gut bacteria related it may be fecal transplants needed. Type 2 diabetes can be helped with ketogenic diet as well. I’ve read a few studies on gut permeability and auto-immune disease and neurological-immune disease and the lack of certain gut bacteria with allergies. So if people want something to do while waiting for a cure, focussing on improving gut health is probably a good place to start for anyone with auto-immune issues. At least just to cut down the inflammation. I think that the above showing T cells could be affected by gut bacteria is a really good as it fits in with the gut hypothesis. Hope that waffle makes sense I got terrible brain fog at the moment fro PEM.
Yeah Jen, I agree totally. Mine started after I was given the medication, FLAGYL, and I was an undiagnosed Coeliac at the time too. Gut problems , major, and lived in a high chemical use area. Time bomb waiting to happen. Done 15yrs of probiotic foods, taking probiotics etc. Gut healing diets, you name it (GAPS Diet , BODY ECOLOGY Diet, never helped, but did keep me from being bedridden) Then went and had an FMT last year, got rid of my constipation and bowel problems, but still have major MCS/CFS. I think that all the chemical exposure, when my gut/colon was in such a bad state (leaky allowed too many chemicals into my cells. And quite frankly, stuffed up my body.
Totally agree Donna. Diet alone isn’t enough to fix it as it’s a combination of factors and we don’t yet understand enough about what’s actually happening. Is it pathogens in the gut, is it chemicals? It’s sadly a lot more complicated. For me though, it’s something to focus on, something I can do for myself while science brings more answers.
As told in Surviving Mold by Dr. Ritchie Shoemaker, I was unwilling to help Dr. Cheney with his project to start a new syndrome. I told him “Get someone else”
But he launched into a list of reasons why I should volunteer to act as a prototype.
He pulled out his easel and drew diagrams of immune system components. Little x’s, o’s, dashes and dots to represent B cells, NK cells, various macrophages and lymphocytes.
And yes, little “t’s” to be the T cells.
He told me “Your mold illness doesn’t matter. You have the right markers to serve as a prototype”, and slammed his marker into his easel. “Something has hijacked the T cells… we don’t know what.”
I thought “If he doesn’t think the mold illness will interfere, then great. I’ll do it. For then I can ask researchers to look into the mold that was making us ill.”
As told in Dr. Shoemakers books, not a single CFS researcher ever came back to where he syndrome started.
So not a single one of them ever looked into it.
Interesting how the T cells are coming back into fashion.
I wonder if the mold toxins had anything to do with “hijacking” them?
Very possibly mold is…It’s going to be interesting. If Mark Davis can track down the antigen that is sending the T-cells into a tizzy – it could be a mold toxin. Wouldn’t that be something!
It could be a variety of things that trigger different people. I had all of the symptoms of CFS/ME years ago and my doctor suggested that I remove my copper IUD. The symptoms went away within hours and I was healthy for years as long as I didn’t wear earrings or have metal in my body.
Unfortunately I ended up in a moldy apartment and got CFS/ME again. While I am out of mold now, it’s taking me longer to get back to 100% this time around. Having two distinct triggers makes me wonder what other triggers people might have.
I agree – I’ll bet there will be a variety of triggers…which may end begging the question – why are the T-cells so darn trigger-happy? Their over-reaction could be causing ME/CFS/FM, etc.
Some creative person should be able to make a nice cartoon out of “trigger happy T-cells”. Love the notion, Cort.
🙂
Myrax, I found your two triggers most interesting. Have you ever found a common element between them? One that comes to mind is candida. There is a study showing that copper IUDs increase candida levels. And with mold, some forms of toxic mold are believed to be immune analogs to Candida. So in theory mold exposure could be triggering an old candida sensitivity response in the immune system. Have you evaluated candida? That might include being highly sensitive to simple carbohydrates, and being gluten intolerant. Anyway, your two triggers leads me to wonder whether mold problems are related to a prior candida immune response some CFS patients.
