

Dr. Anne Oaklander didn’t just discover the small nerve fiber problems in fibromyalgia, she’s literally trying to build the small nerve fiber field from the bottom up. We can thank the NIH for that: it awarded her with a big ROI grant a couple of years ago which, among other things, tasked her with identifying the best way to diagnose small nerve fiber neuropathy or as she more accurately calls it, small-fiber polyneuropathy (SFPN).
The Study
Specific symptoms may discriminate between fibromyalgia patients with vs without objective test evidence of small-fiber polyneuropathy 2018. Lodahl, Mette; Treister, Roi; Oaklander, Anne Louise. PAIN Reports.
First Dr. Oaklander lays out what we know – that many studies indicate that the small nerve fibers in the skin of about 40% of the people with fibromyalgia have been damaged or partially lost. Oaklander seems to be more and more confident of her findings.
Disregarding the numerous brain scanning studies, presumably because they don’t elucidate a “cause”, she states that fibromyalgia had “no known biomedical cause” until the SFPN was found.
Then she rolls through the many ways SFPN might be causing FM. (If you have chronic fatigue syndrome (ME/CFS) these may apply as well.) The gist is that because the small, lightly or unmyelinated nerve fibers seem to be ubiquitous in the body, damage to them could affect just about every symptom present in FM or ME/CFS.
- Pain – Because the small nerve fibers transmit pain sensations they could be causing or contributing to the pain sensitization seen in FM.
- Gut Issues – Because they control gut motility they could be causing or contributing to the gut problems.
- Fatigue – Oaklander attributed the fatigue problems in FM and ME/CFS to something she called “neurogenic myovasculopathy” – which may be a new term. (Neurogenic – nerve system caused; myo – muscle; vasculopathy – blood vessel disease: a nervous system disease causing problems with the blood vessels in the muscles).
- Inflammation – Because the same nerve fibers regulate and are regulated by the immune system, damage to them may be producing inflammation.
- Brainfog/Fibrofog – Because the nerve fibers extend into the brain, damage to them could affect cognition.
- Sleep – several studies suggest that neuropathy is more common on people with some sleep disorders.
It’s an impressive list. It’s no wonder that Oaklander dismisses any idea that FM is psychosomatic and calls it a neurological disorder.
(On a side note – FM finds its unhappy home at the NIH in the National Institute of Arthritis and Muscoskeletal and Skin Disorders (NIAMS). NIAMS is an Institute that would apparently rather treat FM as a behavioral disorder than a physiological one and has little interest in funding it. (Funding has actually dropped over the past five years.) With its funding among the lowest in the NIH – just $9 million a year or about a dollar a year per patient – perhaps FM would do better if it moved to the Neurological Institute (NINDS). It was NINDS, not NIAMS, that funded Oaklander’s NIH grant.
The really good news is that, because those small nerve fibers never stop growing, if whatever is damaging them can be stopped, they should be able to grow back; i.e. a full recovery should be possible (!). All that may be needed, Dr. Oaklander suggests, is to remove the “neurotoxic” conditions causing the damage. A recent Oaklander treatment study was not a full blown placebo-controlled, double-blinded trial, but it did suggest that immune modulators may be helpful for many with SFPN.
Small Nerves – Big, Big Problem? Drug Trial Points Finger at Autoimmunity in Fibromyalgia and ME/CFS
The possibility of a treatment makes it all the more reason, Dr. Oaklander asserts, to find a way to easily determine who among the millions of FM patient has SFPN and who doesn’t.
Symptom Questionnaire
It could something be as simple as a symptom questionnaire. The symptoms of SFPN and fibromyalgia overlap greatly. (Note how close they are to ME/CFS as well.) SFPN sufferers report that their worst symptoms are fatigue and tiredness, poor endurance or strength, deep pains or aches, tingling or pins and needles and difficulty thinking and concentrating.
