How fibromyalgia, chronic fatigue syndrome and allied diseases are so different from diseases like rheumatoid arthritis
Fibro-fog, brain-fog, chemo-fog… It can get pretty dim out there if you have fibromyalgia (FM), chronic fatigue syndrome (ME/CFS) and environmental illness (EI).

Cognitively speaking – lots of fog out there.
If you have these conditions and feel like you’re having more trouble focusing, paying attention, and processing information – you’re right. Studies have shown that information processing and working memory have taken a hit. That means you just can’t keep up with the streams of information that you used to. (People with post-concussion syndrome and whiplash syndrome experience similar cognitive problems).
In my experience, these are amongst the most disturbing aspects of these diseases. A reduced inability to follow and to take part in conversations, to communicate effectively, to engage at the intellectual level one is used to, is disturbing, to say the least.
Recently, a couple of studies have highlighted the cognitive problems in fibromyalgia, and one of them did so in a way that demonstrated why FM is so different in some ways from other pain disorders.
FM is kind of a multidimensional illness, masquerading as a pain disorder. It’s different from other pain disorders in the sheer spread of symptoms it can produce. Problems with stimuli, cognition, sleep and exertion often exist right alongside the problems with pain in FM.
Even the pain in FM is different. While people with rheumatoid arthritis (RA) experience pain in the many places where their immune system has attacked their joints, skin, eyes, etc., the pain people with FM can experience doesn’t appear to result from localized spots of inflammation. The multidimensional pain experienced in FM appears to derive, at least in part, from their brains – and that may make all the difference regarding cognition…
The Fibromyalgia/ Rheumatoid Arthritis Study
The “Attentional function in fibromyalgia and rheumatoid arthritis” study focused on one aspect of cognition: attention. Researchers have identified three different kinds of attention – all of which were tested in something called “the Attentional Network Test (ANT-I)”:
-
-
- alerting – vigilance.
- orienting – determining which sensory information to pay attention to.
- executive control – top-down control of information processing; i.e. – the major regulator.
-
Pain, anxiety, depression, sleep and fatigue questionnaires were also given. Fifty-six women with FM, 41 with RA and 50 healthy women participated.
Results
The multidimensional nature of FM showed up in spades in the symptom questionnaire scores. People with FM had higher pain, anxiety, depression, sleep and fatigue scores than the RA patients and the healthy controls.
Cognitively speaking, the FM patients had slower reaction times (slower information processing times) and made more errors than either the RA patients or controls.
The reaction times of RA patients, on the other hand, did not differ from those of the healthy controls; e.g. people with rheumatoid arthritis do not have problems processing information. Each of the three attentional domains was affected to the same degree in FM.
Importantly, the inability to stay focused and respond quickly during the test was not a function of how much pain the FM patients were in, as some have thought. Instead, this study suggested that problems with attention and concentration come from somewhere else. A 2018 study came to the same conclusion. While the study showed that diverting one’s attention away from pain onto another task did reduce the pain FM patients were experiencing, it did not find that pain was actually interfering with attention.
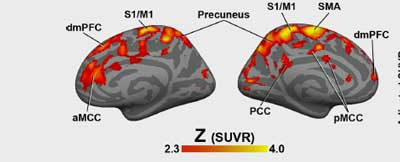
As did Younger’s chronic fatigue syndrome (ME/CFS) study, a recent study found extensive evidence of neuroinflammation in fibromyalgia but no evidence of neuroinflammation in RA.
Two diseases: two completely different ways to produce pain and fatigue
The question is why FM patients experience brain fog while people with RA – who also experience a lot of pain and fatigue – generally do not. This study suggests that the pain and fatigue in these two diseases are being produced in two fundamentally different ways.
The authors believe the core differences in the two diseases may account for the increased cognitive problems found in FM. One disease (RA) is an inflammatory one centered in the body, while the other (FM) is a central nervous system disease characterized by central sensitization.
The Gist
- Problems with fibro-fog, brain-fog, chemo-fog pervade fibromyalgia, chronic fatigue syndrome and environmental illness. Studies indicate that slowed information processing and problems with working memory are often present.
- Rheumatoid arthritis (RA) is a fatigue and pain disorder as well. The authors of this study wanted to see if RA patients experienced the same kind of attentional deficits that have been reported in FM.
- They did not. While the RA patients looked much like the healthy controls, the FM patients scored high on attention problems.
