

A Story With Hope
“Just over a year ago, I could not leave my house without a wheelchair. I spent most of my day on a couch or a bed, lying or sitting down. I avoided light, sounds, gatherings.” Christine

A year ago, Christine, a nurse, was in a wheelchair herself. (Image by Peggy und Marco Lachmann-Anke from Pixabay)
I attended the Accelerating Research on ME/CFS Conference at the National Institute of Health (NIH) in April 2019. I am a Nurse Practitioner (NP) who worked for many years in a setting where I often sent my patients to the NIH to participate in particular studies. I was not at the Accelerating Research on ME/CFS conference in my capacity as an NP, but rather as someone who has lived with ME/CFS since 2004.
I have my own story of hope, and I decided to share it here because I met so many people at the conference who, upon hearing a bit of my story, pulled out a paper to jot down the name of the method which I credit with my recovery. If this account can be helpful to even a subset of people who live with ME/CFS, then it will be worthwhile.
Just over a year ago, I could not leave my house without a wheelchair. I spent most of my day on a couch or a bed, lying or sitting down. I avoided light, sounds, gatherings.
The Change
My journey to that point is a complicated story. The change in my health status started in 2004, when I was hospitalized on a neurology unit with difficulty walking, extreme fatigue, strange sensations in parts of the right side of my body, and vertigo. I was discharged after a few days of studies, with the evaluation to continue as an outpatient.
The work-up continued for weeks, including further MRIs, an electroencephalogram, a sleep-deprived electroencephalogram, an electronystagmography (ENG), and lab tests ordered by specialists in Infectious Disease, Rheumatology, and ENT. The only abnormal result was the ENG, which pointed to central nervous system pathology, though all MRIs of the brain and spine were normal. I spent 8 weeks on sick leave, puzzled, extremely concerned, and frustrated that I could not regain my energy.
Finally, I was given a diagnosis of vestibular neuronitis of viral origin, though the virus was not identified. I was suspicious that it might have been West Nile Virus, which was endemic in my neighborhood. The diagnosis felt pretty nebulous and not completely satisfying. A colleague at the clinic where I worked later told me that she had suspected I had a brain tumor when she heard about my symptoms. My neurologist was contemplating a diagnosis of multiple sclerosis.

Over the next ten years, Christine was on an ME/CFS rollercoaster with her health declining, getting better, and then declining again. (Image by Free-Photos from Pixabay )
Fortunately, after my 8 week leave, I recovered sufficiently to gradually return to work part-time – though I always said I was never the same after that. I needed more sleep and water, a schedule with a mid-week break, and to avoid heat, standing, and excessive exertion.
I had been a generally healthy 43-year-old when my symptoms began, though I had taken many rounds of antibiotics and anti-parasitic medicines during the 9 years I lived and worked in Central America from 1985-94. In 1992 I also was diagnosed with Erythema nodosum, a skin condition where red painful lumps would periodically appear on my shins. This condition is sometimes an indication of underlying infection, though, as in my case, the cause is often not identified.
After 2004, I would relapse in 2005, 2007, 2011, 2013, and 2014, spending weeks off work. The trigger for the relapse was usually some form of physical exertion. I had always enjoyed running and still kept this up with less frequent, shorter runs, except during relapses, and never in the four hottest months of the year where I live.
My doctor, my family and my community would all wonder about the “mysterious illness” that would periodically resurface and take me down. I returned to my neurologist for further testing, and revisited rheumatology and cardiology, ENT and Infectious Disease for multiple work ups over the years.
Then in 2011, I started to have significant gastroenterology issues (diverticulitis, Irritable Bowel Syndrome) and ended up with major complications, leading to heavy antibiotic use, and repeated Clostridium difficile (C. difficile) infections that would not respond to high-powered antibiotics.
In April 2014, I hit my head in my kitchen and was diagnosed with a concussion. All of the symptoms that had started in 2004 immediately returned: the unusual gait in my right lower leg that was always present with an episode, the changed sensation in my right lower leg and the right side of my face, profound fatigue and the need to avoid exertion. After weeks of rest, my symptoms gradually resolved and I cautiously and very gradually re-entered my workplace.
In the summer of 2014, I had a repeat episode of diverticulitis and C. difficile infection. Concerned about needing to repeat rounds of high-powered antibiotics without complete resolutions of the symptoms, I researched fecal microbiota transplants (FMT).
After finding a gastroenterologist who would perform the procedure, I had an FMT in September 2014, which cured my C. difficile infection. Interestingly, however, my level of energy also dramatically improved, and I felt energetic again. My family commented on how I seemed to be coming back to my pre-2004 self.
A Major Decline Begins
In late August, 2015, though, while running on a relatively cool day, I suddenly had to stop, and then could hardly walk. I stumbled home feeling nauseous and disoriented. Another work-up began: cardiology, neurology, emergency room visits, a lumbar puncture, and repeat MRIs of the brain and spine. Since nothing significant had appeared in the past (beyond low white blood cells, no fever with infections, overly brisk deep tendon reflexes, and the abnormal ENG test), I figured it would just result in another 6-8 weeks off work.

In 2015, out of the blue, Christine’s health took a deep dive.
This time, however, my health and level of functioning continued to decline, in spite of normal labs and imaging results. When I felt like I was improving, I would take a walk around the block and then try to extend the walk the next day.
On one of these occasions, I suddenly felt like I could no longer move my legs, and electric sensations started climbing up my legs to my lower spine, then to my waist. I somehow managed to get home, and then I trembled in bed, on a hot day, incoherent and barely able to move. Apparently I was experiencing post-exertional malaise, though all of us who have lived through it know it merits a different term.
This last episode convinced me I was facing something more serious. I resigned from my job in December 2015 so I could focus on recovery. I was given the diagnosis of ME/CFS in March 2016, when both my primary care physician (PCP) and I recognized that I met the criteria. I had this diagnosis confirmed in October 2017 by an esteemed ME/CFS specialist who was a panelist at the April 2019 NIH conference.
By then I was in a wheelchair, which I finally requested in early 2017, so I could attend my father’s funeral. I could hardly leave the house. My world had become very small and unpredictable, as I found I needed to shield myself from stimuli and exertion.
I would say to my spouse that I felt “activated,” and he could often recognize the process in me. Even my PCP would say, “It’s happening again, isn’t it?” The onset of my symptoms felt like a switch had been turned on in me that I could not control.
What To Do?
Along the way, I tried many methods and many medicines for recovery. My PCP, whom I greatly respected, told me in March 2016 to find a specialist, since the condition was outside her realm of expertise. She also made the comment that she did not think that we would find a treatment for this in my lifetime. My thinking: I only have this lifetime, and I have 2 daughters. So I set out on my own quest, when energy permitted.
In the first episode in 2004 when I was diagnosed with vestibular neuronitis of viral origin, the neurologist prescribed low-dose Clonazepam. He knew I was an NP, and that while that class of medicine is typically prescribed for anxiety, he was prescribing it instead “to cool down your whole nervous system.”
It seemed to be helpful. I would use the medication in very low dose twice a day for the periods of my “relapse” and then wean off it again. In late 2015, my PCP suggested staying on it, which I did for three years. In 2004, I also decided to visit an acupuncturist, since Western medicine was not offering me any other suggestions for recovery. I found it helpful, so would make an appointment periodically.
After my second round of diverticulitis in 2012, given all my gut symptoms, I started reading about different diet approaches and was particularly struck by the book Breaking the Vicious Cycle, by Elaine Gottschall, who recommended the Specific Carbohydrate Diet. I followed the diet for almost a year and then was able to expand my food choices. The diet pretty much eliminated my abdominal pain, which was helpful in avoiding the stress of wondering if I was headed toward another episode of diverticulitis. However, I had trouble sustaining my normal weight, and so added in other foods.
The Gist
- Christine, a registered nurse, first became ill in 2004 as the result, doctors thought, of a mysterious virus.
- Over the next 15 years, she relapsed and recovered five times but did not recover from the last relapse which came out of the blue in 2014.
- Besides the possible viral infection she also experienced a C .difficile infection and concussion, and was diagnosed with HHV-6 reactivation and irritable bowel syndrome.
- She was diagnosed with ME/CFS by her primary physician in 2016 and by an ME/CFS expert in 2017.
- Before she began the DNRS program she’d become wheelchair bound and was hypersensitive to light and noises.
I went gluten- and dairy-free, which I pretty much maintain to this day. I tried a more extreme elimination diet, which was not particularly helpful. I take a probiotic and saccharomyces boulardii, a yeast recommended by my gastroenterologist given my C. Difficile history.
I also read the book The Wahls Protocol, by Terry Wahls, in pursuit of other potential remedies, since multiple sclerosis was in my differential. Her focus on feeding our bodies with quality foods high in nutrients and good fats, and avoiding toxins, processed foods, sugar was something I chose to adapt.
As it happened, after my own fecal microbiota transplant, I became very interested in the microbiome and attended a conference on the topic in Barcelona in early 2015. The link between the brain and the gut felt so pertinent to me. When my gut was in distress, it impacted my cognitive and emotional state of being and my level of energy significantly. Unfortunately, I was too weak to attend the follow-up conference in Miami in 2016.
I visited an osteopath and received craniosacral therapy, which I found helpful, if not curative, though it was expensive and far from my home. Looking back, the osteopath’s advice to increase the time spent in the rest and recover mode of the parasympathetic nervous system makes even more sense.
She recommended oil of oregano for management of candida in my gastrointestinal tract, visible on my tongue. This slower method of killing it off was easier for my body to tolerate than Fluconazole. My acupuncturist is also a Qi Gong master and showed me a few helpful moves to incorporate into my day. I also started listening to a short Yoga Nidra tape, a form of guided meditation, on most days after lunch. I meditated for 30 minutes a day on most days.
When I saw the ME/CFS specialist in Oct 2017, I tested positive for Human Herpes Virus 6, and was initially prescribed the antiviral Valgancyclovir (Valcyte). However, after an unexpected trip to the ER for chest pain, my white blood cell was again low and declining. I was not a candidate for Valcyte. I opted to take Acyclovir for 5 months from January until July 2018.
I also started low-dose Naltrexone (LDN) in December 2017, which I continued to take through December 2018, and soon added methylfolate and glutathione nasal spray for a few months in 2018. An earlier SSRI (anti-depressant) trial over 8 weeks was not helpful, as it disrupted my sleep no matter what time of day I took it. I tried many other supplements as well as tapping, body brushing. I experienced small gains with many of these remedies, but it did not feel like I was restoring my health as I wanted.
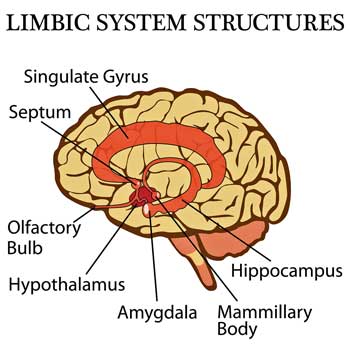
Researchers and doctors have pondered the role the limbic system plays in ME/CFS for decades…
In 2016, while visiting the Health Rising website, I read about the upcoming Cortene trials that treated ME/CFS as a limbic system disorder. I had not thought a lot about this approach to the illness, but found it intriguing. However, I knew it was unlikely that I would be accepted into the trial, and I also felt extremely cautious about the idea of taking a new medicine, leery of the possible side effects.
Then, having heard some of my story, a colleague of my husband’s suggested I read Wired for Healing, by Annie Hopper. I had read so many books that I did not immediately request it.
A little later, however, I heard a video series on brain injuries where Annie Hopper was interviewed, and once again her approach caught my attention. Her name then came up in a third setting with a friend who had used the method to overcome extreme sound sensitivity, so I decided to learn more about the method.
I visited Annie Hopper’s website to order her book, and also decided to order the DVD series where she teaches her method, the Dynamic Neural Retraining System (DNRS).
Rewiring My Brain
Here my story begins to change. Within a week of beginning the DNRS method in March 2018, I felt a significant shift in my body — not huge, but enough to tell me that I was on to something, and that I would stay the course.
The DNRS regards ME/CFS as a brain injury, specifically to the limbic system, and uses a method of neurorehabilitation as treatment. Foundational to this method is the science of neuroplasticity – the findings that our brains have the innate ability to change and are vulnerable to being altered by the environment, in good or bad ways.
Now, I pause.
I know that because the treatment involves neurorehabilitation, some will say that “it is all in your head.” I have come to agree that the condition begins in my head, where my brain resides, just as a stroke is in your head, or a brain tumor is in your head, and no one denies the severity of that or the fact that it is a physical finding.
I believe that in ME/CFS, the injury is real and physical, even if science has not yet found the tools to identify it. In the movie Unrest, I so appreciated the story of how multiple sclerosis was for many years known as “hysterical paralysis” before imaging could identify the damage to the myelin sheaths. The same will eventually happen with ME/CFS, which is why studies and research are so crucial. But since we only have one lifetime, those of us alive and suffering need more immediate solutions or methods that can improve quality of life, and even provide recovery.
In 2015 when a new setback with concerning symptoms sent me back to the ER, I was told to see a neurologist. Since my original specialist was not available, I obtained an appointment with a neurologist newer to the institution whose specialty was multiple sclerosis. By that time, I had also spoken to a family friend who is a neurologist and who insisted that I needed a lumbar puncture.
I saw the new neurologist on a day when I was able to leave the house and tried to convey the urgency and severity of my symptoms. She reluctantly performed the lumbar puncture. Later, my PCP allowed me to read the note she received from the neurologist, which essentially suggested that the problem was psychogenic – essentially “all in my head.” I felt like I had been punched in the stomach when I read this: it sucked the air out of me. “Do not go back to that neurologist,” said my PCP. So, I mean “in my head” in a very different way.
I recall the NIH ME/CFS conference where I heard specialists speaking of ME/CFS as “brain-centered,” “autonomic dysfunction,” and “immune-mediated brain dysfunction.” The DNRS method treats the illness as a dysfunction in the limbic system, a very primitive part of the brain. The dysfunction leaves that part of the brain susceptible to an involuntary trauma pattern in the neurocircuitry, particularly an overactivated fight-or-flight response of the sympathetic nervous system, which overreacts to stimuli and exertion (Hopper, 2014).
(From Dr. Jay Goldstein MD, to Andrew Miller PHD, to Lucinda Bateman MD, and Mary Ackerley MD, and most recently, Angus MacKay, many researchers and doctors have proposed that the limbic system – which links together the endocrine and autonomic nervous systems – plays a significant role in ME /CFS. Cort)
In ME/CFS, case reports suggest that the insults that can cause the injury are varied: a virus, a bacteria, mold or a chemical toxin, or physical or psychological trauma. In my case, the insults were multiple and cumulative over time: they include a virus, a concussion, and gut microflora disruption.
The fight-or-flight response is a reaction that our bodies use for life’s emergencies, and produces a particular set of neurotransmitters. However, if the switch is overactivated and a person becomes “stuck” in this state, the neurotransmitters like cortisol and adrenaline are overproduced and contribute to exhaustion, inflammation and damage to different body systems.

Christine’s recovery has been gradual but steady.
By learning how to block this inappropriate pathway to the fight-or-flight response and rewire the brain away from this injury, my body was able to gradually return to a state of equilibrium. The DNRS method was powerful in teaching me how to reinterpret what was going on in my brain, and then to block negative pathways and rewire my brain, so that I learned to change my body’s response to triggers and gradually restore my wellbeing.
Treatment Takeaways
- Craniosacral therapy, Clonazepam (initially), and, in particular, a fecal transplant, helped.
- Annie Hopper’s Dynamic Neural Retraining System was the key, though, to her success.
- Her program was slow but steady. A year after starting the program, Christine was able to successfully run again. Eighteen months later she reported that she travelling freely, taking hour-long walks without incident and rarely needs to use the program anymore.
- She stated: “I credit the Dynamic Neural Retraining System with the huge shift in my body that allowed me to reclaim my life. In my autonomic dysfunction, it directed my responses away from the overactive sympathetic nervous system ( fight-or-flight) that had created a state of chronic inflammation, and it boosted the parasympathetic nervous system. (rest and digest) allowing for rest and restoration. A wonderful part of the method was that I was in control, so it felt very empowering.”
- She recommended the Wired for Healing, book by Annie Hopper, and the Dynamic Neural Retraining System. Check out doctors who recommend the DNRS here.
- Her advice – “Surround yourself with people who believe in you. Keep hope alive.”
I implemented the program in my home in late March 2018. It requires dedicated attention, and at the beginning, I did the training lying down.
My recovery has been gradual. Within a week of starting the training, I left home without the wheelchair for some brief outings. I gradually was able to tolerate noise in restaurants that in the past felt unbearable. I was soon able to walk outside again, and to go up and down the stairs in my house.
A year later, in March 2019, I took a run. Symptoms fell away as I rewired my brain to respond differently to stimuli and exertion. I found myself celebrating triumphs: “I walked around the block!”; “I drove to my daughter’s track meet, watched it and drove home!”; “I went to a loud restaurant and enjoyed a meal!” All of this had been unthinkable in the previous year.
In consultation with my doctors, over the year of implementing the training, I gradually stopped the 5 prescription medications I had been taking — Acyclovir after 5 months, Clonazepam weaned over 6 months after 3 years, low-dose naltrexone weaned after almost a year taking it, glutathione and methylfolate, after taken for a few months.
I no longer take any prescription medication, though I continue to take magnesium glycinate, vitamin D, metamucil, probiotics, and senna as needed. I understand that it is possible that all the medications I took along the way altered my physical chemistry to allow my body to then respond differently to exertion. But I am also convinced that without the DNRS method, my brain would still be stuck in a pattern of overreaction.

People who get well or improve greatly from ME/CFS do so in a wide variety of ways. For Christine, the DNRS program has been the ticket.
I have been so incredibly fortunate to have the unwavering support of my spouse and two daughters, and a wonderful community of friends and family around me. They all celebrate my return to fully participating in life, after years of needing to shield myself from most stimuli and exertion. For this, I am so thankful, and I tell my story to offer hope to others.
(Christine’s Jan 2020 Update: I don’t feel like I have unusual limitations any more. I travel as I want to, including a 10-day trip with a 2-day workshop for health care providers in November. At the end of the trip, I took the metro home from the airport and walked the mile to my home with my luggage on my back. Then I just kept going. I think recovery now feels like the right word. Amazing!!! I am still so grateful.)
- For more info on Annie Hopper and her program check out Chris Kresser’s interview with Annie Hopper here.
- Have a recovery / recovering story? Don’t hide your light under a bushel! Please use the contact form to share your story (using your real name or a pseudonym) and spread the news. Recovery stories provide hope and new options….
Health Rising is not affiliated with the DNRS program in any way






I feel that I can no longer recommend this blog to fellow patients in good conscience.
