

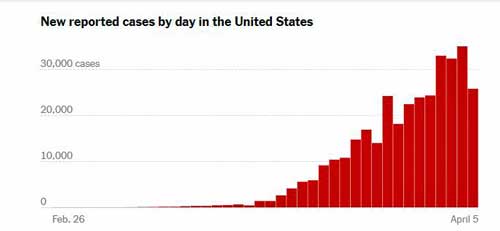
Just seven days ago, the U.S. had 131,000 confirmed cases. Today, it has 375,000 confirmed cases of the coronavirus, and we obliterated our past records of new confirmed cases with 30,000 each over the past three of the past four days. At this pace, the U.S. will hit 500,000 confirmed cases in the next week and a million in about three weeks.
That’s six times as many as China – whose numbers no one trusts anymore. (China, for some reason, does not count asymptomatic people who test positive.) China, it turns out, has a lot to answer for. The Washington Post reported that the CDC tried to get a team into China to get samples of the virus in early January, but were rebuffed and didn’t get the samples they needed to build the U.S.’s tests for weeks.
The U.S. continues to up its testing program dramatically and is now testing 100-150,000 people a day. Except perhaps for China, no country has come close to that and it’s going to get better. STAT news projects that in the next couple of weeks the U.S. will be running 200-300,000 tests a day.
- Check out the number of coronavirus tests run in the U.S. by day.
Percent of positive coronavirus test results gives us a rough idea of how much virus is out there and how effective our testing is. A climbing percentage suggests the virus is continuing to spread. A declining percentage suggests the opposite. Over the past three days, the percentage of positive tests in the U.S. has climbed from 18.3% to 18.6% to 19.4%.
Want to track the virus? Check out Health Rising’s new Coronavirus Tracking page for the many different ways to track its spread.
Peaking?
Thankfully, the coronavirus outbreak is not a forever thing. It will peak – and will probably peak in the not very distant future in most countries. The virus will probably still be around, but the worst, at least for the time being, will hopefully be over.
The peak is important because it’s during the peak that health resources are most stretched, resulting in more fatalities. One of the goals of social distancing has been to push the peak back as far as possible to provide more time to produce the needed health resources (everything from masks to respirators) to deal with it.
The IHME models predict the peak outbreak times for countries, states and provinces across the world
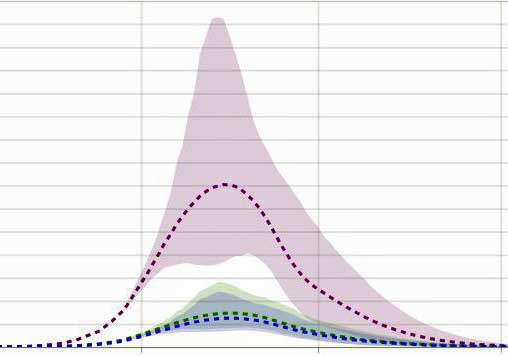
The models most commonly used are coming out of The Institute for Health Metrics and Evaluation (IHME) in Washington, a worldwide health data gathering institute funded by the Bill and Melinda Gates Foundation.
The IHME’s models, which are being constantly updated using data from a variety of sources, are generally predicting an earlier and smaller peak to the virus than some other models. Let’s hope they are right.
- Check out when the IHME predicts a peak in your area and how well your area hospitals are prepared.
The different models can vary greatly, but most suggest that the U.S. and other countries are moving into the thick of it and that a peak rate of infection and deaths will hit over the next couple of weeks to next month. The IHME suggests that the U.S. as a whole is 8 days from the peak, and on that date will be 36,000 hospitals beds, 16,000 hospital beds and 25,000 ventilators short (!). Now is not the time to get ill!
Once the peak came in China, it lasted for a week or more before declines came. That may be the situation Italy is in now.
The Hot Spots
New York City, New Orleans, and Detroit – The hot spots in the U.S., are believed to reach the peak of their outbreaks over the next week. Projections suggest that, at the peak, the virus will probably kill 500-700 people a day in NYC. New York crematoriums are now running 24 hours a day and even requesting that the dead be buried in cardboard boxes because they burn faster. The city put out a wireless emergency alert on Friday asking any licensed medical personnel to volunteer to fight the virus.
Italy’s hot spot, Lombardy, has been the scenario no one wants to repeat, yet the New York Times graphs (new weekly confirmed cases per thousand) suggest that the virus is on an even greater tear in New York City, Albany, Georgia, and New Orleans. New York posted its largest gain in confirmed cases ever (10,000) yesterday.
The United Kingdom – As expected, deaths have shot up rapidly in the U.K. The deaths now are occurring to those at risk who caught the virus 2 or 3 weeks ago. With the expected peak, ironically on the day, Easter Sunday, Donald Trump once predicted the U.S. to be back in business, the country may see rising deaths over the next month.
The country is expected to remain in an intense lockdown until the end of May. The Imperial College Modeling team reported a couple of weeks ago that with the social distancing practices put into place, the British medical system should be able to withstand the peak.
