

I can hardly believe it myself. My ME is in remission. Jen Brea
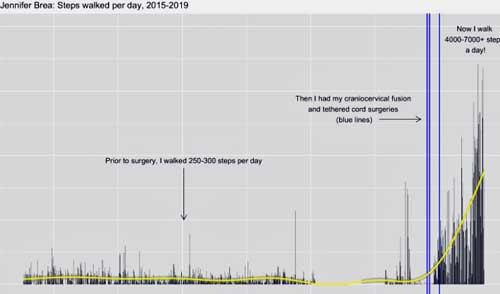
Steps per day – Jen Brea – before and after surgery (see blue line) (From https://forums.phoenixrising.me/threads/my-me-is-in-remission.76324/)
She ditched her wheelchair seven weeks ago. Her POTS disappeared in March. The sensitivities to sound, light, vibration and touch are gone. So is the muscle twitching, the air hunger, the restless legs, the brain fog, the short-term memory issues and the flu-like symptoms, For the first time in eight years, she’s walking for exercise and, well, for the thrill and joy of walking. She’s lifting light weights for 30-90 minutes and getting stronger, not weaker. She recently did an hour of water aerobics. She knew her PEM was gone immediately after the CCI/AAI surgery.
Her spine is still healing, but it seems it’s just a matter of time before Jen Brea’s ME/CFS is totally gone.
All it took was a series of spinal surgeries done over several weeks about six months ago. That sounds like a lot and it is – neither craniocervical instability (CCI) and tethered cord syndrome are easy to diagnose and are even more difficult to get treated – but her rapid recovery after 8 years of moderate to severe illness is amazing. She’s been in a wheelchair almost her entire time with this disease.
Just six months ago, following a thyroid surgery which exacerbated her then undiagnosed case of CCI, Jen Brea was arguably at her lowest point ever. Besides all her ME symptoms, she was having trouble breathing, had flaccid limbs, numb, painful and weak legs, and was experiencing difficulty speaking and thinking.
That all rather quickly disappeared.
Recovering / Recovery
We know Jen Brea and her husband’s story on an intimate level through Unrest. Jen may be the only person some people feel they know with ME/CFS. She doesn’t appear to have ME/CFS anymore, though, and in six months, she may be completely healthy.
We’re complex beings and even a remarkable story like hers can bring up a mix of emotions. Happiness that someone who has been so ill may no longer be suffering. Hope that it could happen to us. There’s a potential dark side as well which Jen Brea alludes to – the survivor’s guilt for her of getting better while others continue to suffer – and possibly a feeling of getting left behind by those who haven’t recovered.
The Recovery/Recovering Stories section of Health Rising often triggers differing emotions – some people love them, others hate them. It’s not hard to see how someone else’s recovery story could trigger some issues. The sick raise their heads to be counted again. Conversations, once vanquished, about the unfairness of it – a tunnel down which no cheese exists – show up again. The problem is not someone becoming well but the shadow that recovery casts on our current situation.
I’m luckily rather immune to that. After 40 years of ME/CFS, I can hardly remember the healthy Cort. He’s not a problem anymore. Besides, if I could pick one person to get well – one person who, if healthy, could advance our cause the most – it would undoubtedly be Jen Brea. Her new health – she says she will stay involved – is a gift not just to her but to all of us.
The story of remission makes it even more clear to me than ever that we must fight for research to better understand the mechanisms underlying all of our cases.
I will never forget the experiences that I have gone through over the last eight years of illness. With my improved health, I will continue to fight alongside each of you for equality, dignity and better care; to challenge stigma and advocate for research dollars and medical education. I will not give up. I am in this fight until every person living with ME, no matter the cause, has access to diagnosis and care. Jen Brea
The Craniocervical Instability Subset in ME/CFS – Just How Big is It (and How Big Do We Want it to Be?)
Jen Brea makes two people with severe, apparently classic cases of “ME/CFS” who have recovered or are recovering after being treated for craniocervical instability (and in Jen’s case, tethered cord syndrome). Two more people on PR, @mattie and @StarChild56 have recently had fusion surgeries to correct CCI. Another’s surgery is on tap and one was recently done.
Jeff just interviewed Mattie three months post surgery. Mattie, a web developer in the Netherlands, had a gradual onset of ME/CFS in 2010 and slowly declined over time. He didn’t consider himself a candidate for the surgery but was living near a center in Germany which could do the tests. To his surprise, he met the criteria. Three months post-surgery he’s nowhere near healthy, but he’s no longer mostly bedridden, POTS, dysautonomia, headaches and neck pain have disappeared, and he has more energy. The interview includes a particularly good discussion of the doctor and the decision to have the surgery. Jeff will interview Mattie again in a couple of months.
Find out more about Jeff’s story
Could Craniocervical Instability Be Causing ME/CFS, Fibromyalgia & POTS? Pt I – The Brainstem Series
The fact that 20 people on the Phoenix Rising Forums have been diagnosed with craniocervical instability/atlantoaxial instability (CCI/AAI) over the past 8 months or so is remarkable, and suggests that the condition may not be as uncommon as one might think.
- Check out the Tracking CCI/AAI thread on Phoenix RIsing.
Difficult Diagnosis and Treatment
There’s no doubt this is not the easy way out for ME/CFS. If I could choose a way to recover – which I obviously can’t – neurosurgery would be one of the last options on my list. I think I would rather swallow a toxic chemotherapy drug than have a neurosurgeon fuse my head to the top of my spinal column. That procedure sounds about as spine-tinglingly scary as anything I can imagine. (Brain surgery would probably be worse.) The fact that only four neurosurgeons in the world can be trusted to do this procedure doesn’t help.
Among the first thoughts I had upon learning of Jen’s recovery was that if this is what it takes – a rare diagnosis and neurosurgery – if that’s what it really takes to recover, I don’t know that that’s ever going to happen.
After some reflection, I don’t think it’s as bad as that. Jeff and Jen and two other people have found a way and a remarkable 20 people on Phoenix RIsing have gotten a diagnosis. While getting a diagnosis isn’t a piece of cake, it can and is being done. Be sure to check out Jeff’s recommendations on his website. Plus, other less invasive treatment options are available (see below).
Focus on the Spine
Jeff and Jen’s stories do bring a new focus to the spine and brainstem. Hip, on the Phoenix Rising Forums, pointed to five structural conditions which can cause brain stem or spinal cord compression – and ME/CFS-like symptoms:
- cervical spinal stenosis — spinal canal becomes too narrow, which can put pressure on the nerves
- syringomyelia — fluid-filled cyst in the spinal cord which compresses the spinal nerves
- Chiari malformation — where brain tissue is pushed into the spinal canal due to a skull which is too small
- tethered cord — where spinal cord is “stuck” to a structure within the spine such as scar tissue
- craniocervical instability — instability of head & neck bones compressing the brain stem or upper spinal cord.
Other spinal conditions that could cause or contribute to ME/CFS/FM/POTS include cerebral spinal fluid leaks and intracranial hypertension.
Even if you don’t have CCI/AAI, the search for it may help uncover other problems. One person on the Phoenix Rising forums reported that she didn’t have CCI but that the search for it turned up “severe stenosis, edema, compression fractures, and other issues causing my spinal cord to be affected” and that treatments for those conditions were helping.
Still, I’m hoping that: a) CCI/AAI is not a common diagnosis; or b) if it is, that non-surgical treatments can be as helpful as surgery. What I’m really hoping, though, is that Jeff and Jen’s stories are pointing to a problem area that can be helped with other means.
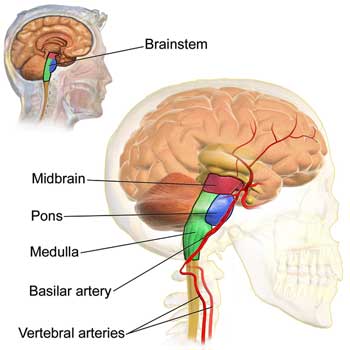
Focus on the Brainstem
Jen and Jeff’s experiences are shining a bright light on a potentially very important, and until recently, little explored area of the brain – the brainstem. Structural issues aren’t the only way to potentially tweak the brainstem in ME/CFS; inflammation, infection or autoimmunity would probably do quite nicely, and some evidence suggests at least one of these may be happening in ME/CFS. Each of these could trigger a different (and less invasive) treatment approach.
Van Elzakker pointed to four ways the brainstem may be involved in ME/CFS:
- via the dysregulation of immune signals traveling from the vagus nerve to the brain
- via activation of the many mast cells found in it
- via problems with its regulation of the autonomic nervous system
- via a stunting of the anti-inflammatory response.
See – The Brainstem, Vagus Nerve, Neuroinflammation and Chronic Fatigue Syndrome: The VanElzakker Way
Some evidence directly implicates the brainstem in ME/CFS. Reduced brainstem grey matter volume suggests that the neurons in the brainstem may have been damaged. The fact that the damage correlated with autonomic nervous system problems suggested brainstem problems could be affecting exercise, sleep, the gut and cognition. A communication breakdown from the brainstem nuclei to other nuclei in the brain suggested brainstem problems could even be contributing to the motor cortex, i.e. movement problems in ME/CFS. Barnden proposed problems in the brainstem could be inhibiting the flow of signals from the motor cortex in the brain to the muscles.
The Japanese have echoed that general idea. A 2003 study suggested that reduced motor cortex output was reducing muscle recruitment in ME/CFS and causing fatigue. Given the recent brainstem findings, though, stopping at the motor cortex would seem foolhardy. Given the extreme disability sometimes found in ME/CFS, it’s possible that two of the crucial brain organs involved in movement – the motor cortex and the brainstem – may have both taken a hit.
Studying the brainstem requires special techniques not usually used in brain imaging. Both VanElzakker and Barnden are employing those techniques as they continue their brainstem studies in ME/CFS.
HIP on the Phoenix Rising Forums suggested an intriguing pathogen connection. Enteroviruses (the first viruses associated with ME) produce enzymes called matrix metalloproteinases (MMPs) that destroy connective tissue proteins like collagen, elastin and gelatin. It’s possible that an enteroviral infection could be causing the ligament laxity issues in CCI.
Jeff and Jen’s Atypically Typical Recovery
The only things we really know about recovery is that: a) it’s not common; and b) it occurs in a variety of ways. When it occurs, it often occurs using nontraditional approaches found teetering on the skinny branches of the medical system. Just yesterday someone reported that getting treated for pyroluria – a condition many doctors don’t know about or believe in – made a huge difference.
I was recently diagnosed with Pyroluria. I had a urine count of 27.5 so I was severe. I am also copper zinc imbalanced. I am one of those rare people that the illness was shutting down physically and crippling me due to brain inflammation. I had constant vertigo, extreme light and sound sensitivity, sensory processing disorder problems that were so uncomfortable I would beg god to let me die. My body aches and couldn’t turn my head without severe symptoms. These are not symptoms that are easy to fake….. The saddest thing is how the healthcare system didn’t help at all. I was incapable of seeing, walking straight, or talking right some days but yea… not serious enough. I tried so hard to get help and they didn’t seem to care. So I was forced to an FMT; my last resort. Once diagnosed with severe pyroluria I started supplementation and had very quick results. I immediately had changed in functioning and energy. I can work now.
Finding an unusual treatment that works is fairly typical in people who recover. While there are certainly cases of gradual recoveries using supplements, pacing, and mind/body practices, many of the recovery stories involve unusual, out-of-the-box treatments.
Jeff and Jen Brea are leading examples. Not only is the CCI/AAI surgery they had unusual but they were unusual CCI/AAI patients as well. Both were classic ME patients with all that implies (post-exertional malaise (PEM), viral infections, MCAS, POTS, sensory sensitivities). Jen’s doctor told her he didn’t know how the surgery would go for her because he’d never had a patient like her. Whatever kind of CCI/AAI she had, it was different from what he’d seen before.
So it goes for many people who’ve recovered. Ken Anbender recovered from 26 years of hell using the Pridgen Protocol. After spending over $200K on more traditional treatments, mold avoidance did it for Joey. Valcyte did the trick for Kate and her 25 year struggle with ME/CFS. Sinus surgery proved the cure for Diane. The winner for one recent onset but severely ill patient was desmopressin – something that doesn’t work that well for most. It took a particularly astute practitioner to diagnose the heavy metal poisoning, that put one severely ill patient on the road to recovery.
Another remarkable thing is how sick some people can get and still recover. Jeff, Mike Dessin, and the heavy metal poisoning patient were more similar to Whitney Dafoe than your run of the mill (but still incredibly limited) ME/CFS patient – and yet they fully recovered. Prior to her surgeries, Jen Brea was at her lowest point ever – having trouble breathing, unable to speak or think at times – yet six months later she is able to exercise. When given the chance, the body can come back from an amazingly debilitated state.
