

It’s complex; it causes fatigue, pain, sleep and cognitive problems; it’s underfunded; and it’s not chronic fatigue syndrome (ME/CFS) or fibromyalgia (FM) – it’s Gulf War IIlness (GWI) – and it may be more relevant than you think.
We do have quite a bit in common. Imagine being healthy and strong, and then suddenly not being that way and then staying that way for decades. We can relate.

It took less than a week for Coalition ground forces to prevail during the first Gulf War, but nearly three decades later many are still suffering
It’s a remarkable thing that several wars and almost 3 decades later, about 30% of Gulf War Veterans are still sick. That’s obviously not what they signed up for, but then again we never signed up for fibromyalgia (FM) or chronic fatigue syndrome (ME/CFS) either. This study points to ways, though, that we may all be able to help each other.
Few disorders cause such a wide range of often debilitating symptoms as GWI – and few fit so well with ME/CFS and FM. While GWI was initiated by a toxic trigger, it’s very possible that whatever is causing the fatigue, pain, sleep and cognitive problems in GWI is also causing them in ME/CFS and FM.
Nancy Klimas’s clinical trials for GWI and ME/CFS, it should be noted, are employing the same drug combination. Despite the dramatic differences in immune networking that she’s found between GWI and ME/CFS, her models are telling her the same drug combination should work in both.
Jarred Younger believes that small tweaks in the microglia – the cells believed to be causing the neuroinflammation – could easily account for the slightly different symptoms found in these diseases.
The idea is that something – an infection, toxins, some stressor – primed the microglia in these diseases to become hyper-reactive and continuously pump out a vast array of nasty substances (reactive oxygen and nitrogen species (free radicals), cytokines, chemokines, inflammatory prostaglandins, proteases, excitotoxins, glutamate) that are causing pain, fatigue, etc. Once they’re primed, it just takes little, little stressors to keep them going.
Getting them primed may not be so difficult. Animal and human studies suggest that many things – infections, toxins, physical trauma, stress (including high cortisol levels), sleep disturbances, heat – can send glial cells into hyper mode. Interestingly, rodent studies suggest that experiencing a double whammy (e.g. being exposed to a toxin while you’re being physically or emotionally stressed) can really send your glial cells into a tizzy.
The Study
In-vivo imaging of neuroinflammation in veterans with Gulf War illness ZeynabAlshelha1Daniel S.Albrechta, CourtneyBergana, Oluwaseun Akejub, Daniel J. Clauw, Lisa Conboy, Robert R.Edward, Michael Kim, Yvonne C.Lee, Ekaterina Protsenko, Vitaly Napadow Kimberly Sullivan, Marco L. Loggia. Brain, Behavior, and Immunity. https://doi.org/10.1016/j.bbi.2020.01.020
The study (15 GWI and 33 healthy controls, including 8 healthy veterans of the Gulf War) used positron emission tomography (PET) and a radioligand called [11C]PBR28 which binds to a mitochondrial protein (TSPO) that becomes dramatically increased during microglia/macrophage and reactive astrocyte activation. It’s considered a surrogate marker of neuroinflammation.
(Note that activated macrophages in the brain would produce the same signal. Macrophages should not be found in the brain – they belong in the body – but if they get into the brain though a leaky blood-brain-barrier (BBB), they can cause a lot of trouble. Jarred Younger is currently assessing that possibility in ME/CFS. (Past research suggests that the BBB has been compromised in GWI.))
Marco Loggia, PhD, a Harvard neuroscientist and senior author of the study, has been focused on understanding the relationship between the brain and pain. In 2016 Loggia, a leader in the field, wrote “In Vivo Imaging of Human Neuroinflammation“, which provided “an overview of state-of-the-art techniques for imaging human neuroinflammation”.
Despite the fact that GWI and fibromyalgia are triggered by very different events, Loggia hypothesized that given the huge overlap in symptoms the same pattern of neuroinflammation would prevail.