Italy – The virus has been churning through Italy for 6-8 weeks and the country has been in lockdown for almost a month. The percentage daily growth rate of new cases has decreased and deaths have stabilized. Still, Italy is adding over 4,000 new confirmed cases a day. Thus far, Italy has been in more of plateau than a peak.
Seattle – Seattle is interesting because it was an early hot spot. Projections now indicate that the peak will hit over the next week. A recent report suggests that the R0 for the virus – the number of people that each infected person is likely to infect – is down significantly from over 2.7 to 1.4.
Others
The predictions for the not-so-hot spots suggest that the peak in most cities will follow the peak in the hot spots by a couple of weeks; California (and Philadelphia) appear to be exceptions. California’s institution of more rigorous social distancing measures earlier may have allowed it to push back the peak to mid-May and blunt it. (Every model shows that pushing back the peak also blunts it and results in fewer deaths.)
Some more peaks predicted: Miami – end of April; Boston – April 10-20th; Philadelphia – mid-May; Phoenix – late April; Chicago – later half of April; Minneapolis – early May.
Is It in the Air?
Is the virus spreading through the air? There’s no doubt that if someone sneezes or coughs on you or next to you, you can get it that way, but could somebody sneeze, cough or simply breathe, and thirty minutes later infect you if you walk through the air they were in? Staying aloft that long would require that the virus be present in aerosolized particles (as opposed to droplets) smaller than 5 micrometres (.0002 inches) in diameter. These tiny aerosolized particles can be passed simply by talking and breathing.
You’d think this would be worked out by now but it hasn’t been. On March 27th, the World Health Organization stated that “there is not sufficient evidence to suggest that SARS-CoV-2 is airborne.”
Nature reported, though, that experts on airborne infections assume the virus is airborne but that it will take time – too much time – to gather the evidence that it is. Aerosol scientist Lidia Morawska, of the Queensland University of Technology in Brisbane, Australia, said:
“In the mind of scientists working on this, there’s absolutely no doubt that the virus spreads in the air. This is a no-brainer.”
A Chinese researcher found evidence that viral transmission through the air can occur and “impact people both near and far from the source”. He recommended that the public wear masks. Two other studies, however, did not find airborne coronavirus, and one that did so didn’t find any infective particles. One study attempted but failed to find RNA from the virus in air collected just 10 centimeters in front of an infected person who was breathing, speaking and coughing,
The sole study, amazingly enough to test the aerosol idea out, demonstrated that the virus can be found for up to three hours in the air under laboratory conditions which involved using a nebulizer to feed viral particles into a special drum. The study found that the viral infectivity half-life – that is, the amount of time that half the virus was still able to infect a culture – was just over an hour. One of the co-authors noted that the conditions were “highly artificial”, but that there is probably “a non-zero risk of longer-range spread through the air”.
Another question involves whether enough virus is present in the air to infect someone. Quickly passing through an airspace where someone was breathing or emitting virus is one thing – standing next to someone who’s been hacking away for 30 minutes is quite another.
The consensus right now appears to be that when the virus is being transmitted, it’s usually being transmitted by picking it up on our hands and transferring it to our mouth, nose and eyes. When respiratory transmission occurs, it probably most commonly occurs via large droplets passed by coughing or sneezing which quickly fall to the ground after travelling usually a couple of feet – but possibly 25 feet.
STAT News reported that microbiologist and physician Stanley Perlman of the University of Iowa stated:
“I think the answer will be, aerosolization occurs rarely but not never. You have to distinguish between what’s possible and what’s actually happening.”
Some epidemiologists believe that we would see far higher rates of transmission, particularly among people who don’t know each other, than we are seeing thus far if the virus was strongly aerosolized. Earlier this month, CDC reported that 10.5% of household members are getting the virus, but only 0.45% of close contacts. That figure suggests that aerosolization of the virus is not a major source of infection as well.
Aerosolized transmission may be occurring but it’s not now believed to be a major source of infection. It should be noted that the danger of picking up an aerosolized form of the infection is worse in poorly ventilated areas.
Intensive Care Unit Doctor in New York City Shares About His Experience with COVID-19
“What I want you to know is that every single day we’re learning more…I’m not scared anymore.” Dr. Mark Price

Dr. Mark Price, an ICU doctor in the thick of it in New York City, urges people to be careful and not to be scared.
Check out a hopeful commentary on COVID-19 from an intensive care doctor on the front lines of the pandemic in New York City. His ICU unit is only caring for COVID-19 patients at this point.
Staying Safe
The virus goes throughout the entire body. About 80% of people just don’t feel good. The disease typically lasts between 5-14 days. People who get short of breath usually do so about day 3-5.
The overarching theme is sustained contact with someone who has the disease or someone who is about to get it. It’s almost exclusively from your hands to your face (eyes, nose, mouth). In order for an aerosolized infection to occur, they believe you need to be in sustained contact in infected air for 15-30 minutes.
COVID-19 is in your community – wherever you are – it is in the community. That is not to scare you.
Become a “hand-Nazi”. Know where your hands are and keep them clean all the time. He walks around with Purell. Every time he touches something, he Purells his hands.