It’s a shame because it’s been a helpful resource to me over the years—both personally and as something to share in the online patient communities I frequent. But I would feel too bad if, because of my recommendation, someone I knew spent money on DNR, or if they became disillusioned with ME/CFS research by this blog’s habitual overhyping of preliminary scientific findings.
Sorry to see you go, Jonathan. Let me point out, though, that the DNRS costs peanuts compared to most treatments that people try and Health Rising ALWAYS makes an effort to point out preliminary findings when they occur – which is most of the time.
Perhaps it’s the focus on a mind/body technique that disturbs you? I recognize that this is a difficult subject but let me tell you what drives me with regard to treatments: if I was to neglect something or dismiss something because it didn’t fit with my belief system or my idea of how things should go – and thereby denied someone the opportunity to get better – that would be awful. Just awful.
That’s why if someone has ME/CFS or FM and they improve significantly Health Rising will report it. In Christine’s case she clearly met the criteria for severe ME/CFS, had a diagnosed viral infection, and had a symptom presentation that fit.
If you look at the Health Rising’s Recovery stories section you’ll find many different kinds of recovery stories.
Thank you for the article.
Please hear me out.
People with ME/CFS are correct not to give limbic retraining programs a try (such as DNRS). The reason being that it is completely structured as a scam. I’m not saying they are a scam or even that they don’t work, I am saying the structure is wholly unethical.
ME/CFS is such a wretched, living horror of a disease, and so many people around the world dedicate themselves tirelessly to finding a cure, yet these programs claim to offer the cure and keep it behind a digital content paywall.
To me, this is truly sickening. Imagine thinking that you have the cure for ME/CFS and managing it in such a way.
However, I’m not just complaining without proposing a solution. There is a very elegant solution in my opinion:
Ashok Gupta’s limbic training program, for example, is available via torrent online (TPB).
Personally, I am trying the program out. And I swear on all the is holy that if it helps as the program claims, I will cut a cheque to them directly. From reading this article, I think hardly any patient experiencing such benefit would take issue with paying after receiving such benefit.
By any ethical standard, these programs should have a donation, and ‘pay what you can’ purchase model.
So, to be blunt, as has been asked on the forum before. If you have a copy of the DNRS program DVD’s, please make them available online. If you are not tech savy, send an anonymous reply to this comment and I will help you do it.
Good luck with the program but check this out – everybody unless they’re wealthy – has to survive somehow. I have to ask for donations not just to keep HR on the web but to pay for food, health insurance, etc. Annie Hopper’s program is not cheap for sure but it’s also not expensive relative to other medical expenses – and if she really wants the program to spread – she has to raise the money to hire administrative staff, do advertising, hire program leaders, etc. Would she be able to cover that with pro bono donations? That might be dicey. There’s probably a reason no one has tried that yet.
She’s really no different from a doctor charging for his services.
One thing I would hope some of these programs would do, though, is provide help for the many people with few resources…
I never comment but I must say DNRS made me significantly worse. I think it’s hogwash and extremely exhausting, causing PEM. I developed extreme Multiple Chemical Sensitivity because of the brain rewiring program even though it’s designed for stopping MCS. they wired MCS in my brain by focusing on it.
I highly recommend people avoid DNRS or other brain rewire programs.
Hopper’s program has several different options or pathways – there’s the chemical sensitivity pathway, the pain pathway, the chronic fatigue pathway and, I believe, an orthostatic intolerance pathway.
The focus of the program is to replace bad responses to chemicals to good responses and replace bad experiences with chemicals with good experiences. I don’t know how good the program is with ME/CFS but, as the doctors attest, and as many people have reported, the program does appear to be quite effective with chemical sensitivities.
Instead of replacing bad experiences with good experiences causing his alert system to ramp down and John’s awareness of chemicals to subside John reports he experienced the opposite. I imagine that The DNRS is not helpful with everyone with MCS but this is the first time I, at least, have heard of a negative experience like this
I started Annie Hopper’s DNRS on the recommendation of my doctor, but then concluded that it’s not appropriate for me. Subsequently I tested positive for Babesia. So if anybody would like the DVD’s and workbook (which, unfortunately, I have written in), let me know.
did you still want to sell the dnrs program?
Sure, aya.
@Tim (see comment below) I have had CFS for a little over a year now. I am so depressed and exhausted with trying to chase down remedies Anyhow, I noticed that you offered to send someone the DVDs and workbooks that you used from the brain recovery program. Is there a way we could pay you for shipping and handling if you still have the DVDs and workbooks? Please let me know if this is what you meant when you offered to share the DVDs with someone in need.
I plan on trying DNRS as I definitely believe ME/CFS/Lyme is a nervous system issue. I personally suggest neurofeedback if you have not done it yet. I bought a system and have been doing it everyday for 6 months and I am 97% recovered.
I had Lyme disease and was bedridden for 4 years. I did antibiotics, then moved to herbals, and tried LDN as well.
I pay very close attention to my gut, I eliminated gluten and dairy and soon will move to plant-based. I do yoga daily, meditate daily, and became a reiki master.
However, my biggest change came from learning about the epigenetic changes due to trauma/ptsd as I thought maybe childhood trauma had created a dysfunction in my nervous system- I basically would go into fight or flight at the smallest amount of stress which obviously messed up my hormones and the endocrine system etc.
I started doing neurofeedback for the brain fog from Lyme disease. Neurofeedback changes or trains the brainwaves in different areas of the brain. Once I started doing it, I decided to train the areas related to the amygdala and after 3 months of doing it I was able to come off of all medications.
So if you haven’t tried neurofeedback definitely give it a shot. I bought my system through brain-trainer.com but there are neurofeedback specialists all over and you don’t need to buy a system to do it.
That’s tremendous progress Lisa. Definitely need to look into neurofeedback. I’ve from others that it can be helpful. Good luck with the DNRS.
I too had CFS/ME. The WORST thing I’ve ever experienced.
Brain fog, fatigue, tinnitus, couldn’t walk, heart racing, post-exertion malaise.
I had to live with my parents for months as they tended my every need. From being a fit, healthy, 40 year old active secondary school teacher in Manchester in the UK I was struggling to stand up.
I started to chat to friends who had the disease – they were SO SUPPORTIVE.
But they were also so negative. They had been battling this so long it was terrible and they (understandably were very closed minded). I found no answers.
I started to research those who had RECOVERED. There are 1000s.
I found the website RECOVERY NORWAY (all not for profit) and LIGHTNING PROCESS (brain retraining)
I did the 3 day course and on the first day walked to the post box 🙂 within weeks of the exercises I was driving, chatting to friends.
Within 3 months I was back to work, jogging, cycling (which I love), cooking
I’m now 6 months in, full time work back at school, better every week. Full and active life.
I’m so happy you SHARED you’re STORY and CONGRATULATIONS.
After experiencing such horrors, I’m both totally understanding and equally baffled why so many people are so quick to disregard you’re success.
Well done and wishing a positive future to all xxxxx
@Cort – is there any way of finding this Ellie who posts below at “Ellie on May 16, 2021 at 12:46 am” – I’d love to know if her tinnitus disappeared also
I agree with David somewhat (not about the overhype, as I see that as hope, and hope is so important) However a pay-wall system for a mind therapy treatment sounds like those corrupt folk selling the ‘Lighting Process’.
If we had 100 patients all saying this works wonders then I’d be more interested. But one person with a history of previous good remissions and then severe relapse isn’t really even anecdotal, as she maybe just in remission again. Her ME/CFS didn’t even sound normal to me as the remissions and relapses were extremes. Most ME/CFS people (95%) I’m aware of have an onset and no recoveries, their remissions that happen are only slightly better than their normal baseline bad, and relapses are regular.
As for those that do well with mind therapy I wonder if these people had a condition that gave them a type of chronic fatigue and it became behavioural and habitual, so yes then a mind therapy process may work.
But a real ME/CFS patient who we know has massive unusual immune gene expression after exertion, unusual under utilised oxygen uptake in cells, stiff red non-deformable blood cells, and cells proven with the ‘Nano-Needle’ experiments to be in a state of exhaustion / hibernation, highly likely isn’t going to be cured by mind therapy.
The author putting a paywall on the therapy is appalling. If I found a way to help people with this vile disease there’s no way I’d charge vulnerable desperate sufferers.
For the record I’ve read a transcript of the other mind therapy the ‘Lightning Process’ and it definitely would trigger PEM to real ME/CFS suffers if used. I can’t say I know whats involved in this ‘Annie Hopper’s Dynamic Neural Retraining System’ but I can’t see how ‘thinking’ is going to change immune gene expression, red blood cell deformability, and cells trapped in a hibernation state, etc
All that said I’m still an avid fan of HealthRising and am surprised only 80 people donate. Yet thousands benefit from the hope it gives! $5 or $10 each from the many would be well worth it for the goodness this site brings us!!!
You make a good point about benefiting from Healthrising yet not donating at all. I have been guilty of this. As typical of most sufferers over the years I have spent incredible amounts of money (when able) trying to find relief. I appreciate the information here and the efforts to put this together. Especially Cort’s work which I can’t even fathom doing at this point. I dont have alot but I am making a small donation in thanks for having a place to get information and hear the thoughts of others. Thank you.
Thanks Sue – appreciate it in the midst of this rather tumultuous topic:).
I agree with the view of thousands benefit from HR free of charge despite the huge amount of work that is goes into producing it. I say this because of the hideous struggle that is my daily life with ME/cfs. HR has become my friend in a way, it gives me hope and something else to focus on with my recovery. A large number of us are completely isolated with this illness. We have lost friends, jobs, even family because of it. This is why I am making a regular donation, small but insignificant compared to the relief and comfort I get from reading it, and I have even taken some articles to my Dr to discuss and try Treatments based on it’s findings.
As far as the whole “re-wiring” programs available… I do feel like they are slightly taking advantage of the desperation that comes with this disease, but any hope is a help. I say this because I do believe that ME/cfs has its rotten hooks deep in your emotional state and by softening that grip, by doing something that gives hope, that you are in control of, that you can do daily to give you hope (even if the actual program doesn’t do a lot) is the an important part to the recovery journey for us all, regardless of our individual cause of sickness, we all share the emotional part of this evil illness. There is not a lot we are capable of doing to treat ourselves that is not another “blind-shot” medication. So yes these re-wire programs might be hyped up “promises to cure” to make money, but we all can make the choice for ourselves to use them or not. But if we feel it helps us personally, that’s our decision. We just need to have it in perspective.
Whew!! That took me 3 hours to write.. got to close my eyes to recover now. Lol
I have to agree 🙁
Nobody would recommend this a HIV patient, and ME is also a infectious disease with cluster outbreaks worldwide. Nobody would believe this healing a HIV patient…
Anton, please provide some proof — any proof at all — that ME is ‘also an infectious disease’.
Marcia, there is a tremendous amount of evidence of ME/CFS occurring in “outbreaks” which points to infectious disease, in the absence of some sort of massive chemical leak, nuclear explosion, contaminated water, etc. Dan Peterson has kept a comprehensive database of his patients, originating with the outbreak in Tahoe decades ago. I’m sure there is a great deal of evidence among many ME/CFS Specialists that has historically pointed towards infectious disease; the challenge has been identifying a SINGLE pathogen causing the disease. Thus, a paradigm shift is evolving in that multiple pathogens appear to be capable of causing post-viral syndrome. The “long haul” COVID patients who are developing a condition that meets the criteria for ME/CFS is further evidence of this new paradigm.
Katherine, just seeing your r eply now — three years later. If the outbreaks you mentioned featured thousands and thousands of people in each area, that would make the hypothesis plausible.
The fact that there is indeed no single pathogen, nor will there ever be — after decades looking down that rabbit hole — also proves it’s not infectious.
The key is asking yourself — what ELSE was happening in the years prior to getting sick. Sometimes, or even often, decades before getting sick. Why are almost ALL ME/CFS patients more likely to be sensitive introverts, rather than outgoing extroverts? Or why are they perfectionists or people pleasers? Why do they so often put everyone else first instead of themselves?
Answer those questions in your case and you’ll find the things you need to address.
It’s also worth noting they’ve found a trauma connection to long-covid cases.
Christine,
Thank you so much for sharing your story.
Cort,
Thank you so much for publishing Christine’s story on your blog.
Many parallels exist between our journeys Christine.
I too was exposed to a ?.
I too acquired a secondary bacterial infection, C Diff that was resistant to a plethora of antibiotics that treat C Diff.
I too had an FMT transplant.
I too had my C Diff go into remission. No trace of the pathogen ? to this day last three times tested.
I too finally embraced functional medicine and limited my prescription medication.
I too am focusing on nutrition, supplementation, and adopting a wholistic approach to healing, both mentally and physically.
I too understand the significance of neurotransmitter health and how it drives our debilitating illness: specifically Dopamine, GABA, and Serotonin, Epinephrine and Norepinephrine to a lesser degree.
I too have suffered from mTBIs and concussions.
I too have been tested and found to be positive for HHV6.
I also tested positive for Varicella.
Mixed results but the fight continues!
I too have had extreme tendon reflex issues which I am currently working on in a plethora of treatment approaches.
I too have experienced the weirdest sensations along PNS nerve pathways. Everything from ice water running down my skin, to numbness, to tingling- to PSI like pressure.
I too have experienced extremely painful skin rashes. So painful that even clothes brushing the area hurts in the most painful alloydinic way.
There is one huge distinction between our parallel journey.
I have had leukocytosis for over a decade now.
My WBC hoovers around 14,000.
I think this is due to the way my ? processes the fight or flight response and the parasympathetic and sympathetic in action.
The ? for me has been using a three pronged target ? approach to combating my illness. ? the ?, the gut, and the immune system.
Not sure if I want to lower my WHC count because I’m pretty sure my immune system is in a constant battle with a dormant pathogen ? rather than a battle against a perceived autoimmune antigen or hidden inflammation.
I would love to hear this community’s thoughts about what they think it is that I am battling, any parallels they may be experiencing, and any qualitative and quantitative input that can be beneficial in understanding, combating, and troubleshooting this disease.
Christine’s account reminds me of what I perceived early in my own journey with ME, and that is it appears to me that there are many causes of ME. so why not many pathways to relief, at least some relief? For some, that never happens, for others it happens profoundly and many fall somewhere in between. I’ve been helped by K PAX Immune Support and the way it addresses mitochondrial fatigue, and I found it doing research on the mitochondria. I believe that many with ME the basis is mitochondrial malfunction.
Glad to hear about KPAX! They recently did a successful Gulf War study if I remember correctly – it’s on my list of blogs to do. 🙂
To those who think DNRS made them worse. The process shines a light on the emotions behind decisions. AS this happens, yo have a choice as to accept this or RESIST this awareness. Just like with a bowel movement, if you resist it, it will get worse.
You made my day..lmao!?
On that note laughter is great medcine why humor is my coping meck ??
No one thing helps everyone with ME. If DNRS helps some, more power to them.
I’ve done the program it works. Thousands of people have recovered. I find it repulsive anyone who says it didn’t work. You obviously didn’t do it. The brain has no choice but to change if you do it correctly!
Thanks Matt. You speak the truth.
It’s actually common sense. I remember a thread over on the “Science” for ME site, where patients were discussing how they’d keep doing some activity that they KNEW would result in a crash, but ‘couldn’t stop’ because they knew they’d crash, so they kept going…and then crashed even more so.
It’s not about this bug or that one, as the case above shows. 97% of all humans have HHV-6 yet only a tiny percentage get sick from it.
It’s about the brain. Brendan Rob above says ‘if we had 100 patients’ that recovered using brain retraining, then maybe he’d take it seriously.
Well, I suspect there’s far, far more than one hundred who have indeed done just that. On the youtube channel for DNRS alone, there’s probably 2 or 3 dozen. And there are so many more programs than Hoppers out there…
I agree with Jonathan. People suffering from health issues are a vulnerable group. I tried the DNRS program by Annie Hopper and it felt like a completely overhyped product that is NOT worth the money.
The are better options available for a fairer price. I’m totally skeptical of articles like this, as I’m sure they are sponsored by Retraining The Brain somehow.
For people thinking about using DNRS, please read My review at http://www.bloomingturtle.com
It breaks down what the program is, and offers a way for you to create your own “retraining” program. The page was created specific to help people looking into the merits of “retraining”. I don’t make money from the article, and am not affiliated with any company.
Just so you know Angie Health Rising is not affiliated with DNRS in any way; it is not sponsored by them or receive any funding from them.
You may be skeptical because it didn’t work for you (although you only tried it for a month) and therefore you can’t imagine it working for anyone else. I haven’t received the benefits that the person in this story did but it did work for her and it’s worked really well for several other people I know. It has also not worked for other people, I know.
This pattern – where something that works for someone doesn’t work for others is not unusual at all – in fact, it’s very common. It doesn’t mean a program or treatment is bogus – it means ME/CFS is a heterogenous disease in which different things work for different people.
Unless you actually tried the program for amount of time it’s designed to work it’s hard to assess your experience with it.
By the way, the “click your heels and the pain disappears” description in your blog of the DNRS doesn’t help it or your argument. It simply makes you seem like an angry person.
In reply to Cort Johnson’s response to my post:
In my blog post, I didn’t say that DNRS’s strategies don’t work. I said that It’s pretty much the same program as another program that I took, Curable Health App, which did work, and was better priced and more engaging.
I apologize for the suggestion that you are affiliated with DNRS.
My post was about how DNRS was overpriced for the value delivered. I didn’t say that it wouldn’t work for people, only that there are other options out there that cost a lot less, and more enjoyable to use.
If I do come across as angry, that’s because I am somewhat. Angry about the way that vulnerable people in pain are overcharged for things that can help them. This include many practitioner’s of New Age Woo. But thank you for your feedback. I didn’t realize I came across that way. I thought it was more of an attempt at a kind of sarcasm. I will have to re-word things.
Even if you aren’t affiliated with DNRS, you probably have some vested interest in keeping well known healing techniques a secret, for whatever reason.
All I’m doing is breaking down what these techniques are, so that people can be helped without spending more money than they need to.
So, yes, DNRS does work, but it’s techniques aren’t revolutionary or proprietary. If you think they are, then my interpretation is just that you are seeing stuff in DNRS that isn’t there.
My blog article is for those looking for potential DNRS counter claims so they can make an informed choice.
Since DNRS has no Google or Trust Pilot reviews ( which they should), I thought I’d post mine on a separate website. I needed to add a lot of text and images so that it would show up in searches.
The wizard of OZ analogy is meant to show another version of Annie Hopper’s graphics on how to heal. But perhaps you are interpreting it differently.
My critique could be viewed as just some angry person venting, or it could be interpreted as valuable information that can help businesses improve their product. All negative reviews online are kind of like this, though mine is just much longer.
