

“The bottom line is that we should rethink this whole area and encourage proper clinical trials.” Dr. Nancy Klimas
This article is the last of a three-part series on IVIG which came out of my attending the 2018 Dysautonomia Conference in Nashville, Tennessee.
- An IVIG Chronic Fatigue Syndrome (ME/CFS) / POTS Treatment Success Story: IVIG#1
- Are Chronic Fatigue Syndrome, POTS and Fibromyalgia Autoimmune Dysautonomias? IVIG #2
- The Case for IVIG Treatment in Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia, Small Fiber Neuropathy, and POTS: IVIG#3
IVIG is a very expensive but commonly prescribed immune modulating drug used extensively in autoimmunity and immune deficiency. The article examines the evidence base for IVIG in chronic fatigue syndrome (ME/CFS), fibromyalgia and POTS and looks to the future to see what possibilities may emerge.
I queried ME/CFS experts on their use of IVIG in ME/CFS/FM and did a literature search. Four experts answered – Dr. Lapp, Dr. Sivieri, Dr. Klimas and Dr. Levine. Dr. Lapp and Dr. Sivieri sent short replies and Dr. Klimas and Dr. Levine – both obviously very interested in this drug – sent several page-long answers. Dr. Klimas, an immunologist, provided both a historical and present-day overview of the drug’s use in ME/CFS.
About IVIG (Intravenous Immunoglobulin) Treatment
Available since the 1950s, IVIG contains massive amounts of gamma globulins or antibodies which are gathered from the plasma of at least a thousand healthy donors. (Dr. Schofield noted in her video, though, that it probably comes from many thousands more.) Filtering the plasma to get the antibodies and produce the IVIG takes upwards of nine months.
Dr. Klimas believes that the pooling of IVIG from a large population gives it a “tremendous advantage”. If an infection is the problem, then potential protection provided by the product is so complete that you don’t necessarily need to know what virus is present – you just need to boost your immune functioning with the product.
IVIG is a blood product used to fight off infection, boost immune system functioning or tamp down inflammation in people with inflammatory, autoimmune or neurological diseases like Guillain-Barre syndrome, lupus, multiple sclerosis and others. People with immunoglobulin deficiency states (low levels of immunoglobulins or immunoglobulin subclasses) who experience recurrent infections are eligible for IVIG.
First used to boost the immune systems of people with immune deficiency disorders, IVIG is now mostly used as an anti-inflammatory treatment to combat autoimmune disorders. It’s been used in virtually every autoimmune disorder. Dr. Klimas reported that the list of diseases treated with IVIG grows longer every year. IVIG has an advantage over some of the monoclonal treatments used in autoimmune diseases because it’s safer and not as immunosuppressive.
It’s also used as a treatment of last resort in a number of disorders.
Three Types of Gamma Globulin Products
Gamma globulins can be administered in three different ways – via infusion (IVIG), subcutaneously, and intramuscularly.
Intravenous gamma globulin (IVIG) – The most commonly used form of gamma globulin is administered intravenously, usually once a month but sometimes weekly. If it’s administered monthly, IgG levels will rise and then dip, leaving a gap in coverage during the month.
Subcutaneous gamma globulin – One advantage of the subcutaneous product is its ability to be self-administered. Dr. Lapp pointed out that you can even throw it into your suitcase and travel. The fact that it produces steady levels of immunoglobulin makes it probably more effective in people who are fighting off infections. Dr. Levine reported that she’s switching some of her patients to weekly subcutaneous injections of Hyzentra in order to achieve more even levels of gamma globulin in their bloodstream.
The subcutaneous form has mostly been used to restore immunity and fight off infections, but Dr. Klimas reports that for people with autoimmune diseases a single high dose IV infusion followed by weekly, lower dose subcutaneous injections can be effective as well.
Intramuscular gamma globulin – is not commonly used. In the first 10 years of her career (80s and early 90s), though, Dr. Klimas reported that she used a lot of IM gamma globulin and her clinical impression was that it was very helpful. During the Gulf War (1991), however, the army bought all of the available IM gamma globulin and it was off the market for several years. When it came back on the market it was prohibitively expensive.
Now, even though intramuscular GG is less expensive than intravenous gamma globulin, she’s rarely able to get it. She finds it easier to get IVIG or the equally expensive subcutaneous product.
Brand
IVIG is produced by a number of companies that make different brands of IVIG. Because the IVIG brands can differ in so many areas (concentrations, formulation, osmolality, product stabilizers, sodium concentration, anti-infective activity, IgA content and pH) it can, at times, be important to match the patient to the right brand of IVIG.