It is not a disease that is primarily being transmitted by someone with the disease touching something and then passing it on. It’s overwhelmingly driven by being in sustained contact with someone.
Out of an abundance of caution, we make sure that after you touch something, you clean your hands. Always know where your hands are.
Be aware of when you touch your face. Wearing a mask stops you from touching your face. So, wear a mask. Washing your hands and wearing a mask (not touching your face) will stop, he believes 99% of the cases.
A medical mask is not necessary. The general community has zero need for N-95 masks. the mask is there to train people. Nurses and doctor’s in his hospital only wear an N95 mask when they’re doing something to a COVID-19 patient which will make them spit or cause aerosolization of the virus.
The health-care workers getting sick now have been in: (a) sustained contact with COVID-19 patients; and (b) were not protecting themselves properly earlier in the epidemic. He said now that they are protecting themselves properly, they are not getting sick.
In other words, so long as you keep your contacts short, you don’t have to be scared of your neighbor or the outside world. Throughout the world, the vast amount of transmission is via family and close friends – not through casual contacts.
(But what is sustained contact? One epidemiologist stated it was having a face-to-face discussion with someone who is infected. Note that a small German study suggested that people infected with the virus are most contagious before they develop symptoms. Viral shedding dropped by day five in the mildly affected patients and continued to be high for ten days in two patients with pneumonia.
That may mean that while this doctor is surrounded by seriously ill COVID-19 patients, he may not regularly be in contact with the most contagious patients – the asymptomatic ones. It’s remarkable how few studies have examined patterns of viral shedding thus far.)
The doctor recommended that we shrink our social circle dramatically, but continue to go out for short walks.
- Staying Safe – Check out Health Rising’s Staying Safe page including including hand washing, nasal irrigation, disinfecting, making a mask, plus – is the virus being aerosolized? How long the virus is alive on different surfaces, and does the amount of virus present matter?
If You Get Sick
What to do if you get sick? You will probably get a fever (90% get fever), body aches, etc., and be sick for a week or more. Isolate yourself from your family. (Avoid sustained contact…) Have the sick person in a separate room/bathroom if possible. If you have to be in contact with them – wash your hands, put on a mask, wash everything you touch. Don’t take their temperature constantly.
If you live with someone who is vulnerable, they need to be completely isolated from you.
The current indication from the CDC is that when you start feeling better, you can return to work with a mask.
Going to the Hospital
“Going to the hospital is not a death sentence. The hospital is a safe place to be.” Dr. David Price
When should you go to the hospital? When you’re feeling short of breath. Not if you have a fever or have body aches, etc.
People feeling short of breath are short of breath for 5-7 days and then can go home. About 10% people with COVID-19 get short of breath and need to go to the hospital (10% of all infected). Of those who need to be in a hospital, 1-3% end up on a ventilator. When people get so short of breath that they can’t get to the bathroom, we put them on the ventilator. Of those, the overwhelming majority come off the ventilator 7-10 days later.
(The early studies are not so promising – thanks Richard. Price did say they are learning more and more all the time and are presumably getting better at keeping people alive. On the ICU subject the CDC recently reported that 78 percent of patients in the ICU had a pre-existing condition such as heart or lung disease or diabetes.)
With regard to younger people getting sick. Except for people 0-14, younger people are getting sick, are going to the hospital, and are being put on ventilators as well. Price said
“We (in the ICU) see a bit more older people, but we get a ton of 35-year olds. We see young people who get really sick and we see older people who do just fine.”
His hospital is not using ibuprofen – it’s using acetaminophen.
Laura Hillenbrand’s Probable COVID-19 Experience
Laura Hillenbrand, the author of Seabiscuit and Unbroken, both of which were made into films, vividly (of course) describes her harrowing descent into coronavirus hell on a Facebook post. She describes feeling short of breath and flu-like symptoms first, having the shortness of breath resolve temporarily, and then come roaring back:
“It began with a strange shortness of breath. I couldn’t seem to get a full breath of air, and found myself panting. I had a constant urge to cough. Friends commented on the odd hiss in my breathing, and the brevity of each breath I took. I was winded just having a casual conversation. My throat was raw…My muscles ached and I was perpetually chilled, sometimes shaking. My lymph nodes were swollen and painful. I had no congestion, yet my chest felt as if it were wrapped in duct tape, and I was breathing through gauze. This was nothing like the flu, or anything else I’d ever had.”
One takeaway is that Laura didn’t know how dangerously ill she was until a pulse oximeter reading indicated the oxygen saturation of her blood was 89 – way below the cutoff point – 92 – for getting checked out in the hospital. That morning, she was lightheaded and was “gasping wheezily” to get air, and was then directed to go straight to the emergency room. After testing negative for the virus (very likely a false negative) she was given a breathing medication and returned home. As of a couple of days ago, she was doing better but was still sick.
She didn’t mention ME/CFS in her post. To my knowledge, she hasn’t referred to it much for years, and it wasn’t clear if she still has it or not. She said she was not in a high risk group, doesn’t have a compromised immune system and called herself “fit”. Perhaps she’s recovered.
Still, she provided a cautionary tale for everyone – and a good reason to possibly get a pulse oximeter. (Note that they may not be completely accurate.)