Results
He was right.
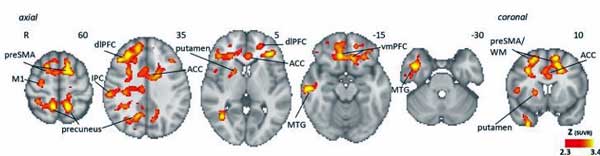
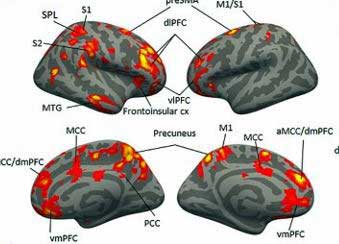
The first neuroinflammation study ever done in GWI found evidence of neuroinflammation throughout the cortical or outer areas of the brain (precuneus, prefrontal cortex, and primary motor and somatosensory areas), as well as underlying white matter and the basal ganglia. The cortical areas of the brain are involved in ‘higher-order’ functions, such as memory, concentration and reasoning.
That made sense given the cognitive issues in GWI, but the key finding may be the unusually widespread nature of the neuroinflammation – and the similarity to other findings in fibromyalgia, chronic fatigue syndrome (ME/CFS) and migraine.
It should be noted that neuroinflammation doesn’t have to be widespread to be devastating. Loggia found neuroinflammation in Huntington’s disease in the basal ganglia. Loggia’s amyotrophic lateral sclerosis (ALS) study found neuroinflammation in the primary motor cortex. His multiple sclerosis study found neuroinflammation in the cerebellum or hindbrain.
Compare that to the long roll call of apparently inflamed brain areas in Gulf War Syndrome: the precuneus, prefrontal cortex, the primary motor and somatosensory areas, and the basal ganglia, as well as underlying white matter.
They’re almost identical to the inflamed areas Loggia found in his 2019 fibromyalgia study: prefrontal cortex, primary somatosensory and motor cortices, precuneus, posterior cingulate cortex, supplementary motor area, supramarginal gyrus, and superior parietal lobule. With different methods showing evidence of neuroinflammation in FM in different ways, that finding is looking pretty robust.
FM is common in migraine as well, and Loggia’s migraine study also found evidence of widespread neuroinflammation (thalamus and primary/secondary somatosensory, insular cortex, visual cortex, basal ganglia) with quite an overlap with both FM and GWI.
Not surprisingly, Watanabe’s small 2014 PET chronic fatigue syndrome (ME/CFS) study also found widespread signs of neuroinflammation (cingulate cortex, hippocampus, amygdala, thalamus, midbrain, and pons).
Younger’s 2020 ME/CFS neuroinflammation study used a different method, but Younger’s heat mapping study came to the same conclusion: large areas of the brain (right insula, basal ganglia, frontal cortex, thalamus, and the cerebellum) appear to be inflamed.
Compare those findings to the quite restricted neuroinflammation found in low back pain (thalamus and somatosensory cortices). Apparently, it takes much more neuroinflammation to produce the wide range of symptoms (pain, fatigue, sleep, cognitive, sensory) found in FM, ME/CFS, GWI and migraine than to produce chronic low back pain.
The Gist
- Neuroinflammation refers to an excess of immune activity in the brain.
- It can be caused by glial and/or astrocyte activation but in ME/CFS and FM is believed to mostly concern glial cells.
- Hyper-active glial cells can pump out an astounding number of pro-inflammatory substances including cytokines, chemokines, prostaglandins and excitotoxins to name a few.
- After a Harvard neuroscientist, Marco Loggia PhD, found neuroinflammation in fibromyalgia he went after Gulf War Illness and found almost exactly the same pattern: widespread neuroinflammation in the cortical or upper brain areas.
- While some serious diseases such as ALS and MS have very localized patterns of neuroinflammation, similar patterns of widespread neuroinflammation have been found in migraine and chronic fatigue syndrome (ME/CFS).