Dr. Levine prefers Gammagard. Dr. Klimas reported that the insurance company usually decides the brand and her experience is that the results are generally similar across brands.
Dosing Regimens and Safety
IVIG is usually given every couple of weeks, often needs to be given continuously (is not a cure) and is incredibly expensive (can cost $100K a year). The risk of aseptic meningitis is low but increased in patients with autoimmune dysautonomia. (That problem can be ameliorated by slower infusions and hydration). Blood clots and kidney toxicity are two other rare complications.
Two dosing regimens exist: a low dose one for patients with low antibody levels (immune deficiencies) and a higher dose for patients with autoimmune dysautonomia who need the extra antibodies in the high-dose IVIG to swamp the bad ones producing their disease.
Schofield usually starts out with 1 gram/per kg in her autoimmune patients, and that’s usually enough, but she can go up to two g/kg monthly.
Schofield warned that giving IVIG slowly and using aggressive hydration is important in her POTS patients. She generally starts off with 1/4 g/kg weekly and works up to 1 g/kg given all at once. (Some patients peak at ½ g per kg. She warned never to give IVIG and fluids at the same time.)
Schofield and Dr. Klimas agreed that in ME/CFS (where IgG1 and IgG3 – which fight off viruses – are more important), weekly injections are more likely needed to ensure constant antiviral protection in some patients because the half-lives of these antibodies are shorter.
Why IVIG Works When it Does
Why IVIG works when it does isn’t exactly clear. Several attempts have been made to explain IVIG’s success. Several suggest that IVIG simply swamps the immune system with good antibodies thereby displacing bad ones.
One idea is that it halts autoimmune processes by stopping autoantibodies from binding to their targets. Another is that IVIG binds to and halts the autoreactive B-cells from producing autoantibodies.
Yet another is that it hastens the degradation of pathogenic antibodies or that it scavenges complement (C3b, C4b) proteins before they can cause tissue damage.
All these hypotheses may, in fact, be accurate in different diseases.
IVIG in Chronic Fatigue Syndrome (ME/CFS)
Studies
Significant interest in gamma globulin resulted in several clinical trials in the 1990s that had mixed results. Peterson’s 33-person placebo-controlled blinded 1990 study found widespread evidence of immunoglobulin deficiencies. Despite restoring some of the deficiencies, the six-month trial of IVIG given monthly found no evidence of significant improvement.
Hickie et. al. found improved mood and immune functioning in a smaller 1992 IVIG trial and Lloyd’s placebo-controlled 1990 trial found significant improvement in approximately 40% of patients with many resuming work and other activities. Lloyd’s larger 99-person 1997 follow-up trial, however, was unsuccessful, as was a smaller American trial that targeted IgG deficient individuals. The Lloyd study, the largest ever done in ME/CFS, found high levels of side effects and reported that “Intravenous immunoglobulin cannot be recommended as a therapy for the treatment of CFS. A better understanding of the pathophysiology of this disorder is needed before effective treatment can be developed.”
Dr. Klimas, however, pointed out two glaring problems with the study. First, it included autoimmune (high dosing) patients and it used a subpar product whose impurities eventually forced it from the market. If the dosing had been lower and a different product had been used, the outcome might have been different. Plus, the trial only lasted for three months.
Dr. Klimas believes that Stephen Straus’s 1997 editorial, “Intravenous Immunoglobulin Treatment for the Chronic Fatigue Syndrome”, published in the American Journal of Medicine, effectively put an end to IVIG clinical trials in ME/CFS.
Rowe’s 1997 IVIG trial, on the other hand, found significant functional improvement as did her five year follow-up. Rowe’s five year follow-up was reported in a publication (Journal for Chronic Fatigue Syndrome) that was unfortunately not included in medical indexes such as PubMed and therefore was not widely disseminated.
In 2003, Jonathan Kerr reported that IVIG treatment in three cases of parvovirus associated ME/CFS led to a resolution of symptoms, improved functional ability and normalized cytokine tests. A 2005 case report of a young boy with parvovirus associated ME/CFS treated with IVIG had the same result. A 2015 case report of an ME/CFS patient with documented parvovirus infection, however, found IVIG had a paradoxical effect, increasing viral replication and symptoms.
Autoimmunity, Inflammation and ME/CFS
Dr. Levine believes recent findings indicating that antibodies are targeting receptors on blood vessels in a subgroup of ME/CFS patients will open the door for IVIG treatment for ”autoimmune autonomic gangliopathy” in this group. Studies are underway at several centers to assess IVIG’s effectiveness in these patients. The German CellTrends lab is the only lab doing these tests at the moment.