One doctor advised that if you’re taking 12-18 breaths per minute, or if you can speak in full sentences and are not feeling short of breath, you probably have enough oxygen in your blood.
- Update! – Laura talks with an Oregon newspaper about her coronavirus experience.
Treatment Updates
No study results are in, but the news – the really big news – is the enormous number of studies underway. Clinicaltrials.gov lists over 230 trials (50 in the last day!) involving dozens of substances that are underway or about to get underway. In just a couple of days, the number of hydroxychloroquine and IV plasma studies, for instance, jumped into the high teens.
Check out Health Rising’s new Coronavirus Treatment Page For More.
Two Very Different Treatment Approaches from ME/CFS/FM Practitioners
(Please note that Health Rising does not endorse any treatment approaches and simply presents them for your information.)
Dr. Ian Hyams
Dr. Ian Hyms is the medical director of the Pain and Fatigue Clinic in West Vancouver, BC., and is the Interim Lead of the Complex Chronic Diseases Program at BC Women’s Hospital + Health Centre in British Columbia. He’s also a clinical instructor at the University of British Columbia. He provides an hour-long plus take on COVID-19, ME/CFS, FM and Lyme disease.
Courtney Craig – Nutritionist / Recovered ME/CFS Patient
Courtney Craig was able to use integrative and traditional medicine to recover from ME/CFS, but COVID-19 – that’s an entirely different ballgame. She doesn’t recommend any supplements
“There is NO evidence that any herbal or vitamin product, or dietary measure can prevent or treat this particular corona virus.”
and recommends not taking on a new supplement regimen now.
“Now is not the time to change your routines. Do not attempt a new ME/CFS-specific supplement, dietary plan, or fasting protocol. Keep your condition as stable as possible. Avoid activities that may trigger post-exertional malaise.”
Instead, focus on being as safe and as healthy as possible. Check out her “Chronic fatigue syndrome in the Time of COVID-19” post.
Health Rising’s ME/CFS/FM Doctors Resource Page
Check Health Rising’s ME/CFS/FM Doctors and Researchers Resource page on how to stay safe and support your health.
Say What? A COVID-19 Voice Detector (??)
It sounds space-agey, comes with a bunch of provisos, and is decidedly preliminary but then again, the people who created this app aren’t exactly guys in a diner, either. Researchers from Carnegie Mellon University and other institutions are creating an app they hope will be able to determine if you have COVID-19 just by analyzing your voice. The idea is to determine if signatures in your voice are similar to those found in COVID-19 patients.
Not approved by the FDA or CDC, definitely not a substitute for a medical test – and not available yet – but symptom tracking apps that can show outbreaks in real time are. Check them out on HR’s Coronavirus Apps page.
Jarred Younger Seeking Info on COVID-19 Patients and LDN
From Jarred Younger:
“I am interested to hear of anyone’s experience with COVID-19 while taking LDN. If you were taking LDN and had/have a confirmed or suspected case of COVID-19, let me know how severe your symptoms have been and how long they lasted. You can email me at the address below (please use the email instead of facebook discussion). I don’t know if I will have a chance to respond to everyone, but I will definitely read everything sent. Please forward this on to anyone who might have information to share. Thank you!”
Please email Jarred at youngerlab@uab.edu.
Coronavirus Central – Resources From Health Rising
- Tracking – check out the multiplicity of ways the virus is being tracked: its spread, its infectious rate, the deaths it’s causing, efforts to model its effects.
- Advice From ME/CFS/FM Doctors and Researchers – ME/CFS/FM doctors and researchers give advice.
- Staying Safe – how to stay safe: including hand washing, nasal irrigation, disinfecting, making a mask, plus – is the virus being aerosolized? How long is the virus alive on different surfaces, and does the amount of virus present matter?
- Treatments – Check out the astonishing number of COVID-19 treatment trials underway.
- Apps – be part of the solution; use apps that help us understand the spread of the virus; plus, use apps that can warn you if you’ve been in contact with someone who is infected.
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy? A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?









“…the overwhelming majority come off the ventilator 7-10 days later.”
Hmm, that’s not what’s been seen elsewhere, e.g. in UK where it’s 50-50 death-recovery (dropping lower as time goes on) and many on ventilators for weeks: https://www.icnarc.org/About/Latest-News/2020/04/04/Report-On-2249-Patients-Critically-Ill-With-Covid-19
Good work again thought Cort. 🙂
… Via this article: https://www.npr.org/sections/health-shots/2020/04/02/826105278/ventilators-are-no-panacea-for-critically-ill-covid-19-patients?t=1585967142836
Thanks Richard. I will put that in. I thought it was low. Maybe he’s part of a really skilled group?
I’d love to think this is down to competency, Cort. Very interested to hear what different procedures they’re implementing, if so.
I’ve heard that moving to ITU earlier helps, and treating with hydroxychloroquine earlier probably has some effect (compared to later).