If you look at Annie Hopper’s “Wired for Healing” book reviews on Amazon:
https://www.amazon.ca/Wired-Healing-Remapping-Mysterious-Illnesses-ebook/product-reviews/B00WYPXHKO/ref=cm_cr_dp_d_show_all_btm?ie=UTF8&reviewerType=all_reviews
You will see that I’m not the only one who sees DNRS/Annie Hopper this way (overhyped). And that it’s the negative reviews that people are finding the most helpful, not the positive ones.
You should have seen a LLMD (Lyme-literate Doctor) and had a Western Blot test done through Igenex, and been tested for Lyme, Bartonella, Babesia, and other co-infections. I have a very similar misdiagnosis story (and I had c diff twice), I was misdiagnosed with Multiple Sclerosis by 4 neurologists for 7 years — I really have Lyme and Bartonella. Your symptoms and history just scream Lyme. “CFS” is the most common misdiagnosis for Lyme and co-infections.
I’m not surprised at all and I expect to hear of more recoveries using this kind of treatment.
Cell Danger Response is a mirror of a mid-brain danger response. Slow wave sleep is disrupted and a snowballing situation occurs where the sufferer is kept in a physiological trap….probably many of them. Gut, fascia, muscular and immune issues are downstream of what’s occurring at the brainstem level.
Thanks for sharing your story Christine, and thank you too Cort for steadfastly remaining open minded and curious.
How about an interesting analysis of both Hopper and Gupta programs by a third party who uses both? This is a long but very enlightening article. It gets down to making new pathways in the brain so it reacts differently to improve our health.
https://www.holistichelp.net/limbic-system-retraining.html
Thanks for sharing that article, Laura – it sure is a long read, but I have bookmarked it and will finish it as I can!
Hi Anne,
That’s a really interesting theory a mirror from a macro systems level to a micro- cellular level. Where did you read about that?
It’s psychoneuroimmunicological
It is in the head but it ain’t
just psychological
My poem. Feel free to use
Deborah Foster
?
DNRS as well as the Gupta Programme have helped me immensely.
Thanks Michael – can you say how your level of functioning has changed?
I want to point out that Health Rising will never – until there’s some large clinical trial – say “X” is the way to go. The reason for that is that ME/CFS is clearly a large, very heterogeneous disease. Nothing is going to work for everyone. I imagine that the best we can do is to find something that will regularly work for a subset of patients. Then we find something that will work for another subset of patients.
Unfortunately, that leaves us with the option of trying many different things and hoping that something works – a costly approach. I don’t think I’ll ever forget seeing a functional medicine doctor stand up at a workshop and saying to the effect of “we don’t know what we’re doing; all we know is that sometimes what we do works and we don’t know why.”
What exactly does this DNRS have you do? It’s it meditation? Interrupting thoughts? Proper resting? Exercise?
Blog posts like this are always so almost secretive/go buy it and you’ll find out! Come on – if it can really help, share the knowledge!
Explain at least a lot more about what it is and has you do beyond “it rewires the brain”.
If I can try something for free and it gives a bit of improvement, I’m willing to look into it and maybe buy it, but I am so very much done with just trying anything and everything that could possibly maybe help me because it helped one single other person. Who in this case had very different symptoms. Happy for her that she can live again! But this blog was not very helpful in a practical way.
🙂 I can’t give away Annie’s program! It’s her program – she developed it, probably patented it but I can say that it is not meditation, and that it tries to tone down what Hopper believes is a hyperactive limbic system and over-active brain-based fear response which is causing the brain to blast out cytokines and cause neuroinflammation, pain and fatigue at the slightest hint of a threat.
It’s actually quite simple; it involves mindfulness, focused attention and a mental process using memory designed to rewire – i.e. return the brain to a settled, healthy state. I think the video’s are helpful in that they kind of reinforce the process and get people enthused about doing it. Given that it’s probably going to be slow going and take months to be effective, that kind of boost is helpful.
I don’t know if she has a money back guarantee or not. It’s been a while since I tried Ashok Gupta but as I remember he had a similar approach and I believe he still has a money back guarantee.
That’s a big red flag when participants aren’t allowed to discuss a program. Business, religious, health or whatever the case, if it quacks like a duck it is probably a duck.
I just googled ‘Annie hopper dnrs scam’ and once you get through all the testimonial sites, you’ll find a blog that actually tells you what the program is. It’s basically changing thoughts and behaviours to deny you have an illness. And you also do a little dance and chant some words.
I mean, it sure sounds stupidly unbelievable to me and maybe I’m the idiot to accept this description which may well be false. But I can’t find another source for what it actually involves so I’m forced to accept the one result out of three pages of google results that contains any actual detail.
Well – that is not the course I did.
It is emphatically not about denying that you have an illness.
If you want to know the different practices the course derives from simply go to the website and check them out – https://retrainingthebrain.com/how-the-program-works/
I will say that if you do this and start one part of the program you’ll probably look over your shoulder for fear someone is watching you :).
Do you really think, though, that Christine was able to go from being wheelchair bound to travelling freely, going on long walks and feeling totally recovered by doing a little dance, clicking her heels and wishing upon a star? Obviously not.
It took a lot of serious work. All this kind of stuff does. If you’re not willing to buckle down and put the time and effort in – don’t even try this stuff. For one thing you’ll fail and for another, you’ll blame the program (while not doing the program). It’s not an easy program. If you’re going to do it – then do it fully for six months – and then come to a conclusion.
Thanks for clarifying that this is not what the program involves. I don’t plan on doing it but my support group has a copy so I might take a look for curiosity’s sake.
I just think, like others, that a person prone to going into remission now and then might not be correct in attributing their success to specific things. There are probably many other factors at play here. I don’t doubt that his person recovered, I just hold high skepticism about DNRS being worth consideration for a vast majority of PWMEs.
You bring up a good point. Christine has had remissions before. Let’s hope she stays healthy. I have the feeling that she’s being careful.
Nothing the matter with skepticism…Until we have studies we have no idea how many people can significantly benefit. I tend to think that because this program involves stress reduction that it could be at least somewhat helpful for many. Recovery is far more difficult.
I would like to know some idea of what the program entails so I know if I am capable of even using this method prior to committing to that high of a fee. Can anyone explain a bit of what you have to do each day?
The DNRS program involves a very small bit of walking like 20 steps and standing but as Christine notes she started it lying down. Other than that it’s all mindfulness practices.
Thank you Michael
Hey Cort, sorry I can’t seem to be able to reply to your comment above. Just wanted to say God bless you for funding HR via donations. I’m sure it’s not easy, but it is damn noble. Many patients simply don’t have the resources, including myself. It is such a terrible tragedy, but it’s to be expected in any situation where people can’t provide for themselves financially that they will already be spread very thing.
In my opinion, the program would spread much further if it were cheaper, doubly so if available for free. The marketing dynamic in my opinion is inverse to the product’s price. Take a look at artists who offer their music for free to gain exposure.
You can justify the program’s cost to pay for staff, by not to justify accessibility. This is why a high price tag for digital content is a red flag, usually the only business model that requires it is taking advantage of a susceptible few that’ll get drawn in by marketing (not saying that’s the case for these programs, just in general).
There’s no question Hopper and her staff need to make a living, but charging desperate patients for digital content, which calls almost nothing to distribute, and very little to produce, is not the way. I’m sure many patients who see benefit from her program will donate, and that she can make a fine living from her reasonably priced books, workshops and one on one services if indeed the program is so beneficial.
I would truly like to see DNRS available for free.
Surely people have $1 or $2 or $5 or $10.
I’m on a tiny disability allowance and I’m debt but I still chipped in a tiny bit.
There’s a lot of people benefiting by getting hope from HealthRising yet only 80 people donated!!! That to me is wrong, even the poorest of us can spare a few dollars once a year.
Just imagine no Health Rising = no hope. No knowledge how to talk to our doctors or disbelieving friends.
Thanks Brendan. Actually more than 300 people have contributed during the month long drive and the response has been good – a big thanks to everyone who’s done that. 🙂
Nope not all of the poorest of us can spare a dollar or two. I’m on a tiny disability check, constantly in overdraft mode and drive an ancient vehicle (when i am able to drive 1/4 mile to the grocery store and spend at most 20 minutes grabbing some necessities then getting back home before I have to sit down on the store floor, which has happened). Please don’t speak for everyone. Each of our lives is different. Never had issues knowing what to say to doctors. I’ve typically at first allowed them to try to figure it out going just by my symptoms. They love that.
I enjoy HR when I am able to come here.
It certainly would be nice if it was cheaper but the cost is similar to other programs of is type. Gupta’s Amygdala Retraining Program is more expensive and Dan Neuffer’s program is around there as well.
Would a cheaper program get more sales and provide more benefit overall? It would be nice to find out
I heard Dan Neuffer say that he tried offering his programme for free but then he thought it wasn’t taken seriously.
Cort, thank you for the many options you present. We never know what might be the key to some level of improvement.
Thanks Cort for all the articles you post?
The take away from all the articles is to keep an open mind..try it or not..is a personal choice and decision..it either works for you or not and a little benefit is better than none at all but you gave it a go..
Thanks for always keeping it real, Cort!
I am very grateful and Many thanks to Jennifer Brea for her courage and shedding light on this devasting disease that has been overlooked and hidden for to long..
Stay Strong and Never Give Up All and keep the hope?
I’m pretty horrified that the program costs $249.95 (I kid you not…she couldn’t just make it $250?) upfront, and that the book (which also costs money) is reported to be one long infommercial, without enough actual information to help anyone. This is the “scam” structure that David is talking about.
I would NEVER buy something presented in this way, and, Cort, honestly, you should not help to promote it. I find it very upsetting that people are manipulating and using the patient population in this way. As David says, if this treatment actually worked, it would spread like wildfire if it were more freely available, and the thousands of patients who would benefit would easily donate enough to make up the difference. Plus, the provider could then publish inexpensive books supporting the program that would sell in the tens of thousands, making yet more money. But that would require a program that actually works, and so the fact that the whole thing is behind this kind of paywall makes me seriously doubt it and means that I will never consider it.
David, could you help those of us who are less tech-literate to access the Gupta program? I am curious about the general approach, based on Christine’s experience. All previous accounts I’ve heard of this approach sounded like they risked huge setbacks from PEM (when you fool yourself for a while that you’re able to handle more activity and then crash massively), and maybe this has the same dangers, but Christine’s description made it sound pretty safe to try. Do you think Gupta’s is safe?
Note: When I say I will never consider it, I mean I will never consider paying in this way. I am curious about the approach, if it can be made safe, because I’m chiefly interested in non-drug-based approaches. My big concern is safety and not risking a worsening of my condition.
Agatha I agree with every word. I will never consider paying in this way, just like you said. And very good info about the book, I didn’t know that. Btw from what I heard this video By Dr. Hart explains the method quite well:
https://www.youtube.com/watch?v=pmP7mtaFyrc
I honestly don’t see how this program – with one exception – could make you worse. It does not involve pushing through stuff. Instead it tries to build a base in which you can naturally do more.
If anyone tries it, though. I would caution them to take it easy during the first day or two or three when you’re requested to do the program a lot. At that point you can surely overdo it and I did…
It seems clear that those who are shocked by the structure have never been involved in running a lifestyle business. My wife is a very gifted life coach and people who have worked with her openly testify that it has been life changing. Working hard with a good coach can save your mental health or your marriage, and so many relationships.
On the other hand, anytime that my wife has given coaching away for free or for cheap, the results have consistently been underwhelming. It is hard for my wife to feel like she has something life-changing to give someone and money is in the way. Unfortunately, for many people (not all), the commitment to spend the money seems linked to the commitment to the work. It is something we’ve heard from many coaches but didn’t get it until we saw it with our own eyes.
All the marketing “tricks”, the payment plans, the memberships, the not rounded prices, actually help the client. There’s a reason people do it, the scammers and the legitimate programs alike.
My wife does happen to give away a lot of content for free because she knows that thinking people realize there is more to working with a coach than free information you could find on the internet. But why reject a program because of the structure of the sales page? You may disagree with her business coach or philosophy, but why discredit first hand reports of people seeing improvement?
The sales page isn’t an indication of the authenticity of the program, only the program itself is. I am planning on purchasing the program because honestly, I spend $250 on groceries for one to two weeks. I don’t think it’s a big investment at all. If it were a vaccine or special cure, you’d be on causematch raising the $80,000 you need for a dose.
I do Landmark Education programs. They said when they tried giving the program away they got the worst results they’d ever had. People just have to have skin in the game to really commit to doing something difficult.
Actually, the program seems to be doing quite well – she seems to be adding staff regularly.
I don’t think that this or any program like it will ever spread like wildfire and the reason is that it’s darn difficult! My experience is that it takes a lot of time and effort and it works quite slowly. I’ll bet that most people will have trouble investing the time and effort needed for it be successful in the six months Annie asserts the program should be done. I did. Even after being happy with my progress I fell off the wagon when circumstances intervened.
This is not like a take a pill and get better. This is like mindfulness boot camp. It’s a lot of work, sometimes rather dreary work. You go up and down – sometimes it didn’t appear to be working – and then some surprising progress would occur – and then it would be back to plodding away.
The $250 might actually be a pretty good incentive to really buckle down and do it.
Cort, are you saying you did the program and are now cured ?
I’m afraid not. I did it for six weeks or so, received some benefit then let circumstances intervene and fell off the wagon. One interesting benefit – my experience of nature was enhanced quite dramatically. I am going to give it another go shortly.
I agree. I use the gupta programme and find it a life saver. It’s definitely not a quick fix and involves a lot of persistence. I think actually if I’d found it for free, I mightnt have given it the commitment it needs. And it’s not just the programme itself – I find the Facebook group that goes with it is a really important support for motivation to keep going.
Yeah I think it’s a scam.
I think Christine just happened to be in remission again when she tried it, wait a few months or a year and she’ll most probably relapse (I hope not as I don’t want her suffering)
But I bet she won’t be given a refund when she does. She definitely had unusual massive ups and downs compared to the average ME sufferer. She was even able to run with her condition prior to mind therapy!!! To most of us that’s a dream. Running with MEN is not possible without PEM. She’s got something else going on.
I guess you see what you want to see but I, anyway, didn’t see any evidence that Christine was in remission. She was kind of at the bottom of the barrel.
Then she started the program and began to see results. You can twist yourself into in all kinds of knots trying to come up with an alternate scenario’s – that seems to happen a lot when stories like Christine’s come out, but in general I would go with the most logical scenario which is simply what she said happened: she started the program, began to see results and it slowly worked.
With regard to the she didn’t have ME/CFS?. I don’t know how typical or atypical Christine is but I do know that some people got hit by issues (infections, a concussion) which slowly chipped away at their health. Each time it took them awhile to recover from whatever happened. If they got sick they tended to really get sick. If they got food poisoning it tended to drag on longer and at some point their health collapsed, there was no recovery – and they had true M.E. That sounds like logical, if perhaps not typical pathway, to me.
Note that Christine was unable to exercise at all and eventually ended up in a wheelchair, hypersensitive to sensory stimuli – and that her relapses tended to be triggered by physical exertion. What other disease does that occur in? That sounds very much like an M.E. state to me – and as she noted, she was diagnosed with it by an ME/CFS expert.
Agatha, I tried the Gupta approach in 2014 when I had been ill with ME/CFS/FMS for 10 years and was spending most of my time in bed. My husband was planning a 6-month jaunt around Europe upon retirement, and I wanted to go with him. I was genuinely afraid I was unable to go, almost sure of it. But the prospect of remaining at home without him was equally scary. The Gupta program helped put me in touch with what I wanted (which was to go) and allowed me to consider that I might be perfectly fine pursuing this at-the-time-seemingly-outrageous activity.
We made concessions–staying in airbnbs with kitchens, staying in places for a month instead of hopping around like normal tourists, allowing me to stay in bed as much I felt I needed to, etc. And I went, and I’m so glad I did.
The Gupta program helped open my mind to possibilities that I had categorically ruled out. I was able to act on my own behalf from there. On the trip, I still spent half the time in bed, but in the afternoons I could go out to museums, etc. And occasionally we’d go out to a play at night or out to eat.
This disease is certainly real, based in physiology. However, at least for me, part of what it brought was a mind-trap. I was so beaten down by such horrendous symptoms for so long, I had ceased to even consider that I might be capable of reaching for happiness. Through mindfulness or thought training, paired with some easy physical movements, I could envision myself as able to get on that plane with equanimity. And I did. I’m very thankful I went.
These days I spend mostly in bed, going out once a week or so to the grocery store. I’m unable to sustain upright activity for very long without really feeling ill in all kinds of ways. That hasn’t changed, and I’m certainly not cured. What perhaps remains with me from the Gupta training is being able to envision myself as healthy and happy. Mind you, I don’t summon up this image very often, but I do feel supremely blessed in my bed, able to rest.
The problem is they claim they are curing people with this condition. They aren’t. I have severe ME and take care of three kids. I’m sorry you convinced yourself you couldn’t do normal things, but the program is clearly trying to sell a cure.
I use tools to do the things I need to do and lots of rest. Wheelchair and feeding tube. I don’t need a guide to tell me how to modify my life and if thats what people need I can help with that for free. You don’t need a 250 dollar program. Just an experienced disabled person (I have been sick pretty much my entire life with ME).
Yes, but Samantha several people have reported that they have been cured using this technique. Will everybody? Obviously not.
Unless you have training in the different disciplines that make up that program I don’t see how you could replicate it”.
I am doing a free 9 day brain rewiring course. I just found out today on day three that the entire course would cost $4000!!! So, Annie’s is a steal!
I say to all of us not to put Cort down or expose him to undue stress for reporting whatever to us. I am sad that if this program does indeed work that it is not available to all of us immediately. I would send up flares and report to all of us. Making a living is one thing but, having any answer to this horror we all go through should be available to all of us with love and hope. If ANNIE is right, she would be amply rewarded. Share any information to all of us. Sincerely, hipjaven@gmail.com
I had to stop reading this blog – it jumps all over the place as far a timeline and is impossible to follow and I’m not even having a brain foggy day. Maybe a list of points of what she tried and when would help….
Also, with ongoing major diet changes, LDN, and whatever else I missed, how much of the improvement does Christine attribute to DNRS?
Check out the GIST and Treatment Takeaways for some quick takes. While she tried a lot of things only a few actually helped. LDN was not one of them actually. A fecal transplant helped but it was after that, I believe that she fell apart.
All of her major improvements occurred after she tried the DNRS. After it proved helpful she was able to get off all her drugs except for some supplements which she continued taking.
I have looked into DNRS before, mostly out of curiosity as it was being peddled as a miracle cure & I had not heard of it. I was not impressed.
DNRS, along with similar concepts like the lightning process both recommend that you cut people out of your life if they are not supportive of ‘the treatment’, or if they ‘perpetuate illness beliefs’ (which in this case means the belief that the person is ill). This is a massive red flag for me.
I don’t dismiss the improvement that Christine has had, and I am glad for her – but that doesn’t erase all of the problems there is with the concept of DNRS, as well as the fact that she was seemingly trying different treatments alongside.