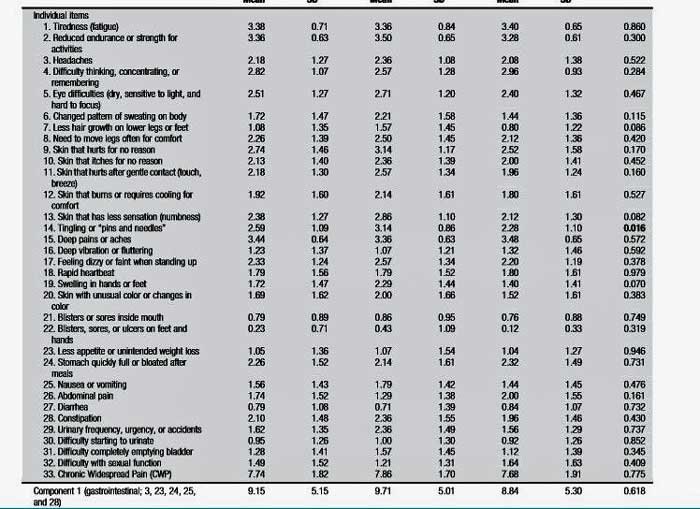
The survey’s five components (gastrointestinal, somatosensory, miscellaneous, vascular, neurological) identify symptoms that could be arising from nerve damage in different parts of the body. An earlier study confirmed that the MGH-SS questionnaire was accurate and reliable in identifying FM patients a biopsy confirmed had SFPN in their skin.
For the purposes of this study, small fiber damage in the skin was confirmed using a skin biopsy or by autonomic nervous system testing which included: a heart rate variability test during deep breathing, heart and blood-pressure responses to the Valsalva maneuver and tilt, and quantitative sudomotor axon reflex testing. Furthermore, every person, whether they had SFPN or not, underwent the autonomic nervous system tests, took a pain survey, and did the SF-36 questionnaire.
The objective was to determine if a symptom questionnaire could identify FM patients with SFPN from those who don’t have it. The ancillary question – how much does SFPN in the skin affect symptoms? Dr. Clauw proposes that SFPN in the skin is a minor issue, kind of a side-show in FM. The real problem, he believes, lies in the central nervous system. Dr. Oaklander obviously believes differently.
The Quandry
Oaklander’s starting point illustrated how widespread small nerve fiber problems may be – not just in FM, but also in other diseases. She started out with 159 patients with “multisymptom illnesses” that had been referred to her. Thirty-three percent of those patients met the 2010 criteria for FM. Others probably met the definition for ME/CFS or POTS or other diseases. The wide spread of patients suggests a big group of similar patients across several diseases exists.
Thirty-nine FM patients ended up in this study, 36% of whom were determined to have SFPN by skin biopsy. Again, the most severe symptoms in this group were familiar – deep pains, fatigue, and reduced endurance.
Of the 33 symptoms measured, only pins and needles sensations were significantly increased in the FM patients with small fiber neuropathy in their skin. The vascular group of symptoms was significantly worse in the SFPN group as well, and they scored worse on the cognitive component of the SF-36 test.
There was no difference, however, in the autonomic nervous system scores, the pain scores or the functionality scores. If people with positive skin biopsies were worse off than people without them, it didn’t show up in decreased autonomic functioning or even in increased pain levels. It simply showed up as an increased incidence of pins and needles sensations.
The presence of pins and needles symptoms, then, “may” (it was not a large study) be able to differentiate between those who have SFPN and those who don’t.
The larger issue, though, is the inability of the symptom questionnaire to demonstrate that people with small nerve problems in their skin are significantly symptomatically worse off or significantly different from those who don’t have them.
That finding could suggest that SFPN either doesn’t account for much in FM; that it’s, as Dr. Clauw believes, a mostly innocuous add-on problem which causes pins and needles sensations and perhaps a few more vascular symptoms but doesn’t significantly affect the main symptoms in FM.
It’s also possible that SFPN is an entirely separate disease which just happens to have almost exactly the same features as FM. That seems unlikely.
A third, more intriguing possibility is that the small nerve problems exist throughout the bodies of many FM patients but only show up in the skin of about 40% of them. If that’s true, then the autonomic nervous system scores, pain tests, etc. would be similar in everyone in this study, which is what happened.
We seem to be left with two options: SFPN is either a relatively mild issue symptomatically or it’s the issue in FM. Time will tell on that but Oaklander’s last retrospective study suggesting that immunomodulators can be quite helpful in FM suggests the later.