- The results also suggested that the problems FM patients have focusing are not directly due to the amount of pain they are in.
- They speculated that despite their symptom similarity, the two diseases were fundamentally different. RA is produced by an inflammatory reaction in the body while FM is a central nervous system disease which is characterized by “central sensitivity”.
- They proposed that overactive pain producing pathways in the brain were stealing resources from the attention regulating pathways found next to them.
- The differences between RA and FM (and other pain producing diseases) can help explain why so many rheumatologists simply refuse to see FM patients. Doctors report that FM is much more difficult to treat.
- Fatigue, difficulty paying attention, pain and dysautonomia may be core features of several diseases including FM, ME/CFS, Ehlers Danlos Syndrome and joint hypermobility syndrome.
- Stimulants, and mindfulness techniques have all been used successfully to ameliorate some of the effects of ADHD.
It turns out that the brain networks (anterior cingulate, prefrontal cortex) that process pain, and those involved in paying attention, partially overlap. The authors propose that heightened activity in the pain networks is stealing resources, so to speak, from the brain networks designed to help us concentrate and pay attention. They’ve been partially reconfigured, in other words, to focus on pain. That leaves FM patients with less brain bandwidth to focus on what’s going on around them.
This pattern appears to hold up within the FM community itself. An earlier study found that FM patients with allodynia (where touch elicits pain) – an extreme marker of central sensitization – had more cognitive issues than FM patients without allodynia.
Jarred Younger may have provided the most intriguing difference between RA and ME/CFS/FM. Despite the severe fatigue reported by some RA patients, Younger, to his surprise, was unable – using both thermal mapping and metabolite analysis – to find any evidence of significant brain inflammation in RA.
Compare that to the widespread pattern of neuroinflammation Younger and others have found found in ME/CFS, fibromyalgia and Gulf War Illness.
“We previously reported elevated CHO, LAC, MI, and temperature throughout the brain in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) [14]. Despite the fact that both the ME/CFS group in the previous study and RA group in the current study had significant self-reported fatigue (≥ 6 out of 10), only the ME/CFS group evidenced signs of brain inflammation.” Younger
The neuroinflammation findings lead Younger to suggest that RA is primarily a disease characterized by peripheral inflammation (i.e. inflammation in the body), while ME/CFS (and FM) are central nervous system diseases characterized by neuroinflammation.
“The difference in results could indicate ME/CFS is a CNS disease, while RA is a disease primarily of the peripheral joints. The MRSI scan may, therefore, be useful in identifying individuals with central inflammatory origins of fatigue.” Younger
Fibromyalgia, Chronic Fatigue Syndrome, Gulf War Illness – the Widespread Neuroinflammation Diseases
Younger recently published a small study that validated the thermal brain mapping technique he used to find neuroinflammation in ME/CFS, and I believe that he’s doing a similar study in FM. If Younger’s approach holds up, it presents an easier and possibly more direct method of measuring neuroinflammation.
Younger has also finished his study of botanicals with neuroinflammation-fighting potential. Hopefully that study will be published soon.
Fibromyalgia’s Bad Luck
The disjunction between an inflammatory disease and a neuroinflammatory may explain why rheumatologists – who have been trained to treat inflammatory disorders – are so poor at treating FM.

Rheumatology and fibromyalgia have turned out to be a bad fit.
A small, recent study found that 47% of rheumatologists refused to treat FM patients at all. The survey suggested FM was not only considered more difficult to treat but was also more apt to be characterized by problematic doctor-patient relationships – which the doctors, of course, decided was the fault of the patients.
Another, larger survey found that only 44% of physicians were willing to accept further FM patients, largely because of the doctors’ inability to control their patients’ symptoms. Patients’ emotional responses were considered another factor.
Of course, it’s not just rheumatologists. Neurologists display the same pattern (but perhaps worse). No one right now is particularly good at treating neuroinflammation. The good news is that neuroinflammation is a growth field with lots of funding going to find better treatments.
That’s good news as for RA as well, as somewhere around 25% of people with RA develop FM during the course of their illness. Acquiring FM has, not surprisingly, been associated with increased symptoms and worsened disease outcomes in RA patients.
It turns out that if you stress the pain processing systems long enough, some will go haywire; fibromyalgia actually shows up in a subset of patients in many chronic pain illnesses.