For me, the recovery stories provide hope and are a sign not to give up, to stay curious, to keep reading and asking questions. Medicine, as Jen Brea noted in her recent blog, is ever-evolving. What was cloudy yesterday may become clear today. It wasn’t that long ago that CCI/AAI surgery wasn’t even considered for Ehlers Danlos Syndrome – it was the province solely of whiplash and trauma patients.
We should also remember how vitally important sharing our stories – both our ME/CFS stories and our recovery stories is. Jeff’s publication of his story may have saved Jen’s life. It’s now enabled 20 people to be diagnosed with CCI/AAI and three are undergoing surgeries. Please share your improvement or recovery story (and if Health Rising asks you to respond to a questionnaire on how you improved, please fill it out!)
Our goal has to be to assist the medical system in its evolution, to keep the hope alive, to keep sharing, to have the courage to keep knocking on closed doors, and eventually getting the light to shine through.
____________________________________________________________________________
Getting Diagnosed and Treated for CCI/AAI – a Review
Symptoms
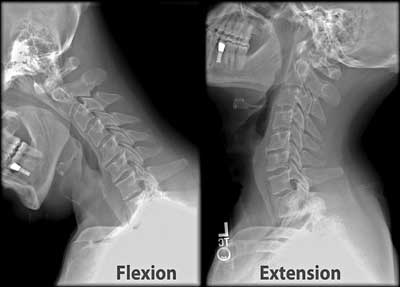
An X-ray of an neck being flexed back and forth to check for instability. (X-rays are not sufficient to test for this condition, however.)
The Zebra Network and other websites report three central symptoms of craniocervical instability (CCI):
- “Heavy” headaches (feeling like the head is too heavy for the neck) and a bobble-head feeling.
- Pressure headaches generated by things like yawning, laughing, crying, coughing, sneezing or straining.
- Symptoms of autonomic nervous system functioning problems such as tachycardia (rapid heartbeat, heat intolerance, problems standing (orthostatic intolerance), gut motility problems, thirst and chronic fatigue.
Other symptoms can include neck pain, central or mixed sleep apnea, facial pain or numbness, balance and coordination problems and vertigo, dizziness, fainting, vision issues, difficulty swallowing, choking, tinnitus, nausea, vomiting, paralysis, downward nystagmus (irregular eye movements).
Note that physical discomfort in head/neck area is not required! For the vast majority of their time ill neither Jeff or Jen experienced the kind of head or neck symptoms one would have thought would have accompanied CCI/AAI. Neither could have pointed to their head/neck area as a likely cause of their illness. Nor did Mattie – the third person with ME/CFS to have recently undergone CCI/AAI surgery. After reading Jeff’s account Mattie thought he didn’t have CCI/AAI – but got it checked out anyway – and found, to his surprise, that he did.
Diagnosis
Tip! – a physiatrist (pain doctor) reported that physiatrists are trained to look for CCI/AAI. It might be best to look for a reputable pain clinic in the area, call them up and ask them about it. They’re probably a lot easier to get a hold of than a neurosurgeon.
Both Jen and Jeff’s stories highlight the need for a really good diagnostician – someone who is plugged into the latest ME/CFS news. Jen has said she will tell her story, and Jeff was lucky enough to find Dr. Kaufman. His partner, Dr. Chedda, now regularly checks for CCI/AAI.
Quickie Diagnostics
Two methods can provide an indication that CCI/AAI might be present.
Cervical Traction: Jeff reported that a trained physical therapist who applies cervical traction is the gold standard for home diagnostic efforts. Dr. Bolognese told one potential patient on Phoenix Rising to “Try cervical traction with your local physical therapist. If you obtain dramatically positive results with the traction, then email me back about your feedback, and we will select you for a visit or a videoconference.”
Merck reported that symptom improvement during a procedure called Invasive Cervical Traction (ICT) where one’s head is pulled upward by a pulley system can help diagnose CCI/AAI.
Lacking those things, a doctor can simply pull the patient’s head up off the spine in the doctor’s office, and see if that helps! (Dr. Chedda reported that she routinely does this.)
Philadelphia or Aspen Vista Collar: Both Jeff and Jen were given valuable information when a Philadelphia Collar or an Aspen Vista collar helped their symptoms, at least for a time. The collars do not always improve symptoms, however.
Brain Scans
Brain scans provide the final determination.
On his Mechanicalbasis website, Jeff provides crucial advice for getting tested and fully diagnosed – including how to get your scans into the right hands. Most neurosurgeons aren’t trained to recognize craniocervical instability, and finding an imaging facility that does the right kind of scans can take time. Different neurosurgeons will employ different scans.
There are upright MRIs with flexion, extension, and rotational views, or supine CT scans with flexion, extension, and rotational views or 3Tesla supine MRI’s. (A patient of Dr. Kaufman’s reports that the extremely strong 3Tesla MRI’s may be the best and are more readily available. Check out the difference between the 3T and 1.5T machines).
Chiaribridges reported that “the ideal tests to diagnose CCI and AAI are an upright MRI with flexion and extension (bending one’s head forward and backward as far as one can) and a 3D CT with rotational views, respectively. Ventral brainstem compression is not always seen in traditional supine MR imaging but it’s usually very evident on dynamic upright imaging which has the patient flex and extend their neck. Upright scans are harder to find and are not necessary if good MRI machines are available.”
On Phoenix Rising, Jeff reported that the dynamic imaging should also check for Chiari Malformation (which can cause similar issues), craniocervical instability, and tethered cord syndrome (which Health Rising will cover later).
- Comorbid Diseases and ME/CFS/FM Mimics – check out the growing list here.
Treatment – Nonsurgical Procedures
Surgery was the only option for Jeff and Jen, but it’s not for everyone. Dr. Bolognese reported that a treatment plan for craniocervical instability typically begins with things like neck bracing, activity limitation, physical therapy (including isometrics, core strengthening and cardio), as well as pain management.
One person diagnosed with CCI reported on the Phoenix Rising forums that manual traction (having someone pull on one’s head while lying down) can help, and prescription drugs have resulted in major improvements. Some people with CCI also benefit from home neck traction devices. Sleeping in a bed with the feet elevated and the head down in the Trendelenburg position can help.
A procedure called AltasPROfilax, specialized chiropractic care and the Perrin technique is another possibility for those with neck issues.
Some people with ligament laxity have improved using the Cusack Protocol. Regenex is another procedure mentioned. In it, bone marrow concentrate (BMC) containing a stem cell fraction (same-day stem cell procedure) is injected directly into the lax ligaments.
Prolotherapy? – I don’t know if prolotherapy is an option for treating CCI/AAI, but it is used to treat ligament laxity which is found in CCI/AAI and a number of neck and spine issues. Prolotherapy involves injecting an irritating glucose/dextrose or other solution at painful ligament attachment sites to produce a mild inflammatory response which, hopefully, initiates a healing cascade which then increases the strength and elasticity of connective tissues. It’s been used to treat whiplash for years and has been used in EDS but is not well studied.
Treatment – Surgery
Surgery is considered the last option – a good thing, as Jeff lists only four neurosurgeons (3 in the U.S. and one in Europe) proficient in this kind of surgery. Wait times to get the surgery done can obviously be long. During craniocervical fusion the skull is pulled upward and placed into the correct position, and the occipital bone of the skull is fused to the upper cervical vertebrae to hold the head in the correct position; i.e. off of the brainstem. A halo or cervical brace is worn while the bones completely fuse together.
CCI/AII Resources
Health Rising’s ME/CFS/FM Spinal Series + Recovery Stories
- Could Craniocervical Instability Be Causing ME/CFS, Fibromyalgia & POTS? The Spinal Series – Pt. I
- Jennifer Brea’s Amazing ME/CFS Recovering Story: the Spinal Series – Pt. II
- Spinal Stenosis, Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia: The Spinal Series #2
- Recovery/Recovering Stories Section
Jeff’s Story and Website
- The MEchanical Basis of ME/CFS. – includes his story and resources on diagnosis and neurosurgeons
- An interview with Mattie – three months post CCI/AAI surgery
Jen Brea’s Story (Most recent to oldest)
- Health update #3: My ME is in remission
- Health update #2: My POTS is in remission (My POTS has been in remission for 21 consecutive days! — an outcome of my craniocervical fusion surgery. More on this and why I think we need to be looking at the brainstem.
- Do you have ICC-ME and other FAQs (The previous post somehow had some folks thinking I have hEDS and that I don’t have ME, even though all the previous posts have conveyed the opposite. I wrote this for all avoidance of doubt!)
- Are a subset of us members of a lost tribe? (On the possible connections between EDS and ME and the questions I wish researchers were asking.)
- Health update #1 (Feb 21) (Healing takes time)
- A new diagnosis to add to the list (I stopped breathing and was diagnosed with craniocervical instability)
CCI/ AAI Threads on the Phoenix Rising Forums
- Have you ruled out Chiari or Craniocervical Instability (CCI) as a cause of your CFS
- 20 patients now found positive for CCI / AAI, there must be many more…
- Tracking CCI / AAI MRI & Treatment outcomes
- Regenexx for craniocervical instability: my experience
- Update: CCI Surgery
- Pursuing CCI/AAI, have questions, former high jumper & figure skater
- Jeff anyone who have consulted with Dr Bolonesse … help confused!








I am so happy for Jen Brea and I hope that she extracts every ounce of joy out of her newfound health and second chance at life. You are right though Cort that it raises some difficult emotions. I am surprised by how angry I feel, not at Jen, but at the quirks of fate and geography that dictate whether we will receive help or no help at all. I live in NZ and so my geography currently puts me in the position of having almost no help at all and I am forced to manage my illness with lifestyle measures and supplements alone. Sometimes I’m winning, sometimes I definitely aren’t. I would dearly love to get my hands on Mestinon and my mind boggles at the testing regimes and treatments that some patients are offered in the US (as they rightly deserve). NZ is third world by comparison and I am so tired, not just from the illness, but from the complete absence of any support, medical or otherwise.
PS. High oxidative and nitrosative stress can also damage the brainstem.
Not even Mestinon, an old and safe drug which Jen, by the way, found that helped her. So sorry to hear that Deb. I really don’t know what to say…It must be hard, indeed, to read some of these blogs. 🙁 I wish you the best!
Thanks so much Cort. I’m sure that one day we will all have access to great medical care and the work of yourself and people like Jen sure does go a very long way to this end. I’m in awe of what both of you have achieved. I’m glad Jen is comparatively well and getting better all the time. She is an amazing and resourceful woman and she worked bloody hard and endured a lot to get her break. Is a powerful reminder not to give up and to push for help. Thank you.
This did not cure my daughter.
Hi R, did you mean that surgery to correct CCI/AAI did not cure your daughter of ME/CFS? If so, might I ask who performed her surgery?
It’s great that this worked for her, BUT the very fact ME/CFS has had clustered outbreaks in many places makes it evident that this is some kind of infection. (herpes 4 seems to be the current candidate)
That does not mean similar examples such as Brea’s are not real, but are the exception.
They (her’s & others) can distract us from the underlying cause of this devastating illness so many of us have.
This type of surgery is absolutely not an appropriate treatment for illnesses such as ME. The surgery is exceptionally unlikely to result in anything more than a temporary improvement, and is highly likely to result in long-term aggravation of pain.
Neurosurgeons advocating surgery of this nature are preying on ill people with ME who are desperate for cure.
If you have ME and are contemplating such surgery you should be extremely circumspect and examine the evidence with great care.
If you can’t access Mestinon, you might consider trying the nutritional supplement Huperzine A. It is a cholinesterase inhibitor like Mestinon, available over the counter. Not sure how available nutritional supplements are in NZ, but Huperzine A is well known in Chinese and Indian medicine. Unlike Mestinon, it only needs to be taken once or twice a day. Best of luck!
Huperzine A caused tummy issues with me, as did mestinon. It wasn’t my answer. Quite a few can’t tolerate it or it doesn’t help.
Would you share the Hyperzine product that’s working for you?
Parasym Plus is a supplement that I take. It contains Huperzine A (HupA), Thiamine (B1), L-Carnitine and A-GPC (a form of choline) and is available via Amazon. I’ve been taking it for over a year and it has been a miracle, not a cure, but I couldn’t live without it since it keeps many of my symptoms, especially the cognitive dysfunction (e.g., short term memory problems and brain fog, etc.) and many of my autonomic manifestations, including POTS, under control. I still suffer with fatigue and PEM but I can at least manage my symptoms better with this supplement. I take one pill in the morning and one in the early evening. A word of caution. Do NOT take any other acetylcholinesterase inhibitor, in any form, while taking this supplement since HupA is a VERY potent drug. Even though I have a super sensitive digestive system, and always have, I’ve had no adverse affects. It seems to bring balance back to the sympathetic and parasympathetic nervous systems. I also use Lipid Replacement Therapy using an organic sunflower lecithin powder. The common thread between the two is choline, the precursor to the neurotransmitter, acetylcholine, which appears to be low and/or impaired in people with ME CFS. Also…check out the website, Hormones Matters, and all the articles about Thiamine Deficiency. The symptoms are VERY similar to many of our ME CFS symptoms. Recently, after reading an article on the HM website titled, “Thiamine, Epigenetics, and the Tale of the Travelling Enzymes,” I added Thiamine (a bariatric formulation) to my vitamin and supplement regimen. Again, none of this has been a cure but with pacing, infection and stress avoidance, and staying within preset limits (total daily steps and anaerobic heart rate), I’m less sick and have an improved, albeit still limited, quality of life. Please note: You may need to reduce your dosage or cycle off it periodically if it becomes less effective.