Next for Oaklander is apparently finding some way to show that the small nerve problems in FM extend beyond the skin to the nerves that affect muscle functioning, gut issues, cognition and others.
If you have pins and needles sensations it might be good idea to get a small nerve biopsy done or the right kind of eye scan. (Dr. Oaklander is assessing the effectiveness of different SFPN tests as well.) If your test comes back positive, it’s possible, but by no means guaranteed, that you might be able to get IVIG paid for. (See Small Nerves, Big, Big Problem?)








Thanks, Cort.
Sign me up, nearby, would take questionnaire and biopsy though my symptoms are not 100% similar.
Happy holidays.
Yes …All of the symptoms and SFPN idiopathic. I also have vascular abnormalities (cavernous hemangioma) in my brain. Most people that do have them experience the same symptoms of FM or SFPN. It’s very interesting.
I think I also have vascular symptoms, because I developed pulsatilla tinnitus.
Another dead end article. My doctors refuse to even do tests and I have deteriorated for 2 years.
Amanda, I have this as well. Have you ever been diagnosed with seizures? Do you experience brain zaps? I hope we can discuss.
David wrote:
As a man the first thing i noticed was the “low hair count on lower body… from being/having hairy legs 6/8 years back i’ve got not one left very smooth.. and also having had Helicobacta Pylori twice since i got fibro i’ve had exactly the same feeling as pylori since..
It’s horrible living with that 24/7 just a case of living with it but not being able to enjoy life.. impossible to be happy as all well-being is lost with the feeling sick… as for the rest of the symptoms i have nearly all of the time..
Loss of hair is a vascular symptom on that test and there was a trend towards more vascular symptoms for the people with SFPN. That seems to make sense since the small fiber problems they had were in the skin.
I hope you can get tested. Do read the Small Nerves – Big, Big Problem blog? Dr. Oaklander’s initial study suggested that IVIG can be helpful….
Good luck!
Lack of hair for a man can also indicate an imbalance in testosterone and estrogen. Seems a lot of men are low in Test. If estrogen is too high – the imbalance occurs. All sorts of issues when that happens.
Issie
Interesting – a blog on sex hormones is coming up….
Thank You forYour comments!It is very interesting you mention hair loss- I used to have plenty of fair hair on my legs and arms- they basically dissapeared since my SFPN symptons began!My skin is smooth, shiny, very thin. You mentioned a vascular conection. My carotid artery is blocked up to 80% with a glutenous mass of colestrol- lump- a dangerous form to become detached and a massive stroke could appear….I wonder if there is a connection- but nobody takes action to give me an answer. The specialists never concentrate on the whole body and its present function- they just section it off…extremely frustrating and dangerous too…..
I would love to see her, or be involved in a study. Glad I’m in the correct state – just the wrong end of it, but that’s easily fixed. There were only two things in the above questionnaire that didn’t apply. Now we have two potential participants!
Cool. She is apparently collaborating with Dr. David Systrom – a Boston pulmonologist who has been studying the exercise intolerance in ME/CFS/FM/POTS. Both think the small nerves are getting whacked….
Boston could be ME/CFS/FM central over the next couple of years….
Who knew?
She’s not taking new patients but any doc can order the test (skin biopsy and autonomic testing) which can be done at MGH or Faulkner Hospital.
Do you know what is involved in the autonomic testing? I found a neurologist near me that does the skin biopsies. Is there a specific name or a reference regarding this autonomic testing that I can share with the physician? Thank you.
Lost the hair on my lower extremities a couple of years before I was hit with ME/CFS, Drs didn’t seem to be concerned. Very interesting, I can check off every symptom but two. Thank you once again Cort.
Having other autoimmune diseases and a family history of such I believe that eventually “they” will find fibro/ME/CFS/POTS to also be autoimmune related. Also, include MCAD. I’m in if the need more subjects.
If you look at the talk given by Mark Davis at the (OMF) community symposium you’ll see that people with ME/CFS have activated T-cells. I think Mark Davis is proposing that ME/CFS is an autoimmune T-cell disease. On the face of it this would appear to be consistent with Cort’s statement above i.e. “A recent Oaklander treatment study —did suggest that immune modulators may be helpful for many with SFPN”. However, if it all those with ME/CFS had an autoimmune B-cell disease, then rituximab would have worked;it may be that some do have an autoimmune B-cell disease.