Dr. Levine reported that a diagnosis of inflammatory neuropathy” (burning, pain, tingling in the extremities and sometimes loss of reflexes and/or abnormal EMG response) which has been validated by a neurologist may open the door to IVIG treatment as well. (The dosing schedule for inflammatory neuropathy is a bit higher and more frequent (1-2 gms/kg for a 50 kg woman or 50 to 100 gms daily for two days in a row every 2-3 weeks for a total of five or six doses.)
Dr. Klimas believes gamma globulin could offer a two-for-one option for one set of patients: ME/CFS patients who have an immune deficiency and viral reactivation but who also have an autoimmune condition.
See below for autoimmune diagnoses which may in the future assist some people with ME/CFS get IVIG.
Effectiveness
IVIG appears to be like many other drugs/treatments for ME/CFS. Some people – probably a small percentage – do really well, more do moderately well, and some do not respond at all. Dr. Sivieri has reported before that IVIG can be effective but believes it works best when administered within a total treatment paradigm.
In Dr. Levine’s experience, gamma globulin given either intravenously or subcutaneously is a moderately effective treatment in ME/CFS patients who frequently suffer from upper respiratory infections or who experience chronic flu-like symptoms. If infections are a problem, sometimes she’ll reduce the infusion frequency (to every 6 weeks) during the summer months.
IVIG’s effectiveness should increase as the autoimmune subsets in ME/CFS/FM and POTS become better elucidated and more easily targeted.
Getting Coverage
All the experts agreed that insurance companies want to see evidence of an immune deficiency and active infections. Dr. Lapp reported he only had a low number of patients on the products because insurance companies will “fight harder than a marlin on a hook” to keep from paying. Similarly, Dr. Sivieri wrote that while he is still “doing a fair amount” of IVIG, it is, in his experience, getting harder and harder to get insurance companies to cover it. If the trend continues, he worries about IVIG becoming a “lost” treatment.
Dr. Levine reports that insurance companies most commonly want test results showing that a person’s immune system does not get boosted by a vaccine shot. If the immune boost is not seen, the patient is diagnosed as having Common Variable Immunodeficiency (CVID) and can be eligible to receive monthly IVIG infusions.
Even though “dead” vaccines seem less problematic than live vaccines in ME/CFS, administering any kind of vaccine to an ME/CFS patient can be problematic. Since insurance companies have decided that the vaccine test is the gold standard for coverage, getting it via other routes is more difficult.
Lacking the vaccine challenge, Dr. Levine’s experience is that at least four annual episodes of sinusitis, bronchitis or other infections requiring the use of antibiotics are needed to get covered. (A bout of sinusitis can send some people into a relapse and IVIG can stop that.) She noted that insurance companies will sometimes even request receipts for antibiotics from the pharmacy to show that the patient has filled these prescriptions.
Finding evidence of autoimmunity (autoimmune polyneuropathy, autoimmune autonomic gangliopathy) is another option which may emerge in the next couple of years.
If you have ME/CFS or fibromyalgia, keep reading! The next sections may apply to you.
IVIG in Small Fiber Neuropathy (Polyneuropathy)
These families’ relentless testing for treatable causes of their children’s chronic pain generated the abundant data analyzed here. Oaklander and Klein
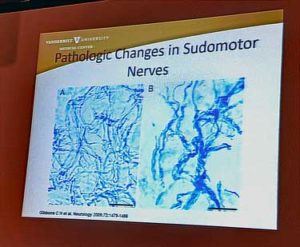
Dr. Oaklander reported some promising results using IVIG in children with a putative diagnosis of small-fiber polyneuropathy (SFPN); e.g. small fiber neuropathy (SFN). SFPN or SFN has been documented in fibromyalgia and is being documented in chronic fatigue syndrome (ME/CFS). (Both Dr. Systrom and Dr. Kaufman have found it extensively in ME/CFS; Systrom will presumably report on this soon in a study.)
This was an ME/CFS/FM/POTS/EDS type group for sure. The most common “label” attached to these patients was fibromyalgia. Others included most of the long list of diseases or conditions associated with this illness complex: “functional disorder”, central sensitization, chronic fatigue syndrome (ME/CFS), POTS, irritable bowel syndrome, migraine, chronic headache, EDS, myofascial pain syndrome and chronic (treatment resistant) Lyme disease. Almost 70% of the participants were disabled. Sixty-one percent attributed the onset of their illness to an instigating infection or injury.