I am glad for Jen Brea but hope it lasts. I absolutely feel she should not feel any guilt. Nor could I ever feel any envy. But I’m leery of these fixes. Jen I just really hope it works, and not only longterm, but for the rest of your life.
I believe I’ve had CCI for over 25 years which doctors have refused to image properly. I have had CFS symptoms several times a year lasting from 10 days to over 6 months. I have not come across a doctor in that time that either understands or knows about CFS so there has not been a diagnosis; usually just shrugged shoulders.
My symptoms start after I do too much work/exercise that includes my shoulders and neck. What has helped somewhat is daily valacyclovir. Each episode of CFS would start out with cold sores, sore throat, severe fatigue, sleep disruption, achy joints and muscles, etc. Since valacyclovir those symptoms are not near as severe. There are still the vagal sympathetic synptoms and the neck pain.
Haven’t we been through this before? Around 2000, a group of Fibro and CFS patients, including myself, were diagnose with Arnold Chiari Malformation. I and others had surgery, some at CINN in Chicago, but I saw E Neurosurgeons to confirm. The surgery did nothing for me.
I’m very happy for those who benefit from surgery – but a new diagnosis may just add another name to my long long list.
The USA funding is minimal and she quoted $5 p.a.
Has there been any research using Infra red light therapy , it is low cost, non invasive and the target areas are the Gut Microbiota, no medication is required. I am a research Scientist that have had one success, of treating a person who had been ill with ME/CFS , Fibromyalgia , Depression, and associated sleep without feeling refreshed, since 1990’s. After ten weeks of treating his gut microbiome, he has improved out of sight, and it is now a whole year and two months that he has not had any relapses. I have videos, and written testimonials, and Glen Miller aged in his Sixties can be interviewed in, Melbourne, Victoria, Australia.
Laurence Fang.
7/12/2020
I just bought an infrared light machine for my husbands arthritis. Could I use it for my chronic fatigue? If so, how.Thank you
I am incredibly happy for them, and it is a good reminder that good news can surprise us as well as the other sort.
I am absolutely thrilled to hear such wonderful news! Sometimes, hope shows up where you least expect it and we are reminded that all things are possible. Thank you, thank you, thank you.
I am in the same place as debs. in belgium. wrong country. and am even sobedridden I could not go to see a specialist or getting at a hospital. so I am desperate, said and angry to. glad for jen ofcourse. But I see no future for me anymore, getting rapidly worse and am alreaddy 99% bedridden. It all comes to late…
I hope not. I do think that if something like Ron Davis’s nanoneedle is validated or some other discovery that wakes up the medical is – it will spread to Belgium and New Zealand and just about everywhere.
The need to get the news out – to make sure that everyone benefits – is one reason we need strong advocacy networks everywhere now. This is yet another area where Jen Brea and ME action have made such a difference: they’ve provided a locus for people to rally around.
Oh Brigitte, I am so sorry. I send you love and every wish that you will get help soon. You deserve it so much more than me. Gentle hugs
Brigitte: how is your financial situation? Would it be possible for you to follow De Meirleirs regime for some symptom relief while you wait for the world to catch up? He is located in Brussels, and I have heard of occational home visits….
Thanks for sharing this Cort. I just want to put out there that as a physiatrist CCI is a diagnosis that we’re extensively trained in and we don’t miss. It’s not a difficult diagnosis when you’re training encompasses actually looking for this. I had the opportunity to work at a fairly renowned clinic for a brief period that works with people with ME/CFS. Unfortunately, I saw a number of diagnoses that were being missed and being labeled as ME/CFS – particularly traumatic brain injury – hence the opportunity to appropriately treat and for folks to heal was being overlooked. (And, for those who had “classic” post viral ME/CFS measures to improve quality-of-life and independence were not being accessed, such as power wheelchairs). I highly encourage folks to find physiatrist in their area if they have them. We have a very different lens in looking at chronic conditions vs internal medicine. A big difference, in pertinent to this article, is our training in CCI. It’s one of those you don’t want to miss this diagnosis that is “drilled” into our specialty training. Thanks again for this coverage of an important topic.
That is great to hear! I will put that in the blog 🙂
In wich country is it and what is physiatrist? is there one in belgium you know?
This is really interesting to know. A good physiatrist is amazing, but I’ve found, a little hard to find in the US. I think Europe has a stronger tradition of (and gives more value to)physiatry. I had an Austrian physiatrist, who would probably be over 100 by now, and she was amazing. Thanks for the comment.
I was told by a Woman last night to look into a condition called ‘Systemic Nickel Allergy Syndrome’ I was very surprised she said this to me, a Doctor a few years back told me I was Allergic to Nickle he never said anything to me about foods,
vitamins, minerals, medicines that contain Nickle…I was reacting very badly to belt buckles, wrist & neck chains, watches I would break out in severe itchy hives & itch until I would bleed. She said it can also cause countless symptoms, when I saw the
food list I could not believe the foods I reacted to already & it goes undiagnosed, one girl she is allergic to her braces in her mouth she has the illness she is also Allergic to stainless Steel products knives forks spoons pots pans etc.
Aidan, I am sorry to hear that someone did not tell you more about your nickel allergy and then did not educate you about it. Nickel is an every single food, pretty much. So, it’s a matter of reducing the amount of nickel. It is a rarer true allergy, but it is out there.This is another important point about ME/CFS. Truly is a diagnosis of exclusion. All things that are treatable, should be treated. All possibilities to heal should be pursued. I’m constantly disappointed in my colleagues in their inability to rule out and hunt down all possibilitiesand find something that could be treated and healed. It requires a keen eye, and the ability to think “outside the box“. The body/being truly does want to heal, and it’s only a matter of knowing how to support that … I can speak from very personal experience, having been erroneously diagnosed with another chronic “incurable” condition interstitial cystitis. I am pain free now because I found the right people, the right diagnosis, and the right “tools” to heal my body. It is from this experience that drove me on to, in very short, to become a Ayurvedic Naturopath and then medical doctor and work with people with the “incurable” .
I am happy for Jeff and Jan! It has also caused to wonder about my own possible CCI. I have had ME for almost 14 years but am not bed bound.
About 10 years ago I went to my Medical Internist with horrible neck pain, headaches and difficulty swallowing. I had a neck MRI (not with flexing) and a barium swallow with neck x-rays. I was told I had anterior osteophytes on my cervical spine along with arthritis. I wanted some sort of cervical traction because my head felt too heavy. Instead my doctor sent me to PT and it helped….for awhile. I could hold my head up again.
Now today, my neck hurts everyday especially at the base of my head. My difficulty swallowing remains unchanged but I was told if the osteophytes increased in size and I couldn’t swallow, I would have to have surgery.
I think I am going to pursue this neck thing, return to PT for my neck and maybe try a cervical collar. I have been trying to find someone who does cranial sacral massage but since I live in Hilo, I can’t find anyone who does it (at least correctly). I do ice my head and neck almost everyday. That plus certain types of medical marijuana have definitely helped. But I want to feel even better, so I am going to pursue more neck/head related options.
Also last year, I bought one of those bed bases that lets you elevate your head and/or feet. Surprisingly, I find I sleep best with my legs higher than my head. Go figure.
Love and support to all those suffering.
🙂
Interesting – we did a blog on how raising the head of ones bed can help with sleep. You never know! Good luck on your ongoing search.
https://www.healthrising.org/blog/2013/06/16/heads-up-are-you-missing-an-easy-way-to-improve-sleep-and-health/
Thanks Cort, but my legs are way above my head when I sleep, not the other way,
Hi Cort, my head is LOWER than my feet in my bed.
Whoops! Auto-correct said Jan instead of Jen!
Yes. I know. It shows how variable this all is – some people get helped with the opposite practice.
Amy, if you have the possibility in your area, look into Alexander Technique. You need an individual practitioner (“teacher” in Alexander Technique lingo) though there are a few things you can do at home on your own. The teachers go through a rigorous 3 year training (post BA). Alexander Technique is big in the UK and the US, and probably Canada. I don’t know about elsewhere in the world. They have a specific focus on the neck. I found them after PT worsened by double cervical herniated discs, a few years ago. It has helped a lot with my pain and function, though not a cure.
Amy, re raising your head or raising your feet for sleeping: I found raising my head (through one of those anti-reflux cushions) killed my neck! It also did a number on my lower back. My spine prefers as nearly completely horizontal as possible. Am going through a difficult bout of neck pain right now, and it seems to be because of the variable barometer. Haven’t figured out the solution to that one yet, though Alexander Technique helps somewhat.
Amy, not knowing truly more about your situation, you did not have the correct type of imaging. Traction is very dangerous in CCI. If you really think you have CCI, go to a if you really think you have cc hi, go to a neurosurgeon.
Christy Ceraso for CranioSacral in Hilo
I had to write about my feelings for an hour or so yesterday in order to help process – it was definitely a case of mixed emotions. I’m very happy for Jen and anyone who manages recovery or remission, I’m a tiny bit scared of losing her as one of our primary advocates. The fear I think is due to the lack of support we’ve had over the years and still do.
That said, this news has spurred me in a new direction in the chase for the cause of my ME/CFS. I had a very long onset, starting with loss of very high functioning memory (both muscle memory and factual memory) approx 18 years ago, with PEM and more severe cognitive issues showing up 4 years ago. I remember I pretty much overnight went from being able to remember and repeat physical movements after one or two demonstrations and having no trouble recalling them days or weeks later, to flat out forgetting them entirely within a few minutes. It was a bit devastating at the time, but I just carried on thinking my memorisation capabilities would return. I’m still waiting… 🙂
From the list of symptoms, I clearly don’t have CCI, so I’m going to search out regions of the brain that are implicated in muscle memory and other types of memory, then investigate any associated conditions that might shed some light and hopefully lead to a treatment.
“from being able to remember and repeat physical movements after one or two demonstrations and having no trouble recalling them days or weeks later, to flat out forgetting them entirely within a few minutes. It was a bit devastating at the time, but I just carried on thinking my memorisation capabilities would return. I’m still waiting… ?”
I had something similar. Every bad turn this disease gave me went hand in hand with randomly losing certain factual memories and certain abilities, both mental and motoric.
I believe two things are at work here:
1) ME causes all cells in the body to work differently compared to before and that includes brain cells. Brain cells in hibernation don’t process information at the same speed and strength. That means both previously stored factual information and trained skills and movements are basically near inaccessible. E.g. you’ve forgotten them or they are lost to you.
2) Your muscles and sense don’t operate anymore in the way they used before. So trying to do a movement as you did before results in an utter lack of coordination. Having your senses reporting different information about speed and position makes it worse. Compare it to be used to ride a car and all of a sudden having that car replaced by a truck for mining operations. Using the old trained skill won’t help you much and just confuses you.
I had to relearn doing thins as simple as how to stand up from a chair, opening a door and walk through it without bumping into it and how to “do corners” like walking around the corner of a table. I had at some point absolutely no clue how to do it. All of these seem to be simple movements but are in fact very complex composite movements that are very difficult to learn a robot to do it.
At the same time I learned that I still could do very simple basic movements well. It makes sense as those are computational far far less complex to do. So I learned “to go back to the basics” each time that happened.
Just like a kid has to take plenty of time to learn basic movements, so had I. I speed up the process by systematically decompose the complex movements in its very basic components and I separately trained these slowly. For example, walking around a table requires to be able to stand still and turn the outermost feet inward without lifting it or losing balance. So I had to learn that component by doing it slowly, observing how it went and how it felt and repeating it. Basically it’s do-it-yourself re-validation therapy like someone with brain injury would receive.
It’s a slow process but it was and still is to some extend an essential step in increasing my capabilities again after each crash. I use the same process for mental skills. It makes me “unbalanced” as there is so much to relearn and few usable time and energy. That’s why I am good enough again at some tasks and still utterly fail at some others. Having skills retrained makes them (much) more energy efficient too so it has part in a slow process of increasing the energy envelope too.
Hope the ideas may help you in your recovery.