I’m still not clear what the test for SFPN is and the confidence you can have in it. Also, how does this link to the metabolic ME/CFS studies by Armstrong, Naviaux —sphingolipids– . Interestingly, Armstrong did suggest gut problems (including motility?), check out his 2016 webinar.
I think this looks interesting but it needs to be linked to the immune findings and metabolic findings. OMF have decided to fund Mark Davis’s T-cell work, i.e.out of donations (no NIH grant yet) so maybe that will turn up something.
SFNP still could be a co-morbidity with FM, like many other things. Not just a coincidence that people have co-morbidities, as if they came down with two or more things by sheer bad luck, but rather that they are already depleted in ways that render them vulnerable to further dysfunctions. There are so many differing FM patient stories.
“…All that may be needed, Dr. Oaklander suggests, is to remove the “neurotoxic” conditions causing the damage…”
Quite so! So whatever is causing the neurotoxic conditions, is the cause of FM. In some people it also results in SFNP. I think the one thing that is common to everyone with FM, is myofascial adhesions. I think this is a result of toxicity, period. This toxicity could have multiple contributors. I think people with FM have ended up in a vicious circle where the toxicity creates myofascial adhesions, which then interfere with micro vessel flows and nerve signals, leading to toxic energy metabolism and debilitated post-exertion toxin clearance, leading to worsened toxicity, leading to increased adhesions.
So many hypotheses I am reading, have the potential to be just one more piece in the “toxicity / myofascia” puzzle rather than “the” explanatory hypothesis in its own right. Just as I have been saying that of course the CNS is rendered dysfunctional as a consequence, likewise SFNP is a possible consequence of bigger-picture dysfunctions.
I agree with you on the myofascia adhesions. Although it’s very painful to have those broken up and released, I have it done about once a year. The benefits of my body moving and feeling better outweighs the pain and bruising of the procedure.
Thank you for your thoughts on this.
Kim, how do you have those proken up and released?
Not really correct. These two conditions cannot be co-morbid, at least not based on current medical definitions (look on criteria 3).
Fibromyalgia diagnostic criteria is quite simple, and include:
1. Widespread pain lasting at least three months
2. Presence of other symptoms such as fatigue, waking up tired and
trouble thinking
3. No other underlying condition that might be causing the
symptoms.
I live in Mass and would gladly take the test
Is this actual questionnaire available anywhere so I can give it to someone?
The only thing I could find on the questionnaire was in the results of the study which is embedded (in small print) in the blog. If you can read them it does list the symptoms the questionnaire asks about but does not list the actually questions.
The questionnaire is probably in this study – https://www.ncbi.nlm.nih.gov/pubmed/28063957 – but I haven’t been able to get it yet.
Re your side note “…FM finds its unhappy home at the NIH in the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS). NIAMS is an Institute that would apparently rather treat FM as a behavioral disorder than a physiological one and has little interest in funding it. (Funding has actually dropped over the past five years). With its funding among the lowest in the NIH – just $9 million a year or about a dollar a year per patient – perhaps FM would do better if it moved to the Neurological Institute (NINDS)…”
I am afraid that FM is indeed a physiological disorder, and the “physiological expertise” gatekeepers are acting like they are corrupt, charlatans, and sadists, towards FM sufferers. Something I have been reading, is the work of fascia experts like Robert Schleip and Klaus Eder and various colleagues, and a sad story is emerging. Many of these experts commenced their careers as physiotherapists and other hands-on therapists, and became so frustrated at the arrogance and closed-mindedness of “mainstream” medical practitioners and researchers in the area of biology and pain, that they made costly vocational changes into that field. For example, Robert Schleip got his PHD in human biology in his forties, and became Director of the Fascia Research Institute at the University of Ulm.
The so-called experts in mainstream medical biology have an insufferable arrogance towards those in hands-on vocations, who often have studied human biology in equivalent depth already. Central to this arrogance, is the topic of hands-on palpability of tissue deformation as a form of diagnosis. The “mainstream medical” experts want to “see something in sophisticated scanning techniques”, otherwise what patients and practitioners can feel with their fingertips is irrelevant, and hands-on treatments that are successful for millions of people over a long history, is just so much pretence, quackery and auto-suggestion!