This also is not solely a CFS/ME treatment. It has almost 50 different illnesses and health issues listed as things that it can cure – all of these things are not going to respond to the same treatment. It’s illogical.
I think that it is also worth pointing out that the 5 day seminar costs over $3000. They also highly recommend utilising their telephone coaching system which will cost you over $100 for 70 minutes – this is on top of buying their $200 ‘instructional video’.
Like I said, I’ve taken the DNRS – and I can tell that you haven’t as
I never came across anything like that. For one thing Hopper is not focusing at all on belief systems. If that was the case she would ask you to bull through your illness. Instead she’s trying to replace the wiring that’s causing your brain to spit out cytokines and keep your system on alert.
If you ever read Annie Hopper’s rather horrific personal story of chemical sensitivities – and I suggest that you do so before spreading more false information like this – she encountered plenty of bias and prejudice as she struggled with her horrific chemical sensitivities. She would NEVER suggest someone with these illnesses is not ill.
Actually given that the DNRS is attempting to rewire a part of the brain involved in sensory awareness, the autonomic nervous system, the HPA axis, the immune system and the emotions I’m not particularly surprised at some of things Hopper asserts it can help.
Again – if this program works or even helps – it’s a heck of lot cheaper than seeing a doctor. While I wouldn’t spend $100 on coaching the fee is actually quite low compared to fees from other life coaches, etc. I couldn’t afford $3000 either, but I just saw that Dale Carnegie charges $1,995 for a 3-day program and another $1,995 for an 8-session seminar.
The program has a list of medical doctors who have publicly endorsed it by the way – https://retrainingthebrain.com/what-doctors-have-to-say/
I did Hopper’s dnrs program for eight months. It helped immensely with environmental sensitivities.
I had to quit practicing when s family member had healthcare issues. I’m back on the program and feel it’s helping me cope with caring for my loved one.
If you think DNRS is a scam, you can try reading one of Doidges books on neuroplasticity. He does a good job of explaining how the brain can heal itself. I’m so glad I spent the three hundred on the program.
I agree that the seminars seem overpriced. On the flip side, there is a money back guarantee on the DVDs.
The best way to heal is to keep trying new things,at least that’s been my experience. Good luck.
Yes, I’ve heard Norman Doidge speak on a video online. He’s very encouraging about improving brain functioning.
If you google ‘Norman Doidge skeptic’ or something similar, you can find articles highlighting how his later works go way outside the bounds of science and into quack territory.
I was a huge fan after reading The Brain That Changes Itself (I think that was the title) but after reading some analysis of his subsequent works it seems his ideas and stories lead to us all getting carried away with the concept of neuroplasticity being some kind of miracle. However, just like the gut microbiome hype of the last 5-10 years, it’s probably going to be just another tool in the toolbox and not some world changing method that will enable direct targeting and resolution of most maladies known to humans.
Time will tell. My guess is that these techniques are going to be very effective for some, moderately effective for many others and not effective for a significant subset. For one thing they are just too difficult, proceed too slowly, and take too long for many people to stick with them. for another I really don’t think they are going to be effective for a significant subset of people who do stick with them. Some people, though, are going to find them quite effective.
I like what Christine said – given the lack of other options – why not give stuff like this a try? When we know more about ME/CFS and FM, and good, easy to use, treatments come up, then they will get precedence. I look forward to that day!
That’s not evidence and there is NO evidence that you can rewire the brain in this manner (otherwise all stroke victims would recover and they don’t). Not all brain damage can be reversed and it definitely can’t be resolved this easily. It often takes years with guided therapy. There has been no evidence ME can be treated through brain rewiring or that brain damage is even part of it. You can’t rewire sensory nerves. This person doesn’t even understand basic biology of nerves or how sensory nerves are dramatically different from brain neurons.
This isn’t a agree to disagree. You are literally posting fake science trying to pass it off as real and it will kill someone.
Read Norman Doidge’s book and then say neuroplasticity e.g. rewiring the brain is a scam. Textbooks – large textbooks have been written on it. Comparing stroke victims for whom sections of the brain have been destroyed – never to come – to people with ME’CFS and similar diseases for whom no structural damage has been found – is like comparing apples to kumquats. Even people with stroke can improve markedly using neuroplasticity.
I agree there are no studies using this technique – if you;ve read the comments you’ll know that the technique is being put to the test – although in which diseases I am unclear.
If you knew this program I think you would find it very hard to believe it would kill someone. I’ve done it and I can’t imagine how that could happen.
As to the sensory nerves – we don’t know that aensory nerves are causing the problems in ME/CFS.
Just to say if you were to scam me which i Ofc do not belive but idk you if so was the case i Would Report you to all 3 scamdatabases that almost all people check before paying for unlicensed treatments and i Would Report you to roblox and to alert scammers group and tell all My 200 roblox friends to spread the word, so you Know think twice about scamming me!!!!!
Check out the physicians who recommend the DNRS program to their patients.
https://retrainingthebrain.com/what-doctors-have-to-say/
Beside Mary Ackerley who is not mentioned they include Dr. Neil Nathan – a well known functional medicine practitioner, Dr. Raj Patel – another mold specialist; Dr. Chris Kressor – another functional medicine specialist and others.
You may find the English processes of Alex Howard align to the concept also of calming the nervous system to allow the body to commence its own healing process. Whole tones I believe also rely on a somewhat similar process.
Sure enough…your body wants to heal…but in some cases it’s just so busy regulating all the disregulation that it cant heal properly.
Cort. Try a Vipassana. Its WAY more intense the the brain retrying systems you are talking about, but literally the same thing and far more effective. Th other thing you could do is careful (high) dose of pcilicybin and you will see your feedback loops in crystal clear terms. It won’t be easy, but you ll change forever in short period of time.
Thanks Mathew,
I’m reading Pollan’s book now on the healthful effects of psychodelic drugs. Fascinating stuff.
I will check out Vipassana.
Functional medicine is literally a scam profession.
https://sciencebasedmedicine.org/functional-medicine-the-ultimate-misnomer-in-the-world-of-integrative-medicine/
https://www.skeptic.com/reading_room/why-functional-medicine-is-bogus/
Also called functional neurology
https://rationalwiki.org/wiki/Functional_neurology
Scam professions selling scam cures
I think many people who would disagree with you.
Interesting take on this subject…. pharmaceutical companies don’t hand out free scripts, or get ‘donations’ if you feel their drugs were helpful, doctors don’t ask for payment IF they were useful (or they would mostly all be poor)!Supermarkets don’t give away free organic veg to the suffering.
no person or company can survive like that….except perhaps Cort who seems to run on an oily rag….why would someone hand out a free mind reset system?
It always seems easy to put such a program together when SOMEONE ELSE did all the work!
It’s great to hear all these things reported by the site. It’s good that subscribers can express their doubts about such treatments. That is how the site can hone down such options to the relevant subsets of users who may potentially benefit. As Cort correctly says…not every option suits every person.
Sift through the offerings and find what you may like to try.
And good luck to you all.
Mind/body techniques often seem to inflame some in our community, me included at times. I think it’s understandable that we’d be prone to a knee-jerk reaction, given the insulting and damaging nonsense from the BPS crowd.
However, I classify mind-body techniques like DNRS – that don’t lie to us (unlike the BPS – see PACE trial for an egregious example) – differently.
To me, they fall under the category of calming down our nervous systems. Most, if not all, ME specialists include techniques to accomplish this — like pacing, for example. It’s not the *only* treatment, but it’s usually part of the treatment complement.
This field simply doesn’t have clear answers for us — some (subsets) are helped by any number of treatments – but calming down the nervous system seems like it’s worth a shot, even if it helps a little.
Recovery stories are essential for us to know about — you never know when you’ll find one that might work for you – even if they can sometimes hurt (I.e. “why not me?“) because we all desperately want to recover.
Congratulations to Christine for finding her answer. I really do hope it continues to work for her – and thank her for taking the time to report on it!
I agree with you in that it’s great to see what other people are trying to see if there’s any relevance for us.
Some things in different blogs fit with my portfolio of issues and others don’t.
I was caught in a vicious circle of extreme stress, tapping into very basic survival processes. One of the problems was that I had become accustomed to this level of chronic stress.
What I had to do was to separate out my stressful situation from my response to this stressful situation. That’s not easy when my situation is very stressful!
However I do get the point that I need to repeatedly provide evidence, to my highly reactionary and primitive survival system, that really I’m doing ok. I can see how this would be beneficial and it’s definitely helping me.
I bought the DNRS DVD course with the idea of debunking it for a friend who would not stop bugging me to try it. Then I would return it. But surprisingly it helped with sleep and lowered my anxiety levels. And I am making tiny breakthroughs in exertion capacity. So I can’t return it now since there was some improvement.
DNRS raised my curiosity about brain plasticity re-training, so I’ve started reading other books, and the field is fascinating to me. I’m now studying the latest findings related to the Limbic system, there is a possible correlation with all of the common ME/CFS symptoms, and even a possible explanation for CCI sometimes causing ME/CFS due to how the Amygdala connects with the brainstem.
I just wish Hopper followed a more scientific approach, there is a lot of ‘just believe me and try this’. I want to know all the details of how and why this works. Also, I believe a person could construct this type of approach themselves after reading the same neuroplasticity books she references in her course. But that would take time and brainpower I don’t have, so I would say this is a worthwhile shortcut to figuring it out for yourself. For those interested.
I’m right where you are. Limbic system rewiring is an exciting field and, I think, potentially explains a great deal about what’s happening in a subset of ME/CFS patients.
I’ve found some of the scientific papers discussing “trauma” or PTSD treatments – for example using bilateral alternating sensory stimulation – explain the science of calming down the amygdala well.
Fantastic it helped with your sleep!
Warm wishes for continued improvement.
Well, yeah. Annie Hopper’s “limbic injury” is probably anxiety or PTSD or neurosis, and retraining is essentially what garden variety therapy does. It reframes how you think and respond to unhelpful thoughts.
The difference is that a therapist can offer different techniques and delve into the roots of a maldaptive emotional response and help heal the pain underneath.
These programs are not necessarily safe or harmless for everyone.
There is such a pull to dismiss practices like this. I get it – it does seem incredible that a non drug treatment like this could move someone from a wheelchair to health in 18 months.
Suggesting that Christine, a nurse, who had successfully recovered from numerous relapses in the past suddenly became neurotic or developed anxiety, doesn’t for me, at least, make much sense either.
If you check out the practices that Hopper employed you’ll see that most of them are probably not employed by therapists.
I have never in 25 years have heard of a therapist curing ME/CFS or chemical sensitivities for that matter.
@cort below. Ok, what exactly is a limbic injury? Come on! She calls it that so people won’t be upset realizing they have some mental health issues.
Hopper does a bunch of wellness work: NLP, emotional distancing, positivity thinking, avoidance, visualizations, textbook CBT (changing behaviors, taking small steps) etc. Have you been to therapy? CBT, visualizations, avoiding stress are very normal therapeutic advice. There are books upon books written on SNS activation in trauma (I am reading one right now).
I don’t know Christine but repeated relapses are stressors that would lead to health anxiety at least. Which is perfectly normal.
If MCS is caused by a “limbic injury” it can certainly be treated by a psychotherapist.
The pushback is normal skepticism.
Thanks for sharing this story Cort and for sharing the many ways people find improvements to their health. I have always chosen to be very open minded in what I try to support my health and I prefer interventions that are less intrusive, such as NLP. I find the scientific explanation of the neuroscience to be a plausible one- that is, that the brain physically gets caught in a sympathetic nervous system response, and rewiring those neural pathways (a scientifically proven process- neuroplasticity) can help to calm it down- I struggle to see the controversy around that (as it’s not stating that’s it’s psychological) and am not sure why so many get so upset by this. There’s so much related evidence as well of people improving pain through neural retraining.
I’ve benefited hugely from the Gupta program (not a cure all, but a huge help), and I see this as one tool of many in my toolbox to help support my genetics and biochemistry to function as well as they can (as a result of what I suspect are several root causes of illness).
I note that rewiring neural pathways does take a lot of consistent effort and so someone has to really feel keen to commit to the work to make a physical change in their body. I personally love doing it- I feel so much happier and calmer afterwards (the Gupta program uses a neurolinguistic programming technique that involves body language to help you connect with an SNS thought, and then move immediately to a calm state to break the SNS/amygdala reaction to it- it’s a straight forward, non-‘woowoo’ process).
Congratulations on your improvements.
This is actually how I think of the program – as one of several tools that can help. Calming one’s system down using something like this can only help. Better sleep, more rest and rejuvenation can only aid whatever else one is doing. Besides an inability to exercise or ve very active without PEM and cognitive issues the one thing that has always stood out for me with this disease is difficulty relaxing.
My motor, as weak as it is, oddly enough always seemed to be turned on. Naviaux actually believes that’s what happens in the low energy state.
I think your comment sums up really well what I think. ?
Agree wholeheartly with you and Cort, to as well!??
@Gemma
Thanks for the gist on Gupta..
Going to take a look see on both openmindly try out takeaways from both..
Will add to my tool box..??
There is no science that says you can cure 50 diseases + with brain retraining. Functional medicine isn’t even a real profession.
https://www.ifm.org/functional-medicine/what-is-functional-medicine/
I agree Samantha. While it’s true that people can learn new skills as adults (rewiring), neurogenesis is unsettled science (https://www.statnews.com/2018/03/07/adult-brains-neurogenesis/) and yet DNRS suggests people do activities to create new neurons. There are a lot of red flags. Annie Hopper has no academic credentials as far as I can tell, seems to lump several illnesses into one all caused by the same cause. Which, btw, what exactly is a limbic injury? I asked a neuroscientist I know and he was frankly baffled.
I guess if giving your symptoms euphemisms and positive thinking makes you feel better, it’s great.
What I don’t think others (and Cort) are understanding about these types of mind body cures is that they might sound like they’re rooted in science but underneath it all is a bunch of books written for lay people cobbled together by NLP which has never shown to help anyone. Doidge is a psychiatrist, ME is not a stroke or a concussion, and we have a lot to understand about both this condition and neuroscience in general before touting $300 cures.
How about an interesting analysis of both Hopper and Gupta programs by a third party who uses both? This is a long but very enlightening article. It gets down to making new pathways in the brain so it reacts differently to improve our health.
https://www.holistichelp.net/limbic-system-retraining.html
Thanks!
Thanks..that sum it up for me!
Thank you Christine for your story. I’m incredibly happy that you have found your way out of this disease. A win for one of us may potentially be a win for us all.
I don’t usually post comments, but I’m saddened by some of the comments posted. Firstly, Roy, what is an average ME sufferer? I’ve not seen or heard of two people that are alike in this disease. I don’t have some symptoms that others have, yet I have symptoms that others don’t. That is one of the major underlying problems with this disease; we aren’t identical in the way we develop the disease or how the disease plays out in each individual, and hence the reason why some of the best scientific minds are still trying to work it out.
I’ve had ME/CFS for fifteen years and for the first eight years, my disease was similar to Christines. After an initial illness, I recovered for about three months before I got hit again. I would recover, go back to living normally and be hit again usually for longer periods each time. My crashes would last from three months to eight months, but after I came out of the crashes, it was like I was never sick. Bizarre? Absolutely. But nothing about this disease makes sense. Psychological? No.
Then eight years into the disease I decided to do a fifteen minute jog ( more like a shuffle) as I had been walking regularly and wanted to do more. Twenty four hours later I went into a crash that has now lasted seven years and I am housebound and at times bed bound and can only leave the house in a wheelchair or mobility scooter.
For the first eight years of my illness I didn’t have a diagnosis. All the doctors I went to here in Australia dismissed my symptoms. It wasn’t until I inadvertently pushed myself into a more debilitating state of the disease that I was taken seriously. Do I believe that I had ME/CFS in the beginning? Absolutely. I was just more fortunate than some that I wasn’t as debilitated at the beginning. And yes, three specialists both here and in the U.S. have given me the same diagnosis.
So please, for those of you that made the comment that Christine probably never had ME/CFS to begin with, you should know better. We’re all in the same battle here remember?
I understand why people get upset when any type of neural treatment is mentioned. Goodness knows we’re sick to death of being told it’s all in our minds. Since I’ve tested positive for EBV consistently for the past six years, and Dr Chia found positive chronic enterovirus infection, I know my symptoms are not all in my head. But since drug therapy and every natural therapy known to man have not made any significant improvement in my symptoms, or made me sicker, I like Christine and Cort thought I’d give DNRS a try.
I like Cort, fell off the wagon after a month and a half because I actually felt okay enough for my husband to get me onto a cruise ship using a wheelchair and out of the four walls of my home. I didn’t keep up the training whilst away.
Do I think that DNRS will cure my ME/CFS? Who knows? Why I did decide to give it a try is to see if it could help with the smell and noise sensitivity that I struggle with, and in the weeks that I did the program daily there was a significant improvement with those sensitivities.
I would never do this program if it was going to make me sicker, and I can reassure those wondering, if you can’t stand up, then you sit and do it, and if you can’t sit, you lay down and do it. Remember, I am at a point where I am unable to walk for more than two minutes continuously, and I don’t want to be permanently bedbound. This program helps to calm the autonomic nervous system which plays a role in the immune system, and my immune system could do with any help that it can get.
After six years of unemployment due to this illness, I’ve not once had any doctor or therapist offer their services for free or for a donation. People need to make a living themselves, and Annie is no different. Here in Australia you spend more on a naturopath appointment than the cost of this program.
For a disease that is so confounding, maybe the remission and cure that some are getting are because of treatments that are as out of the box as the disease itself. We should be cheering on those that are out of this hell, not pooping on them because we’re still in it.
Would love to get an update in the future from you Christine. Enjoy your life, and be sure to make up for all the lost time in a grand way.
Sandra,
Your post made my day! ?
Your post made my day as well, Sandra. You are a pure voice of reason. Thank you! ?
Sandra,
Here,here! Could have not said that any better! So happy and glad you got to do an walkabout (cruise)! Awesomeness!
Congrats to Christine and thanks for sharing you and your story! Understanding that everything is worth a look see into and a try to help with coping with horrible condition and state that we are all in this together! Blessings to you both!
Sandra I totally agree ❤️
Hi Cort, I’ve just made another small donation. Hope others are able to do the same. I know that every bit helps. ?
I find the DNRS programme interesting as I have read a lot about neuroplasticity in the past few years.
Whether it is applicable to ME/CFS or not, I’m not sure. I hope you are able to restart and continue on with it this year. I for one would be very grateful to know how you get on with it.
It is always encouraging to hear of another sufferers improvement.
Cheers,
Gail
Thanks Gail!
My experience leads me to believe this could be one aspect of approach to reestablish the lost balance in the entire system, whether using this particular programme or not..
I had an 80% recovery for over 5 years following a regimen of food & other triggers being excluded, various complementary therapies, but most importantly, learning self-hypnosis.