Like Linda B (below), I’m also very very interested to hear follow-up on Vit-C as a therapy. If it has been confirmed to be anywhere near as successful as some of the Chinese studies (and Dr Richard Cheng) have claimed. Linked in this part of my personal blog (just for reference): https://lewyland.blogspot.com/2020/03/covid-19-part-2-daily-updates_29.html#2020-04-02
I know some NY hospitals were trialling it too: https://nypost.com/2020/03/24/new-york-hospitals-treating-coronavirus-patients-with-vitamin-c/
I suspect that the threshold for being in hospital or being in hospital and on a ventilator may be different in the UK and America. In the Uk you will not be in an ICU unless you are a Prime Minister or you need to be on a ventilator, in which case you are in a medially induced coma. If you dont need that you’ll be in a makeshift coronavirus ward possibly with a Continous Positive Airway Pressure machine and an oxygen supply or sent home maybe with oxygen.
People do stay on ventilators for weeks here but your chance of survival goes down if you are on for more than 7 days. Maybe in America you dont make it to ICU if you only have a 50/50 chance of survival?
This article discusses the over active immune system response to Covid 19 that turns fatal quickly. It made me wonder if those of us with over active immune responses are more at risk. This article discusses successful use of immune suppressing drugs with severe Covid…
Why Some COVID-19 Patients Crash: The Body’s Immune System Might Be To Blame
https://www.npr.org/sections/health-shots/2020/04/07/828091467/why-some-covid-19-patients-crash-the-bodys-immune-system-might-be-to-blame
Once again thank you Cort for great reporting
I have read that in some US hospitals they are ‘pre-treating’ those who present with severe symptoms with high dose IV vitamin C…..seriously high doses. These patients are responding much better and are off ventilations in a few days with sustained Vit C treatment over the time.
This treatment finally seems to be gaining some foothold in medical arenas. It has been around for years.
Dr Brownstein (USA) is also having success with a nebulizing treatment and some supplements. Vit A keeps coming up a lot.
Unfortunately, to complicate matters just slightly…the hydrogen peroxide added to his nebulizing formula is something they mix ‘in his office’ …they add minerals? to the mix. At a pinch one of his videos describes how to mix this yourself (or someone do it for you if you’re not well).
In Australia we have the ‘fortunate’ circumstance of being behind so many other countries and are trying to do better what other countries have learned at such a great cost.
But…winter is coming here…this is not over yet and as the blog points out the Spanish flu epidemic came in waves….my gut tells me we are facing a similar circumstance.
Keep safe, stay alone but stay connected. All we can do is hope for ‘the best outcome we can manage’ …so do all you can do is your best to help each other and not increase the spread..
CNN reported yesterday that two thirds of patients put on a ventilator die. This was during the discussion of Boris Johnson in hospital..
Additionally, Courtney Craig advising people NOT to take supplements seems silly and dangerous. At the very least vitamin D optimization fights viral infections, and Vitamin C, especially IV C, can fight viral infections and sepsis. Why encourage people not to take supplements?
I’ve had moderate to sometimes severe ME/CFS for ten plus years. This past year I have made big improvements but for over two weeks, I have been holding down the fort at home looking after my husband with positive Covid and daughter with a presumed case.
I have no idea if my immune system is still in overdrive or not. Do I have it and not showing the typical symptoms? they won’t test me so I will never know. Both hubby and daughter haven’t had any fever.
Nat, all hail to you, good wife and mother.
I seriously hope your immune system is helping you avoid the dreaded Covid-19.
Good luck. Remember…it takes No1 to look after No2 and No3…so remember to put yourself at the top of the list.
Thank you Linda B you are absolutely right ?
Good luck, Nat!
I wish I could remember where I read this, some interview with Laura Hillenbrand, but she said she had found that some of the experimental drug treatments had worked with her CFS/ME and she wanted others who had it to know that there was help on the way. Must have been maybe 2-4 years ago. If I can track it down I will. I had the impression she felt she was largely or completely recovered now.
Wow…..would like to know about that.
I would like to know what Hildebrandt treatment was as well. And where she got the treatment. And why this information isn’t being shouted from the rooftops?!!? Thanks
I would also love to hear more about this…
I would love to know how Laura Hillenbrand recovered. I’ve been very ill with CFS over 2 decades. If there are treatments that work, we need to be sharing that information widely.
Laura Hillenbrand wrote this 4 days ago in a comment below her Facebook post last week sharing she thinks she has CoVid 19. It suggests to me she doesn’t view herself as fully recovered. She had though seemed to have made significant improvements in the last few years. I too would be very interested to know if this was due to any new medications. Her Facebook comment:
“I do not have fibromyalgia. I have ME/CFS. Patients with ME/CFS are not officially classified as a high risk group for this virus. There are a host of marked immune abnormalities in all patients with ME/CFS, but our responses to infections differ dramatically. Many ME/CFS patients clearly have impaired immunity and for them, this pandemic is especially frightening, and they are indeed at high risk. Any virus can devastate their bodies. I appear to fall into the subgroup of patients whose immune systems are dramatically *over*active. I generally throw off viruses almost instantly. I have been in very close contact with people who have totally disabling flu and I don’t become sick. I don’t get colds even when living with someone who has one. I know other ME/CFS patients who have gone decades without contracting a single virus. So while I have less energy than a healthy person to deal with COVID — and I am indeed absolutely exhausted — I don’t believe I am at special risk of complications and death from COVID, as diabetics, the elderly, and those with cardiovascular, kidney, lung, and liver disease are.”