I read a study about people with allergies are missing certain strains of gut bacteria. So the triggers could be different for different people. So some may be triggered by mould, while others it could be something else. I can’t remember the name of the study, but all allergies may be caused by the lack of this particular strain of gut bacteria that somehow regulates immune response. We know so little about gut microbes and how each one affects the body. Lots of interesting stuff too about how gut bacteria affects the brain too. This would make sense why for some the trigger is mould, some candida and some something completely different and why patients are not all triggered by the same thing. I developed an allergy to sulphates since I got the ME.
Kurt, I’ve tried avoiding gluten and simple carbohydrates and nothing changed. I don’t think my triggers are actually related as I was fine around mold for years after the metal trigger developed. It was until prolonged exposure that I got sick.
It is believed that the toxin-eating EBV kof which there are dozens of strains) and similar viruses (like CMV,internal shingles) living in the liver, spleen, brain, spinal nerve, thyroid and/or vagus nerve are behind CFS. So many medications (‘chemicals’), molds,and ‘modern’ preserved foods will trigger or worsen CFS symptoms.
Makes sense that autoimmune issues are at play with mold. Having been DXd with CIRS and having 5 different genetic markers of inability to throw off mold and biotoxins — if the immune system isn’t detecting an issue to attack it – there is an internal mold and biotoxins issue and it makes us very sick. I had exposure my whole life and a more recent exposure caused a crash. Now with no exposure, a clean environment and lots of detox – I’m better – but there is still an internal toxic issue. We found mold/fungus in my thyroid biopsy. I have recently had the yearly ultrasound. Will get results this week. See if all the antifungal herbs and medicines have made a difference. I’ll come back and tell if there is a change. Radiologist indicated that I have less tumors now. So very hopeful.
Issie
Got my report. There are less tumors large enough to measure and the largest tumor has shrunk by .5. So probably, doing the mold and fungal detox are helping. I’m needing less supplements and less medicines. I’m very encouraged by my results. Still have a ways to go – but will definitely take improvement.
Issie
What many don’t realize is that Nancy Klimas carried out the same studies of natural killer cells and T’s etc etc for decades on HIV patients. But she was more forthright about what she felt was the cause : “Psychological distress, killer lymphocytes and disease severity in HIV/AIDS.” The idea of these studies is that yes, the patient has an illness, but it’s not overload of mold, virus, bacteria, chemicals that are the cause of the severity of the illness simply the psychological distress of the patient. https://www.ncbi.nlm.nih.gov/pubmed/18321678
With all the researchers milling around investigating everything they can think of,I expect someone will trip over the answer quite by accident. I applaud their efforts. I’m 69,and may not live to see this puzzle solved, but I’m watching the unfolding saga of discoveries that lead to more questions with interest.
Cort, thanks for all your hard work and for the blog. I am happy to become a subscriber and sustaining donor if not for much.
Every bit counts JoAnn! I am very, very happy to get your support. 🙂
While I call what I have ME/CFS, my neurologist ignores that designation and he calls what I have autonomic neuropathy. He initially called what I have pandysautonomia. Like you Cort, I too felt (very) disappointed that research into the autonomic nervous system aspects of ME/CFS was not a focus for the recent grants.
POTS was identified in the younger among us, those early in their ME/CFS “careers”, and SFN (small fiber neuropathy) was identified in those with Fibromyalgia, including those who “qualify” as having both FM and ME/CFS presumabling, but what I have, as a 68 year old who has had ME/CFS for 22 years, is disabling hypotension—no racing heart—almost nothing about me ever goes up, but virtually everything is low. And I was diagnosed with SFN too years ago though I have no diabetes or blood sugar problems. So I do hope those kinds of studies will be done, to show the incidence of hyptension and small fiber neuropathy in those with long term ME/CFS. I have a lot more of the problems listed from autonomic neuropathy, and some not on that list yet, but which may belong there too. Dr. Anne Oaklander’s research into SFN expanded the range of problems and symptoms which can be associated with this to what she calls polyneuropathy. It can be all over the body, as in the pain of FM, and it can affect memory and cognitive function too.
I have found that the various aspects of neuropathy I have increase with the years, so that—researchers take note—longer term patients may be fertile subjects who can more easily and clearly reveal what is going on with our kind of condition.