Thankfully, Jen has made it clear that’s she will remain active and I imagine be more active than ever. I do hope that she will -as she improves – also enjoy and reacquaint herself fully with the benefits of better health and come back rejuvenated and ready to rock and roll 🙂
I congratulate Jennifer as well as Jeff for obtaining such stunning results, results that were not easily obtained and demanded an uneven fight against this debilitating disease.
As to “but her rapid recovery after 8 years of moderate to severe illness is amazing” I wonder:
did you not mean “moderate to severe ME”? Moderate to severe ME equals to “severe to devastatingly severe illness” IMO. People unaware of this may underestimate how debilitating this “moderate to severe illness” truly is.
I immediately also got a mixed feeling when reading about her recovery. I certainly believe she more then deserves it. And I do appreciate any new information about anyone recovering or improving a lot and how they got to this point. Both Jennifer and Jeff sure do provide a clear story and path to recovery for their case.
It’s just that I hoped for something making this disease easier to understand and treat rather then even more diverse and complex to comprehend.
As I don’t believe at this point that treating cranial instability will be a one-size-fits-all treatment it makes the challenge of treating ME seem even more perplexing. Even if treating cranial instability would treat a large percentage of ME patients, it’ll take plenty of time to train enough professionals to get such numbers of patients treated well.
Not knowing the problem at hand might be even more complex then anticipated doesn’t magically makes the problem easier to solve. So absolutely nothing is lost by knowing this new information, except of the hope for a quick, easy and simple solution for the masses of us. That kinda bites.
If anything their recovery may reinvigorate the medical field by showing how profound the impact of things like physics, gravity, interaction between organs and signalling throughout the body can be. It also may demonstrate how each individual change in the body can affect the entire body, just like an individual change in an ecosystem changes the entire ecosystem.
In the end, my dream is that all of the suffering caused by this disease and the large effort needed to combat it will increase understanding of this disease as a series of mechanisms, learn how to differentiate between symptoms that drive this disease and symptoms that are the result of fighting this disease and result in a sort of extensive diagnostics and treatment plan that gets to the root of our health issues.
That wouldn’t offer a single golden ticket to recovery for us all by having a single medical discovery. But it would mean that every single Jennifer, Jeff and the many others help shed light on a single aspect of this complex disease and help pull all of us bit by bit out of this swamp.
I felt uneasy writing moderate as well. I did it because that is how Jen described herself. At one point as I remember she reported that she could do a lot of mental activity but hardly any physical activity. I would put anyone who’s in a wheelchair as having a severe illness however. The scales are certainly off in ME/CFS.
Relative to others I have mild ME/CFS – but there’s nothing mild to me in something that precludes me from doing just about any exercise at all.
Sounds like I am like you Cort. I have ‘mild’ CFS, I work full time, but it’s tough. BUT, I cannot exercise in any meaningful way (although walking is generally OK).
Although things aren’t easy for me, I consider myself quite ‘lucky’ (so to speak) in CFS terms, knowing how many sufferers are sadly much worse than me.
Dear Cort
Thank you so much for this article, and care you have taken. Being able to write an article that reflects both the happiness for Jen and being pleased for any of us who find a way back whilst recognising there are other complex emotional responses going on is an honest thing to do.
You write so well here. Thank you.
Also in terms of severe, moderate, mild these are relative terms. All of us know that any level of ME/CFS robs us all of so much of what we would want for our lives, this is the one place we don’t have to explain that.
It is very upsetting to me that what has happened to Jennifer Brea is called a recovery or even a remisssion of ME/CFS. On the contrary. This is not an example of remission or a recovery from ME/CFS. This was a misdiagnosis plain and simple.
Let’s not add to the confusion that this high publicity case is going to bring to us. We have had to deal with mountains of misinformation over the past 30 years, with a long line of false hopes, quack treatments and cures. The fact remains, that while there are things we can do to make us feel better, ME/CFS remains a disease whose cause and cure is still unknown. Accepting our current status through a critical analysis of all claims to the contrary is the only way we can move ahead.
I am happy that Ms. Brea health is vastly improved and perhaps even cured of her malady, but she never did have our thing,
“but she never did have our thing”
Maybe, maybe not. Our disease is very diverse. We do not know what exactly causes it nor what sustains it. Saying that a viral onset causes this disease it too short of an explanation. Many people have viral infections but never develop our disease.
As long as we don’t know what causes and sustains our disease we can’t say she never had our disease.
Let’s go back to Naviaux’s research and Ron Davis comments on it. They believe our cells go into a sort of hibernation, Dauer after an initial onset of the disease and “try and wait the danger out”. Ron Davis and to some extent Naviaux believes that in many cases this danger is long gone and hence the hibernation is wrong and should be reset.
I doubt so. Many of the symptoms I experience seem to point to something the body is trying to resolve. When I try to support the body in resolving the problem I believe to perceive I often get a modest amount of improvement. Over several years that improved my abilities and life quality from near none to a lot better but still limited.
So what if our bodies were not in hibernation but rather in something I would call “pro-active hibernation”?
Hibernation itself is a damaging process if the patient isn’t doing a winter sleep like a squirrel. Trying to move, work, think, speak while your body is in hibernation causes plenty of damage, metabolic waste, inflammation…
As such, hibernation is a very wasteful process. You can’t for example just “hunker down or hibernate” if you’ve got a nasty gut bacterial overgrowth. That’ll kill you within days. The gut and it’s immune system cannot hibernate it’s defenses. It !must! try and activate the gut’s defenses to the optimal extend in order to even have a change for the body to “wait out the danger”.
The same happens for example when the blood flow to the brain is impaired by inflammation blocking good brain liquid drainage. The body !must! try and summon all means to restore liquid balance in the brain, even if these have devastating side effects like providing so few blood pressure that standing up from a chair can be enough to faint and fall down. Waiting out the danger by just hibernating and not minding accumulation of liquid in the brain would kill you within less then a day.
So maybe at the core of ME is “pro-active hibernation” with the body waiting out a problem it can’t resolve all by itself but very actively trying to provide, restore, improve and replace vital affected functions just to allow us to survive long term and hopefully even do so with very few permanent damage.
Finding one or more such core problems necessitating “pro-active hibernation” and solving it could in such cases yield near full recovery with very few permanent damage left. Jennifer’s case may be a good example of this hypothetical disease mechanism.
Dejuergen, if in theory Jen and Jeff’s CCI was caused by inflammation triggered by an virus why would treating the CCI heal all symptoms, surely some illness would still be remaining? Thanks
Sorry Dejeurgen, reading your reply again my question isn’t relevant to your theory, so please ignore. Thanks.
I think the question of just what exactly is ME/CFS is going to come up more and more. Certainly her CCI/AAI diagnosis is now the correct one but its interesting that neither her nor Jeff fit a typical CCI/AAI diagnosis either. They were different from the typical CCI/AAI patients.
It makes me wonder if their CCI/AAI is the result of the same infectious, autoimmune or inflammatory process that undergirds ME/CFS – it’s just showing up in this particular manner. The addition of EDS – in Jen’s case – restricted to the ligaments involved – and MCAS adds more layers that folds her into a huge assemblage of ME/CFS/FM/POTS/EDS/MCAS patients. It’s going to be interesting figuring this all out!
My daughter’s ligaments peeled off like paper. This is most likely from tryptase which acts like a meat tenderizer. She can bend her hand flat on her arm. Yet she is 8 of 9 on Beighton and so am I. I guess what concerns me about this is the pursuit of these diagnoses if you get one (I didn’t and my daughter has 2.. we have yet to pursue stenosis in veins in brain because we completely crashed from all this). My daughter is still mentally recovering from the CCI and suboccipital craniectomy. She will not pursue the tethered cord surgery because of that. It can be grueling and I was exposed to a lot of medical trauma during our three plus year investigation and not from the super specialists but from all the gate keepers, all the ruling out docs and their people. There are so many people in the forums who are not that much better from these surgeries. Just talk to others of us. The title is triggering and I am sure it is for people like me who were broken by the process and people who did not find relief and people fearing they cannot manage this physically, emotionally and financially. It is not a cure for everyone and I am not sure what was cured here besides the targeted outcomes. The rest is speculation. BTW, there were several miraculous recoveries from brain stenting as well. Also from SCIG and IVIG when autoimmunity involved. We worked with the best in the field.
I’m so happy for Jen and excited to see where she lands. Thanks Cort, for reporting on this and other stories of recovery. Although it’s painful to take in, it’s important for patients to hear and read about patients, like Jen and like me, who have recovered in different ways. Thank you for using these stories to educate and to keep hope afloat. June 1st will mark one year since my full recovery. From 2012 to 2015 I used a Lyme and heavy metal treatment program. I went from 40% functioning to 60%. Then in 2018 I did another recovery program for 3 months, bringing me to 100% functioning. I am still amazed each morning when I wake up symptom free, and I marvel at how much and what I am capable of doing with only normal healthy responses. My days are now filled with thoughts about life, not illness and symptoms. There is a huge emotional adjustment that comes with recovery, especially after decades of illness, but for me that journey is a beautiful unfolding to becoming my new self.
Recovery is possible. Best to you all.
Cort, I don’t think Jennifer was ever an EDS patient. She speculated and conjectured on Medium that she might fit the mold of EDS, but there is disagreement within that community (join and search ‘hypermobility’ through the backlog discussion on the Cusack protocol group) over what constitutes an EDS diagnosis and what does a hypermobility spectrum disorder.
Jennifer Brea I do not believe was ever diagnosed with EDS. She had conjectured, I believe, that she had a hypermobility spectrum disorder as a result of her CCI.
The difference is important. It means we get to see people like Jennifer Brea as being new or hybrid types in the context of both CCI surgery and future treatment. It means we get to debate whether she really was an ME patient, whether she purely and only was an ME patient, or whether she was ME + HSD. However, and I state again, she was not an HEDS patient.
From someone on the Cusack protocol FB group: Hypermobility disorder is diagnosed when the symptoms are primarily joint related. Ehlers Danlos has that plus a bunch of other issues—GI issues, stretchy skin, thin skin, easy bruising, abnormal scarring, prolapse, blue sclera, etc, plus all the comorbidities (POTS, MCAS, migraines, etc). Basically the criteria states if there’s only x amount of these symptoms it’s hypermobility. If there’s x amount more symptoms it’s eds. hEDS and hypermobility were often interchangeable until the recent criteria establishment.
Cort, your question is a very good one about is CCI an autoimmune consequence. Rheumatoid arthritis is a main cause of CCI. Hence why it’s one of those you don’t want to miss complications of rheumatoid arthritis, or don’t want to miss for any reason.
@George Moujas, the following paragraphs from an article explained most clearly to me the updated hEDS criteria and the new asymptomatic and symptomatic hypermoblity spectrum disorder category.
““Many people do not fully meet the new diagnostic criteria for hEDS but their hypermobility still causes problems for them. They may experience pain and dislocations, have a poor sense of where their joints are without looking, be prone to injury, have curvature of the spine, and degenerative joint and bone disease. These people may also have many of the non-musculoskeletal disorders associated with hEDS, but they do not quite ‘qualify’ for hEDS. After other possible conditions are excluded, a diagnosis of generalised hypermobility spectrum disorder may be made here.
Joint hypermobility with its possible complications is now classified using the idea of a spectrum. At one end is simple hypermobility which causes no symptoms, is not a disease and is a trait, like height. (My words – this is technically called asymptomatic localised or generalised hypermoblity) At the other end of our spectrum is hEDS, and in between falls a range of hypermobility-related conditions called hypermobility spectrum disorders (HSD) (my words these are symptomatic HSD)
HSD are likely to be common. Someone with HSD can be just as symptomatic, more so even, than someone with hEDS. Management advice for both hEDS and HSD is the same.”
I agree, misdiagnosis big time.
ME is buried more.
This is sad situation for those who are sick with the Real ME, Post Viral Enterovirus, Myalgic Encephalomyelitis is Atypical Poliomyelitis.
Ask the doctors in UK who have stayed true to what ME is.
Dr. Nigel Speight, is one .
Sheeze wish Jen Brea would stop messing with ME.
She even changed the color of Royal Blue to Red , Red is HIV
Carol
I know this is how ME started but its been decades and we’re no further on the atypical poliomyelitis front. How about tho an enteroviral attack that weakened those ligaments? Hip alluded to that possibility. Or an enteroviral attack which sparked an immune response which attacked those ligaments? Could Jen and Jeff – and the 20 people on Phoenix Rising – who have tested positive for CCI/AAI be the ME/CFS wing of CCI/AAI?
It could be argued there has been insufficient research to build on Ramsey and Dowsett’s hypothesis of ME being atypical polymyelitis.
Jane Colby of UK ME children’s charity, Tymes Trust tweeted just the other day the UK MRC some years ago dismissed her proposal to build on Dr Betty Dowsett’s work (Bryon Hyde’s too) and that the infecting viruses in ME could be identified, given the will There was no will and they didn’t want to know.