IVIG was tried in eight patients who didn’t respond to corticosteroids or who required long-duration treatment. Three did not respond but five received significant improvements including, in those who were tested, improvement on autonomic tests (Tilt, Valsalva, heart rate variability).
Autoimmune SFPN (AaSFPN)
Now calling the condition “autoimmune SFPN (aaSFPN)” Oaklander’s larger IVIG study (n=55) found 74% of the participants rating themselves ‘improved’ and their neurologists calling 77% of them IVIG responders. Almost 40% reported that they were “very much improved”. Ten percent reported they were worse. For some reason, males responded spectacularly with 100% improvement rates while females had 61% improvement rates.
Sixteen percent of the participants entered a sustained long remission (average of 20 months). The study, interestingly, tried the highest suggested dose first (1.3–2.0 g/kg/4 weeks) and then titrated downwards, if necessary. It also lasted longer than many trials (at least 3 months).
Only one-quarter of the participants had a “systemic” autoimmune diagnosis (high ANA titers) while three quarters had a small fiber autoimmunity that was restricted to the small nerve fibers in the body (and wouldn’t be picked up by standard blood tests).
Except for transient infusion reactions (headaches, nausea, flu-like symptoms, stiff neck) which were common (60%) and addressed by slowing infusion rates, hydrating patients, etc., side effects were low.
The authors asserted that their results “imply that aaSFPN may be far more common than appreciated” and “provide strong evidence that medical insurers should no longer reflexively decline to pay for IVIG treatment of aaSFPN.”
The data is clearly calling out for a large placebo-controlled trial in SFPN. Given the rigorous classification of the patients, a successful larger trial could open the door for treatment of a significant subset of ME/CFS/FM patients with documented SFPN.
Fibromyalgia
Back in 2008, Carol found that a third of fibromyalgia patients had a chronic demyelinating polyneuropathy. He reported that a brief IVIG treatment significantly improved pain, tenderness and strength.
Postural Orthostatic Tachycardia Syndrome (POTS)
No studies have examined IVIG’s effectiveness in POTS, but Goodman reported good results at the 2018 Dysautonomia conference and recently published a case report in which IVIG, low dose naltrexone and antibiotics (for SIBO) resolved the POTS of a severely ill patient.
In 2018, Dysautonomia International funded the first placebo-controlled pilot IVIG trial ever in POTS. (The trial is already filled but if it succeeds a larger trial will open up.)
Conclusion
The case for the use of IVIG in treating ME/CFS/FM/POTS in the medical literature has mostly consisted of small clinical trials and case reports. The findings are mixed with more recent, better targeted studies being more positive, but the studies are too small and lack the rigorous placebo controls needed to get doctors to prescribe it or insurance companies to cover it. Larger studies are underway, however.
Suzi’s successful IVIG story demonstratives how effective the drug can be in the right ME/CFS/POTS patient. The real excitement with IVIG lies in the future with the validation of autoimmune subsets which affect the small nerve fibers the blood vessels or possibly the mitochondria in ME/CFS, FM and POTS. The emergence of those subsets will likely result in the reconfiguration of the ME/CFS/FM/POTS disease group. Successful IVIG trials in autoimmune POTS and small fiber neuropathy, if they occur, should open the door for more insurance coverage of this expensive drug in these groups.
IVIG Series
- An IVIG Chronic Fatigue Syndrome (ME/CFS) / POTS Treatment Success Story: IVIG#1
- Are Chronic Fatigue Syndrome, POTS and Fibromyalgia Autoimmune Dysautonomias? IVIG #2
- The Case for IVIG Treatment in Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia, Small Fiber Neuropathy, and POTS: IVIG#3
Other Articles from the Dysautonomia Conference
- 2018 Dysautonomia International Conference I: Small Fiber Neuropathy, POTS, MCAS and Vagus Nerve Stimulation
- The 2018 Dysautonomia Conference Pt. II: Could You Have a Spinal Fluid Leak? An ME/CFS, POTS, FM Perspective
- Dysautonomia International Conference Pt III: The Autoimmunity Revolution in POTS
- “Sticky Blood” – Antiphospholipid Syndrome, POTS, Chronic Fatigue Syndrome and Fibromyalgia – The Dysautonomia Conference #4
- Stagnant Hypoxia – Where Chronic Fatigue Syndrome and Hyperadrenergic POTS Meet?