Mystery solved! Thanks. As neither the About section of her Facebook page or her book publisher mention the fact that she has ME/CFS, I thought she had left if behind her. Unfortunately, not. Her exhaustion continues. It’s amazing she can write the way she does with it and her other symptoms.
I am glad the info was helpful. It is amazing what she has achieved whilst being ill with ME. I do get the impression she has improved in recent years at least.
This information and those two videos were so helpful! I had questions regarding if I should restart the Imunovir and about the LDN. The video from Dr. Hyms answered all of my questions. Also Cort the verdict is in and you must secure an interview with Hillenbrand! I know you can do it ???
:)I would love to and I’ve tried. No luck so far but you never know…:)
I have not followed Laura Hillenbrand on face book, so thanks for sharing her post. The last thing I knew from her was the interview published in summer 2016, almost 4 years ago, by Stanford Medicine, where she said, referring to her trip across the US the year before, “What I experienced was an overwhelming sense of gratitude because I had been set free. I was not well. I am not well. I am always dealing with symptoms, but I was free enough to have that experience, to see America.” (‘am’ was italicized in the article.)
Source is Costello, Paul (Summer 2016). “Leaving frailty behind: A conversation with Laura Hillenbrand”. Stanford Medicine. Retrieved September 4, 2016. http://stanmed.stanford.edu/2016summer/leaving-frailty-behind.html It is a source for the Wikipedia article about her. I got the idea she still watches herself, but through diligent efforts over two years, she broke the worst constraints that the disease imposed on her, which was a huge change in her life. Doctors do not know if M.E./CFS makes a person immune compromised, or if we fall in a group, like people with diabetes, that seems to be less able to survive a bout with covid-19. Plus she was speaking of covid-19, not M.E.
Thanks! She really opened up there. I had forgotten about that.
is there a clickable link in the menu or at very bottom of this page for the how to?
make masks, disinfect, …….
and the apps and maps with # cases etc.?
Would be cool if a banner at start when open website to click on——and then also each with a gist short box.
Though as is often said,
——can’t take care of others unless you take care of yourself…….
and you Cort have been in overdrive for some time and have been making a large difference.
acronym:
C.O.R.T.
creating
outstanding
resources
today
🙂 Thanks!
Here’s the link to Staying Safe page – https://www.healthrising.org/coronavirus-resource-central/safety-practices/
Didn’t get to the Gist this time – too tired but am planning to put a banner on the website.
Many ME and POTS patiënts are also short of breath and have airhunger. So what is the different with COVID19. Fever, caugh?
I would guess so. Fever is apparently present in about 90% of people with COVID-19. I wonder if the pulse oximeter would be helpful for people with breathing issues and ME/CFS if their blood oxygen levels tend to be in the normal range.
The difference is being so out of breath that you can barely hold a conversation. And I suspect the 90% may not apply to ME/CFS patients. Neither myself nor my friend who got it from me had any fever at all but still had very bad breathing and lung problems (for 5+ weeks now though things are improving). I had severe chills at times which according to my doctor is my body trying to fight the virus, even without a measured fever. I do normally get a fever when fighting a flu or severe cold so this was unusual.
Thanks for this. I have watched Dr Mark Price’s video, however, I am little confused by some of it and would be interested in hearing other people’s interpretations of the info he shared. He said the vast majority who get CoVid 19 are people who have sustained contact with an infected person using the example of shaking the hands of the infected person and then touching their hands to their face. He also said another way you possibly get it (he seemed to suggest this wasn’t as definite as the physical contact) is by long sustained contact (15-30 mins or more) with someone who has the disease. I was confused by him using the word sustained for both physical contact with an infected person and sustained contact by talking to someone for 15-30 mins or more. I interpret the word sustain as a longer period of time, yet he uses it also in the example of shaking hands with an infected person?
I also picked up though he said you can get it by touching surfaces he thought this was a lower risk than touching someone physically? I was again confused when he said this isn’t an illness that say a community of ten gets by touching a spot an infected person touched? Surely if they all touched it they would, or does he mean enough people touch an area that has virus particles on it the particles would die after a few touches? Many thanks
I know what you mean. The way I interpret it is that most people get it through sustained contact with an infected person but you can get it through brief contact including touching a doorknob say,- so be careful both ways. Shrink your social circle – don’t put yourself in situations where you’re in sustained contact with anyone and diligently wash your hands, clean surfaces, don’t touch your face, etc.
Another expert quantifies sustained contact as just speaking to someone face to face with the virus. I don’t have the feeling that Price goes that far.
Thanks for giving your interpretation. I need to have carers visit daily so I am most interested in the debate of whether the virus can linger in the air. I still chat to my carer with her standing at a distance when she is in my bedroom (she does wear a surgical mask) and I wonder whether I should. Dr Price seems to think there is low probability for that whilst others in the medical field think it is more likely.