Colby said enteroviruses can be cultured from stools at beginning of infection as was done in polio. Colby said they could find the suspected neurotropic viruses implicated in ME by this tried and tested method if samples were taken early in the illness but it’s no longer done. Later on it’s harder to find them as they hide away in tissues eg brain.
Re Jen and Jeff’s CCI surgery, if in theory their CCI was caused by inflammation triggered by an enterovirus that caused Classic ME in others, why would treating the CCI heal all symptoms, surely some illness would still be remaining?
* I should note I am not sure Ramsey himself described ME as an atypical poliomyelitis (believe Dowsett did and Hyde definitely did), perhaps someone if reading this can confirm, but he did call it was an illness triggered by a virus. He did also say the Royal Free outbreak he documented as he was a physician there when it happened seemed to resemble previous documented atypical polymyelitsis outbreaks. He thought probably various viruses were responsible. Not sure whether he meant various Enteroviruses which have an affinity for the brain or more than one type of virus. Again happy for someone to elaborate if they know. Thanks.
@Kim
“why would treating the CCI heal all symptoms, surely some illness would still be remaining?”
Maybe the comments I made on https://www.healthrising.org/blog/2019/05/29/spinal-stenosis-chronic-fatigue-fibromyalgia/#comment-874284 can answer your question. It’s the first comment of dejurgen with 6 replies of myself to it to break it up in smaller pieces.
In short: spinal stenosis can potentially (help) disrupt blood and oxygen flow to the brain, cause inflammation of the main spinal nerves leading to a “rigid posture” and tense muscles wasting energy and more IMO.
It could be *part* of ME and for some a dominant part. If one can tackle a dominant ongoing “driver” of the disease one may have sufficient “self healing” left IMO.
Dean, I couldn’t agree with you more. This is one of the problems with ME/CFS is that it is a truly a diagnosis of exclusion. I have witnessed first hand that even so-called experts miss other diagnoses and then “diagnose” someone with ME/CFS. There’s so much education that is needed on so many different fronts.
I can understand the objection, but I wouldn’t call Jen Brea case a misdiagnosis. I immediately recognized her CFS the first time I saw her by the way she sits. And she had suffered from PEM which most of us CFS patients consider a hallmark symptom. It is more likely that her recovery is a coincidence rather than her diagnosis having been wrong.
Agreed. She didn’t have ME and i found her film attention seeking.
also people like her with plenty of money can access all treatment s.
The top docs are only available to the rich
Im amazed people here cannot see that, the majority suffer and the rich can see any doctor
I’m so happy to hear Jen is improving so quickly and doing so well!! What an unbelievable relief that must be.
I appreciated your your emphasis on the importance of staying curious, given the wide variety of ways out of illness that some people are finding.
And I also wanted to express how much I love how you write, Cort – with this example being particularly resonant (and “delightful”):
“When (recovery/remission) occurs, it often occurs using nontraditional approaches found teetering on the skinny branches of the medical system”
It is very frustrating…even devastating…when people outside our community do not accept ME/CFS is a real illness. I am increasingly finding it just as frustrating…even maddening…when people inside our community refuse to accept that people DO recover from ME/CFS. What is it that makes people not want to believe recovery is possible? Maybe not probable but at least possible. Claiming those who recover never had the illness in the first place or were misdiagnosed seems a popular response for some. We are becoming more and more militant with those outside our community who do not accept the validity of ME/CFS. It is time we become just as militant with those inside our community who refuse to accept the validity of recovery. Let’s have respect for those who have suffered and not discredit them or what they experienced when they recover. Let’s instead spread realistic hope that there are answers, varied as they are, to our collective suffering.
Well said, Michele Brown. It is clear that there is more than one single cause of ME/CFS that leads to the symptoms that we suffer. I didn’t think it would be long before some people proclaimed that Jenn had never had it in the first place, even though she was satisfied all the relevant criteria. Dr Myhill describes ME/CFS as a collection of symptoms rather than a diagnosis. It is clear that there is no single cause and we need to learn whatever we can from individual cases that may be of help to various subsets of patients, whose lives have been blighted by this dreadful illness.
Nicely said.
Angela, I agree with Cort, Nicely said! I think it’s a shame that folks with ME/CFS have been convinced that there is no cure or there’s no hope. I don’t know if you saw my post above about having an “incurable” condition called interstitial cystitis. It was a long road, but I am cured. That road is what took me to being trained as an Ayurvedic Naturopath, medical doctor, and researcher. What is very different about the Ayurvedic training and Western Medical Doctor, is as you alluded to calling a symptom or collection of symptoms a definitive disease. Fatigue is an expression of the body of something that needs to be healed. Not a destiny. The other big distinguishment between the two paradigms is in Western medicine people identify with their “disease.” They are their “disease.” I like bringing these two worlds together because as a medical doctor I have the tools to hunt down every possible thing that could be contributing to fatigue. As an Ayurvedic physician I can help people unhook their identities from their suffering and heal. Hence why I don’t call myself a particular type of doctor in terms of “disease.” I just consider myself a facilitator of healing. It amounts to success for everyone that I have worked with.
Is it necessary to have headaches or neck pain to possibly have CCI or AAI?
Neither are required. That’s one of the startling things about this condition. Even though its a spinal condition you don’t need to have either I don’t believe.
Cort, there is a profile of symptoms that our surgeon requires in addition to radiographic confirmation for CCI and tethered cord.
This surgery doesn’t always work.
https://www.reddit.com/r/ehlersdanlos/comments/7oro4c/rip_nina_parsons/
This was a friend of mine and it was horrible for her. At least now, she is out of her pain.
Issie
https://www.healthrising.org/forums/threads/how-bad-can-ehlors-danlos-syndrome-get-really-really-bad.2205/
Another post about Nina
So glad some are helped, but it’s not something to jump into without lots of research.
I have issues and stenosis, but my spine doc doesn’t feel surgery is best option for me. Lots of bracing and proper alignment with body posture very necessary. EDS is a difficult and painful thing.
I remember her horrific case now. It was really hard to read…
Apparently she had the surgery here – and then went to Dr. Bolonesse (sic) in Europe for followup surgeries which failed.
https://www.facebook.com/MegsEDS.MedicalJourney/posts/it-is-with-great-sadness-to-share-this-this-hits-way-too-close-to-home-this-is-n/2302315926661395/
The first surgery was done by the doc in NY and they tried to repair it in UK afterwards, according to one of her relatives email to me. They did several surgeries trying to fix it and get her out of pain. It was not tolerable and she was in a real bad way before she passed.
Exactly Issue. The surgery with a well respected neurosurgeon who does many of these surgeries helped with pain and some symptoms but did not help with CFS-ME. One liter of saline x5 week dripped slowly at night took away flu like symptoms.
Sorry, Issie, not Issue. 🙂 And I am talking about my daughter who improved from CCI surgery but it did not cure her. EDS type 3 is one presentation of MCAD and my daughter has Hereditary Alpha Tryptasemia (as per NIH) and MCAS as per qualifying for activation by strictest diagnostic criteria. The SYNDROME of HATS (or MCAS) is (1) MCAD (2) EDS type 3 (3) POTS or OI. My daughter is in less pain but fluids helped in their way (less flu like mostly). She has a tethered cord but that surgery does not cure CFSME either. So many people have had CCI and tethered cord surgeries and are not cured. We will trial SCIG soon. Our doctor has a high success rate with this for people with our profile which includes MCAD, POTS_OI and EDS type 3 with autoimmune profile I’d be happy feeling better at this point.
This is why I’m curious if Jen’s MCAS or mast cell activation came on as a result of environmental trigger (mold) or has a genetic origin. In your daughter’s case it would make sense that having HATS the surgery wouldn’t cure anything. In fact, the tryptase from the mast cells will likely continue to degrade the collagen, to my understanding, so such a surgery would only be a temporary band-aid for *some* symptoms, not all. Most of us with MCAS don’t have HAT, so your daughter’s case is unique. This surgery is extreme and I hesitate to see it as a “cure” for most of us.
Dear Cort
Congratulations and thank you for your work !!!!
Please, I would sugest you to read the book “Accessing the Healing Power of the Vagus Nerve by Stanley Rosenberg.
Also … pay attention to the “Polyvagal Theory” of Sthephen Porges
I am with Fibromyalgia and I am reading the book above … have not finised yet It looks promissing ….!!!!
Raquel from Brazil …
Sounds like a case of misdiagnosis to me! Her symptoms caused by the brain stem compression & tethered spinal cord were just very similar to the symptoms of ME/CFS, she has surgery to correct the spinal & vertebrae/brain stem deformity & all the symptoms have gone!! I was always curious over her “moderate/severe” ME/CFS ?? She was traveling all around the world giving talks & lectures, going out for meals, consecutive days, & always looked vibrant & well, with an incredible upright strong posture, obviously no brain fog or PEM etc etc was puzzling to me? I know she was using a wchair but that was because it kept her HR down from the POTS, not because her legs were so weak & wasted that she could no longer walk!
Will be interesting to hear what Ron Davis, Don Staines, Naviaux & others think of this Recovery from ME/CFS due to corrective surgery alone!
I think there’s more to it in Jeff and Jen’s case. Both were after all atypical CCI/AAI patients. CCI/AAI after all, can be caused by a number of factors – one of which apparently, is an ME/CFS-like illness. My grand hypothesis is that whatever caused their CCI/AAI is at work in other ME/CFS patients but is manifesting differently….Hopefully we will know at some point.
I agree, misdiagnosis big time.
ME is buried more.
This is sad situation for those who are sick with the Real ME, Post Viral Enterovirus, Myalgic Encephalomyelitis is Atypical Poliomyelitis.
Ask the doctors in UK who have stayed true to what ME is.
Dr. Nigel Speight, is one .
Sheeze wish Jen Brea would stop messing with ME.
She even changed the color of Royal Blue to Red , Red is HIV
Carol
Way to go Jennifer! I can sympathize from bed with your suffering, but can only be amazed at your courage to undergo such surgeries. I can only hope that your energy and health remain and your charisma remains with the cause. That being said it is my hope that you can put your forces behind the search for a biological marker. As Dr. Davis has recently pointed out, that is key to gaining acceptance by the Medical Community, as well as much more money and research and hopefully a cure for this dreaded disease. Be well!
This did not help my daughter’s CFS-ME. It helped with pain and some symptoms. She saw a world renown surgeon and we are very happy with the surgery. But better not cured.
If it looks like a duck, swims like a duck, and quacks like a duck, then it probably is a duck and most likely not MECFS
Yep!??
Cort, A lot of us are going to have these presentations or one of them or none of them because the SYNDROME presentation of Hereditary Alpha Tryptasemia (a mast cell disorder) and the SYNDROME of MCAS is: Hereditary alpha tryptasemia syndrome is a condition characterized by high blood tryptase levels, and by several symptoms associated with multiple organ systems. These symptoms may include allergic-like symptoms (skin itching, flushing, hives, or anaphylaxis); gastrointestinal symptoms such as bloating, abdominal pain, diarrhea and/or constipation (often diagnosed as irritable bowel syndrome), heartburn, reflux, and difficulty swallowing; connective tissue symptoms such as hypermobile joints and scoliosis (often diagnosed as Ehlers-Danlos syndrome, hypermobile type); heart symptoms such as a racing or pounding heartbeat or blood pressure swings sometimes with fainting (frequently diagnosed as postural orthostatic tachycardia syndrome (POTS); as well as behavioral problems.[1][2] https://rarediseases.info.nih.gov/diseases/13193/hereditary-alpha-tryptasemia-syndrome But like I’ve shared multiple times in comments, my daughter had CCI and mild chiari and tethered cord. We stopped before looking deeply (pardon the pun) into venous stenosis in brain. I have a mild chiari that is not obstructing flow but what happens when I have inflammation? Maybe it does then. One of these docs talked to me about people like us having angry or unhappy brains and he can do procedure on someone and they have major improvement and on another and no major improvement. Many of us have the syndrome. But people should have support and pace through these studies and surgeries. I cannot see not addressing symptomatic radiographic presentations and the good doctors know what to look for symptomatically and radiographically. People get defensive because we hear these stories and there is never a cure all, plus these things involve a lot of energy and risk emotionally on so many levels including continued exposure to the medical community. We could not avoid the unsafe people during this process that took us at least 3 years and only one surgery accomplished. I’m going to try to walk away from this topic now. It triggers me (pardon another pun) just like the mold topic does. I am trying to get the sympathetic dominance under control a bit here. Going by Jen’s movie, this make sense for her. I thought about this during the movie. The symptoms matched. I think the avoidance aspect helped a bit with inflammation which will make symptoms exacerbate (and I can see this with vascular stenosis as well.. nothing like inflammation to make a brain more unhappy and even angry).