- Promise Fulfilled – A New Chronic Fatigue Syndrome / Fibromyalgia Practitioner Steps Forth
Your Support Is Needed
The Nashville conference was one stop on an East Coast trip which provided a gold mine of information, inspiring new insights and a wealth of articles. Upcoming blogs include one on Dr. Klimas’s exercise study, a possible new treatment for fibromyalgia, talks with Jarred Younger, Avindra Nath, Vicky Whittemore, Dr. Pridgen and – on the return home – the folks at the Bateman-Horne Center. Next up on the travel agenda is the Stanford Symposium. Travel provides many opportunities but travel to the East Coast, in particular, is expensive for a small organization like Health Rising which hasn’t even begun to recoup its trip costs. If you find conference reports and other travel related blogs helpful and want to see these in the future, please support Health Rising.






Hi Cort,
Great piece. A couple of things I would add. I have been on IVIG for immunodeficiency (CVID) since May 2014. I have gone from 20% of pre ME/CFS self to over 70%, sometimes 90%. My IgG was low (558), but would not have qualified for IVIG (usually under 500 qualifies) unless my doctor did what is called a “vaccine challenge”. This is a test of the function of your IgG antibodies. This is a similar concept of NK cell function which so many of us have been tested for.
The Vaccine Challenge test: To achieve a baseline a blood test is run to see the function of 13 to 16 different serotypes of antibodies, typically for Streptococcus Pneumoniae. Then a vaccine is given and you wait. After 6 to 10 weeks the serotype test is run again to see if your immune system has responded to the vaccine creating and created its own antibodies.
This test was run for me and I had essentially zero protection at baseline and after it 6, 8 and 10 weeks I was still at essentially zero with no antibody protection. This demonstrated significant immunodeficiency and I was put on IVIG immediately. No insure problem at all. Several of my ME/CFS friends are also on IVIG after a Vaccine challenge test. My theory is that this is most likely to be positive in long term ME/CFS patients who’s immune system is exhausted. It also took at least a year before I felt better. The new antibodies in my system from the IVIG had to fight off a ton of low grade infections, so I was worse before I was better. If you have immune deficiency the normal Elisa antibody tests to determine if you have an infection are invalid! You don’t create functional antibodies so your test would be falsely negative. I now insist on PCRs for all tests. PCRs look for actual microbe DNA – more expensive but more reliable (if the microbe is still in your blood).
Best,
Pam
Such helpful information Pam! Dr. Levine said the vaccine test was the gold standard as well. It’s good to know that insurance companies accept it so readily. It’s also very good to know that it can take a while to work. I think one of the studies was only for 3 months.
I, too, have benefited from IVIG. My situation was similar to the previous poster, but I’d like to clarify a couple of misleading points.
First, it’s important to check with your insurance to understand the criteria needed to qualify. My policy does allow for some autoimmune conditions as well as for immunodeficiencies.
2) For immunodeficiency (CVID), my policy will allow it if total IgG is less than 700 and/or multiple subclasses are low, like subclasses 1 and 3 which can be low in ME/CFS patients. Also they like the Pneumovax 23 challenge, with only a 3-4 wait, rather than the lengthy wait shared by the poster above.
3) Finally, about 70% of IVIG prescribed in the US is for autoimmunity and people are getting it covered. It is more scarce in other countries as the US is the only country allowing donors to be paid, according to a recent article in The Economist magazine.
I get 1.5g/kg/mo divided into 2 doses. My ME/CFS specislist says my dose is not appropriate for SCIG (nor would I want it).
It has helped me kick 7 chronic infections and has improved my function.
Thanks for relaying that Learner1 and glad to hear that it kicked those infections. I take it that the battle has not been completely won. How much would you say it’s improved your functioning? I wonder if other immune improvements are needed?
Hi Pamela! If you don’t mind me asking, was this a CFS/ME specialist as opposed to a standard primary care physician that streamlined this Vaccine Challenge Test for you?
Who is your doctor?
Health Rising postings about IVIg treatment have been incredibly helpful to me. Thanks to this site, I have tapped into research that I shared with my neuro. She used it to easily get me coverage for IVIg. The treatments have been rough and outcome for me is still uncertain. But it’s hugely comforting to know I am getting cutting-edge therapy. I feel seen and, more important, I still have hope. THANK YOU for your amazing work. I am about to make anothr donation <3.
Cool! Glad you’re able to get a stab at it! Do you know how she got it covered? Are you taking at a couple times a month or once a month? Dr. Schofield Starts out with a couple times a month and then ramps up to once a month as the person’s system adjust. Also do you know if you’re taking a immune booster dose or the higherbautoimmune dose?