- Loggia has also found neuroinflammation in many other diseases including autism, depression, anxiety, Huntington’s diseases and Parkinson’s.
- With so many diseases demonstrating that neuroinflammation is present, the race is on to find drugs or other means to tamp the immune fires of the brain down.
With several studies that have used different methods to find evidence of neuroinflammation in fibromyalgia, that finding is getting pretty robust.
It’s hard to imagine that Loggia is not right about inflamed brains causing problems. The FM, GWI and ME/CFS studies, after all, found no evidence at all of neuroinflammation in the healthy controls. It’s only showing up in people with diseases, and right now with the widespread neuroinflammation findings, people with GWI, FM, ME/CFS and migraine are sticking out like a sore thumb.
With improved scans the field seems to be booming: neuroinflammation has only shown up in PET scans in FM, GWI and migraine in the last year (thank you very much Mr. Loggia),
The wide range of neuroinflammation findings should spell good news for potential treatments. Loggia hoped the GWI findings “could help motivate a more aggressive evaluation of neuroinflammation as a potential therapeutic target.” On the ME/CFS/FM side Jarred Younger’s been hot on the trail of possible neuroinflammation treatments, but we need to keep our eyes open outside the field for the other possible treatments that will surely pop up.
Neuroinflammation is a known factor in epilepsy, for instance. A 2019 Nature review targeted four potential neuroinflammatory pathways to attack (IL-1 TLR-4 axis, arachidonic acid–prostaglandin cascade, oxidative stress and transforming growth factor-β) at least three of which have been discussed in ME/CFS or FM. Neuroinflammation has become a major field in Alzheimer’s research as well. The need to develop effective anti-inflammatories for the brain is clearer than ever, and with ME/CFS, FM and GWI joining the neuroinflammatory disease clique, hopefully they will benefit as well.
For More on Neuroinflammation in Fibromyalgia:
- Genes May Be Causing Neuroinflammation and Pain in Fibromyalgia
- The Brain Game: The Search for Neuroinflammation in ME/CFS and Fibromyalgia
- Fibromyalgia – Neuroinflammatory Disease? Savella – Anti-inflammatory?
- The Neuroinflammation Man: Jarred Younger on Inflammation
- Low Dose Naltrexone, Inflammation and Pain: A Different Approach to Fibromyalgia
- Microglial Inhibiting Drugs and Botanicals to Combat Neuroinflammation






I’ve been thinking about the “novelty effect” that allows me to do more without crashing when in a new environment or while traveling or doing a new thing. Then I found a paper that says dopamine down-regulates microglial cells.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6141656/
Maybe the sense of accomplishment that Dean Anderson talked about as being helpful works the same way.
Interesting. I have mild CFS but yes have often felt better and more energized when traveling, or doing new things.
I must have missed the “new environment” benefit in the article, but it applies to my experiences as well. When I travel out west, the travel and elevation cause significantly increased fatigue for a day or two, but then I rebound and am able to enjoy the rest of my vacation time.
I noticed the same thing when I still able to go to my now ex”s home on weekends. I felt better than ever on the second and third day.. even falling asleep at a normal hour, staying asleep and waking with the stiff joints of FMS, but free of the excruciating pain and brain fog that takes over an hour to shake daily at home. I came to wonder what the deal was, because it was consistent and profound.
Fascinating that others have experienced this.
You may also find it interesting the connections to dopamine, glutamate and histamine. The latest thing, is finding histamine at the H3R (receptor) to be helping Alzheimer’s. There is a close connection to it and dopamine. And also glutamate as a help with cognitive function. But getting things in proper balance is a whole other topic.