The course challenged us to recognise detrimental beliefs, to tune into the body’s small signals, and “rewrite” that faulty belief.
Using this tool, for that’s what hypnosis is, a tool, I was able to gradually restore close to normal function gradually getting back to full time nursing in acute paediatrics. Also studying for degree etc.
However, 5 years of this put me right back where I began. Very ill. I believe the primary “trigger” was the highly stressful life I was living. Night duty, overworked, forever expected to do more and more both at work and at home, children’s schools etc.
So I firmly believe that the permanently overstimulated autonomic nervous system & it’s effects on immune, neurological and hormonal functions is hugely significant in ME.
I crashed again because I went back to overworking, overcommiting and striving. So it’s important to change the beliefs that drive us to that behaviour if recovery is to be sustained. I’m currently making slow & steady progress from the very deep pit. Thanks for all you do Cort.
Thanks for everything you share, Cort. My naturopath wanted me to try DNRS, but the price tag is a deal breaker. I am trying to do my own thing through writing and trying to return to my own mindfulness/yoga program. I’m at a low point, but I really think it will help. I know my brain is locked into that fight/flight/freeze thing ever since I first got sick and was totally disbelieved by doctors, family, etc. I’m glad to say the latter has changed quite a bit, but I’m still in a very reactive place – again, slowly getting better, but 30 years is a long time to be in that place, so it takes time. CBT literally saved my life years ago, so I’m not afraid to look at how the brain and nervous system play a role in making things worse, even if they are not the cause.
I appreciate being shown different viewpoints on what helps – the review someone else posted in the comments is also very interesting.
Of course it’s impossible to share someone else’s program – it’s copyrighted, and I’m sure you don’t have the funds to fight it out in court! Thanks for everything you do – I much appreciate it!
Thank you Christine and Cort for sharing this experience.
I would share Christine’s view of just needing to try different things.
Over the years no one has actually said I have anything, apart from asthma – and I had to suggest that.
I have cobbled together my own program – diet, relaxation and stress reduction, restorative sleep and supplements.
I have to do everything, everyday – my immune system doesn’t take a day off!
I’m actually doing well. I would have incorporated Dan Neuffer’s ideas into my approach, which I think is working on similar areas to Annie Hopper.
Though I was struggling with my health from 2007, I made progress by adjusting my diet – more nuts less carbs. However my health started going rapidly downhill in 2016 – stress levels skyrocketing and possibly hormonal changes – I was 55 then.
So I’m a lone parent, couldn’t eat anything to give me any energy – in fact eating nuts seemed to be putting me into a negative energy situation. My legs were collapsing under me. Went to pick my son up from school, as he was unwell. As I saw him approaching laden down with a packed school bag, I got out of the car and started to walk towards him. My legs couldn’t hold me up, so to avoid collapsing, I had to step backwards and nonchalantly lean against the car. I didn’t say anything to him – he was 13 then.
I’ve had so many symptoms, I was completely bewildered. I have no diagnosis of ME/CFS and have never seen anyone in relation to this condition. But whatever anyone wants to call what I have, or say I don’t have – I was still left with the reactions to food, medications, total exhaustion etc etc.
I was deteriorating fairly fast. As I said was on my own with my son, then 15. No one believed I was so unwell – most of my family are extremely unsupportive and quite openly discussing my mental health issues. My doctor also believed my condition was a mental health issue.
Over the winter of 2016/17, I started bleeding and became anemic. I developed an infection and had a fibroid removed. It took 3 rounds of antibiotics to get rid of the infection. But then in February 2017, I had the worst flu/respiratory illness I’ve ever had. I think the high temperature of at least 41°c caused brain issues. It was an absolute nightmare to live through.
For the next few years I struggled with trying to find food that I could eat, that wouldn’t set my brain off -smouldering, painful and malfunctioning.
So over the winter of 2018/19 I came across Dr Nancy Klimas and she drew me into the world of ME/CFS, which I was completely unaware of until that point. That then gave me a clue where to look for more information and I came across Dan Neuffer.
I watched all of his videos and bought his book CFS Unravelled. At the time I couldn’t honestly see how his ideas related to my food intolerances etc but I was going downhill fast and needed to be around for my son.
So, in April or so 2019, I really focussed on calming down, despite everything going on in my life ie – no support, very little money, ancient car and an extremely debilitating illness no one believed existed and tried to put myself in the totally made up frame of mind that things were ok, so I’d sleep better. Well believe it or not, I felt different in my body after the first night’s better sleep.
Later that day I tried to eat a bit of olive oil on my meat and vegetables and I could tolerate it just fine. Previously eating olive oil and the other oils like coconut would result in numerous ulcers on my tongue and my throat would swell up. This went, and that made a huge difference to my diet.
I continue to make progress. I’m currently struggling with what I would see as being a kind of PTSD because I have been so ill and totally disbelieved, unsupported and openly rejected by most people. Now I’m getting better, I have no proof I was ever unwell. The internal landscape of my life resembles a warzone. There are bits remaining but otherwise it’s fairly stark. I sometimes find that if I have instructured time on my hands that I’m feeling a bit lost.
Yes, I’m much better – steadily improving my health – I just need to start building a new life.
I do feel my progress has been muddly and by trial and error with my body’s reactions as a guide but it’s working.
So I would say Good Luck to Christine and thank you for sharing your thoughts ?
I would really hope that if you requested a discounted price based on your financial situation that they could work something out. It’s worth a try – you never know.
The fight/flight/freeze thing has been a notable part of my ME/CFS/FM since the beginning. I don’t know how important it is but I know it isn’t helping.
In
Hi Christine,
I’m intrigued by your recovery story.
Since being born in posterior birth position to a highly medicated mother, my life has been a series of insulting traumas in every sense; physical, emotional and mental. I have had severe paralytic viral attacks, the worst one striking when I was 17 years old. Anyway, the list goes on. I am now almost 66 years old and finally got a CFS diagnosis about five years ago. No help really, just a dismissive this is what you have so go home and figure it out yourself.
About 20 years ago, my PCP diagnosed me with FM. While being a very kind and caring physician, he was too busy to really dig into it and come up with practical solutions.
Recently I have been reading about the mitochondria connection; essentially a disruption of the necessary energy producing “fuel” at the cellular level. So my question would be that if that’s the case, do you think healing the limbic system also changes that disruption? Theoretically it would seem that in order for true healing to take place, the energy production disorder would need to be addressed first. Yet, it seems this program has worked amazingly well for you. Clearly you were committed and focused.
I am anything but a scientist, so if you could respond to this comment with your thoughts on my question I would greatly appreciate it.
Congratulations on your recovery – I am truly happy for you and your family!
Warm regards,
Mavis
I don’t understand where all this anger is coming from. You can get your money back within 6 months, less a 15% processing fee, so for $37 (for just the DVDs or the online course) you can try it out. I have no connection to the sellers of this program nor have I tried it. Please fellow patients, if our illness is mind/body, that’s OK! There’s a lot of evidence that it is, and pretty much all illnesses are anyway. People with less social connection are more likely to get infectious diseases and cancer, just to name one example. Please, please, let’s stop getting angry about this. Whatever works! That’s the bottom line.
Thanks for pointing that out. I just spent about $100 in supplements at the health food store. I doubt that they’re going to return my money if I don’t return to health or get better.
Va faire tes emplettes aux Whole Food.. Ceux-ci rembourse le prix global des bouteilles de suppléments si non utilisé au complet!
I signed up to the Gupta course when it first came out – about ten years ago I think. It seems very similar to DNR. I think many of the strategies advocated by these approaches are fairly mainstream now – so there is lots of material out there to draw on freely available. There will always be individuals who make what might seem like miraculous recoveries to those of us who struggle on
with less remarkable results from trying different treatments. There never has been a one size fits all for ME/CFS so I’m very happy that some find their ‘key’ in limbic retraining. Mainly, I feel no harm can come of it if one is careful not to be over-zealous – it is important to listen to our bodies and not misinterpret these approaches as meaning that our bodies are always in overdrive and sending out faulty signals. We simply don’t know enough to be certain of that. I found Gupta to be very modest in his claims and not stating he’d found a cure for all. A lot of the material is common sense once you accept the central premise – the Gupta programme definately helped me with anxiety – reading this article has motivated me to give it another try.
The promoters say their treatment works. Great. Now where is the evidence? No, not anecdotes; a real clinical trial with objective endpoints that can be replicated (or not).
In 2008 I experienced a near-complete remission that lasted long enough to buy a trailer house, build a basement, and get everything set up. I ate lots of Subway sandwiches that summer. Should I promote Subway sandwiches as a treatment? After all, I don’t eat them anymore, and I am very, very far from any kind of remission.
I don’t know Jmells. Clinical trials are incredibly expensive and few treatments for ME/CFS will ever get one. Expecting one practitioner to do that is asking a lot. They do sometimes – the LP got an academic to do one. I think Alex Howard is trying to get one done. The vast majority of things we all try have not had clinical trials done – so why require one here?
Besides as someone just pointed out – there’s a money back guarantee (minus processing) that is available. If it doesn’t work it out it cost you $37. You can’t get a better deal than that.
If no evidence is required, then why not support CBT and Lightning Process? Some people even claim that graded exercise is a cure, so why not support that as well? After all, it doesn’t cost much.
If poor quality evidence and anecdotes are good enough, why bother with clinical trials for anything? Think how much money could be saved if this approach is adopted for pharmaceuticals as well.
Anything with the power to help has the power to harm. But trials are expensive so we’ll just not bother to look for and measure harms. Drug companies will like this new approach. Patients, maybe not.
There is evidence – just not the kind of evidence you want. There are people’s reports. That’s the evidence.
It’s your decision whether you want to wait for expensive clinical trials – which will likely never be done for most possible treatments – or whether you will use the evidence at hand – even if it is clearly imperfect – and use it to assess the effectiveness of each approach. Health Rising is going to introduce a program that will help with that.
Clinical trials provide the best evidence – they will never go away and should never go away -but are extremely expensive and rare. The question is how do you move forward if you don’t have them?
There’s some good news, though: two studies are underway – how about that?
https://chriskresser.com/how-to-rewire-your-brain-using-dnrs-with-annie-hopper/
As to CBT/GET I think the studies demonstrate they aren’t particularly effective.
There is one thing for sure one would need very big pockets & very receptive Dr’s to sample all the treatments mentioned in this article two things that appear to be in short supply by most ME/CFS patients. It probably stood to this woman that she was a NP when seeking medical care as they tend to look after their own or at least they seem to do so in my country anyway. Whatever about her later on she definitely didn’t seem like someone with severe ME/CFS earlier in her illness.
This woman doesn’t sound as if she has severe ME/CFS to me anyone with the energy to read & research all these treatments doesn’t fit my experience of the condition.
I don’t know what the criteria of severe ME/CFS is but anyone confined to a wheelchair has a pretty severe illness in my book. Anything that can get somebody out of a wheelchair and back to normal life again – particularly with this difficult to treat illness – counts to me as something of a miracle.
I’m not a fan off all this functional medicine stuff it’s another word for all in the mind well and good if it worked for this lady but I can’t see it working for people like me whose condition was triggered by a mixture of viral triggers EBV, Bornholms & Endometriosis.
Actually one of the reasons I think these programs work, when they do, is that they may be effective at fighting off herpersvirus infections. The reason I think this is that stress is notorious for reactivating herpesvirus infections – and with both axes of the stress response (HPA axis, autonomic nervous system) messed in up ME/CFS – I would think we are ripe for herpesvirus reactivation.
If these programs can do what they claim they can do – which is to reduce the stress response – then they might be able to calm these infections down. Plus sympathetic nervous system activation results in an allergic, sensitized immune system and impairs the ability to fight off intracellular pathogens like HHV-6 and EBV.
Very good insightfullness, Cort!??
As I try to keep in my mindset and have a sign that says,
“Keep Calm and Carry On”
posted so I can see it everytime I wake to start the day..?
I avoided these type of brain training programs for 8 years because I believed they were scams. Then I became so desperate I decided to have a go. I had tried everything else with no success so I had nothing to lose. DNRS and similar programs have literally saved my life. After 10 years of being completely housebound and living with ME/CFS, POTS, MCAS, MCS etc I am now well on my way to recovery. I can leave the house several times a week and can walk for 20-40 minutes each day. Most of my old symptoms are either gone or greatly diminished.
Deciding to try a brain training program was the best thing I have ever done.
Congratulations for being willing to try something new and very different out – and, of course, for getting better – and then sharing your experience.
I’m actually glad to see this come up as a discussion here. I would love to see research (or even patient surveys) help identify which subsets of ME/CFS patients benefit from neural retraining programs. I spent about $1000 and a lot of time/energy over several years doing the Gupta Programme with no health benefits, yet I know of several people who have really improved from it. I think these programs would trigger A LOT less hostility if we better understood why it helps some and not others, and avoided the inevitable situation where those who improve take credit and those who don’t are blamed.
I don’t resent that neural retrainers charge for their services; I resent that no research has been done to help me determine what treatments might actually work. Like so many of us, I’ve been paying insane amounts of money to be a human guinea pig for almost two decades, so far with very little success. But, that’s the current state of ME/CFS, and something we’re all working our asses off to change. Many thanks to you, Cort for your invaluable role keeping us educated and up to date with the research and policy, and good luck with DNRS.
Thanks for being so objective despite trying so hard and spending so much money at it Amy! That speaks volumes. 🙂
Your experience jives with mine – that these kind of techniques help some people and don’t help others. I think its going to be that way for the forseeble future for just about every treatment.
I’ve tried things that have vaulted others to health that made no impact on me. Our next recovery blog involves a ketogenic diet. I really hoped that was going to be it for me – but it had no discernible impact – yet it clearly does work for some people.
Well, this blog has seemed to stir up a lot of emotions! Maybe it’s because so many of us have been dismissed as having psychological issues rather than a ‘real’ disease.
As people have mentioned, each of us is a body and a mind. The power of the mind is well demonstrated in stories about placebo cures. I don’t want to weigh in as to the potency or cash value of this technique–except–if it works, it works. But likely not a cure for everyone but may just help a bit with coping…
I don’t have familiarity with Ms. Hopper’s techniques, but I can venture a good guess as to it’s historical underpinnings. I would begin with ancient meta yoga, meditation and mindfulness and then move on to Psycho-Cybernetics. Next would come Neuro Linguistic Programming (NLP), then Emotional Freedom Technique (EFT or ‘tapping’), and perhaps Heart Math. One can throw in CBT (Cognitive Behavioral Training) and eventually EMDR (Eye Movement Desensitization and Reprocessing). I’ll bet that her technique incorporates a mishmash of many of these techniques.
I suppose that many of us could cobble together something similar just by doing our own research–but the allure of her program is that it is secret until you provide the ‘key’ by purchasing it. Perhaps many of us would be too tired to try to do this ourselves, so easier to just pay or fret that our ME/CFS has left us so debilitated that our finances suffer.
I have studied many of these techniques and I still have my symptoms although I admit I probably cope better than if I hadn’t been exposed to them. As for an update on my healing journey; after a FULL thyroid panel (overlooked by Stanford), I now have the diagnosis of Hashimotos and have started a small dose of thyroxine. This may or may not be my problem, but it’s something…
It’s whatever works…
I’m seriously wondering about all the people complaining about the price. How much have you spent on your health?! I assume way more than $250!
Like I just pointed out – I just spent about a hundred dollars on supplements…I’m about to have an MRI done for $300. I’ll bet a Holter monitor test will be similar and I would bet dollars to donuts that none of them provide much of value.
Cort, I have particularly found your last 3 blogs very relevant and beneficial. I have a diagnosis of Fibromyalgia and CFS/ME. I became housebound with a relapse in 2011 and I had to stop teaching but was still able to work from home as a professional artist. In Jan. 2016 I had another relapse and have been bedbound since then.
In addition to Neuro-immune (mono), Neuro-endocrine HPA Axis (adrenaline burnout), POTS, PEM, IBS, chronic fatigue, cog.fog, widespread muscle, joint, tendon, nerve pain, I also have the symptom of severe co-morbid depression.
This inquiry about Neuroplasticity has scientific merit and makes a lot of sense to me regarding linking brain problems, research into brain anatomy and the central nervous system and my symptom of co-morbid depression. My depression consists of fretful anxiety, emotional pain and ruminating negative thoughts and thinking. I have described this as an involuntary physiological neuronal storm but no one understood what I was describing.
What modern medical science knows about the brain is in it’s infancy. To refuse to look at how a afflicted brain would also afflict the emotions and the mind is just outstandingly bad science.
I am interested in looking at and investigating research that looks at Brain/Body/Mind interconnections in hopes of finding potential treatment interventions that might help mitigate or alleviate the symptoms and suffering of this tormenting disease.
There is not enough biomedical research in the fields of Psychology and Psychiatry.This is long overdo. Some studies in Neuroplasticity using brain scanning technology have shown through lab verification that tools of Neuroplasticity can form new wiring, firing and activity- in essence forming new neuronal connections. If I choose to investigate and try DNRS, I will record and report my journey.
Last, I realize that I have taken this blog for granted and I will remedy that today by making a donation.
Cort. I wish you continued ease with your efforts to do this important, valuable work.
Betty Herman
Betty I would have had a similar type of mental health response, when my brain seemed to become inflamed over the last few years. It was very specifically related to a brain issue and not an emotional type of issue.
I am glad that Christine and others have found relief through DNRS and similar programs.
I can’t help but feel wary when the DNRS website reads like one big ad, full of buzzwords and no real substance. I actually learned more about what the program actually is from Cort (and others) who kindly described the gist of it in the comments (thanks so much, Cort and others)!
Just what is so unique about the DNRS that it has to be trademarked and proprietary? From my limited understanding, mindfulness stems from ancient Buddhist traditions that were never meant to be “for sale”…I really don’t think the Buddha would approve of mindfulness getting hijacked by capitalism!
Also, how does this differ from other programs like the 8-week MBSR for Chronic Conditions program? I took this program at a local hospital years ago (for a different chronic condition – migraine – which preceded my CFS/ME). Of course it did not cure my migraine condition (and, importantly, it certainly made no promises to do so!), but it helped me to cope better and it increased my quality of life. It was conducted by an MD with training in MBSR, and it was relatively affordable (we only had to pay for materials – $120 total, Canadian; the fee for the sessions was fully covered by provincial health insurance).
Why aren’t government bodies in countries with public health care (like Canada, or the UK) offering/funding DNRS programs?
I feel very strongly that all CFS/ME patients deserve access to potential treatments, regardless of ability to pay. I share the concern about the cost of DNRS (and similar programs) that others have raised, although this is just one example of a much broader issue (the privatization and commercialization of healthcare).
Another concern I have is that almost every single practitioner that endorses DNRS comes from integrative/functional medicine. If this program acts on the brain, why isn’t there a single *brain* specialist (i.e. a neurologist, or neuroscientist) endorsing it?