Thanks for the donation. That trip completely exhausted our resources.
I’m an autoimminute/polyneuropathy patient, so I get a heavy dose. I started out at 3 days in a row, once a month. That clobbered me pretty badly, so I was switched to 4x/month, every second week. Folks need to understand that it can be grueling, and that you need to stick with it.
Thanks…Good luck again. 🙂
With what neurologist have you spoked any recommendations because I struggle with neuropathy
I went to the top Immunologist in Southampton UK to be evaluated for (CVID)Common Variable Immune Deficiency he at that time ruled this out entirely he ran the entire Panel of IGG IGA IGM & other immune profiles
he said you do not have CVID, I asked about Genetic testing he said if my levels were off that would be the next step on (CVID) diagnosis. I then asked him about Gamma Globulin he said these words you do not need
Gamma Globulin even without (CVID) so all this stuff now about Gamma Globulin is to me not making any sense at all…I thought Klimas claimed to reverse illness with a steroid compound was the answer &
the route to go now? I have lost any faith in Klimas she is all over the place in theories & nothing as far as any answers now…
Yes I agree on Klimas. I came to that conclusion a long time ago.
Still far from convinced that our illness is primarily immune- driven.
Well, in Dr. Klimas’s defense I think ME/CFS/FM patients are all over the place as well. She does think she may have an answer though and she should begin a clinical trial this fall. It’s actually a fascinating story. More on that in a future blog.
Hope she proves us wrong.
With regards to the vaccine challenge, I would not touch any vaccine with the possibility of under-diagnosed Alpha Gal Meat Allergy IgE they contain animal products & a vaccine can kill one with AG…Dr.Levine
years ago was stopped giving Gamma Globulin to CFS patients…You have either CFS or you have CVID all along undiagnosed & this is what we will see here no doubts…I will not gey no vaccine or even Gamma Globulin
Not so clear cut, perhaps. I’m certain I have not had CVID “all along” as I was perfectly healthy until one day in 1993. My immune deficiency is the result of of whatever process ME/CFS or long-term untreated tick-borne disease has had on my immune system. I have both low IgG (below 500) (and low B cells and low NK cell # & function) and elevated autoimmune markers of various odd sorts.
Cort, have you asked Drs. Kaufman & Chheda at Center for Complex Diseases in Mountain View, CA about their experience treating ME/CFS patients with IVIG?
Not clear-cut at all which is totally not surprising to me since we often seem to slip through the cracks. I was eager to get Kaufman and/or Chheda’s reply since I know that they use IVIG. One of their patients told me they were able to get it covered through Medicare for her. Unfortunately they did not respond.
Hi Aidan. I’m curious about your experience with the alpha gal allergy. I have a CFS diagnosis, but I get a delayed reaction if I eat mammalian meat characterised by shocking inflammation, shallow breathing, headache, nausea etc. I spare myself a lot of bad days avoiding alpha gal (including vaccines) . You are the first person I’ve encountered that also has this issue with CFS. I’d be interested in learning more.
Thank you for this, Cort! I’ve been anxiously waiting for this article. I saw Dr. Levine for the first time yesterday. Once she gets the results from my labs, she will decide how to treat me. For the record, I have ME and Fibro.
Ah good luck. Dr. Levine’s Response to the questions regarding IVIG was impressive indeed. ?
How do I contact dr Levine?
Thanks
Susan Levine MD – https://doctor.webmd.com/doctor/susan-levine-99365fc4-92dc-47ae-bf02-299e447a7b1d-overview
To clarify, it’s my understanding that you can give fluids before or after IVIG, you just can’t dilute with saline and run them at the same time (unless you have a dual port system).
I totally agree that there is a lot of hope for IVIG in ME/CFS and related conditions. I also agree that insurance is also the biggest obstacle.
Thanks for clarifying that. That’s my understanding as well. Saline before or after IVIG, just not mixed in the Fusion itself.
Hi Cort
On a slightly differen, if similar track have you come across any feedback or data on the use of IV stem cell therapy in CFS?
The only thing I can remember is that at least ten years ago I imagine Dr. Cheney tried it in a small set of patients. I
don’t remember it being very successful. It was quite a while ago, though, and I imagine that the therapy has improved.
My ME/CFS Dr is beginning the fight with my insurance right now. I’ve had dysautonomia/ POTS since I was a child and it got much worse after I got encephalitis in my 20s.