Hi Cecilia,
Very likely you or your doctors already looked into it, but it reminds me of an experience of mine:
My body is “pretty good at generating high adrenaline levels”. While it comes with plenty of disadvantages I had a few times that I felt that “my body was out on producing any adrenaline at all”. I felt very different: I could barely move my chest to breathe (far worse then at other times), I think my hart was very “relaxed/hard to notice” (I don’t remember that one exactly but it certainly wasn’t overactive) and I had a very remarkable inability to worry or panic. Being *very* short on breath during those nights I had every reason to panic but I just “couldn’t do so”. I felt *very* calm, far more then in a long time. I also had very few emotions/feelings but didn’t feel depressed. I just didn’t seem to have the ability to feel much at all.
If this feels familiar to you it might indicate adrenal fatigue that often comes after having years of ME.
That pattern of “high adrenaline then fatigue” may not be adrenal fatigue at all- it could simply be an overactive autonomic nervous system pushing from a sympathetic dominant to a freeze state.
Hi Barliman,
Thx for the input! That makes sense too. I sensed a great drop that resembled a very sharp decrease in adrenaline and supposed my body temporary couldn’t produce any more. But it may indeed be just as well that it didn’t wanted too, maybe to calm things down.
I didn’t considered it this way as I thought the strong lack of breathing was dangerous enough for the body to fall back deeply as to not try that trick but it might have felt a very strong need to calm the ANS.
Will somebody please get through to Koroshetz that this is not about “terrible fatigue and inability to exercise” but a complete inability to have a life? Am so tired of hearing this phrase from him. Let’s start with the inability to get out of bed, or sit up for any length of time, or think clearly enough to work.
You know I think Koroshetz does get it but I think that the vast majority of researchers and doctors don’t. I think they just don’t come across diseases as debilitating as ME/CFS. That may actually be one of our problems; ME/CFS is so functionally disabling that doctors don’t know what to do with it.
Komaroff’s 1996 study is one of my favorites of all time because it was big and the results were so shocking….ME/CFS patients were not a little worse functionally than diseases like heart failure and multiple sclerosis – they were significantly functionally worse….
https://www.ncbi.nlm.nih.gov/pubmed/8873490
Am J Med. 1996 Sep;101(3):281-90.
Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Komaroff AL1, Fagioli LR, Doolittle TH, Gandek B, Gleit MA, Guerriero RT, Kornish RJ 2nd, Ware NC, Ware JE Jr, Bates DW.
The subjects of the study were patients with CFS (n = 223) from a CFS clinic, a population-based control sample (n = 2,474), and disease comparison groups with hypertension (n = 2,089), congestive heart failure (n = 216), type II diabetes mellitus (n = 163), acute myocardial infarction (n = 107), multiple sclerosis (n = 25), and depression (n = 502). We measured functional status and well-being using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), which is a self-administered questionnaire in which lower scores are indicative of greater impairment.
Results
Patients with CFS had far lower mean scores than the general population control subjects on all eight SF-36 scales. They also scored significantly lower than patients in all the disease comparison groups other than depression on virtually all the scales.
When compared with patients with depression, they scored significantly lower on all the scales except for scales measuring mental health and role disability due to emotional problems, on which they scored significantly higher.
The two SF-36 scales reflecting mental health were not correlated with any of the symptoms of CFS except for irritability and depression.
Cort, I dont know if you have encountered this approach.
https://www.nemechekconsultativemedicine.com/
Dr Nemechek is an osteopath with a long interest in HIV and particularly the sudden cardiac deaths in HIV patients with advanced autonomic neuropathic problems.
He uses a 5 step grading system for autonomic neuropathy.
He is now working on reversing it using a model that goes like this:
Vagal underactivity slows gut motility- allowing small intestinal bacterial overgrowth. That leads to leaky gut and absorbtion of bacterial toxins into the CNS. The resultant microglial overactivation then prevents neuronal repair.
Strictly speaking these problems probably are not “autonomic neuropathy” as in damage to the peripheral autonomic nerves. They are more likely to be brainstem issues that scramble the input signals and the aberrant autonomic responses.