My having pretty severe MCAS and trying to get my histamine receptors to work properly has been a real challenge. Finding out that Histamine blockers was probably one of the worst things I did for my brain. Resetting function after over 8 years of daily use has been a challenge to say the least. But now things are working better and my brain is back in the “on” position. I actually used external histamine cream to trigger a response of my H2R and H3R receptors. Therefore not causing a H1R response as the need of histamine to activate those. (I know that sounds like a foreign language to those who don’t know how the receptors work and what activates each in the cascade to turn on or turn off. But it is fascinating research.) And I also feel is a key point/part to our issues.
Histamine can also moderate the autoimmune system with regulation of our T Cells. But there again comes in the need to regulate it and how much of it is in the body. We don’t want too much either. But we do need some.
https://www.nature.com/articles/s41598-019-44816-w
It just makes sense. I think Alex Howard calls it “environmental fatigue” or something like that where being in the same environment all the time is fatiguing in itself. You think of the difficulty of being in solitary confinement in prison. It’s not so different for many with ME/CFS
You could certainly explain that with regards to neuroplasticity – neurons that fire together wire together – when neuronal pathways stop being used they start to die off. Being in the same environment all the time means less and less stimulation – and probably very little positive stimulation. Finding ways to introduce forms of positive, not too stimulating forms of stimulation for those who are bedridden would surely help a bit. For others finding way to introduce new things would be good too.
I’ve definitely noticed a sort of energy stream I find I can tap into now, especially when I’m engaged with other people who are on my wavelength, in a beautiful natural environment, listening or watching something fascinating/inspiring on the radio/TV. This happens spontaneously, it’s not something I can consciously conjure up. It’s a mental/emotional energy I’m referring to.
However negative stress can, on the other hand, completely wipe me out.
But I think this is only possible now, as I’ve generally improved. I remember Tim’s comment from the Sleep blog, saying he believed he didn’t have enough energy to sleep deeply and that stuck with me.
There were times over the years from 2016 to early 2019, when I felt like I didn’t really have enough energy to run all the systems in my body and live in the world. At my worst even thinking, (particularly if there was any kind of negative stress attached) would seemingly take me into a deficit of energy. At those times I would feel as though I was at the point of shut down. So what I’d have to do was ruthlessly shut people/situations out of my life. It was extraordinary and something I’ve never experienced before.
Thankfully I don’t feel like that anymore and I’m much more resilient.
Yeah it’s really strange. I took 20,000 steps every other day in NYC last November for 9 days and I was fine. In December I started weekly skiing and, for the first 3 weeks, it felt like a complete recovery. Then the novelty faded and I started crashing. I continued skiing and I ended up with a PEM for 4 months, lol. I couldn’t walk a mile without crashing for days. I would’ve gone on a overnight trip somewhere to see if I could get out of it, but then the coronavirus hit and I suffered at home.
maybe a dopamine response?
(increased dopamine)
I used to think microglia was the next big thing in CFS but now am not too sure. I think it more likely that microglial activation is a secondary factor.
I think in a way it has to be. Something after all starts off the hyper-activation. It’s possible, though, that a process that feeds on itself gets started with the microglia and if you can break that process things can go back to normal.
Any particular reasoning? I used to think hypothalamus, the nexus between the body and brain, must be central to CFS. But hypothalamus can’t explain PEM from mental exertion, so now I’m thinking something closer to the end in the chain, like hyperactive microglia, must be at the center.
Not really any particular reasoning, although partly because the research doesn’t seem to have kicked on in the last five years.
My current ‘favourite theory’ is an autoimmune disease, which inflammation and neuroinflammation is secondary to.
The inflammation is important, but I think it’s downstream to the autoimmunity.
So treating the neuroinflammation may reap some reward.
That’s true, theories/studies appear and then nothing concrete ever happens. I guess that is the sorry state of CFS research..
Thank you, Cort, for yet another really excellent article.
Just as Covid-19 is infamous for its debilitating “cytokine storm,” or cascade, the studies noted in this piece identify a _microglia hyper-reactivity storm_.