It’s interesting to me to look at the mast cell angle. Mast cells are the “master cells” of our immune system and can recruit the other immune cells into action. Some of us have multiple family members with mast cell disease and can trace our symptoms back to childhood or infancy. I was born sick (MMAS), my brother was born sick (mastocytosis) and my son was born sick (MCAS). So this makes me wonder if Jeff or Jen showed signs of MCD from the beginning.
Jen has said she believes that mold exposure in Beijing may have triggered her MCAS which may have caused collagen degradation which may have led to the CCI… the CCI can also trigger mast cells and immune dysregulation as well as POTS, hEDS, etc.
Whether or not she had “true ME/CFS” is up for debate, but the fact is, her and Jeff’s cases could be the catalyst we need for a new direction for research into the complexities of all of these debilitating yet seemingly intricately connected conditions.
No – mast cells are not the ‘master cells’ of the immune system – I think you mean the inate immune system.
If you can’t access Mestinon, you might consider trying the nutritional supplement Huperzine A. It is a cholinesterase inhibitor like Mestinon, available over the counter. Not sure how available nutritional supplements are in NZ, but Huperzine A is well known in Chinese and Indian medicine. Unlike Mestinon, it only needs to be taken once or twice a day. Best of luck!
Didn’t she had thyroid cancer and removed her thyroid? This also could explain all her symptoms and maybe her recovery. But i am very happy for her 🙂
I wonder if anyone looked at the thyroid tissue for viruses. I had 4 episodes of viral thyroiditis before I had it removed.
Hi! My thyroidectomy has no impact on my ME symptoms, for better or for worse. It did worsen my instability, which is how I got diagnosed and treated.
Slightly off topic, but just to let others know that diphenhydramine as per Dr Younger has made a huge difference to my cfs. Not a cure, but much improvement in brain fog and fatigue & recovery times from over exertion. Looking forward to hearing the results of his study and of the herbal study.
Keep up the great work Cort!
Hi Ruth
One of the key side effects, apparently, of diphenhydramine is sleepiness. How does that line up with improving fatigue?
Hi matthias,
I take it at night… Help me fall asleep and most of the time sleep through the night .
Hi Matthias, this is not something i have experienced.
My suspicion is that it’s such a small dose (at 10mg twice per day – am and pm) that any sleepiness is negligible. At larger doses this may be an issue for sure. But it works in the body differently at low doses (aka to calm microglia and reduce brain inflammation rather than suppress coughing).
I found LND problematic but much prefer the dextromethorphan 🙂
Indeed, Jen Brea’s recovery is wonderful news. I also agree that spinal fusion, especially such a highly specialized procedure as craniocervical fusion, would not be my first pick for treatment. Unless, of course, it works!
Now that I am walking down this pathway myself, I’m experiencing some very contrary feelings, as you discuss. I learned about 2 months ago that Dr. Bolognese read my cervical MRI (standard supine is all he needs, unlike some others) as “possible CCI”, and have since begun the physical therapy routine that he uses as part of diagnosing whether the MRI findings are clinically significant. The encouraging news from Jeff and Jen (and now, hints of such from @mattie and @StarChild56) make the prospect of this being the solution all the more real.
On the one hand, how wonderful to have possibly found a cure after 26 years of illness! But the other hand is less delightful. I’ve seen many spinal fusions in my work (though not of this type) and I know recovery from these operations is no walk in the park. The larger bugbear for me, however, is the issue of money. My insurance is through the Healthcare Marketplace (ACA), and I’m very grateful to have it, as I was uninsurable prior to the ACA, being self-employed with pre-existing conditions. However, these policies are limited to in-network providers and facilities. My insurance will not cover this operation, which is estimated to cost approximately $150,000. This is such an obstacle that it almost makes me wish I’d never heard of CCI! I have insurance, but it is in-network only: the surgeons who perform this operation are not in-network for my insurance.
The saying goes, “Where there’s a will there’s a way,” right? With that in mind, I’ll continue the protocol to find out of CCI is likely to be my way out of illness.
Good luck Vlynx with the protocol and I hope you will continue to share how it goes.
The money issue raises it’s head – no surprise there really. I have the same issue actually – AFA will only pay for local providers.
I wonder if a move is in store? Is that possible?
So so happy for her! I’m pretty sure my ME has a biomechanical cause. I’ve had neck issues for many years, but can’t convince doctors to investigate. I benefit enormously from neck traction-like interventions like the neck hammock. Just wanted to say that the Perrin technique, mentioned above, plus other osteopathic techniques, did nothing to me. A huge waste of money.
nice article; good perspective in the article and comments on ‘cures’, ‘remedies’, ‘recoveries’ – message of hope – keep trying, everyone!
Jeff just interviewed someone who recently had the surgery.
Mattie, a web developer in the Netherlands, had a gradual onset, of ME/CFS in 2010 and slowly declined over time. His activity level at the time of the surgery was 5/100. He didn’t consider himself a candidate for the surgery but was living near a center in Germany which could do the tests. To his surprise he met the criteria. Three months post-surgery he’s nowhere near healthy but he is no longer mostly bedridden, his POTS, dysautonomia, headaches and neck pain have disappeared and he has more energy. The interview includes a particular good discussion of the doctor and the decision to have the surgery. Jeff will interview Mattie again in a couple of months.
Check it out here: https://www.mechanicalbasis.org/interviews.html
Jen’s story beginning with thyroid cancer reminds me of this story told on the TV show “Northern Exposure” by character Marilyn to Ed.
“My uncle once told me about a warrior who had a fine stallion. Everybody said how lucky he was to have such a horse. “Maybe,” he said. One day the stallion ran off. The people said the warrior was unlucky. “Maybe,” he said. Next day, the stallion returned, leading a string of fine ponies. The people said it was very lucky. “Maybe,” the warrior said. Later, the warrior’s son was thrown from one of the ponies and broke his leg. The people said it was unlucky. “Maybe,” the warrior said. The next week, the chief led a war party against another tribe. Many young men were killed. But, because of his broken leg, the warrior’s son was left behind, and so was spared.”
Jenn,
I can’t even find the words to let you know how thrilled I am for you! I have only been bedridden for months at a time, and it was just horrible each time. I cried for you when I watched Unwell, and now I’m thrilled to cry tears of joy for your recovery.
I am improving on electrolytes, high-salt diet, ldn, lauricidin, and several other treatments, but it’s been a long, exhausting, expensive, and excruciating journey which will probably continue for the rest of my life.
Keep getting better, advocating, and now – enjoying yourself!
Thanks for all you do.
I think the reason that I have problems emotionally with recovery stories is the same as the reason I can’t watch inspirational stories on the news. These people fought and triumphed. I’m fighting when I have the energy but I don’t feel I will triumph. I am hopeful that someone will figure this disease out but realistically I don’t think it will be in my lifetime.
I know how you feel – it’s hard not to feel that way after awhile – but check this out Dana – we didn’t know anything about CCI/AAI a year – and now Jen Brea is recovering. If you were a betting person what odds would you have put at that happening? Yet it did.
With all of us working together who knows what will happen? Who knows what will happen if the nanoneedle provides a diagnostic test?
You don’t have to have the energy for breakthroughs to happen. Other people can take of that. Good luck and keep the hope up 🙂
Hey Cort! Thank you so much for this excellent overview. It really helps pull together all the threads!
One quick clarification: I didn’t have overt neck symptoms until after my thyroid surgery. For the first seven years of illness, I had no symptoms I associated with my neck. Everything felt to me to be systemic.
Thanks! Congratulations again and good luck on your continued recovery:) Your story is really helping move this aspect of ME/CFS forward. Hopefully we will get much more brainstem research.
Speaking of that I emailed Avindra Nath Jeff’s story and today your story and asked him if he was looking at this in the NIH Intramural study and I gathered from his answer that he is. I hope that’s so!
The neck issues or lack of them, at least at times, in this spinal issue are so interesting.
That’s wonderful news! Thanks!
Can you make a correction to your article? Reason being that NEITHER Jeff nor I had overt neck symptoms before our surgeries. We BOTH had neck symptoms only after dental surgery (for him) and thyroidectomy (for me). I think that is important and I want folks to understand that I perceived my symptoms as systemic (which obviously they were—my brainstem was compromised!) and not as referrable to any specific part of my anatomy for the vast majority of my illness.
Sorry for the delay – I changed this: Jeff reported that, for most of his ME/CFS, his vague headaches and neck symptoms provided no clues that his head and neck. Jen reported that turning her head to the side did cause strange symptoms and that she had been averse to running when healthy.
To “Note that physical discomfort in head/neck area is not required! For the vast majority of their time ill neither Jeff or Jen experienced the kind of head or neck symptoms one would have thought would have accompanied CCI/AAI. Neither could have pointed to their head/neck area as a likely cause of their illness. Nor did Mattie – the third person with ME/CFS to have recently undergone CCI/AAI surgery. After reading Jeff’s account Mattie thought he didn’t have CCI/AAI – but got it checked out anyway – and found, to his surprise, that he did. “
Learning about Jen’s recovery yesterday and how she recovered, blew my socks off and I don’t think I’m alone in that based on all the responses. Im really happy for her, even ecstatic, but it opened some things up for me. I broke my neck in 2000 snowboarding at Snow Summit in Big Bear. I broke my C5 vertebrae and impacted my C4 and C6, so much so that there was no light between C4, C5, C6 on the X-Ray. It was a 6 month recovery and right before getting surgery, to make a long story short, my neurosurgeon decided that I was healing on my own and we didn’t need to fuse all three vertebrae together. Since my accident I’ve had very few issues with my neck. The only thing that stands out in my mind are a series of incidents where I was looking down at my phone, texting with someone, when I almost lost consciousness. This has happened maybe 8-10 times in 7 years. I always chalked it up to POTS and I’m an expert at dealing with weird shit going on in my body anyway. So at the end of all this, despite having extremely high IgG and a very low NK count, I need to eliminate the possibility of CCI/AAI. Talk about a head trip!
I’m sure Ron and Janet have thought a lot about this. Jen’s and Jeff’s stories make me think of Whitney. EDS does run in his family. If he did test positive I wonder if a) he could get to a neurosurgeon and b) if he could survive the surgery! Jen’s rebound after being in such bad shape did suggest we have amazing powers of recuperation.
I also wonder if the long term bed rest could contribute to ligament laxity (?). I couldn’t find any information on that so maybe it doesn’t. According to one site, though, these ligaments get reduced blood flows – which is another issue in ME/CFS – which does make one wonder if CCI/AAI is a more a risk for people with ME/CFS.
“I also wonder if the long term bed rest could contribute to ligament laxity … …which does make one wonder if CCI/AAI is a more a risk for people with ME/CFS.”
I know few of the above. But mechanics says that the position of skeleton and surrounding muscles will be determined by the quality of the skeleton, the surrounding connective tissue and the quality of the muscles keeping everything in the wright position.
With ME we can safely say that the range, strength and control of our skeletal muscles is below par. It’s easy to see how a borderline structural problem can become problematic when the muscles can’t keep good posture.
It is wonderful to see these kinds of stories, and for so many reasons.
Jennifer’s story provides a clearer picture (and a good example) of how one “small” thing, like an environmental exposure can, in susceptible people, cause a cascade effect that quickly causes dysfunction, and disability, in the body on so many levels at once.
To think that something like an environmental toxin can (amongst other things) invoke an immune response…that can (amongst other things) affect the strength of connective tissue…that causes (amongst other things) hyper-mobility in key spinal joints…compression of the brainstem…and POTS…which, in itself, leads to so many other far-reaching symptoms…and internal compensatory mechanisms (which cause symptoms of their own, and have many other systemic implications)…
This renews my confidence in the “invisible train” that I’ve been tracing in my own apparent “cascade”: Infection…systemic inflammation and autoimmunity (and likely MCAD)…(joint laxity appears to fit in here somewhere/somehow for me too)…POTS/Dysautonomia…full body “shut down” and “collapse”…sympathetic overdrive…gastroparesis…chronic SIBO/dysbiosis…leaky gut…increased inflammation and autoimmunity…(and around and around again).
(Recently I’ve come to view my own condition as more of a cascading, self-perpetuating cycle, rather than a linear “cascade”. I’ve been working on intentionally breaking that suspected cycle at multiple points within it all at once – whatever parts I can most easily get my own two hands on – and have had far more success with that approach than my previous, more scattered, attempts.)
Recovery stories bring up a mix emotions for me, as well. But mostly they make me want to keep on keeping’ on…keep organizing my efforts as best I can…and, to have faith in what I feel internally and observe about myself, even if those things cannot easily be seen, diagnosed, described, or defined.
Congratulations Jennifer!
You have worked so hard on your own behalf, and on the behalf of everyone who is affected by this condition, and (what may prove to be) similar/related conditions. Thank you for all of your work, and for your tireless advocacy efforts. I wish you all the best in your continued recovery!