This arrogance extends to the withholding of funding for anything based on palpability, and an anti-scientific incuriosity regarding the uselessness of their own much-vaunted sophisticated diagnostic tools so far. Far from wishing to improve their tools as a result of this debacle, they do not even want to know about promising new developments that potentially confirm what the hands-on therapists have been saying all along.
http://www.doctorschierling.com/blog/thoracolumbar-fascia-videos
Whatever the motives, I am starting to conclude that the “mainstream medical biology” establishment is guilty of one of the worst ever systematized abuses of a massive victim cohort; not just those with FM but numerous specific chronic pains and dysfunctions for which “alternative” diagnoses and therapies have actually been the HONEST and objective ones all along! I fail to see what is objective and scientific about deliberately ignoring visible / concrete / palpable evidence. By this standard, if a cancerous growth that was pressing on vital organs still looked like normal tissue in an MRI scan, it could be ignored, the patient dismissed as hysterical, and their pain dismissed as a CNS heightened by the patient’s hysteria and hence their own fault anyway, the remedy being “Cognitive Behavioral Therapy”!
Phil! I SO agree. Many examples of this and here is one. There were some studies in the past showing that certain types of massage by a highly-skilled therapist were rated by patients themselves to have the longest lasting, most helpful results. And, in fact, that is true for me. It took almost a dozen massage therapists before I found two who can help me greatly, and have often wondered if I would be MUCH improved if I could go weekly. But insurance won’t pay for it.
Years ago I sent my Blue Cross plan an inch-thick packet of information including studies and trials, asking them to reconsider paying for my massages. Of course it was fruitless. They’re run by lobbyists I suppose; likely mainly the drug industry. “Follow the Money”…because I finally called when they didn’t respond to my packet of information. That packet took me a LOT of time to put together and they didn’t even feel it necessary to reply or respond at all. The telephone customer service manager finally gave me an answer. No-never-not happening, “BECAUSE THEY HAVE NOT FOUND MASSAGE TO HAVE LONG-LASTINGS EFFECTS.” So of course here was my logic- I immediately asked what long-lasting effects they think are possessed by the expensive drugs they’ll approve. Bingo- she was stumped, but remained certain I couldn’t expect even receive a written answer.
Prof Phil, yup, it’s like having a car with a flat tire, with allopathic’medicine’ ignoring the nail [magnesium deficiency:’Early signs of magnesium deficiency include loss of appetite, nausea, vomiting, fatigue, and weakness. As magnesium deficiency worsens, numbness, tingling, muscle contractions and cramps, seizures, personality changes, abnormal heart rhythms, and coronary spasms can occur…hypocalcemia or hypokalemia (low serum calcium or potassium levels, respectively) because mineral homeostasis is disrupted.’ https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/ Much more, https://www.easy-immune-health.com/signs-of-magnesium-deficiency.html ], but insisting it’s the tire’s air/rubber compound that needs further analysis. If mainstream med docs fixed cars, we’d all be walking, not driving. BTW, after a short time of transdermal Mg usage, my Rolfer was amazed at the transformation of the body & the ease with which it accepted his corrections/re-alignments.
Holy Cow! That questionnaire nails it for me. Yes, yes, yes, to so many items on it. So glad to know that someone else out there knows about this misery. Most of my friends just think I’m so weird.
Agnes wrote:
“I’ve read all the symptoms, and I must admit that I’m suffering from many of these symptoms. I also have Myalgic Encephalomyelitis. No energy, time of récupération very long, may be days after I go out for a grocery shopping, that means a lot of time in bed.
I hope that funding would be more important because we lose everything agpfter this diagnosis, work, social life. Friends. Capacity to cook a more complicated meal.
I eat the same diet singe my diagnosis, quick thing, I tried to eat healthy though, but I’m sure that I must be lacking important nutrients.
My last blood work shows that I was low in iron. My NK Celles are almost always way below the Norma as well as the ANA.