Cort, why did you say, “After testing negative (Laura Hillenbrand) for the virus (very likely a false negative) she was given a breathing medication and returned home.”
Do you believe, in general, that there is a high false negative rate? Otherwise we have to remind ourselves that way more people test negative than test positive and that is with careful screening of who can get tested. I think most places you have to have symptoms and test negative for the flu to even get a COVID test? And still, in WA they say they have an 8% to 9% positive rate for COVID. I have been tracking it here in Louisiana for the past 14 days and we are showing between 13% and %21 positive for COVID. We are getting slammed here in Louisiana and still a very large portion of people tested do not have COVID.
I haven’t been able to find any definite false positive and now that so many tests are being used I don’t know if we’ll ever know. Laura’s symptoms were so COVID-like, and so unlike her usual symptoms or other flu symptoms that personally I would be shocked if she didn’t have a false negative. Hopefully, she’ll get an antibody test later and let everyone know.
Check this out (https://www.advisory.com/daily-briefing/2020/04/06/false-negative)
“Ultimately, Bill Miller, a physician and epidemiologist at the Ohio State University, said, “The whole testing field is in flux.” He explained that the majority of the tests are “going through a really rapid validation process,” due to increasing demand, and “[a]s a result we can’t be completely confident in how they will perform.”
and…
“based on the available information, Mike Lozano, an executive at Envision Healthcare, estimates the sensitivity of currently available tests appears to be lower than comparable tests—likely around 70%, which means nearly one-third of patients who have the virus receive a false negative.”
Having a false negative doesn’t necessarily mean the test was off. The swab could have been applied improperly or the test transported incorrectly. If I remember correctly it may have been applied correctly in Laura’s case – back of the throat.
Some doctors whose patients are testing negative are later seeing some of those patients end up in the hospital…those are most likely COVID-19 patients.
According to that article so long as anyone is still symptomatic – even if they have a negative test – they should quarantine themselves.
You’re in a real hotspot in Lousiana – good luck!
My doctor has said her experience has been about 25% false negative for the nasal swab test (through Labcorp or Quest). The test can be negative for many reasons including to little virus in the location tested (it maybe in the lungs not the nose), too long after infection and the person is not longer shedding significant amount of the virus, and improper collection or handling of the sample.
And remember that the tests for Covid19 are only 70% accurate.
This may be useful
https://www.youtube.com/watch?feature=youtu.be&v=u7sJw5ecFUU&app=desktop&fbclid=IwAR3R9lG9fETZ4LI26zenvJGIalu01yx1FgQ_PdKA_HzBDWIHKXVSj-uGWh4
Hi Cort, I am an NP. I found Dr. Price’s presentation misleading and inaccurate. He made this video at home; not from the institution where he works. Maybe he was emotionally and physically exhausted.
Nansy, I found some of Dr Price’s comments confusing, see my comment above. Are you able to share which of his comments you believe are misleading? Thank you.
He seems very confident doesn’t he! I hope he’s right. I’m just being careful whenever I am around people. I’m wearing my triple ply t-shirt mask, staying as briefly as possible, and washing my hands and everything they touch… This bug is too nasty to take a chance.
Hi Cort, I’d love to see an article about Natural Killer Cells and CD 8 T cells which seem to be very correlated with Covid19 prognosis. Considering these are areas that are badly affected by ME I’d think these studies would be highly significant to our population. https://www.nature.com/articles/s41423-020-0402-2?proof=trueIn%25EF%25BB%25BF
Masks have been criticized before and with President Trump recommending cloth masks he is giving a false impression. If you are near an infected person with a mask on who then coughs into the mask, you will probably get a dose of virus:
A small study from South Korea cast doubt on the ability of surgical or cotton face masks to effectively prevent dissemination of COVID-19 from the coughs of infected patients.
Median viral loads were negligible when comparing coughing samples of COVID-19 patients without a mask, with a surgical mask, and with a cloth mask, suggesting these masks were ineffective at filtering SARS-CoV-2, the virus that causes COVID-19, reported Sung-Han Kim, MD, of University of Ulsan College of Medicine in Seoul, South Korea, and colleagues.
In a letter published in Annals of Internal Medicine, they cited the size of viral particles as a possible reason for masks’ poor ability to filter the virus, despite their effectiveness against other respiratory infections. In particular, prior studies found surgical masks, as well as N95 respirators (which were not tested in the current analysis), help prevent dissemination of influenza virus.
Citing concern about asymptomatic and pre-symptomatic spread of COVID-19, the CDC recommended late Friday night that all Americans should wear cloth masks in public.
Kim and colleagues examined data from four COVID-19 patients admitted to negative pressure isolation rooms. They were instructed to cough five times each onto separate petri dishes while wearing no mask, a surgical mask, a reusable 100% cotton mask, and no mask again.
Nasopharyngeal and saliva samples had a median viral load of 5.66 log copies/mL and 4.00 log copies/mL, respectively. However, median viral loads for patients without a mask, with a surgical mask, and with a cotton mask were 2.56 log copies/mL, 2.42 log copies/mL, and 1.85 log copies/mL, respectively. Interestingly, swabs from the outside of the mask were positive for SARS-CoV-2, while most swabs from the inside of the mask were negative, the authors said.