I have progressive pain, low blood pressure, tachycardia, loss of feeling in my limbs and peralysis of my intestines.
I tested positive for small fiber neuropathy but it’s still going to be hard to get coverage. I came close to an IGG3 subclass deficiency but it wasn’t low enough.
I’ve also developed progressive dry eye disease and test positive for early Sjogrens antibodies. I want to do a lip biopsy to confirm, but I’m worried it will be negative and then I’ll be ruining my own case for coverage.
The vaccine test is interesting. I don’t have antibodies to chicken pox despite being vaccinated as a child. My CFS drs have advised against vaccines due to my immune abnormalities, but I’m so desperate to try IVIG I might do the vaccine challenge. I’d discuss the pros/ cons with my doctor first though.
I’ve also tried reaching out to my disability case manager to ask for help getting insurance approval. I doubt anything will come of it, but they should want me to try treatments that could help me get back to work.
“My CFS drs have advised against vaccines due to my immune abnormalities”
I wonder if that would be the reason why so many of us do get such a large setback after getting a flue vaccination? If you would be getting a yearly flue vaccination despite having ME anyway, it might double as a vaccine challenge test just as well?
I do struggle for 2 weeks after flu vaccine. I did some search and found a paper that flu vaccine causes low grade inflammation.(I don’t have the link handy at the moment). If that is the case, then inflammation sensitivity, rather than immune abnormality, could explain the struggle.
I’m planning to get flu vaccine regularly from now on, after nasty bouts last winter. 2 week struggle is still better than getting completely knocked out for a week or two.
The inconsistent and unreproducible results over 3 decades mean immune therapy should not be recommended for CFS, especially if it is expensive and/or has bad side effects. We don’t even know if the autoimmune subset exists, other than saying that it is auto/immune if the immune therapy works. That is a tautological definition that justifies immune therapy.
Hi Cort,
It is new to me that Celltrend tests for autoimmune autonomic gangliopathy (ACHR – AAB). At least this test is not on their webpage. There are other companies in Germany testing for the ACHR-AAB i.e. http://www.laborvolkmann.de/analysenspektrum/HTML/index.html (search under „g“ for ganglionäre…)
http://www.laborvolkmann.de/analysenspektrum/DOCS/00/ganglionaere-acetylcholinrezeptor-autoantikoerper.pdf
In addition there is E.R.D.E. – from Dr. Bimmler, a company besides Celltrend testing national and international for the ME/POTS aabs (ATR1, adrenerg 1+2, beta 1+2 and m2) :
http://www.aak-diagnostik.de/englisch/flyer/index.html
From Katrina: I requested IVIG treatment several years ago and received 3 infusions. The first caused the most severe headache of my life (a true 10 out of 10) and a rash on my shins. The second treatment was uneventful. The third treatment I didn’t finish. I experienced severe Raynaud’s (vasospasms) in all ten fingers and all ten toes, even into my palms and feet. I had never had a Raynaud’s episode like that before or since. Started having to put gloves on to get food out of the freezer and could experience a Raynaud’s episode if I caught a chill,even in a warm room. I also started sleeping 16-20 hours a day, with involuntary napping required daily for 2-4 hours at a time. Eventually got diagnosed with severe sleep apnea which was probably mild before IVIG. So, anyone interested in pursuing IVIG should weigh the potential pros and cons carefully. I cannot think of a single benefit in my case.
This is good to know Cort! My neuro is reccomending IVIG but the cons though…
Since this treatment is refused to be paid by most insurance companies, is there a medication (s) that can be used to treat the symptoms of autoimmune small fiber polyneuropathy? Are there people who also have cervical issues with this painful, debilitating disease that makes one feel like they have encephalopathy during flares?
If cost is an issue, IV and IM preparations of immunoglobulin can be obtained in Russia (and probably most ex-USSR countries like Belorussia, Ukraine or Kazakhstan) very cheaply. Although they are labeled as “prescription only” most pharmacies will sell them without a prescription. In Russia in particular, IgG immunoglobulins are available in a many pathogen-specific varieties as well as “normal” (i.e. broad spectrum). They are widely used, including for flu prophylaxis.