Maybe this piece of information fits into Jennifer’s recovery story:
There is someone on HR forum who has a skeleton structural problem and believes the pelvis takes a key role into this disease. I wouldn’t go that far but I combined her thoughts with my keen senses and got to this:
When moving my pelvis in a way that changes my back curvature from hollow to the opposite and back, I sense my head feels different. It started when I learned that bigger of these movements could help turn down a very rapid hart beat in the late night to a normal one.
That was probably due to improving the flow of pooled blood in the legs to the hart. It isn’t the best technique to do so as it’s fairly aggressive to the back but I often felt a clear “surge, fresh flow” of rich oxygenated blood to the head. Part of it probably is because improved blood flow means improved blood flow in the lungs as well and hence improved oxygenation. But the “short shot” effect felt to be beyond just having more oxygen in the blood as the effect lasted a few seconds only each time.
Then, when reading upon Jeff’s story I asked my very good physical therapist to teach me some exercises to help stabilize my neck and, as I believed I could better stabilize my neck with a more stable pelvis, to help stabilize my pelvis.
She is good on telling how things are connected to each others and hinting to what I should feel when doing something. I’m good on interpreting what she says and linking tiny difference in how it feels with what she says about how things are connected.
As a result, I learned that even small regular movements of the pelvis, like every single time I do a cycle of diaphragm breathing, is sufficient to give a single tiny “boost of rich oxygenated blood” lasting one to two seconds to the brains. But when one practices diaphragm breathing it happens over 10000 times a day. I also sense something similar with chest breathing but to a far smaller extend so it’s vague.
My therapist and I combined our thoughts and came to the conclusion that this is what most likely happens:
Each time I diaphragm breath or do a bigger movement with my pelvis, the curvature of my back changes. With it, the line of my spine and the surrounding tissue gets contracted or expands a little bit. This line holds the long tail of the spinal fluid bag.
Two things happen mechanically when pulling onto that tail even a little bit. The first thing is that the tail becomes a bit longer but a lot more narrow so it’s volume goes down. That expels some of the fluid from the tail into the brain part of the bag. The other thing that happens is that the tension in the brain part of the bag rises a bit.
Having continuous cycles of puling / relaxing / puling / relaxing… then does three things in a small but enduring way:
* There is a small but enduring cycle of spinal fluid being moved from the bag to the tail and vice versa. So we’ve got a small spinal fluid pump / mixer which may be a good thing.
* The brain part of the spinal fluid bag sees each breath a wave of contraction / expansion or more pressure / less pressure. Such waves travel to the entire jelly brain structure. There it can help moving blood in the capillaries (as CBF pressure should mechanically speaking help determine amount of blood flow in the brain) and even better help removing “debris” in the capillaries as oscillating movements often are better at getting stuck debris unstuck. Just think about how you try to get stuck objects unstuck: not by keep pushing onto it but by alternately push fort back forth back. This improved blood flow may well be a big part of the “fresh shots of blood flow in the brain” I experience.
* What holds for improved blood flow in the brain should also hold for improved flow of lymph in the recently discovered lymphatic system in the brain. That helps removing waste out of the brain.
I have no clue if this surgery makes the neck and spine more flexible or more rigid. But if it would make it more flexible (or allow better spinal tail deformation) then this “spinal tail puling” should result in a bigger effect in the above three parameters. I’ll leave Jennifer and others to judge upon how it affects them.
As ME patients have very often more tense muscles and a more rigid posture, they should see a lesser effect of this “spinal tail puling”. So if this mechanical pumping action were important enough for brain blood flow and waste removal then having ME rigid neck and back muscles (and other stuff like connective tissue problems) should pose a challenge to the health of our brains.
In that same view, if both my keen senses and my PT and my views on how things connect to each other are correct and play an important role in the brain blood flow and waste removal, having such spinal problem solved would touch to (part of) the core of ME disease. Rather then potentially never having had ME, they may have addressed a key component of ME: dis-regulated blood flow in the brain due to blocked spinal cord movement and spinal fluid flow.
Thanks for the informative article, Cort!
One thing that you didn’t mention is that chiari and CCI are not all that uncommon in people with Ehlers-Danlos Syndrome–though not especially common either. With EDS, having cranial instability (in addition to instability in many other places in the body) is quite understandable due to the compromised connective tissue. The muscles sometimes aren’t strong enough to hold the head stable. Also EDS tissue can have a tendency to stretch and droop out of position.
You mentioned getting the proper imaging for diagnosis. I cannot emphasize this enough, especially for chiari! There are not so many upright MRI’s machines and so many doctors who are not so appraised on diagnosing these conditions, will do a regular supine MRI. Often the drooping brain stem will not be apparent unless a patient is upright.
I have read many stories on my EDS forum about this problem of a missed diagnosis. So, if you have some of the more exaggerated symptoms that Jennifer had (more on the uncommon side of ME/CFS), be sure to go to a doctor who has access to this specialized imaging!
Kind thoughts to all of you who suffer!
Thanks Nancy. The EDS / ME/CFS connection is getting ever more interesting. It will certainly show up in future blogs.
What Jennifer’s story tells me is that skeletal problems should be investigated much more and as a first port of call. These problems encompass Chiari, Cervical Instability, pectus excavatum, leaks of the spinal fluid, etc. They should be checked immediately to avoid years of disability because treatment exists for many of these problems.
I myself had pectus, which was brushed off as a “cosmetic issue”. After 10 years of search for advice I eventually managed to get a scan, and it showed I had a very severe case with heart and liver compression. Decades after falling ill it was corrected. It was a much more difficult and riskier surgery than should have been had it taken place 30 years earlier, and recovery was much tougher and longer. The orthostatic intolerance disappeared overnight, but surgery came too late and I am at early stage of heart failure.
The problem with doctors is the way they think. They think, “Plenty of pectus patients do not have ME, so pectus does not play a role in this”. Instead of thinking, “The patient cannot stand still, are there any “structural” problems that could -even partially- restrict blood flow to the head?”. Doctors are still in the mode of one-cause-one-disease.
Ann, you are so right. When I initially became ill, I had a lot of testing done.
Initial symptoms:
June 2008 a sharp chest pain event, thereafter wild neurological symptoms in limbs and head, extreme post-exertional malaise, cognitive fog and unrefreshing sleep.
Initial testing: (this is not inclusive)
PECTUS EXCAVATUM: Haller Index 3.6
CHIARI-1 MALFORMATION – 8mm, rounded morphology (08/07/2008); 5mm, peg-like morphology (08/26/2014)
Mild CROWDING OF THE FORAMEN MAGNUM (08/07/2008)
DIMINISHED CSF PULSATION IN THE DORSAL ASPECT OF THE FORAMEN MAGNUM (08/07/2008)
Mild degenerative changes are present throughout the cervical spine with posterior disk bulges from C2-C3 to the C6-C7. NARROWING OF VENTRAL CSF SPACE FROM DISK BULGES; no significant overall spinal canal narrowing secondary to sufficient dorsal CSF space. (08/07/2008)
All of this was noted in August of 2008 two months after my initial event on June 8, 2008.
The cardiologist and the neurosurgeon both said my symptoms could not be explained by these finding and in October of 2008 I was diagnosed with CFS.
In 2014 I went to Workwell and my 2-Day CPET showed cardio-pulmonary abnormalities in every category.
In 2017 I was found to have two antibodies, Jo-1 and Ro52 and diagnosed with Antisynthetase Syndrome (ILD with dermatomyositis) and Sjogren’s Syndrome.
My new doctor says he thinks I had the Jo-1 and Ro52 all along. My question is why was I constantly told “you have CFS and there is nothing we can offer but GET and CBT.”
In my experience, the moment CFS was put on my case in 2008 I was not taken seriously until a high resolution CT scan showed mild interstitial lung disease in 2014 following the 2-Day CPET. It was only then that even started to look for anything and I still don’t think they took me seriously until the antibodies were found in 2017 and I still feel like I am told your symptom severity does not match what we are looking at for this patient population.
Ann – again you are right, “Doctors are still in the mode of one-cause-one-disease.”
What I want to know is why aren’t you and Jen counting Dr. Rowe’s patients as having recovered from spinal surgery? And whether if you have cervical spinal stenosis, are you more likely to have CCI and other instability issues? Do we know of any MEEPS beyond Dr. Rowe’s three who have recovered or had major improvements in their ME after spinal stenosis surgery with or without fusion? I had 3-level spinal stenosis surgery with fusion and decompression 5 weeks ago and am wondering if this might give me an ME improvement/recovery? I think that cervical spinal stenosis must be much more common than CCI but I don’t know for sure. But if people are having improvements from cervical spinal stenosis surgery, why would we not count them all together? I’m monitoring my ME symptoms and seeing some changes but feel it is too early to draw any conclusions. Also using the forms that Dr. Rowe used in his study to monitor my results. If someone else would like to use the forms or scales he used, please let me know and I’ll provide them when I am able. It’s wonderful work you are doing, Cort! I’ll kick in a donation now to say thank you!
Thanks Esther, a blog on Dr. Rowe’s reports on spinal stenosis is coming up. Dr. Rowe’s report highlights how important it is to get Jeff and Jen’s and others history into a case report in the scientific literature. That will alert other doctors to this issue and provide the basis for grants to study this more.
Hi Cort- I can’t keep up with all the reading around this issue so I might have missed this, but will their case reports be published? I agree- it’s very important!
When I developed ME/CFS after chemotherapy my oncologist swore this had never happened before. I asked him to write a case study documenting my before and after (dramatically declined) cardiopulmonary test results. He said he didn’t have time. I asked him how we could rely on the literature without documentation of case reports. If he didn’t write it up, how many others didn’t either? I didn’t get anywhere.
Showing up at doctor appointments with published information is the only way I have persuaded doctors to do testing or try treatments.
Hope Jeff & Jen & other cases do get documented.
Birdie, I agree; I do not understand the whole process of doctors reporting things. Not one doctor of have seen has reported anything. This whole bloody process has shown me how much “medicine” is just belief. We read articles and studies and we just believe until we start digging. Like the PACE Trial; garbage in, garbage out. We hear stories about how there have been no reports of adverse effects of x, y, or z but then you look and there are lots of anecdotal reports. We are left trying to figure out where the truth lies. Exhausted by trying to understand the definition of every word, the agenda of who is writing or publishing, etc.
I think the really compelling thing about mechanical explanations relating to the neck and spine–not just CCI, but mechanical Intracranial pressure, cervical spinal stenosis, etc etc.– is that it can potentially speak to two of the biggest puzzle pieces in ME:
1) Why are millions of people exposed to the same viruses, toxins and pathogens but only a few go on to get ME?
2) Why is there such a prevalence of women in the ME patient population?
I know MS research (another illness largely effecting women) is also looking at structural stuff in the head and neck. I am not an anatomist, so have no sense of the details, but it seems likely that women are built somewhat structurally different than men. Narrower spinal column? Narrower everything? More potential for movement in the pelvic area that could cause destabilisation upwards into the spine and neck? And, again, this would also fit in with the prevalence of ME in the EDS population. I also wonder how many men with ME had suffered a traumatic injury to the back or neck at some point prior to becoming ill?
I think CCI is just one way mechanical issues may manifest, but it gives us a clue to the importance of head, neck and spine mechanical issues in ME in general.
This is another interesting bit of research that fits in with the above:
“Borderline Intracranial Hypertension Manifesting as Chronic Fatigue Syndrome Treated by Venous Sinus Stenting”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4648738/
They say IIH “manifesting as” Chronic Fatigue Syndrome, rather than going all the way and saying that this might be one of the underlying factors in ME/CFS. I find that quite annoying, but hey.
The great majority of patients with MECFS do not have Borderline Intracranial Hypertension. What this paper,(and the Jennifer Brea case as well) shows once again is the importance of a proper workup by a good physician to rule out all potential causes of their symptoms. Sadly, no matter the current confusion out there, MECFS remains a diagnosis of exclusion. That means the diagnosis should only be made if after a rigorous and complete workup, there is no known cause for the patient’s symptoms. It’s a hard thing to swallow, but that remains the current state of our knowledge.
I haven’t read the comments above, it occurs to me that Jen would have failed the nano-needle (Ron Davis)/intracellular phenylalanine (Karl Morten)/mitochondrial fragmentation (Bupresh Prusty) tests.
As you highlight, this type of surgery is very risky – it should only be undertaken where the evidence is clear and the surgeon is competent.
If anything I think this highlights the need to validate a biomedical diagnostic test: nano-needle/intracellular phenylalanine/mitochondrial fragmentation — test.
Yes we more than ever need a good diagnostic test think, though, about how much controversy THAT will raise when some people with clear ME/cFS symptoms, onset and other tests, don’t test positive – which I’m sure will happen!