I think we’re going to hear something really interesting on iron and POTS from Mayo any time now. For an illuminating iron story check out the Iron Man blog – https://www.healthrising.org/forums/threads/iron-man-a-young-persons-pots-me-cfs-recovery-story-pt-i.4803/
Isn’t massive destruction of RBCs one of the more common ways to get low iron and ferritin?
If so then it might link to your previous blog containing information on “porblematic/unelastic” RBCs being vulnerable to “squeezing/destruction” in small hair vessels https://www.healthrising.org/blog/2017/12/21/urgency-ron-davis-chronic-fatigue-research-center/
I am grateful and excited that Dr. Oaklander is doing this research. She said she’ll be trying to find and test cheaper drugs than IVIG which probably most people couldn’t get covered—that is my understanding of what was happening.
I was tested and diagnosed with SFN some years back. I have ME/CFS and also Myofascial Pain Syndrome. Many but not all people with FM have MPS, I heard an FM expert say years ago.
The aching from it, contractions and lumps are something. I have two great rollers that I use, one a very large, firm foam roller and the other a polished wooden one of smaller dimensions that can be used many ways. The wooden one is called a MA Roller (forgot how to write it). And I have to do a lot of stretching! There is no way that any pills or even massage would do the trick unless I were able to get skilled Myofascial Trigger Point work every single day. Practitioners with sufficient knowledge and skill are very rare. But luckily, stretching and the rollers keep me out of pain domination. If I slack off, I pay for it with interest.
The small fiber neuropathy or polyneuropathy that is going on is not something I can do anything to fix. It is increasing. I don’t know what the relationship is between/among the ME/CFS, MPS, SFN or Polyneuropathy.
As I get older, my neuropathy gets worse and so does my all over pain. Mayo recently wanted to repeat Autonomic testing. But I didn’t do it. If she sticks me with a pin and I don’t feel it – there are nerve issues. If you feel bees are stinging, there is a vise, have shooting pains and numbness – there is neuropathy. It appears to run in my family and both my parents and sis and I are all Dxd with FMS. You don’t need expensive test – just educated sense. I don’t need to spend thousands to tell me what is already very evident and a one cent pin prick can explain. Now whether it is autoimmune connected – I’m not sure. But we already know I have POTS and MCAS and EDS with FMS. I’d rather my insurance/and me pay for testing on something not already established. I still don’t have a good enough bandaid. But I’m still working on it.
Issie
I have idiopathic peripheral neuropathy and some of the symptoms on the list are those if IPN. I have medication to treat all my symptoms so if I were younger, I could work. But at 78, that’s for sure out of the question. However, the biggie is cognition. I had the ability to do many things at once and do them well. I’m lucky to do one thing well. I’m so forgetful its disgusting. I also have ME and those who are the sickest with ME sometimes respond to a drug that seems to help. Sorry, can’t remember the name. I wonder if it would help those with severe FM. I’m diagnosed with moderate ME and FM thanks to now retiring Dr. Lapp.
I would very much like to participate in any future studies. How do I sign up?
Kendrick wrote: All I can say is WOW! I suffer with the majority of these symptoms. I have CRPS, RA, Sjogrens and CFS in addition to Fibromyalgia. A lot of the symptoms overlap, which I imagine would make it difficult to diagnose, based on these questions. But it is a real eye opener
After developing symptoms like this in regard to 20+ surgical clips that were left in my neck (without my consent nor notification; they were discovered by accident 2.5 years after surgery) I wonder how many people on here have metal in them, either from breast biopsies or gallbladder removal, or other surgeries? Metal is used frequently and the recipient never told. In my case, if they had asked, I could have told them I have allergies to both nickel and titanium dioxide. Even so called pure titanium is often contaminated with alloys.
Response to Agnes above (et al): Does everyone with ME/CFS know about NUUN? Runners use it as a healthy alternative to gatorade: it has vitamins & electrolytes (caffeine optional) so even if you cannot prep food or eat a diverse diet, vomit and/or have diarrhea, you are getting the basics. Each tablet is dissolved in 16 oz water. Thanks for the informative blogs Cort & MERRY CHRISTMAS everyone.