Nemechek’s protocol is interesting, and may be very widely applicable.
https://www.youtube.com/watch?v=Itu7PcIuKTY
Thanks very much for passing that on!
Hi Barliman,
I have/had strong neuropathy problems and indeed there is a strong link to the brain in my case.
I had many times I shortly lost control of some muscles. When I crashed deeply my neurologist (one that does truly want to help ME patients) explained that the problem did originate from the brain. It made a lot of sense: after that crash I could do simple movements but I totally couldn’t do any complex movements. I could for example stand up while putting my socks on (can be done as a series of simple movements) but couldn’t walk around my hospital bed (have to move feet, legs, hips,… in concert and have to keep balance). It took me 5 minutes to get the first turn wright. In robotics complex compound movements are many orders of magnitude more demanding than a series of simple ones; it seemed that was too much for my brain.
I slowly had to relearn plenty of daily “simple” tasks like standing up from a chair. The good thing is: for me quite a large part was reversible. Relearning stuff like someone would after brain injury helped a lot. Improving health further drove back many remaining neuropathy issues.
As for neuropathic pain, I still go with the hypothesis that it is local. Improving local blood flow did reduce it to a small symptom for me.
Please keep contributing Barliman ;-).
As to gut problems: did someone consider chewing ones food *very* well? Most people don’t chew food well. Being exhausted may add to this habit. But from a pure practical point of view: I envision that if you don’t chew well the food takes up more volume in the bowel and has plenty of crevices/gaps. These do not touch your bowel so the bowel has poor access to this part of the food but bacteria can reach it. That gives bacteria a significant competitive advantage over the bowel. Chewing better will not be a miracle solution but even small contributions should help. In addition chewing slower does generate a satisfaction before you eat too much which should be good too. And giving bacteria less of a competitive advantage lets them multiply less and so run away with less calories, proteins, minerals…
I *think* it helped me to remain having decent gut functioning even during this disease.
Cort,
Thank you for your work. I would like to contribute. Would it cause a problem if I sent a check? If so, I’ll set up a credit card payment. If check is ok, to what address should I mail it?
Regards,
Kathy
I love checks Kathy! Checks are great.
Please make it out to Health Rising and send it to
Cort Johnson
2555 Hampton Rd. Unit 6308
Henderson, NV 8905
Thanks so much!
I think that the gut thing is huge and I know Dr Lipkin and Maddy Hornig are well into researching this area and the metabolites that come probably from pathogenic bacteria. I did an American Gut study and the results were very poor with very little diversity and virtually no good bacteria despite an excellent diet and the use of yoghurt daily and many probiotics.
I first got sick in 1979 and had a lot of gut symptoms then but they have changed over time and can be a problem on a daily basis so I would be amazed if the gut isn’t playing a huge part in our illness. The link with the T Cells sounds fascinating.
Now isn’t something – a good diet, lots of probiotics and still low gut diversity! Whoa…Something is going on there. Now that’s a seed for a future study….Other gut studies have shown low diversity in ME/CFS…
I should have said that the gut probably played a part in a sub set of patients with ME/CFS as I am not convinced we all have the same illness.
(aaSFPN)’apparent autoimmune Small Fiber Polyneuropathy’ found by Boston Neurology Mass General Hospital Harvard Professor Neurologist Dr. Anne Oaklander MD Ph.D.
https://www.neuropathycommons.org she had said as much as 50% of patients diagnosed with CFS Fibro IBS are misdiagnosed they have forms of (SFPN)instead or (aaSFPN) NeuopathyCommons.org It was on
Fox Boston News Nov.17th, 2017
Thanks Aidan…Major finding!
https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
See this link for current facts about peripheral neuropathy.
Talking to a doctor recently, I learned the parasympathetic branch of the autonomic nervous system is connected directly to the brain and is a stronger, more supported system. So its particular functions are more apt to continue normally. On the other hand, the peripheral aspects of the nervous systems—those not directly connected to the brain— include the sympathetic branch, and then the sensory nerves including the non-myelinated small fibers which not only provide ennervation in the skin, they provide all kinds of linkages throughout the system.