With all the other factors Jen and Jeff had – the POTS, MCAS, the fact that Jen was taking several drugs that often help with ME/CFS – my guess is that she would test positive on Ron’s test – that their brand of CCI/AAI basically caused ME/CFS while other brands of CCI/AAI do not. It’s going to get really interesting!
I’m so happy for Jen but also Omar and all other caregivers/husbands etc who see reversal or vast improvement in those they care for.
We can not help but be happy for Jennifer Brea but many are now
beginning to think that this is not a case of recovery from MECFS but rather its a case of misdiagnosis of MECFS in the first place. If she had craniocervical instability (or any other variation of Ehlers-Danlos Syndrome) and that explained most all of her symptoms it was not MECFS and never was.
Already those who were caught up in the publicity of this high profile case are starting to twist their explanations of what happened. I am reminded of the damage that was caused in 2009 when after huge publicity was given to the retrovirus XMRV as the definitive cause of MEFS, many could not admit their mistake even after the retraction in the journal Science. The negative fallout from the confusion caused from that episode took years to overcome. I hope that doesn’t happen again.
It’s a definitely recovery if Jen can get away with 30-90 min of weight exercise, light or otherwise. I can do occasional spurts, but exercise of any intensity other than slow walk for more than a few minutes at a time definitely cause PEM for me. That’s despite that I am a mild/moderate patient who can walk 2 miles on a good day as long as I incorporate enough breaks.
That said, I don’t blame patients objecting to this kind of recovery story. People too often tout X as the recovery method when the recovery may well have been just a coincidence; you never know unless you do controlled trial. And NONE of these recovery stories have passed the test yet as far as I know.
Jen’s CCI surgery could be just another coincidence. I wouldn’t read too much into it till a study shows that CFS patients suffer from CCI more often than by chance and that CCI surgery relieves CFS by more than a chance.
The possibility that CCI is not only a necessary condition for CFS but also the reversible cause is intriguing though. Wouldn’t it be nice if it is as easy as getting a neck surgery to recover from CFS? But it is just too hard to imagine that given what we already know of CFS and its known risk factors.
The main thing I know is that NO ONE ever had the slightest intention of solving
the original CFS.
The most important thing for “ME/CFS researchers” now is to try and write a narrative that makes it appear as if they had.
https://youtu.be/OYGIX4iw6Uw
Maybe they thought cfs was related to these outbreaks:
https://www.betterhealthguy.com/episode98
This video is well worth listening to
Dear Cort,
I have found the article below very important and relevant to the topic.
Best regards
Raquel (form Brazil)
http://dysautonomia.com.au/fibromyalgia-syndrome/
It sounds to me like it turns out that Brea never had ME/CFS/Fibro in the first place. If all it took to cure it was a spinal surgery, we’d all be jumping up and down with joy.
What really makes me angry though, is that even if you are privileged enough to live in the US, you still need top notch insurance and a huge amount of money for what insurance won’t cover. Not to mention the ability to take off of work.
It’s so unrealistic for the rest of us to think that we’ll get any help in our lifetimes. All we can hope for, is that this research helps future generations.
interestingly, i was diagnosed as severe back in 93 but i had slow onset starting at the age of 20, then i complete “blow up” of my immune system in 93 and had to stop life…i have all the gut problems..all the brain fog…all the other symptoms to go along with cfs. I also, at the age of 18ish, was involved in not one but two car accidents…one from behind and one from the side. Fast forward to aprox. 2012 i again get hit from behind while at a red light from a full speed (50km/hr.). my head goes clean through the rear window of the truck and im knocked out. I get taken by ambulance to hospital and the doc says take some tylenol..you will be fine…the cop that came into the room with me says to the lady doc…”lady..his head went through the window..he needs an xray”..yes the cop says this! The exray shows major arthritis from the first accident many yrs prior.
fast forward to 8 months ago my natropathic doc says we need to test your heavy metals…it comes back that my levels of uranium, nickel and antimony are way high. I have bought Dr. Raymond Perrins book and no person in this area can do these exersices so im doing them myself…my lumps are going away…i still have many many issues. I went out to shoot my bow this winter..mistake…my legs became paralized due to i know now, spinal pressure from the bow on my neck/shoulders. I never fit cfs criteria as my sever fatigue only lasted a few months…but i am always fatigued..just not in bed full time like some. I do have all the other problems like chemical sensativities…on and on and on with all the other stuff. I was called crazy by doctors ..neighbours…friends….my parents…it didnt sit with me too well. I am quite sure i have , also, PTSD. Its a shitty life but im above ground for now. I recall a time when if i could have gotten out of bed i would have went to the basement and got the gun. Thank god i couldnt get out of bed. My bedsheets were brown in a week with toxins..still are. I believe now that the arthritis in my neck is stopping or slowing down the flow of toxins that get drained from the head..i have constant sinus infections etc. long story version coming soon
….adding to the above….. i know this only pertains to some of us. i now wonder if there is a way to create bone loss. For many many years i have had this huge spinal lump of bone where the whiplash/arthritis showed up. This lump is, over the years, slowly going down and away…could it be that the body is either pulling bone away or could the body be the body adjusting the spine itself. I only started the Perrin exercises about 6 months ago so that cant be why the hump is lessened. If we could find a way to create bone loss, would it take the pressure off our spines ..then we wouldnt need surgery.
Glad she is feeling better but the vast majority of CFS / ME patients do not have this – and some have died in this surgery.
First of all, I’m super happy about Jennifer Brea’s recovery and for new directions for research to go in that this brings about.
This illness is so confusing. To add to the problem, we don’t always know what information is relevant and what is not.
At an attempt to throw it all at the wall and see what sticks. I have found a lot of things of relevance and some of questionable relevance. For example, I found out that I have:
– sickle cell trait
-scrub typhus (since treated)
– low testosterone (possible sign of infection?)
– extremely elevated cortisol awakening response
– antibodies for c. pneumoniae and epstein barr
– igG food sensitivities (many, including unexpected ones)
– multi- and mold-susceptible genes
– reduced gut bacteria
– low pancreatic elastase
– a thyroid nodule
– kryptopyroluria
– low vitamin D.
Try to make sense of that (because I cannot)?!
With moderate brain fog, in a way it seems a cruel joke that I am the one who has to research and make sense of these things. However, I am grateful to at least been able to pursue these different medical tests in a quest for answers.
That said, my older family members all have significant forward neck posture. And right around the time that I got the sickest, I experienced a neck injury from a hair salon wash basin (they had me in it for 20 minutes and my neck was killing me afterwards and almost immediately my health took a turn). So…could my POTs, sleep problems, stomach pain and bloating, and fatigue have been due to a neck injury?? Confounding things I was also exposed to mold right around the same time (and I tested as mold susceptible).
Not sure where to go from here. I am slowly getting improving, but it has been several years now and I am nowhere near 100%… It is very discouraging at times as I used to be a highly active person…
Encouraging story, but she’s not totally recovered. Many cfs suffers like her, seams recovered but actually more problems are waiting! To know a real recovery story from cfs and ALL illnesses without any medication and surgery, check out Julia On Health
I’ve just finished watching ‘Unrest’ which is how I came to this site. I have had M.E since developing Adult on-set Stills Disease in 2011. What I have found most interesting is that I also have spinal conditions too, spinal stenosis, osteo- arthritis, diagnosed in my mid-30’s . Wonder if the two are connected
In my humble opinion, the theory and therapy offered by Dr Raymond Perrin is worth a second look and may fit with/explain Jennifer’s recovery story. Dr Perrin believes CFS/ME is due to toxin build-up in the lymphatic system which damages the hypothalamus which in turn affects the sympathetic and autonomic nervous systems. The hypothalamus is unable to function properly which results in toxins back-flowing into the brain and spinal chord (both of which don’t have a proper lymphatic drainage system) instead of being eliminated efficiently and quickly by the liver. The result of toxin build-up manifests as CFS/ME symptoms. Dr Perrin’s therapy is a specific type of massage – The Perrin Technique – which helps to drain toxins from the spine and brain. He has an 85% success rate. I’m just reading his book and had a eureka moment. I remembered Jennifer Brea recovered from CFS/ME after spinal surgery, so maybe the surgery helped toxins to drain away from Jennifer’s spine, thus leading to recovery from CFS/ME?
Also, it’s always puzzled me why ME/CFS has different causal factors prior to onset in different people. For some people it follows a virus, for others it comes on after a car crash or stressful life circumstances; for others it’s due to mercury poisoning etc. The common thread with all these things is that any form of stress (good or bad) causes reactions in the body which produce toxins as a by-product. Thus if the body becomes overloaded with toxins, it could act as the last straw on the camel’s back resulting in toxin overload and CFS/ME. Dr Perrin explains the back-flow issue in really simply terms making it easy for the layman to understand. It’s to do with the large protein molecules (i.e. the toxins) in the lymph system reducing the hypothalamus’ function. Once the toxins are cleared, the hypothalamus functions normally again and the CFS/ME disappears. This would explain why some people recover on the vegan diet or by juicing fasts or by mega doses of probiotics or by the grain free, dairy free paleo diet or the leaky gut diet, AIP diet – or via the Perrin Technique. All these things (for some people at least) help the body eliminate toxins. It could also explain why a certain type of back surgery (i.e. Jennifer’s) aids recovery – because somehow the procedure enables toxins to drain away from the spine and brain? I suspect – I hope – Dr Perrin is on the right track. I’m about to have my first consultation with one of his associates this week. Best wishes to all from your fellow CFSer (16 years and counting; sometimes bedbound).
I wouldn’t be surprised if Jennifer’s operation helped drain toxins from the spine. If I remember correctly it basically lifted her head off her spine. I imagine there may have been quite a blockage there. For me, toxin buildup in the central nervous system certainly makes sense.
Good luck with Dr. Perrin!
I would love to know how your consultation went. My daughter’s illness started with swollen lymph nodes, mouth and nose ulcers, extreme fatigue, low grade fevers, muscle and joint pain, exercise intolerance, POTS. It was very insidious and progressed with dysautonomias especially gastrointestinal dysfunction with anorexia. Almost every body part is affected. She has been diagnosed with hEDS. She has major problems with neck instability, swallowing difficulties, vertigo, nausea, nystagmus, being over whelmed with thoughts, anxiety, fear, She suffered a lot of trauma from the medical system here in New Zealand. Currently she is practicing Ayurveda and for the first time in 6 years she is getting improvements in many symptoms. We are lucky she’s still alive.
Jen never had ME/CFS. It was a bad diagnosis and all it does is distract from the work at hand to funnel money into the diagnostic test and other symptom minimisation research. I love that she went VERY QUIET when she realised it was not in fact ME/CFS but the CCI thing. I feel no love lost for her as she did nothing in Australia but promote herself and her film with no real support to the 250,000 sufferers DownUnder. She couldn’t even get the facts right here. She was playing to be seen to do the right thing but in fact didn’t. It was all about money and about her and her film production career. The real hero DownUnder was David Tuller. He doesn’t even have ME/CFS and was genuine, heart-felt and went out of his way to help our community raise much needed publicity as well as give so much of his time. he is still going in his support for people with ME/CFS. That’s how genuine he is. His tour was at least factually backed and supported by many state and national advocates with whom he worked plus ME/CFS Australia Ltd who provided him with a thorough briefing on the situation here and key influencers.. He made a conscious effort to use his journalism background and reputation to arrange appointments with key Government decision makers. For those of us still with ME/CFS, look to others who are not flashes in the pan.
It was all about money and about her and her film production career”
Agreed. She made sure to film her worst times her film is cringeworthy
My CFS started 21 years ago. After three years and a dozen doctors started taking cortisol tablets and experienced immediate relief. I have been taking 40 mg daily ever since. For more info call me at 650-868-0603
Hi! I was diagnosed with CFS about a year ago, after several years of struggle. I’m 41 now. My case is in no ways as bad as Jen’s. I have a “normal” life, just I am not the same I used to be. I have much less energy, I have foggy mind, strong memory issues, my batteries last for 3-4 h (in a good day) and after that I just survive doing the mandatory things I need to. I can’t sleep (for years). So my personality, hopes and ability to enjoy life has decreased dramatically. They give me antidepressive pills I won’t take.
BUT, three months ago i started an anti-inflammatory diet (no sugar, no gluten, few carbs) that just changed the game. Almost immediately I began feeling with more energy, clarity of mind and happiness. I sleep much more better, not perfect, but fine most of the nights. So, I don’t know if it’s gonna last, I fear I’m like Cinderella and it’s gonna stop working suddenly, I enjoy wile it does work, and keep looking for clues that help me. It was major for me discovering I need to fight inflammatory issues, as I have always been thin and didn’t understand it is not related with weight.
I know many many things can relate to a CFS, just needed to share my journey in order to help keep building that puzzle.
(Plus, few years I took anticeptive pills for a while, and I got worst, so need to share that too!)