I’ve heard good things about NUUN. Check out some other ways to increase blood volume in Health Rising’s Increasing Blood Volume Resource section
Cort I read a study of 1,300 CFS Pt 90% had a cholesterol > 225
I have been diagnosed with FM in 1999 ( I also have Myofascile Pain Disorder) I heard a report on the excessive pain at an early age before part of the Sympothetic pathways were completely mature, and as a result when later in life a trigger of a new excessive pain causes the parasympathetic and sympathetic to go into hyper drive and not shut off quickly. This would coincide with an extreme episode of pain at age about 5th grade when a huge boil was excised in around the lymph nodes in my leg , and years later just prior to my symptoms showing for FM that I had my hands and face burned by trying to light a gas stove, in which my body began to shake as I was having a shock response to extreme pain. The micro nerves being under fire by the gas ball explosion. Mental stress as well as physical stress sets off my FM . One of the first symptoms was while my husband is driving and stops suddenly avoiding an accident my arm begins to hurt . I noticed this happen often in such situations. Loud noises also cause discomfort. The report showed how the damaged base of the brain that controls these emergencies cause the later in life’s FM to be triggered by pain.
I have been diagnosed with fibromyalgia . My left leg is very stiff It has felt for over 9 years or more ,physically different . Its as if the oxygen isn’t getting to the nerves and muscles . It has felt tender for all those years and seems to be damaged . I would like to know more about what is causing or has caused this problem .Reading the article on neuropathy has highlighted that more investigation is needed to understand this condition.
I have considered oxygen depletion to be a component of my leg problem I hope research in this area will bring promise to help heal us . Happy to be included in this .
4th possible explanation: active inside for years, but showing up in skin only later. A deployment from inside to surface, time related. The manifestations worsening with time attract a series of apparently unrelated diagnoses, or a series of not-well-understood “diffuse” or “vague” syndromes’ labels.
(I suffered both)
I developed every symptom on this list after receiving treatment with fluoroquinolone antibiotics. This antibiotic class does widespread damage to the peripheral, autonomic, and central (brain and spinal cord) nerves, resulting in a form of disability that often gets diagnosed as fibromyalgia.
Just something to look into if you developed fibro after a course of cipro, avelox, levaquin.
I have read elsewhere that Dr. Oaklander has stated the small fiber nerves can heal if the neurotoxin is removed. Has anybody found a way to determine if the neurotoxin might from be a fluoroquinolone antibiotic like Cipro or Levaquin or from other antibiotics that can cause neuropathy like Macrobid (nitrofurantoin.)? How do we recover if that is the neurotoxin that caused the small fiber nerve damage? They say women are more likely to get fibromyalgia. Well, women are more likely to have been prescribed these for urinary tract infections.
I have terrible paraesthesia all over but mostly in my legs. I have the sharp prickling and shooting pain. This started in 2019 and i’m actually at my wits end. I’m a 41 year old man and my life has been totally ruined by this. What I really give up with is the endless complex talk that is impossible to figure out. Every post has someone suggesting something else and some complex mix of medications and tests and research. It is too much for me and I feel like I’ve reached the end of the road.
Help me. I have chronic parasthesia and it’s all over and making my life a misery. My skin is sensitive to clothing too. I also get muscle twitching. I recently came back from holiday abroad in Porto, Portugal and I noticed I had days where I was not too bad there. Since coming back my symptoms have become much worse and I now feel more pain, pricked, etc. I’ve noticed now that I get pains in my back.
I’m a 40 year old Male who was very fit and healthy. They can’t diagnose anything but Sicca. Lip biopsy should some inflammation but no diagnosis of Sjogrens and blood is clear. Dry hair, eyes, and sometimes rashes. My girlfriend is gone and my new life in Spain with it.
This is after a year and a half of battling. I have some neurotonin but it makes me so tired.
It is also always worse when I have my suit trousers on and when in the office at work. The trousers are not tight.
I had days abroad where I was pretty good what does this mean?
What about fibromyalgia? Have they checked for that? Lyrica and Cymbalta might help. There’s also low dose naltrexone – check on this website for more information on that.
The decline in symptoms could be due to reduced stress. Stress easily exacerbates FM and similar diseases. It’s also possible that you could be living or working in a moldy or unhealthy house….