I feel like my own skepticism might actually be a barrier to trying this, which is really unfortunate because we skeptics sure need help too! 🙂 But at the same time, I can’t simply stuff down my concerns and pretend they don’t exist. Furthermore, I know I probably wouldn’t do well with just DVDs/books/online self-help materials…I would need some in-person contact, and the $3000 cost of the seminar is entirely prohibitive me (I have been unable to work for the past 3 years).
I wouldn’t expect neurologists or other specialties that are ensconced within traditional medicine to know anything about this type of program or have access to it.If it’s not in the scientific literature they may not get to it. They’re pretty conservative in general – they have the reputation of being one of the more resistant specialties to ME/CFS.
Have you checked out how expensive some Buddhist retreats are? This article focuses how to go on retreats without going broke. https://www.lionsroar.com/what-about-the-cost-of-retreats/
Comparing DNRS to MBSR is really comparing apples to oranges. MBSR has been around for decades, has received studies, and is covered by insurance. That’s not true for DNRS.
Your points are certainly all well-taken, Cort.
Yes, unfortunately that does seem to be the case (regarding neurology), which is really ironic considering that the WHO classifies ME/CFS as a neurological condition! I was fortunate to have found one neurologist, however, who was really helpful.
I have found the most help, medically, through a specialist in environmental medicine who knows a great deal about ME/CFS.
And I have indeed noticed how prohibitively expensive Buddhist meditation retreats are (hence my comment about capitalism creating an entire industry out of principles that are non-commercial at their core).
At least apples and oranges are still fruit, Cort, so my comparison (while imperfect) can’t be that far off! :p I only mentioned MBSR because, in a previous comment, you mentioned that mindfulness is a big component of the DNRS program (and hence, I was reminded about my MBSR course)…so MBSR and DNRS seem to at least share that commonality. But you did point out key differences. It would be nice to see some impartial scientific studies (particularly brain-based ones) of DNRS, and also insurance coverage.
In any case, I love Health Rising and appreciate all that you do, Cort! If I ever recover enough to be able to work again, I’d gladly donate. I am just about to give low-dose naltrexone a try.
I have nothing but deep respect for you, and hope that you find substantial improvement with any treatments you’re currently trying 🙂
Thanks Brenda 🙂
I have struggled with ME and MCS for 28 years with partial (50-70%) improvement to pre-morbid baseline for roughly 25 of those years. Major relapse 8 months ago. I suspect my situation is like many others with ME/CFS: I will consider almost any treatment that has a shred of support for it, as long as it’s not too dangerous, I can’t wait for proven medical science to come to the rescue; my life is probably 3/4 over (if I’m lucky).
I started the Gupta program about 6 months into this 8 month relapse and I was already taking an antiviral, LDN, liposomal glutathione, and a few other supplements (as well as diet changes). So it’s impossible to know which factor is aiding in my improvement (I’m about 60-70% improved from the worst of my relapse).
That being said, I feel the Gupta Program has been a valuable additional tool in coping with the emotional aspects of having ME and the sympathetic nervous system arousal it engenders. As a clinical psychologist who has spent my career working with chronic pain and illness, my assessment is that the Gupta Program is a well designed and fairly sophisticated program for addressing an illness like ME. It integrates a broad swath of knowledge in a manner that would be very difficult for anyone (including professionals like myself) to do on our own. A colleague whom I’ve share the program with agrees.
The program appropriately addresses the importance of pacing . Ashok Gupta creates a very warm, supportive, even loving ambience. That he himself apparently experienced ME/CFS adds to the power the program. While his limbic hypothesis is somewhat (though arguably necessarily) limited and simplistic, it is basically sound and a good rough model for thinking about the mind-body connection. He clearly has put a lot of time into developing a multilayered program for calming the sympathetic nervous system. He professes an openness to participants modifying and customizing the program.
The weekly webinars are very informative and extra coaching is available for those who want it (I haven’t signed up for coaching but was very impressed with 2 of the coaches who presented on the webinar).
I do object to the warnings that one not engage in other therapies or read about emerging theories of ME that are not consistent with the Gupta Program. That’s infantilizing and condescending. I do agree that it’s not helpful to obsessively research all the competing theories and treatments re: ME. But i can’t imagine doing without Health Rising, which is an invaluable resource for the ME/CFS community (thanks you Cort!).
Should the Gupta Program be free? In a perfect world perhaps, but in spite of the very warm almost familial atmosphere of the program, it is clearly a commercial venture with increasing levels of involvement requiring increasing fees. The pricing seems reasonable given the breadth and depth of the program.
It would be nice to see a small percentage of the participants accepted on a pro bono or sliding scale (I don’t believe I saw that as an option, but perhaps it is.) Finally, I feel that I am benefiting from this program and think it could be helpful to some ME patients. But you have to be willing to stick with it and devote significant amounts of time to benefit from it.
I also have a mental health training in counseling and psychotherapy. But this condition goes way beyond the usual areas focussed on by therapists.
Personally, I’ve seen lots of therapists myself and have worked with lots of clients over many years.
The last few years took me into a zone I have thankfully never had to endure before.
What I would guess was inflammation in my brain, resulted in really extreme agitation, phenomenally depressive thoughts and feelings. When I calmed the inflammation, these desperate experiences went too. My training and experience helped enormously in dealing with this, because I knew it was physiologically manufactured somehow in my brain.
Also with the stress response – that was in a completely different league than I’ve ever come across before.
If I think about it now it’s like I found myself in completely uncharted territory – I didn’t know ‘where’ I was anymore.
Really horrible.
I’ve managed to bring my brain inflammation under control through my diet and have calmed my nervous system down, with the help of Dan Neuffer and reading blogs and comments here on HR and all the researchers featured here and the OMF, Solve ME, Bateman Horne Center and so on.
Thanks Tracey Anne for mentioning Dan Neuffer as I will check him out and I am happy to hear that he has helped as I knew/know about the others but not him..going to give it a whirl??
How do we know that not her body already had recovered and it was just her mind, fear and habits holding her back? There is the story in David Bell`s “Faces of CFS” book about the guy that had healed but he was still afraid to do stuff in fear of relapse. Why is Whitney not yet healed? Why are Jamison not healed? We have no indications that is was the Hopper program that did it. Go to the Hopper website we have a classic marketing operation with some questionable endorsements from “medical” personnel and from patients. Go to any get rich or get any girl scheme you will find the same. The hero story and how the hero overcame it.
All we have is Christine’s story, her extensive search for treatments none of which worked very well and then her astounding success with the DNRS. Again, you can twist yourself in knots trying to come up with some alternate explanation (she was already, in the wheelchair healed but didn’t know it – she had some habit that was getting in her way – but the most logical explanation is simply what she said happened.
She had after all recovered from relapses quite a few times before. Why wouldn’t she recover from this one? Why would she suddenly form some belief system that kept her in her wheelchair?
I think Hopper would say an injury to the brain was – at the subconscious level – was introducing sensitizing the neurons that produce pain, fatigue, etc. Hopper doesn’t work at the level of the belief system – her program is designed to go deeper than that.
Whitney and Jamison Hill are not healed because they have not found anything that can help them. I want to point out that there are probably many types of ME/CFS – check out how many different reactions there at to the same treatment – and requiring that one treatment be effective for everyone is asking far too much. I would never expect the DNRS to be effective for everyone or even 50% of people. I would think a 25% success rate that produced significant but moderate benefits would be pretty darn good. That would probably beat just about other treatment going for this disease.
The better option, I think, is to keep an open mind, try all sorts of things, and see what works, and hopefully you’ll get lucky.
I don’t know what your definition of “Medical” is or why you’re choosing to refer to the doctors as “personnel” as if they were lab technicians or something like that – but for people reading your comment – they are almost M.D’S.
Yes DNRS. like most business does marketing – and if you look deeper you’ll find plenty of success stories. If I had a product like that I would make my success stories as visible as possible.
I am so ill, I even could not listen to the cd’s. 2 years ago I could listen to you tube for 20 minites yoga nidra. I had to quit because I was declining (not from that) but could not understand the words anymore and the noise began to irritate me. Have troubles with noise, licht, etc.
I wonder if you can rewire a brain. why is there then dementia, parkinson and all the other neurological deseases. Not that I would not try anything that would help. But it is everytime , all those programs for me/cfs, chemical sensitivitys, etc and never for a “serious neurological other” desease. that makes me sceptical if you can rewire your brain at all.
I could not read much but indeed this women had so many recoverys and downs that you can not say if it is from the rewiring program. I knew someone who recover by pacing and much luck, just to get ill later on again. I heard og a women who could clean whole her home in & day, to be bedridden for the rest of the year everytime again. I heard so many stories.
I think there is to much not known about this illnesses to say something.
but if simply “rewiring your brain” would help, we would all be cured and healthy.
As I’ve stated I think this type of program will only be effective – and then in different degrees – for some people. I’ve never tried “rewiring” on the scale that Hopper wants, though. I imagine that few people have put in that kind of time and effort.
For the reasons you’ve stated I don’t think this program would work for you or Whitney or other people. For you health lies in a different direction.
The next recovery story involves a totally different approach 🙂
please, if you can, write about nancy klimas an how her trial go’s. I really need help. thanks. or other trials. but nancy klimas ones is so long awaited.
I’m really looking forward to that next recovery story! 🙂
Looking forward to it!??
It is a difficult field. When somone claims to have recovered using a “mental” technique” it raises much skepticism. I suspect this is because people have become very defensive about psychological approaches to ME. Often psychological approaches use personal stories of recovery, as do many different approaches including medical drugs and nutritionals. WE have little option but to accept what the person claims for themselves and this leads many to believe that there different approaches work for different people and to the conclusion that maybe ME is not really just one disorder.
The fact is that many illnesses can go into remission for unknown reasons even cancer can do this and the “recoverer” is recovered for many years or even permanently. Unfortunately in these cases we cannot scientifically (validly) attribute anything to the recovery. This does not negate the individuals personal belief in how they “recovered” – they are entitled to their belief.
If someone wants to try what they did then good luck to them. The main issue becomes whether the intervention has been evaluated independently and until it has it remains a “possibility”. In addition anxiety is connected ( a consequence ) of all illness and if we can reduce our anxiety we are likely to reduce our symptoms, especially if those symptoms are neurological.
I do think there is a kind of system arousal present in ME/CFS and FM which is not found in most other illnesses but if calming that was all I got out of any treatment I would be pretty satisfied. I’m pretty easy to please I guess 🙂
I have done both the CD’s and the in-person program of DNRS (now renamed retrainingthebrain.com). The premise is that your brain/limbic system has gotten stuck in a negative loop due to chemical exposure, trauma, mold, viruses, electrical exposure, stress, etc., etc. Your brain then solidifies these errant pathways and causes all sorts of physical responses such as the fight or flight response, triggering stress hormones, negative thinking patterns, etc. The idea is to recognize these negative connections and triggers and immediately replace them with positive thoughts and reactions. If you do this constantly and consistently you will make new healthy brain connections. The program involves a lot of anecdotal stories and videos of success, reading books written by Norman Doidge and the founder Annie Hopper, and practising your Stop, stop, stop mantra and then visualizing happy memories or preferred realities. The hope is that these healthy pathways will take hold, calm your brain down, and allow for healing. While you do this you are to cut all exposure to negative tv, news, thoughts, talking or thinking about illness, or letting others talk about negative things to you. You then expose yourself to triggers and practice the new response.They encourage you not to talk about or practise other programs at the same time and also not to tell others or your Dr. exactly what this program entails. If your Dr. wants to know the gist they can contact her directly. If you don’t believe in it or aren’t getting a positive response it is suggested your brain might be fighting the process to maintain the negative pathway. They do maintain that the placebo effect can be involved but that this I s a not a bad thing. They have spent the last several years raising a significant amount of money from “Friends and Family” so the Universities of Calgary and Alberta can study the effectiveness but I have yet to see any results. From a scientific standpoint I’m not sure how they will rate this because the program involves individual accounts of health and it heavily stresses not talking or thinking about illness, symptoms, or anything negative. The CD’s cost about $300 and the in person program about $3000. There is an incredible amount of marketing – they have a huge internet presence if you google anything about it with a lot of anecdotal stories. When you buy the CDs they suggest if these don’t help you may benefit from the in person programs. You are required to buy Annie Hoppers book before the program which again is a lot of anecdotal stories. Once you get to the program the encourage you to also buy the CDs if you don’t have them and at the end they promote over the phone coaching sessions that you can buy. My session had about 20 people with 2 coaches so I’m guessing the fees coming in were $50 000 to $60 000 ( it did include hotel and meals and workbook) for 3 full days and 2 half days. And BEWARE there was no refunds or postponing the in person sessions after the cutoff date if you are ill unless you are in hospital or terminal. This was absolute as they made it clear they were running a business. I will leave it at that so people can decide if this program is for them.
I wrote the lengthy comment above as I believe people deserve to know what they are purchasing and what the program is about. I believe that stress, anxiety, panic attacks, and anticipatory anxiety will make most illnesses worse and there is benefit in reducing these by several methods. I am truly happy for anyone who has experienced an improvement in their health. That being said I do not want my explanation to be construed as endorsement of the program. Besides the people in my group I know a handful of people who have also done the In person program who have Me/cfs. Some state they have seen improvements, others not, and some view it just as a tool/coping mechanism but they all still have prevalent Me/cfs. I personally am still very ill. I in no way attribute that to not practising enough or my brain being resistant to change. You generally will not see these stories as they heavily promote the “successes”. Also, the basis of the program discourages any negative talk or thoughts as they suggest this perpetuates these negative pathways and can sabotage your recovery. They have an online forum for members only and I have watched in real time as they delete any negative comments. I applaud keeping an open mind to all available treatments but you should be privy to all stories and not just the fantastic ones. People in this group are very sick and desperate and many in precarious financial situations so they need to be extra vigilant when assessing possible treatments.
You know I regard that as an acceptable outcome. If every $250 I spent gave me a 10 or 20% improvement I’d be running marathons right now.
I suspect that most people who improve will get moderate improvements. That said, I know two people (Christine is one) who have fully recovered, one from years of illness. I also regularly communicated with someone who was terribly ill who recovered completely using the Lightning Process. I know of others who’ve done very well with Dan Neuffer’s ANS Rewire program and Alex Howard has scores of stories on his website. I don’t know how often these things happen but they do happen – and they all seem to involve turning down an overactive stress response.
We’ll have a better sense of what’s going on when the two studies are complete.
I would like to suggest that those people who do not know much about the program that Annie Hopper is selling start out their inquiry by reading the series of articles critiquing the so-called “Lightning Process” written by David Tuller on Virology Blog.
This, I think, will give folks a much better idea of what these so-called “brain retraining” programs are all about, and what the problems with them are, then they likely will get just from listening to the descriptions provided by Hopper and associates or, at least so far, from the Health Rising blog.
http://www.virology.ws/mecfs/
Note – Most of Tuller’s papers on this subject deal with methodological problems with the study.
I thought that this David Tuller article summarizing Joan McParland’s experiences with Lightning Process also was informative.
http://www.virology.ws/2019/08/21/trial-by-error-joan-mcparlands-lightning-process-experience/
Also, as a Ph.D. psychologist who has focused for the past decade of my life on toxicity issues in ME/CFS, I have been asked for my opinion about the Hopper program many, many times.
Although I am not interested in focusing much of my time on this topic, here is a brief comment that I wrote on the subject a number of months ago.
https://paradigmchange.me/wp/retraining/
This does not fit with my experience of the program at all.
Hopper had a horrible experience with her sensitivities and a mold exposure played a role.
https://chriskresser.com/how-to-rewire-your-brain-using-dnrs-with-annie-hopper/
Note also that she was one of the speakers at the ISEAI’s first conference and that Mary Ackerley – a mold specialist – stated that she urges some of her patients to try the program.
She is quite clear that her reactions were real and biologically based. Nothing in the course I took advised people to ignore their reactions – just the opposite. Hopper also strongly urged participants to clean up their homes, and reduce chemical and other toxic exposures.
I think Hopper would agree, on the other hand, that small mold exposures are probably not problematic – just as small chemical exposures are no longer problematic – but only after the Limbic system retraining has been successful.. If it’s not successful they will continue to be problematic.
This is an interesting point. I think they probably do believe this and they may certainly be wrong. As Lisa points out other parts of the body can go wrong which may make individuals hypersensitive – some of which could be explained by limbic dysfunction. For instance autonomic nervous system issues could mess with immune functioning (the Th1-Th2 response Lisa mentions, a tendency for more allergic type responses, poor pathogen protection), the gut, metabolism and the cardiovascular system. I don’t know about problems with the detoxification pathways but I would guess they would not be impacted by the limbic system.
There’s a fundamental misunderstanding here. Hopper’s program does not include ignoring toxins. As I said her experience with chemicals was horrific. As she became sick one exposure overnight changed everything leaving her, incredibly sensitive with massive symptoms to all sorts of innocuous chemicals. She well knows that it is impossible to ignore such symptoms and her attempts to do so left her worse off.
One part of the program does ask you so ask the limbic system to stop its fear messages but the more important and more extensive part of the program has you actively rewire the brain by returning it to its former healthy state. Until that happens Hopper’s own experience aptly demonstrated to her how futile and ultimately defeating it is to ignore symptoms. She specifically warned against exposing oneself too much to substances that are harmful.
I think Lisa was quite objective in her reports that sometimes she’s seen that these types of programs can be helpful. That would be my guess – that SOMETIMES they are.
This, however, does not jive with my experience:
My experience is that so long as mold or other toxins are causing reactions then avoidance – except for the very small exposures used during the practice to retrain the brains response to them – they should be strictly avoided in order to give the brain a chance to heal.
>There’s a fundamental misunderstanding here. Hopper’s program does not include ignoring toxins.
What the Hopper program states repeatedly is that while larger amounts of toxicity may be harmful for anyone and should be avoided, insofar as people are reacting strongly to small amounts of toxicity that would not bother healthy people, the reason that this is occurring is because of damage to the limbic system. And that the way to address the limbic system issue is through the purchase of the DNRS program (or the purchase of the Gupta program, which is very similar).
As I stated in my short article, the idea that the reason that people are reacting so strongly may be because the protective mechanisms of the body have been damaged and are not functioning correctly, and that small amounts of toxicity may be causing actual physiological damage in those people that has nothing to do with limbic system dysfunction, is not accepted as a possibility in any of the promotional materials for the program or in the program itself.
On a more general note, I would like to object to the suggestion being made here that my viewpoint on this topic stems from my having any sort of “fundamental misunderstanding” of the Hopper program.
Apparently, the Hopper program encourages advocates to respond in an almost reflexive way that anyone who criticizes the program in any way does not understand the program.
But considering my own background in psychology as well as the amount of effort that I have put into looking into this particular program, I do not accept that this statement is applicable to my own situation at all.