Ha Ha! Nice catch Elizabeth 🙂
Well I’ll just have to add Marco Loggia PhD to my favourite people’s list. Like Dr Jarred Younger he’s diving right in there, where the regular medical profession won’t go.
I know my brain has suffered from neuroinflammation because it didn’t work properly. I couldn’t wait for a medical professional to tell me, I had to try and sort it out myself.
I did talk to my doctor about it but he smiled and shook his head ?
The obviously neuroinflammatory part of my experience occurred after I was extremely unwell with a flu in 2017, with a temp of 105/41. After that certain foods would set my brain off – processed, high sugar etc.
Since then, after a lot of experimentation, I’ve managed to calm my brain down. Not a medical professional in sight!
I did find that Ibuprofen worked for a while until I developed a problem with it – my heart rhythm goes all over the place. But that gave me a clue – I needed to bring my level of inflammation down.
So I have managed to do that through diet, reducing my stress levels, getting better sleep and taking supplements – like Omega 3. I sprinkle Turmeric on my food and eat loads of green vegetables.
My brain can still be set off. A few weeks ago I ate some oats – that irritated my gut and my brain. Too much wheat also has the same effect.
However, I constantly have a problem with trying to get energy to my brain. The rest of my body isn’t too bad. But as the brain runs everything, if that goes down so do I.
Something has definitely gone wrong with the energy levels in my brain. I have to quite deliberately monitor my brain energy. I’m quite nervous of it, as my available brain energy can drop very fast.
Now this is not an anti-inflammatory answer but I find chocolate chip cookies give me instant brain energy. Yes, I know all the reasons I shouldn’t be eating them but – they work. Now I’m not good at limiting the dosage! And too many also sets my brain off.
I wonder whether, like above, that dopamine plays a part?
I definitely feel like my brain is inflamed, that’s exactly how i described it to my dr. They then looked at me like I was mad? ?
Well if Jared Younger is right it actually is a bit hotter than normal ?
Not patient centred care Kirsten…
Cort, do you literally mean hotter in temperature..than normal?
There was a sportsman in Australia who suffered debilitating CFS suddenly. It took him about a year to shake it and part of his treatment was ice baths! Plus he eventually promoted a green powdered veg drink of some kind which was also used.
Perhaps people have comments if they feel better in cooler weather?
(My daughter reckons she functions better in winter in many ways…but we live in ?Australia…so summer is pretty hot and winter is not outstandingly cold!)
Hi LindaB,
Jarred Younger PhD has been investigating brain temperature, amongst other things.
You can watch him talk about his ideas at one of the Open Medicine Foundation Symposium (2018). I’m hopeless at the links but if you look for How Brain Inflammation Causes ME/CFS Jarred Younger PhD on You Tube you should find it. That talk is only about 20 mins long and he mentions brain temperature at around 14 mins.
He talks in more detail a few months later (Thursday December 13 2018) in a Solve ME/CFS Initiative webinar called ME/CFS Involves Brain Inflammation Results from a Ramsay Pilot Study Dr Jarred Younger. He mentions brain temperature just past 24 mins.
In one part he says: ‘What we think happens with neuro inflammation is those metabolic processes are going so quickly they generate too much heat – more heat that can be adequately dissipated.
Dr Younger goes on to say ‘and when you get a build up of too much heat in the brain you get cognitive problems, balance problems, mood problems and basically the symptoms of ME/CFS’.
I know you asked Cort and I am obviously not him but I’ve watched these talks by Dr Younger and having various brain issues myself, I thought his talks were very interesting. He also puts the brain on the map, so to speak, and doesn’t shy away from the area.
Hi Tracey Ann.
I appreciate the references. I will certainly Google it to see what I find. I am hoping that they are investigating what they can do to reverse this phenomena!
A ‘hot brain’ sounds ‘cool’ so to speak…but obviously it’s NOT.