I don’t know. The Rheumatologist said possible Fibro but they said there’s no further tests and I was discharged. I am British and on the National Health Service. The Rheumatologist was private. I battled for medications but they say there’s nothing more they can do now. I’m not living in a mouldy house no. I talked about QSART and biopsies for Small Fibre Neuropathy but have been told my 2 separate GPs that these tests don’t exist. They have never heard of them. Awful. 1 1/2 years ago I had not a single symptom of anything and was ready to move abroad.
Thank you for answering me. I just wish I could call and speak to someone too.
Hi Johnny, I have similar symptoms to you. The Small Fiber Neuropathy pain is a nightmare to live with. My symptoms accumulated as a result of build up of toxins in my body that I was unable to get rid of. The worst of it occurred after an MRI with contrast agent Gadolinium. Have you ever had gadolinium? I am finding huge help in an algae supplement called BioSuperfood, developed by a scientist Dr Kiriac. You can read about it on various sites on the internet, the testimonials are amazing. It has helped my pain and energy a lot. I also have that horrible skin sensitivity which makes clothing a nightmare. Certain environments I am better in, I think it is places that place less stress on my body, either in terms of less stress (emotionally) eg when I’m more relaxed, or less toxic. I am also better if I don’t sit still all day, but get my body moving. I am very sensitive to EMF’s (eg around lots of computers). I also do a lot of Dr Joe Dispenza meditations and follow his amazing work. There is hope, I hope you find it too.
Ps I know many people who find nortriptyline helps neuropathy but I have not personally tried it as I like to stay clear of pharmaceuticals as I cannot process more chemicals.
Connie
Hi Connie, I wish I could talk to you and others somehow on WhatsApp etc but not sure if I can leave details here. At this stage I’m not sure I care. I just posted on Reddit however on the Small Fibre Neuropathy section. Johnny Zenith.
Hi Johnny, sorry for some reason I did not get your reply 3 years ago. I am a lot better now, and put it down to BioSuperfood Algae (by BioNutrition) and doing Joe Dispenza work too (starting with reading his book You are the Placebo). Sorry I missed your reply so long ago.
Are you still finding success with the Bio Super Food?
Thanks!
Hi D.L, yes absolutely, I highly recommend giving BioSuperfood algae by BioNutrition a go. I am symptom free now, I just re-read my post from 2019, and it is amazing how far I’ve come to be pain free now. I also follow an anti-inflammatory diet a bit akin to Terry Wahls which helps, and keeping toxic exposure low as possible. Where do you live? There is a good supplier in the UK where I am http://www.bluedragonessentials.com, and in the US there is http://www.thealgaeanswer.com . All will often give free advice on taking it.
Wasn’t this discovered by Prof. Üceleyr in 2013 already? https://www.ncbi.nlm.nih.gov/pubmed/23474848
i was diagnosed with FM in 2005 and also sarcoidosis but had symptoms that never really matched FM like unary incontance and urgency.
i never did believe i had FM and now with all the studies about SFN and FM i found many like me with sarcoidosis get diagnosed with one or the other depending on if they go to a rheumatologists or a neurologist
O know for sure I have both
The symptoms of both fit me to a T. I have suffered for years and can’t find
Any help.
Hey Cort,
this is an old article – I know. But whenever I do my research I come across your older articles and I regularly read your newest ones.
I have given small donations when I could, because your work is so so important for all of us. But today I felt the strong need to tell you how much your work means to me and to thank you for all that you are doing.
It is not only the excellent and comprehensive information, you give me hope. That so many people care. That we are not alone. That something will change eventually.
Thank You.
I wish you a happy day, many greeting from Germany
Anna
I have had FM for 20 yrs. Affected me only when laying on my side, couldn’t put one leg on another or arms (still can’t). Almost 5 yrs ago had a TIA and from there went right downhill. Been to several drs and finally a new one thought I may have Small Fiber Neuropathy and I’m being tested now. Continuous Pins and needles in my feet, legs, hands, arms. Pain in odd areas comes and goes. Terrible fatigue even without exercise. Sweating, which I never did. The myelin in my brain is disappearing. Complained about my eyes not being clear when watching TV, told they haven’t changed. There’s more but, I finally feel heard. Have been so overlooked for so long! Would do a study in a heartbeat if asked!