I guess we are going to have to disagree. Several of your characterizations do not reflect the program that I took.
I had a look at the article and wondered which brain retraining programmes Jennifer Brea and Ana Harris were involved with?
As you wrote that they – Jennifer Brea and Ana Harris ‘have stated that they have been harmed by brain retraining programs.’
I see from a tweet from Jennifer Brea that she refers to LP. Would that be the Lightning Process?
I think these programmes are very different from each other and so it may be useful to have accurate information on which ones you are saying they’re referring to.
All “brain retraining programs “ are not the same. It makes no sense to lump them together. I do feel that asking participants to limit what they share with their doctors would be unethical and ill advised. The Gupta Program does not make such a stipulation. As a participant in the Gupta Program, I feel free to take what helps and leave what doesn’t. And I share completely with my doctors whom I fully trust.
Jennifer Brea and Ana Harris both used the Gupta program and said that they believed that they had been harmed as a result.
You can read details provided by them by clicking on their names (in orange) in my article.
The Gupta and Hopper programs are generally viewed as substitutes for one another, with individuals advocating any brain retraining programs usually suggesting that either one would be an acceptable choice.
Lightning Process is not positioned quite as explicitly by adherents as a substitute for the others, but if you look at participant reports of their experiences with LP and at the general theory of the program, it is very similar to the others as well.
Wow, didn’t know Jennifer did LP? Lighting Process
If so, I like to know more about that as well Cort ?Thanks!?
Haha. I still remember when Lisa proclaimed her Ph.D. status as similar to that of Leonard Jason, despite the fact that she got it from the Kellogg School of Management, and not any serious medical school. We all had a good laugh about that on the old HealClick forums, which she of course left after not being able to handle anyone disagreeing with her.
There are so many problems with Lisa and Erik’s fear-based approach one never knows where to start. But I’ll try to list a few, so as to hopefully prevent others from considering such a protocol, especially one not backed up by peer-reviewed science:
1. Her idol, Richie Shoemaker claims 25% — TWENTY FIVE PERCENT — of the population has a ‘dreaded’ mold gene. Even a four year old child knows this is impractical nonsense. If we think of all the natural disasters like Hurricane Katrina, etc., where tens of thousands of homes were flooded for months. According to their buddy (and discredited doc) Richie Shoemaker, they should’ve developed ME/CFS. They did not.
2. Thirty-six years after the fact, Erik Johnson (who by the way hasn’t spoken to Lisa in at least six years) STILL has to avoid all molds. So much for the success of ‘extreme mold avoidance.
3. One does not need to throw out everything — including family photos, clothes, furniture — and start completely over, in order to recover from toxic mold. Many people, even those who LISA KNOWS, did not do that, and yet miraculously recovered. This ‘all mold will kill you if you don’t get rid of ALL of it’, is the CLASSIC fear-based backbone of their protocol.
4. The Locations Effect. Well, that’s just about THE most unscientific piece of work of all of her ramblings. It basically amounts to a website where one can tell others that they had a ‘severe’ reaction near a lake in New Mexico, or the corner of 2nd Avenue and Smith street, in Portland OR is okay, but don’t dare go a block away, or you’ll be confronted by “the ick”, Lisa’s scientific term for some imagined ‘mystery toxin’.
But back to the topic she so hates: Brain-retraining.
Erik is a perfect case study, that is if he wanted to. He admits reacting to ‘something’, some smells, etc., in buildings when he was a small child. If he went in the hotel his family was living in (they remained well, except for his brother), he’d get sick. If he went outside, riding his bike in the sun, he’d feel “great”. He was CLEARLY traumatized as a small child, and that has stuck with him — his SUBCONSCIOUS brain — ever since then, and has become even more paranoid as he goes on.
He could benefit from brain-retraining. But I know he’ll never do it. He’s right, everyone else — including the majority of folks who didn’t do it ‘his way — are wrong. And no doubt he’ll be by here shortly to tell us ONCE AGAIN, that he’s told dozens of doctors about ‘the cause’ of the Tahoe outbreak, and “no one listened”.
I wonder why…
Cort, I worry about you because I think, with some of these comments, you are getting extra beat up. Not so good for your own condition, the stress and all.
Just wanted to say that I appreciate you posting about every kind of treatment–regardless. Hope this particular post commentary doesn’t distress you too much. And wish you continued improvement with it.
Keep up the good work! You have a staunch supporter here and I’m sure with most others. Sending you more healing thoughts! Bless you!
Thanks Nancy. This is actually kind of energizing – hopefully in a good way. 🙂
First I would like to say that Cort has put together the single best and most timely source of information related to CFS/ME and FM. As A retired physician who has done much research and written a few books, I can say that the quality of his analysis of literature and ability to distill complex information is superb.
I am now 68 and have suffered from CFS for the past 18 months. I am in bed about 22 hours/day and housebound except to walk to mailbox. On most days I have spent hours reading about this disease or involved on one of 4 brain retraining programs. My analysis is that if you’ve seen one case of CFS/ME you’ve seen one case. Each patient has huge differences as compared to many other well defined diseases.
I suspect that dozens of etiologies will be discovered. Because of both desperation and boredom, I have taken DNRS, Gupta, ANS Rewired (not finished with last 2) and just completed the first offering of Alex Howard’s Reset Program. They tend to share many features and all aim to calm the sympathetic nervous system, eliminate unhealthy thinking, and all promote mindfulness meditation (DNRS offers a couple but does not require as much as others.)
All are done very professionally with expensive productions and slick websites. All have active blogs of participants. All have many full or partial success stories but hard to convert to percentages. As Cort mentioned above, DNRS is currently involved in 2 studies. All have some type of money back guarantee. All require up to an hour or more a day of effort. All can be done to a great extent sitting or lying. I think these are all designed by individuals who have suffered years of symptoms similar to many of us, before designing their courses. All have optional one on one coaching by well trained individuals who have had one of the diseases.
All double blind studies that involve a placebo arm show some % of participants that have a negative reaction of some type, so no reason to think impossible here, but suspect exceedingly low. I think all these programs are designed to calm a maladaptive stress response which is to be expected in overcoming our many challenges. If you plan on taking one of these courses it is best that you have a deep commitment for a few months, expect baby steps with some ups and downs, and trust that the course designer wants you to succeed.
I am currently finishing 2 of the courses and will then try to fashion a daily routine. To date I have not been committed to a daily routine except during the first 3 months of DNRS. At that point I had made improvements but was not satisfied with the quality of my life and searched for the next great hope.
I would also like to say that the mind-body connection is poorly understood but profound. The Biology of Belief by Bruce Lipton points to the epigenetics that can be altered by our beliefs, and have remarkable effects. If you start one of these courses with a touch of skepticism that is to be expected, but if you are not open to some belief that it may be helpful then save your money.
Lisa,
Thanks for providing the link to your article. I clicked on the Jen Brea link (to her twitter account) & she said (in 2018):
“ I don’t really know enough about DNRS to say. That was my experience of Gupta. I do know people for whom DNRS has been helpful re: managing certain symptoms – another tool in the tool box.”
This was prior to her discovery of her CCI.
So, it seems while she did have a negative experience trying Gupta’s program, she knows of others for whom it was helpful. As with innumerable other treatments, one size never fits all.
Oh great Waiting, I looked at the link and found the same tweet and was thinking I would write that later ?
Also I looked at the Ana Harris Writes article and my view on her experience is that she sort of plunged herself into all kinds of situations and then had a health meltdown.
I went on to look at the comments by people on her article – very interesting. There were negative experiences reported but also positive ones. Though Ana was discussing Gupta, people were also writing about their positive experience with Annie Hopper’s DNRS programme.
I found Dan Neuffer very helpful. I didn’t do his ANS Rewire programme, I just watched his very informative videos and recovery stories for free.
I did get his book on my Kindle for PC and at the time found it hard to remember and there was a lot of information.
However I just listened and watched – my brain at the time was functioning at a fairly low and slow level and I really could remember very little.
The two things I held onto was that I needed to calm down and get better sleep. I was intolerant to most food and I was getting worse, when I came across Dan Neuffer and a video of his interview with Brenten. It’s no exaggeration to say they probably saved my life. That might sound a bit dramatic but my biggest issue is with food and that’s not good.
Dan is very good at stressing the need for rest, pacing and not overdoing it…
He has a website CFS Unravelled. I didn’t pay anything. I did email Dan a couple of times and he did answer. I thought about doing the ANS Rewire program but I kind of figured enough out myself to make progress.
I now sleep well, am no longer exhausted, have calmed my nervous system down and can tentatively add in some new food. But carbs are out – they set my brain off. There’s lots of food I wouldn’t go near. I pace myself and focus on relaxing every day and as much as possible.
And I was thinking yesterday that I don’t feel I need to convince anyone anymore that I’ve been unwell. I know what’s happened to me and I believe in myself and others can think whatever they want ?
… So – I’ve retrieved my Gupta material and trying to refresh my mind as to why, beyond the obvious advantage of learning to calm down the Amygdala, I didn’t feel it was a pathway for ‘cure’ – or a high level of improvement – at least,for me personally.
I just can’t seem to go along with the notion that thinking oneself out of a complex illness like ME/CFS is possible. The level of commitment and belief it must take to fully
follow through on one of these programmes is intense. The hardest and most concerning element I found was the committment to what I experienced as’denial’ – you really do have to cut off those negative (or ‘realistic’) thoughts – depending on how you view this – at the pass. You have to say no,no,no to pain/disability (though your body is screaming ‘yes’) and visualize good health (when your reality is the opposite).
Now I understand the method/ the argument for this approach and It seems to work for some but we don’t hear enough of those it doesn’t work for. Personally, I don’t much warm to the anecdotal accounts of success – they often come across as hyper/almost messianic and far from inspiring hope simply engender fear of failure.
I’d like to hear more from the middle ground.
What I really don’t understand is why all the secrecy? Secrecy is not how medicine and science advances. As I said in my earlier post – all of the general info regarding NLP is freely available – I want to know what is so different about these particular programmes that they can’t be openly discussed at a very general level? What is the secret ingrediant that has to be paid for and can’t be talked about? In their actual method how do the programmes differ from each other?
These are just random thoughts but I’m frustrated by the lack of clarity.
I regularly do “transformational” courses put on by Landmark Education. They use mindful techniques to support people in uncovering new possibilities and acting on them. Every course requires that I agree that I will not splash the course contents across the internet or devise a similar course myself. Their technology is, after all, their bread and butter.
It’s no different with Hopper. It’s pretty standard in these fields.
Academia is different but if you spilled the beans on a study before it was published or before it was presented in a conference – you would be in big trouble.
If that academic was starting a biotech company that was developing a drug you’d have sign agreements up the yazoo, agreeing not to provide any proprietary information to anybody, and if you did you’d get sued.
If you want to know about the difference between Hopper and Gupta I would say, based on my experience with Gupta years ago, that they are quite similar. Someone in the comments did post a link to a comparison.
Hi Cort – I understand what you say about not ‘splashing course material all over the internet’ but find it strange that there is so little discussion of personal experience as to actual method? It’s the evasion of personal experience beyond very generalised statements of ‘it helped’ or ‘it didn’t help’ that seems a bit restrictive. I know that I also ‘cherry picked’ from Gupta (a lot of folks seem to be saying this) but in doing that I’m not really following Gupta – I’m picking the bits that are in themselves taken from other practices (mindfullness, meditation, NLP, etc) There is nothing new or revolutionary in these practices/methods – its just that we’re starting to talk about it all in terms of brain plasticity, etc. I don’t have the link but I watched a series of videos on You Tube where a young woman was talking (as much as she felt able to) about her experiences/progress with DNR – at what one point she was referring to the affirmations she makes but said in so many words (not a direct quote) ‘I’m not allowed to tell you what they are’. I just thought why on earth not? There is nothing new about the use of affirmations – what is there to protect?
All I’m saying is in the interests of free speech – open dialogue – people should be able to share freely if they want to.
bHi Paula,
I agree that the techniques are not new or revolutionary at all and plenty of other groups use them. Hopper has a list of the practices she got them from. You could certanly patch the bones of this program yourself together.
Stating that this process or that process is done undercuts the program, though, because the program is the DVD’S and the workbook. It’s how they are presented, it’s the experiences of the participants ands it’s Annie Hopper herself who is present throughout ws well as the forums that are provided. The program is the sum package of all of that.
I was severely I’ll 2001 and nearly bedbound 4 months do nothing special a local doctor who don’t have no much knowledge about treatment cure me . But I again fell ill this time I am severely I’ll since 2012.
Read Lisa’s article and re-reviewed Gupta materials. I agree with Lisa that the notion that exposures to “normal” levels of mold or other toxins (by patients with MCS, which includes many ME sufferers) should be OK and responded to with affirmations and amygdala retraining, is problematic and potentially dangerous. This is the oversimplistic application of the limbic theory to all aspects of ME . We know that other parts of the brain aside from the limbic system are implicated in ME, MCS and Gulf War Syndrome. That being said, I have benefitted (as a cautious ,skeptical empiricist) from cherry picking from the Gupta program and learning tools to calm an overactive sympathetic nervous system. But until we have evidence to suggest otherwise, avoidance of triggering toxins and other neuro-protective interventions sounds like a good policy.
There is something that is being missed here and it’s probably difficult to get unless you actually do the program. Annie Hopper does NOT recommend that anyone thrust themselves into a toxic environment and then employ affirmations! Beside the fact that it’s a lot more than affirmation, in the course, she specifically tells people to continue to protect themselves and stay away from toxic situations.
It’s hard enough calming down a hyped up limbic system without putting it into hyperdrive by exposing it to a toxic situation. Instead, she recommends that any exposures be done slowly and gingerly…
In other words, David, what you’re agreeing to is a distortion of her practice from some who is well-intentioned but has clearly not done the course. I don’t know how to say it any other way.
I tried Gupta a few years ago, and also shelled out for online DNRS after reading Dr. Neil Nathan’s praise of the program. I did so out of absolute desperation and longing for my old, functional life back.
My Gupta program material was recently donated, as alternative nostril breathing and imagining myself skydiving did absolutely nothing for my Chronic Lyme/CFS/Fibro.
But at least Gupta didn’t make me sick like Annie Hopper’s program did.
I was so drained and wiped out trying to keep up with the DNRS schedule-they DO prod you a little to much IMO-that I shelled out even more money to get the written materials so I could slow the pace a bit. It was also totally exhausting.
I crashed hard and was a brain fogged, inflamed mess for weeks. The materials are in a box on my office floor.
What a steaming pile, lolsob.
Another minute of nonsense about the smell of Tide detergent and I’d have likely poked my own eyes out. There were also some “cult-y”
aspects that I found creepy. Like cutting off family and friends, etc.
It just didn’t feel right.
I think she’s a charlatan but I’m too sick and too tired to jump through idiot hoops to get a partial refund. Also not planning on giving her another dime, although individual support paid for by the hour is the standard recommendation for flunkies like me.
If I could talk or imagine myself out of this misery I’d have done so long ago.
Well I think you made the same mistake I did and I think you point out a problem with the course. It was designed for MCS but they don’t have a specific DVD for ME/CFS. I went full bore, tried to keep up with the schedule and made myself worse at first. I ramped way back and then picked it up again – and then it did help.
It’s also quite possible that if Gupta didn’t work for you and Hopper didn’t work for you then this kind of stuff is just not for you.
I’ve seen many doctors and nothing they’ve done has moved the needle for me one bit. That doesn’t make them charlatans in my book. I know people who have benefited from them. It just means they didn’t have the answer for me.
I don’t remember anything about cutting off family or friends.
There is an advertising banner for DNRS near the end of Christine’s article. May I ask if she included it or if it is paid advertising? I believe that is important to know for complete transparency.
If you check out other blogs you’ll see that I often put the logo of the organisation involved in the blog and that’s what I did here. I added all the images. The DNRS program was not made aware that Christines story was coming out, had nothing to do with the story coming out, and certainly did not pay for it’s banner to be shown.
Aside from watching the DVD’s and contacting them about a damaged one I have never contacted the organization. There is no hidden agenda here. This is simply one person’s recovery story of the many posted on Health Rising. The suspicions, fears and issues that recovery stories like Christine’s provoke are quite impressive. I hope that clears everything up.
I have used mind-body techniques for most of my adult life (but not Annie’s or Gupta’s) and I credit them for my calm response to my health challenges. Many have commented that I seem–dare I say–almost happy–despite all the things wrong with my body. Yes, I am very frustrated at times in my inability to accomplish all the things I want to do…
however, the one area that these practices have not been so successful is with controlling my high levels of pain. I have this idea that there is some sort of personal threshold above which my mind is unable to control the pain. Lower levels I can ignore or deal with, but once they get above a certain point, it is just too difficult.
This is ‘in the moment’ type of pain, not an enhanced worry about how awful the pain MIGHT be (a la CBT). I am wondering, how many others have a similar experience? Do some of these techniques help in one area, but not another?
As an aside, these techniques have not, to my knowledge, gained me any extra improvement in energy, but have helped immensely in coping.
Thanks for sharing that Nancy. I wonder since you’ve been able to induce calming if Moskowitz’s neuroplasticity approach for pain might help?
Thanks for the suggestion! I’ll check it out!
Thank you, Cort, for posting this story. It is very interesting to read, as this year my daughter (also with ME/CFS and FM) has started an at home program for her eyes, based on the same theory. This optometrist treats many with brain injuries and some with FM and related diseases. Though the aim is to retrain the brain to tolerate light and movement in vision, they find that for many patients, fatigue, balance, and other symptoms common for ME/CFS improve as well as the targeted symptoms. My daughter is also using successfully a technique from a therapist-author for complex PTSD, which she has learned on her own from books/audio books. She has a good layman’s understanding of neuroplasticity and believes her ME/CFS will also improve with this intervention. But she says, as you did, Cort, that it’s the daily, or nearly daily, commitment to the program, and finding how it works best for your own situation and diagnoses, that determine how effective it can be. This is the challenge for us with PEM, and in cultures where ‘easy and quick’ are valued. We don’t know if Neural Retraining would help her, and possibly me (this post has caught my attention), but anything is worth a try when you have been housebound for years.
I too wish it was more affordable. Cost has been an issue for us as well, in trying therapies. The very things that helped Christine first, have been what have helped me as well, LDN, Clonopin and recently glutathione intranasal spray. So I am interested in looking into this more….
So happy the fundraising went well. So many of us appreciate and value your work, Cort. I hope you don’t relapse from the endless educating and defending you’ve had to do through your comments on this post! Rest!
Thanks Denise!
Let’s hope your daughter has her own unique recovery to share at some point. She’s luck to have such a supportive mother.
Good luck with your daughter.