My daughter also had a depressed core temperature for a very long time which was amazingly remedied by ONE acupuncture session. Further sessions did not relieve any of the other symptoms. But…thankful for some advancement. Even now though she still gets cold quite quickly and mostly has cold hands and feet!
Sugar ups serotonin. So it gives us a boost to our mood. Thinking before this world crisis is over, there may be many seeking out a diet plan. We all want to feel better and lift our moods. LOL.
Ice cream anyone?
Actually what we really need is SUNSHINE. “always makes me happy”
Sunshine turns off melatonin/histamine and gives us the hormone D3 to help fight off infections, besides it feels so good after being cooped up inside. Twenty minutes is plenty.
Also I think that if I have sort of mild brain inflammation going on, at times, that my brain would probably need more energy than usual.
Whatever I do or not do, I can still run out of brain energy.
cfs medicine possible treatment for corona
…….treatment of sars infected mice gave 100% survival……
https://www.morningstar.com/news/accesswire/579582msn/aim-immunotechs-drug-ampligen-to-be-tested-by-japans-national-institute-of-infectious-diseases-as-a-potential-treatment-for-the-new-sars-coronavirus-sars-cov-2-responsible-for-the-new-human-infectious-disease-covid-19
possiblity of using it with a vaping device…..
https://www.google.ca/amp/s/seekingalpha.com/amp/news/3558704-aim-immunotech-to-investigate-vaping-device-ampligen-for-covidminus-19
corona (prev. said to have ebola insertions )…….. so perhaps additional benefit to using this medicine…
https://www.drugtargetreview.com/news/4095/hemispherx-biopharma-receives-ema-orphan-medicine-designation-for-ampligen-to-treat-ebola/
The organization I direct, Birth Defect Research for Children, has been involved with research on birth defects in the children of Gulf War veterans since 1990 when we began to receive case reports of a rare cranial-facial birth defect in their children in our National Birth Defect Registry. Goldenhar Syndrome, the name for this constellation of birth defects, is very rare, occurring in approximately 1 in 25,000 births. In a short time, we had close to 50 cases in a birth population of 75,000. We had national publicity for our findings and I was invited to present our data to the Presidential Advisory Committee on Gulf War Illnesses. Following this, the Department of Defense funded a study of Gulf War veterans’ children with Goldenhar who were born in military hospitals. They found a tripling of cases. We had cases born in both military and civilian hospitals (about half).
We were then invited to participate in an IRB approved study by the head of epidemiology at the University of Texas, Dallas. This study would be looking at certain genetic factors that prevent the breakdown of organophosphate pesticides and/or nerve gas agents (the grandparents of OP pesticides). This would have been a very exciting study since it evaluated genetic susceptibility; exposure to certain toxins and increases in Goldenhar Syndrome.
Although we completed our part, the study was never finished by UT. There are, however, four published studies that have found Goldenhar and other birth defects linked to fathers’ service in the first Gulf War.
What does this have to do with ME/CFS or Gulf War Syndrome? One exposure of concern in the Gulf was Dursban (chlorpyrifos). It was widely used in the Gulf. In 2001, Dursban was removed from the residential market and it is no longer on the list of approved pesticides for the military. It is still used in agriculture although there have been strong recommendations to take it off the market and this has happened in some states.
Dursban is an interesting pesticide. It has an organophosphate structure in a chlorinated base. The production of all chlorinated chemicals can create the toxic by-product dioxin which has poisoned Vietnam veterans and their children. Dursban also has an unusual reaction with mercury, causing mercury accumulation (in animal testing).
I have more than a passing interest in Dursban. Our home was sprayed inside with Dursban in the early 1980’s for flea control. (This was when it was still on the residential market). I was running BDRC out of our home at the time, but didn’t stay inside when they were spraying.
Since Dursban is chlorinated, it has a long half-life and has been used for termite control for that reason.