My overall sense is that the thinnest, smallest, most vulnerable nerves are the small fibers. After that, in terms of vulnerability, comes the sympathetic nervous system. So the disproportionate weaknesses will be there, resulting in just the sort of symptom picture PWME have, and may increasingly develop the longer the illness continues and the older the PWME gets.
When I look at all the work/functions that small fibers have, then that the sympathetic nervous system has, I see an erosion or loss of these functions in my own condition, as well as the general symptom picture for ME/CFS
I would expect that the symptoms PWME show and develop did originate with either infections or autoimmune processes, both of which point to some change that occurred in the immune system. This change then affects the nerves over time, as the immune and nervous systems are closely linked. Small fibers and the sympathetic branch of the autonomic nervous system would be first to be hit.
Background: ME was classified as a neurological illness by the World Health Organization in 1969. But it has largely been studied as an immune illness. That is where the cause is being sought. Also patients first experienceit as like a flu or infection which they don’t recover from. But the symptom pattern which continues and develops over time, a de-regulation and downregulation of the body’s organs and systems pertain to nervous system.
Specific examples: The adrenal gland is not served by the parasympathic system, but only by the sympathetic. So when the adrenal gland shows signs of falling down on the job (which some call “adrenal fatigue”) the problem may well be originating in the sympathetic nervous system. The organ itself may be entirely healthy, but the management it needs from the sympathetic system isn’t working well. That is my English translation of what I understand from the science.
The sympathetic system also is in charge of making the blood vessels contract—to send the blood back to the upper body, heart and brain to serve all the needs of this part of the body, most obviously being upright. The sympathetic nervous system is also supposed to serve the muscles and capacity of the body to do work. Without it, the vessels stay open and the blood pools lower in the body. Circulation cannot happen normally and do what it was designed to do.
The sympathetic system also causes sweating. Without it, a person doesn’t or rarely sweats. Sensing (the small fibers) and responding (sympathetic system) to temperature changes doesn’t work normally. Pupils also don’t contract normally to adjust to changes in light levels, making sensitivity to light, night driving problems worse.
Something is degrading the nerves—those in the peripheral system first. That something may be an abnormality in the immune system, caused by infection, autoimmune process or some other adverse cause like a toxin exposure.
I hope that research will look at what is different in our peripheral nervous system, what is degrading it and what might help restore or prevent this “erosion”.
Thanks to anyone who made it to the end of my post!
Cort,
I came to same conclusion that it may not be until 2020 that data is analyzed and released. I share in the frustration that 4-5 years is a long time to wait. Dr. Avi Nath alluded to plans of a treatment phase of study during his Webinar if deep phenotyping points to possible mechanisms of disease. This probably means that potential treatment options may be available by 2023-2025?
On a positive note, it is my opinion that our best chances of finding effective treatments will only be possible once the pathophysiology of ME/CFS is sorted out. I doubt someone will stumble on a cure. Hopefully research momentum will build once we get foot hold.
I wonder what percentage actually have (SPS) Stiff Person Syndrome I believe a trial should be done on the (GAD) Antibodies test in about 50 patients & see those results it would even also gives us indicators of where people sit with regards to Diabetes as well it is an important test, I will run the test in early January if it is at 5 Normal or up in the 250’s…I have now seen the following a Woman Vascular compressions Color dopler ultrasound she has small fiber neuropathy also has Genetic CVID she underwent Vascular Surgery an incision at belly button about 12 inches long she is on Gamma as well so the Gut issues may not be SIBO or other issues could very well be (VC) instead. There is a young lady on Facebook from the UK she was diagnosed with this gut issue underwent Surgery in Germany she is recovering now she is on my Friends list her name is Emma Green she say her POTS like issues resolved when they opened her up they said her gut was dying from these compressions…She was no longer able to eat she is now back on foods & gaining strength…I have no doubts she has or had small fiber neuropathy as well…Merry Christmas Happy Holidays to everyone I pray you all get Cure in 2018…