Cort, with love and genuine respect, I stated clearly that I was referring to the Gupta Program and in none of my comments have I stated that I took the DNRS course. Not making any assertions about DNRS specifically. The Gupta program states that offending chemicals are not actually dangerous and that the levels of chemicals one may currently be experiencing in their home or other typical settings should be acceptable. Based on my experience with MCS as a patient and psychologist helping others who suffer with it, I object to that characterization.Small or “normal” exposures can be harmful to some MCS patients. Nonetheless, I’m not throwing out the baby with the bathwater. I believe the Gupta program can be of benefit to many ME patients, but as with any other consumer product or treatment, the buyer has to be well informed and balance a sense of openness with modest skepticism. Now I am more curious about DNRS and plan to look into it. Thanks Cort for leading us through this long, fascinating and useful thread.
Thanks David – I apologize for mischaracterising what you wrote and thanks for your understanding.. Thanks for clearing that up and good luck with your search 🙂
I once gave a speech to a group of Gulf War veterans who had Gulf War Syndrome. I said that if everyone who had Gulf War Syndrome or Multiple Chemical Sensitivity turned green, it would be so easy. No one could deny the condition or suggest that a little mind-body work could make it go away.
I have served as a chair of the National Institute for Environmental Health Sciences’ Partners group for many years. Partners includes national health organizations for cancer, autism, birth defects, heart, lung and other groups where environmental exposures may play a role. Several times a year, Partners has presentations from researchers working at the NIEHS.
My organization studies birth defects linked to environmental exposures. One of our success stories was in a Tennessee community where companies were dumping solvents into an unlined, uncapped landfill that was linked by an underground stream to a river serving the community’s main water well.
We documented an 1100% increase in cleft palate cases over a three year period. This cluster was subsequently validated by the CDC.
The solvent that was leaking into the water supply was TCE, a solvent that can be found in toxic dumps and Super Fund sites all over the country. The cleft palate cases all were in areas served by this water supply.
We were able to get the EPA to investigate and the landfill was eventually capped; the water supply was moved and all residents were warned not to drink well water (TCE had also been buried all over the county).
The point of all this is that toxic chemicals even in small doses can cause birth defects; cancers and many, many other health problems which may, in some cases, include ME/CFS. Many people have deficiencies in the detoxification systems that can break down toxins and carry them safely out of the body.
To suggest that a little poison won’t hurt you is irresponsible and suggests that those who would promote this idea are woefully uneducated in this field.
Just to clear up any confusion about posts by “David.” I am not the David who posted critically about DNRS on 1/5/19 at 3:05 pm. I am the David who posted subsequently. Readers can’t see the difference…Apparently more than one David posting on this thread so I will be sure to post as David S. from now on.
DNRS has helped me immensely. And I was completely bedridden for 3 years, severely ill. It’s not an overnight cure. I’ve been doing it for over a year, but it’s the only thing that has actually helped me and I’ve done every treatment imaginable for CFS.
Hey can you tell me how u did the steps that require standing? As it seems it won’t work from bed as one point is physically moving from one spot to another
My experience with DNRS was the exact opposite—not a good one. I believe the problem with the program is that it tries to do something it can’t—heal severely ill people. I think it is better suited for people who are moderately or mildly sick, not someone like me who can’t walk or speak and is confined to a bed. I have heard some horror stories about the program as well. When the program doesn’t work, it shifts the blame to the patient, not the program itself. It makes the patient feel like they are doing something wrong, when really the program itself is flawed and tries to do too much. Just like celery juice and all the other fad treatments, I wish this one would stay in its lane.
Wow. I never had the experience that the progrsm blamed the patient. I certainly never got that from the DVD’S or the workbook. Did you experience that in the forums?
Several stories were presented of really severely ill people getting better and see Kristen’s story below. People with really severe ME Im sure present the greatest challenge, though. Really tough for any treatment to move the needle on that. I imagine that a treatment like DNRS that required conotive challenges would be particularly difficult.
I agree think it would be more likely to work in the moderately ill.
I don’t know why it would make one worse though unless someone pushed too hard – as I did in the beginning. Is that what happened?
Lumping it in with celery juice and fsd treatments? I don’t know – this program has been around for awhile and there are success stories. Christine worked on it an hour a day for over a year. That’s a little different from drinking celery juice.
ANS REWIRE. I just wanted folks to know that this is another program option that involves neural retraining. It was devised by an Australian Dan Neuffer who suffered from severe CFS/ME for several years and as a scientist devised his own cure. He wrote the book CFS Unravelled which explains his beliefs in great detail. His online course is very well organized with 31 daily lessons. The course also includes a couple of CD’s mailed to you. The US cost is $243 (depends on exchange rate) and is about 1/2 of the other courses. He does get into diet as well as meditation and changing unhealthy thoughts. I don’t believe that Dan is in it for the money. He gave away thousands of copies of his book free. I am not suggesting that this is better than other courses but cheaper with a bit more science included and a focus on CFS/ME and FM as opposed to DNRS which is ideally suited for MCSD. The first couple lessons are free online.
You are literally blaming patients here when they tell you they had bad experiences and dismissing them in favor of selling this scam.
I have the feeling that there’s no winning with you Samantha but for the record and I think my comments bear this out – I believe that DNRS can help some people and not others – not because anyone is to blame but because this is a heterogeneous illness and no one approach or even several approaches will work for everyone.
Hey Jamison – I was severely ill too. I’m still sick but I was also confined to a bed, could barely speak, and couldn’t even look at my phone or write posts like this. I actually started by meditating for a couple hours a day bc doing DNRS seemed to be too much for me to handle. Then I added in an hour of DNRS after 6 months and I’ve been practicing an hour a day, everyday, for over a year and a half. I’m nowhere near cured, but I went from 0 steps a day to now averaging 3,000 steps a day, driving short distances, talking, meeting up with friends. I’m not well, but the improvement is undeniable. I guess different things work for different people, but I just wanted to share my story because I believe it is possible to heal even if you are severely ill. Sending you love and hope! I’m still healing but now I feel like I have a little more control over my life.
Thanks Paul Phd. ??
For the gist on Dan N.
his program on his history !
Thanks for all your hard work Cort. All healing stories are valid.
I am profoundly grateful to Cort for moderating the many responses in a week where my head was in a completely different space. Thank you to those who shared their experiences, elaborated on the program, sent good wishes or expressed doubts. I was initially cautious about posting my story, knowing that to some it may just look like a remission. But, frankly, even that, I would celebrate. I will make a point of adding updates every 6 months or so (I originally wrote the story June 2019)
I want to reiterate that I never suggested this would work for all ME/CFS patients, and stated that if it is helpful even to a subset, it is worth sharing. As a clinician who has prescribed medications, I know that not all treatments work for all people – some have allergic reactions to medicines, others respond in paradoxical ways. We are always weighing potential risks and benefits, and that needs to be done here as well. In my ME/CFS experience, even thoughts can be exhausting. So at the beginning of my training, I imagined what I would do. And I took the training very slowly, because that is what kept me comfortable in the process as a whole, even though there were times when I felt very uncomfortable. I always knew I could pause, slow down the training. I referenced the student manual many times a day as I went through the program.
I realize that the cost of the program is a deterrent to some. I do know that the DNRS receives donation for people who cannot afford to buy the DVD series, so it would be worth making an inquiry, if the cost is prohibitive and the only thing holding you back. On top of that, one does need to choose to invest oneself in the program and commit to it with time and focus.
I have never met Annie Hopper and have no connection to her program other than as a participant. I am not trained to teach her method which she developed after her own health crisis, which was incredibly devastating. She depicts this journey in her book, along with the science, which I found really helpful in trying to understand the method. I really admire her ability to create this program in the state she found herself. Hopper also emphasizes environmental awareness and the need to create living spaces free of mold and other potential toxins.
In terms of family, friends, doctors: my community was important to me, and it was crucial to let them know what I was doing, including my doctors. There is a letter included in the DNRS program to help enlist the support of those closest to you, so they can be understanding and supportive in the process.
I have MANY more thoughts going through my mind- but I will save that for another moment.
Once again, thank you to Cort for so adeptly managing this blog!
The sheer volume of antagonistic comments you’ve gotten on this post has finally convinced me to support your site financially.
Bless you for responding with equanimity.
Thanks JK! 🙂 🙂 🙂
I have 3 in my family with severe MCS , (myself and 2 children) brought on by a drug that wiped out out good bacteria, and we lived in an area, with very high pesticide/herbicide use, in Australia. That was 20yrs ago, and we have never recovered. Had FMT’s, which did fix my chronic constipation. My daughter and I did DNR program for over a yr (did nothing) I never got my money back, I was to upset to try. My son tired the Ashok Gutpa, that never worked for him either. When your cells are so over loaded with toxins, you CAN’T retrain the brain. We have been taking a Zeolite, to detox our bodies, and this has been the first thing that has ever helped my daughter. That was until ALL the bush fires started here in Australia. Now I just stuggle daily , to hold it together , for what is happening to my children and myself. Everyone is different and the brain training stuff has certainly done more harm than,,, good,,,,,mentally, to us. YES, because they really imply you’re not trying hard enough. We also tired a Faster EFT practitioner, well that was the last straw , because that didn’t work, she implied the same thing. I’m over them/it all.
This story, along with reports that younger adults are getting more of their basic healthcare services from urgent care, reminds how important it can be to have a family practice as part of an urgent care center in which these symptoms might go undiagnosed for an indefinite amount of time.
This story is insightful and very relatable to the issues I’m facing with CFS, I have decided to take a natural path to in dealing with my CFS when I found http://bit.ly/ChronicSleepNoMore, it helped significantly me feel less tired, I hope that it helps some others.
Christine your symptoms are similar to craniocervical instability which is detected with an upright MRI.
To me that demonstrates how many different ways the symptoms associated with ME/CFS can be produced. Jen Brea had symptoms of ME/CFS and she turned out to have CCI and other spinal issues. Christine had symptoms of CCI and she was able to recover using DNRS. Perhaps an overactive limbic system is able to produce an immune response which then attacks the ligaments and resetting the immmune system stops that. That seems like a big, big reach but who knows.
I don’t think it’s a big reach. I have been wondering this very thing since hearing about Jennifer Brea’s recovery. Is it possible to recover from CCI using brain retraining programs? If the limbic system was restored to normal could her ligaments have healed themselves like so many other areas of the body do when the limbic system is healed? I think it’s possible. Jennifer presented exactly the same as so many people who have recovered from DNRS and similar programs.
Hi Tim
Do you still have the DNRS program available ? I suffer from CFS, Fibromyalgia, PTSD and multiple chemical and food sensitivities. I believe that i could benefit from the program. Please let me know if its still available ? Much thanks
The DNRS program was not created by Health Rising but it is still available if you wish to give it a try – https://retrainingthebrain.com/ – good luck!
Hey Cort are you still doing the DNRS? How’s it going?
As a result of Lyme disease, Epstein-Barr, heavy metal & chemical toxicity, mold exposure and several extremely stressful/traumatic life events (PTSD), I ended up with the entire gamut of environmental illness – MCS, EH, adrenal fatigue, hypersensitivity to molds, extreme food & environmental allergies/sensitivities and chronic fatigue. I was a patient at a well known environmental illness clinic, which is where I learned about brain-rewiring and DNRS. In 2018 I did the DNRS system for over 6 months and it was a huge help. The program is no joke – it requires an intense commitment, both in time & energy. When I began, I was mostly bedridden and couldn’t eat most foods. My situation was so extreme that if I smelled a strong smell I would literally fall down on the floor, often experiencing a simultaneous emotional meltdown. At the beginning of my DNRS journey I was not able to stand and perform the maneuvers, so I sat on the floor and did them. Little by little, with daily practice, my body & brain calmed significantly. Meanwhile, I was eating a very clean diet, taking lots of specific supplements, detoxifying with a FAR infrared sauna 3x/week and getting a lot of rest. After 6 months I was able to resume going out to do normal activities, eating at restaurants, etc, but I became bored with the DNRS routine, which felt like a chore, and I stopped doing the program. I was also running out of happy memories (part of the training routine). Now 2 years later, I feel some minor symptoms resurfacing and I’m investigating the Gupta Program. I know several people (from the environmental illness clinic I went to) who have done both programs (DNRS & Gupta) and benefitted from both methods. I personally am open to any & everything that could potentially benefit me/my health. Relief can come in many packages…I’ll try just about anything once! In my estimation, limiting beliefs can block you from doing something that could potentially help you. Good health to all!
Thanks for sharing your wonderful story here with us. When a person recovers from issues like this, they become an inspiration for so many others. Really, this will motivate more people to get rid of their health issues properly.
Dentistry Longmont
This is such a great explanation of the brain retraining process and how it has the potential to be a cure. It had honestly helped me more than anything and I have dealt with CFS for 36 years. Like mentioned here by others it is very hard to stick with DNRS and or Gupta. I’m just not sure why that is but it’s absolutely what I think keeps most from completely healing.
Thank you so much for sharing a story that often times it’s not welcomed on this forum!
Hi Michelle,
Which program has helped you the most? Thanks.
Thank you Christine, for sharing your story. Thank you Cort, for so patiently and painstakingly countering the many critics in the comments. I sadly lost the patience and tolerance to do so years ago and now just have to keep quiet. You have a gift sir, thank you for your service to the community.
ME/CFS is a crazily complex illness that affects all of us so differently and what some find to help, others find the opposite. However, what disappoints me more than anything, is members of the community bad mouthing, dismissing and attempting to discredit others who have found things to help. It is this behaviour and corresponding attitudes, that make members of the ME/CFS community our own worst enemies.
My observation over 8-years of searching for any possible way out of this sheer living hell, is that those of us fortunate enough to do so follow ‘recovery journey’s’. Trying anything and everything, slowly building up both ingredients and recipe that works for our specific manifestation of the illness and enables the mind/body to recover/reset from the freeze-fight-flight state in which we are perpetually stuck.
Thank you for the timely and helpful reminder that recovery is possible. Among many things, I previously found the Optimum Health Clinic very helpful and then the Gupta Program, before the Medical Profession forced me through what I can only describe as utterly catastrophic ‘psych’ treatment, undoing all benefits I had realised to that point, overlaying an enormous amount of trauma and reducing me to the worst state since falling sick from the virus 8-years ago. I had always wanted to give the ANS Rewire a go and this article and comments might just have provided the impetus needed. Thank you.
Glad to hear Tim. I certainly can relate to that weird freeze-fight-flight state that some of us are in.
Good luck with the program!
I am doing this program right now! I have had ME/CFS for 10 years. I was first diagnosed at the age of 34. And talk about irony, I was a marathon runner and aerobics instructor! When I first got sick I was bedridden for months.
Over the years I have tried everything from diets to mestinon and LDN.
I have made a slow recoveries over time. I can function, play VB, take care of a busy household. I still get PEM if I over-exert or try to do much cardio.
I have found while doing the DNRS program that much of the success in recovery I found was due to the fact that I learned these limbic system rewiring techniques on my own…reframing from negative, looking for the joy, HUMOR, gratitude practice, Yoga Nidraa, visualization…all of that is included in this practice and it is all helpful.
The mind and body are connected. Thoughts are powerful and cause affects on the body.
The irony is that many of the people angry and posting negative comments would benefit greatly from this or GUPTAs program. Why not try everything? I have spent way more in supplements alone.
This is just another good tool in the arsenal of sleep, nutrition, Mestinon, probiotics.
Thank you for the article!
Is there anybody out there willing to sell their DNRS DVDs to me? I’ve done Gupta. Still struggling. Would like to give DNRS a try but can’t afford the full program. Would love to purchase used DVDs. Anyone?
I admire all the folks that have had the determination and fortitude to participate in the Neural retraining programs. I learned about them a few years back. I had found some used DVDS on line ( i forget where) so the cost was much less than the $250. which is really inexpenisve compared to the CFS and lyme dr’s I have seen at least $500 a visit not counting suppliments .. easy to spend $500 a month on supplements.. I don teven know if they work.
I had another lyme/cfs friend locally that attended the inperson workshop. I think it helped for a whlie. we got together and did a couple sessions .. it was really nice to have someone else’s support and to hear their journeys.
I tried to continue the DNRS on my own for about a month. I was doing better and went on a bike ride with a friend. She fell off the bike and broke her elbow. that sent me into fight or flight as i felt bad about encouraing her to go ride with me.
In that fight/ flight and trying to help her after the accident I never returned to DNRS. I think the hardest part of the DNRS for me was repeating and detailing the memories and recreating that feeling in my body. I believe the memories are NOT supposed to be high adreline producing memories, which was also hard for me becasue some of the best time in my life were having adventures that were high adrenline.
I aspire to get back to doing DNRS or Gupta or something for rewiring the brain. Yet I lack the discipline. for a while I was trying to create a small group of folks that wanted to support and do the work together . no one seemed interested. I used to be good a physical discipline but the brain focus part and especially memory recall has become a problem. (not sure I ever had the brain focus discipline) I believe it can be developed and built like I used to be able to do with my muscles. I just dont know how to get myself started.
PS. when i watched the DVDs for both programs I am pretty sure I Fast forwarded through the beginning stories (sorry no offense intended)
I am late to this thread and yet I am glad I found it. Good reminder for me and I hope i can check out the other rewiring resources listed among some of the comments I scrolled through. so much good brain power in this community. it is inspirational. How do you all keep it up?
thank you
I can’t believe the negative hateful comments. All opinion, no actual bearing, just sick people being negative and hateful. These comments should be turned off and removed so people can make their own educated decisions. I am currently recovering from a huge list of issues using DNRS. It is amazing. 2 weeks ago I was on a very restrictive diet. In only two weeks I am eating what I want. My mood is improved, my head is clearing, me energy is improving. I AM SLEEPING.
If 1 person was persuaded to dismiss this course from all this negativity the entire point of this post is lost. If 1 person was persuaded not to take the course that could have gotten their life back?
Shame on all of you!
How do you expect someone to develop an effective program without charging? How can you run a website if it is not profitable. Servers cost money. So do updates and tech support. Also having coaches on hand and classes available? How? without profits to support these peoples lives.
Not to mention that the course costs less than one dr’s apptointment. Do you loath your Naturopaths for charging? I have done dozens of Ozone treatment, and they didn’t offer the improvement I am getting with DNRS. Ozone $360 for one treatment. I am over $5000 in all that I have done. DNRS 1 $350 payment.
There is also a free trial that goes deep enough for people to decide if it is right for them. They only charge for the program, which as I said costs money to develop and provide. How ignorant to say I hate it because they are charging.
I am so grateful to have found it, and I seriously shame all of you for your negativity. if only one person is still suffering because of what they read here, it is unimaginable.
I has been a great gift to me. I am going for xmas dinner tonight, and I was dreading it a month ago, planning to bring my own roast chicken. Now, I can go eat what I want with out worry and actually enjoy my friends and the evening..
Oh ya, and in six months if it doesn’t work, you can ask for a refund. Give your heads a shake!
I did the DNRS course 5 years ago and it completely changed my life. If done correctly, it can be a beautiful healing journey.