I was in the home almost 24/7 and became ill shortly after the spraying, but was not diagnosed till 1984. Our daughter has also been diagnosed with CFS.
I believe that my illness and our daughter’s (and probably that of many others) was caused by a combination of Dursban exposure and HHV-6 A.
Fat-stored chemicals like some components of Dursban can be stored in the brain because each nerve is surrounded by myelin (a fatty substance).
This may explain why exercise, heat, stress, significant weight loss and/or concurrent illness can make you so much worse if you have a toxin-induced form of CFS.
Detoxification can become a dangerous business since once the chemicals are released they will go into the blood stream and settle in other organs like the kidneys and heart. The only safe detox is one that will release the stored chemical(s); bind to them and take them safely out of your body.
Cholestyramine has been used for this in some chemical contamination settings like exposure to Kepone at Allied Chemical Company in the 1970’s and PBB (fire retardant) poisoning of the residents of Michigan also in the 1970’s.
This is not a perfect answer, however, since cholestyramine doesn’t bind to every chemical.
Here are some other interesting facts. The symptoms of exposure to pesticides and other toxic chemicals often mimic the flu and chemicals that can trigger birth defects have historically caused other health problems in some of those exposed.
Thalidomide was kept off the market in the U.S., not because of Dr. Kelsey suspecting that it is would be associated with horrific birth defects, but because it was causing severe, irreversible peripheral neuropathy in some adults who took it.
Wow, Becky! This is almost as informative as Court’s articles. I’d love to see research done on some of this! Thanks!
And Cort – given our level of neuroinflammation – especially those of us who may have 2 or 3 of these often comorbid illnesses showing this wide-spread inflammation in the brain – it is amazing to me that you consistently research, u der stand and summarize all of this for us! Thank you.
Betty,
Given what you write…would the matters of mercury accumulation be compounded by the vaccines required for overseas military service?
Betty and those interested………please check this out XMRV mouse retrovirus STILL IN VACCINES and a known cause of CFS ………oh and note the lying, fraud and blackmail by none other than Dr Facci ……..head of the USA’s Covid Taskforce!!!
https://childrenshealthdefense.org/news/the-truth-about-fauci-featuring-dr-judy-mikovits/
I would also add…my partners uncle served in Korea, Viet nam and in Hiroshima (after the blast) as a medic. His daughter was born with severe heart abnormalities. So sad. And his wife had several miscarriages.
Hi Linda,
That is an interesting thought about mercury accumulation from the vaccines. I don’t think anyone has looked into this.
We have also collected data on children of Vietnam veterans. If you would like to take a look at this go to the Veterans Research of http://www.birthdefects.org
Sadly Betty it’s unfortunate but my Uncle, Aunt and their daughter have all passed away.
I’m in Canada and mercury has been banned from vaccines for years and years now. Has this not been the same for the US? My concerns regarding mercury accumulation is from tuna. Over 20 years ago our paediatrician told us to eat no more than 1 can of tuna per person per month. This is to avoid mercury accumulation.
Personally I think that’s a great idea. I was experiencing numbness in hands and feet – which disappeared after I stopped eating fish regularly.
Hi MC,
Mercury in vaccines is FAR more toxic than Mercury ingested via seafood etc. I think you will also note that when they took the Mercury out of vaccines they increased the Al (Aluminum adjuvant) and another reason why the Autism rate stayed almost the same -remove one neurotoxin and INCREASE another Neurotoxin.
As someone with occasional migraines, and constant anxiety and depression, I found this article to be very interesting.
if we look at the timeline of this illness, there is clearly a “sweeping under the carpet” going on. We need to push for the REAL TRUTH !! The fact that a huge number of vets got this just after vaccines….in china young women got this after HPV vaccines….and i honestly believe ive had this illness since a child, probably after my vaccines, and many years later a complete blow up of my immune system and here i sit a total waste of a life. THE TRUTH NEEDS TO COME OUT