The authors pointed to earlier research showing particles 0.04 to 0.2 μm “can penetrate surgical masks.” For the coronavirus responsible for SARS, particles were estimated to be within that range at 0.08 to 0.14 μm, they said.
“Assuming that SARS-CoV-2 has a similar size, surgical masks are unlikely to effectively filter this virus,” they wrote. “The size and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.”
When noting greater contamination on the outside versus the inside of the mask, they speculated it may be due to “the mask’s aerodynamic features” or “the small aerosols of SARS-CoV-2 generated during a high-velocity cough might penetrate the masks.” The finding reinforces the importance of hand hygiene after touching the outside of masks, Kim and colleagues suggested.
The researchers acknowledged that the study didn’t examine actual transmission of COVID-19 illness nor whether the masks “shorten the travel distance of droplets during coughing.”
Whether face masks decrease transmission from asymptomatic individuals with COVID-19 or those who are not coughing needs further study, they added.
Disclosures
This study was supported by a grant from the government-wide R&D Fund Project for Infectious Disease Research (GFID), Republic of Korea.
The authors disclosed no conflicts of interest.
Primary Source
Annals of Internal Medicine
Source Reference: Bae S, et al “Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients” Ann Intern Med 2020; DOI: 10.7326/M20-1342.
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30134-X/fulltext
wearing the correct mouth masks when used properly will help reduce the risk of corona contamination.
Nothing in the lancet article contradicts the above article. The point is that an infected person wearing a mask can contaminate the air outside of the mask and even surfaces if close enough. I have worn surgical masks many times and I know these would not be sufficient to contain virus if the wearer coughed forcibly ( as they would if they had a coronavirus infection).
Masks are likely to slow the distance a cough or sneeze travels and therefore reduce infection as long as you dont touch them – the mask an infected person wears protects you, your mask doesnt protect you. Maybe soaking part of the mask in brine and then letting it dry might help https://www.sciencedaily.com/releases/2017/01/170105160228.htm
Be wary of filters. Some of those suggested may include harmful substances .
“the mask an infected person wears protects you”
To a degree but social distancing remains very important. I have seen people wearing masks getting very close to each other – possibly because they think the masks are adequate protection – they are not!
i agree it isn’t 100% safe but it will help to protect you for some degree otherwise the medical people didn’t wear them anymore. Also a professor in Hongkong did this statement after a study last week.
Also – if you live with someone who uses a CAP machine for sleep apnoea or similar you need to know that they aerosolise coronairus so need to be very careful about isolation
Leaving the subject of Covid-19 for the moment and getting back to ME/CFS, I just posted a very interesting study on a new treatment for gut bacteria that can lead to leaky gut and to problems associated with autism and perhaps ME/CFS.
https://safeminds.org/research/positive-results-from-a-microbiome-treatment-trial-for-autism/?utm_source=mc
Coagulation problems and Covid-19
I think it is very interesting that anticoagulants are being given to Covid-19 patients. The very first medication I was given in 1985 was an form of heparin that came from Germany under the orphan drug act.
https://www.medpagetoday.com/infectiousdisease/covid19/85865?utm_source=Sailthru&utm_medium=email&utm_campaign=Weekly%20Review%202020-04-12&utm_term=NL_DHE_Weekly_Active
Cort why has there been no mention of Dr. Prusty and his work yet? I know this thread is not about Prusty but wondering why you have not written a word about his research? Can you please give us your opinion as Covid will pass but we here who have been suffering for decades in the house will be suffering after covid passes. Why no mention of Dr. prusty please?
I did a blog on Prusty’s Ramsay Award win I think it was but that was some time ago and I keep hearing good things but I’m a bit out of the loop. I can promise a blog coming up on him and his work with Bob Naviaux, though. It seeems like really exciting stuff.:)
thanks cort for your answer. thank you for all you have and continue to do for us here with this horrible disease.
god bless
jimmy
I really appreciate all of the information I have received over the years through HealthRising.
Now, more than ever!
In gratitude,
Melanie Rincon
Thanks Melanie. 🙂
Wow, Cort. The world you and Dr Price are talking about is totally different from the world we’re living in in NY. Eg, 80% of people who go onto respirators die. I guess the regional difference in experience and information is far greater than we know here in NY.
NYT had a good article today in what doctors know about corona virus that they didn’t know a month ago. NY Governor Cuomo’s daily news conferences are also very informative. NPR ran a story this morning about the extremely high unreliability rate of the current tests, especially the antibodies tests.
Please note that I reported on what Dr. Price said. Those were his words not mine. He was also referring to his experience in a New York ICU! Eventually we’ll have the right stats which I acknowledge certainly appear to be more negative than he reported.
Hyams says things but can he prove what he says helps ME/CFS?
This information and those two videos were so helpful! I had questions regarding if I should restart the Imunovir and about the LDN. The video from Dr. Hyms answered all of my questions. Also Cort the verdict is in and you must secure an interview with Hillenbrand! I know you can do it