I realize this is a very old post. But I wanted to relate my own experience as a person who most likely falls into the aaSFPN category (along with POTS) and IVIG. I am a 62 year old woman who got sick with what looked like classic ME/CFS after an EBV infection in 1987 (I was 29 at the time). I was bedbound for many years. I was 100% disabled for decades. In 2014 I was diagnosed (a long story on how this came to be) with CVID — Common Variable Immune Deficiency. I did not have this prior to having my colon removed (IBS does not begin to describe the GI trouble I had). I began ICIG treatment in spring of 2014. Due to expense, I was only ever able to get sporadic treatments. Around 2017 I was enrolled in a Phase III study for 14 months — no break in treatment. IVIG (30 grams) every three weeks. The results were extraordinary. I began to work part time again in 2018. I no longer live in disabling pain. I would say I am 70% recovered. I need to be careful not to push beyond my limits (say, doing two days of long distance cycling without at least a day in between – usually two days). I am about to try to work full time. I have been working part time with relative ease. I still struggle to work AND take proper care of my home, get the grocery shopping and such done. I am single and thus have no help. I take a few other supplements (DHEA is one) to help with stamina. But I do believe that IVIG — given for an immune deficiency — which I most definitely did NOT HAVE prior to 2007 (when my colon was removed) has helped to resolve the fibromyalgia and crushing fatigue I had lived with for 30 years. I still carry a high EBV titer count — but this seems to be the ghost of the original infection. I realize this is all anecdotal — but after 30 years of illness, I was able to engage in activities I thought I would never do again. Cycling, hiking, (I have the ability to tolerate exercise now — it takes a while for me to build up my resilience but it is possible). Working again. It has to be the IVIG. I now am enrolled in a program in my state that allows me to buy into the Medicaid here — which I can then use as a secondary insurance — this covers the roughly $400 copay I have per infusion. I no longer miss infusions. Life is good. Hope someone sees this!
Shelli!
Thank you for sharing your story of hope!
After so many years sick it must feel incredible to be able to enjoy life again.
I have been sick for 21 years and am looking into IVIG. I hope it helps me too!
Thank you again for sharing.
Keep enjoying life! <3
Do you have to have the infusions indefinitely to maintain your improvements? I am starting my first treatment next week, and Dr. has left it very open ended. Probably because it’s not really known. Hoping to tolerate it well and slow down my illness if not put it entirely into remission.
Hey Shelli I was wondering how did you get ivig because I am desperate for this too, I struggle with small fiber neuropathy that cause me to barely walk and breath and its been 9 month into my acute illness it affected my breathing, swallowing, heart which is scary and it does not seem that I am getting help here in texas any advice?
We now have a randomised controlled trial of IVIg for POTS:
https://pubmed.ncbi.nlm.nih.gov/38311655/
PDF prepress version:
https://assets.researchsquare.com/files/rs-3500596/v1_covered_bbbeb097-56f0-4d70-9f1b-97f6fade5078.pdf?c=1707145659
Hello All,
When I read this I am struck by the
major condition of:
SMALL FIBRE NEROPATHY.
The way we know this condition best is from studying Diabetes.
We already know that
UNACCOMPANIED GLUCOSE
…un-escorted GLUCOSE is a TOXIN to both endothelial blood vessel cells,
and to the Nerve cells that line blood vessels as if they are lace. Think of the arm-gloves of
Stevie Nicks on…. *that Album.
GLUCOSE should be chaperoned by INSULIN.
INSULIN RESISTANCE is reported in CFS/ME blood analyses.
I believe that excessive blood glucose:
triggers gradual buildup of excessive blood INSULIN levels.
This, according to PhD Jesse Inchausp/e of France.
No one has really (says Mr. Ignorant, here) correlated the INSULIN RESISTANCE in CFS/ME with the INSULIN RESISTANCE as a major componant of DIABETES.
To put it another way, CFS/ME patients are proven to be INSULIN RESISTANT,
but they have not been THEN included as a subset of Diabetes… If I am wrong about this, then PLEASE enlighten ME first, and the rest of us.
Principally, in this message:
I am stressing on the fact that CFS and FIBRO patients seem to have small-fibre-neuropathy.
But these small fibres seem to only occur as the outside lining of blood vessels (I can’t speak for capillaries, or for arteries.) There is a known disease which describes
doubling….or more… profusion of the nerve fibres on the outside of blood vessels.
I am really going backward here, not very fresh on the subject, but it seems possible that a
CFS/ME or FIBRO patient
could be experiencing the body overreaction to surplus small fibres lining the outside surface of blood vessels.
What I CAN’T imagine: is having insulin resistance and that NOT contributing in a HUGE way to muscle cells, or to cognitive brain cells, or to Limbic brain cells:
NOT having enough fuel.
Nerve damage is not always permanent, but in small-fibre-neuropathy I think it is considered on the majority to be permanent.