ADHD in Fibromyalgia and Chronic Fatigue Syndrome
In its more severe form, difficulty paying attention shows up as attention deficit hyperactivity disorder (ADHD). Several studies suggest that ADHD may be quite common in fibromyalgia and ME/CFS, and attention problems seem (to me anyway) to be a core feature in these diseases. It’s no accident that the “wired and tired” symptom popped up so prominently in ME/CFS/FM.
ADHD also, interestingly enough, appears to be common in Ehlers Danlos Syndrome (EDS) and joint hypermobility (JH). One group suggested that conditions common to ME/CFS, FM, POTS, EDS and JH such as fatigue (which is more common in ADHD), chronic pain, dysautonomia, impaired coordination provide a kind of “bridge” to ADHD.
Whatever explains ME/CFS and FM is going to also have to be able to explain the strange ADHD-like nature of these diseases.
- Do you meet the criteria for ADHD? Check out a self-test here.
Focusing Better
Stimulants can help some people with ADHD focus better. Given the hypothesis that activated pain circuits are draining resources from the nervous system pathways that help us focus, it’s not surprising to see that studies have shown that neuroplastic/brain training approaches such as mindfulness techniques can be helpful in ADHD. A cognitive training technique was still effective three years later, and mindfulness-oriented meditation, hatha yoga, etc. studies have produced positive results. While descrying the quality of some of the studies (nothing new there), a review found that all studies showed positive results.
Conclusion
Both people with fibromyalgia (FM) and rheumatoid arthritis (RA) experience severe fatigue and pain but only people with FM demonstrated problems with attention and focus on a cognitive test. That’s because, the authors believe, that the fatigue, pain and cognitive problems in FM derive from a central nervous system condition called central sensitization while the fatigue and pain in RA come from an inflammatory condition in the body.
Neuroinflammation studies back this up. Widespread neuroinflammation has been found in FM and ME/CFS but not in RA. Despite the fact that people with RA and FM have some similar symptoms and see the same specialists they are very different diseases.
This study did not find that the amount of pain the FM patients were in affected their ability to pay attention. Instead they proposed that the pain producing pathways in the brain were stealing resources from the pathways in the brain devoted to focus and attention.
The attention problems found in this study were not surprising. Several studies suggest that attention deficit hyperactivity disorder (ADHD) is common in FM, ME/CFS and allied diseases. Stimulants and mindfulness techniques techniques can be helpful with ADHD.
See the next cognition blog in this series:






I wonder what Naviaux would find if he did metabolomics studies to look for differences – such as whether he’d find the FMS group to be caught more in states of relative freeze/hibernation (more shut down, more immobilized, more brain fuzz) and RA more in predominant fight/flight
Love to see metabolomic comparisons….
So could childhood ADD or ADHD be indicative of increased chance of developing FM MECFS later in life.
ADD AND ADHD IS FROM BRAIN INFLAMMATIONS–NEUROINFLAMMATION IT IS NOT DIFFERENT FROM ME/CFS.—IN FACT ME/CFS IS NEUROINFLAMMATIONS.
WHICH IS NOW SHOWN ON THE CORONA PATIENTS
I think that’s what a lot of people are thinking. We just need more studies. The big Japanese followup to the ME/CFS study has been rumored to be published any time now. It was great to see the Younger method get some validation as well plus we recently had an FM neuroinflammation study published with the same widespread inflammation.
Plus many efforts to combat neuroinflammation are underway.
Darn this is exciting!
Crt I hope this is not too controversial but there is very good evidence now to attribute the bulk of cases of autism to neuroinflammation- especially related to the aluminium adjuvants in vaccines. One could get bogged down into an endless argument about this so I will just drop this paper and let your readers explore the site well:
https://vaccinepapers.org/aluminum-inflammation-interleukin-6/
It is kind of a heavy paper and took me weeks to process it, but it stacks up.
The aluminium is taken up through macrophages, then ends up in the microglia, resulting in a neuroinflammation of a Th2/ interleukin 6 type.
Anyhow that is one element of concern.
Neuroinflammation is a problem in some covid patients but we do not yet know the extent of it. We do know that there is reason to believe that COVID immunisation may prime the immune system for cytokine storms if there is a subsequent coronavirus infection- and most Upper Respiratory Infections are coronavirus.
Again- much too soon to know what to make of all this- but watch this space I guess.
wrong website
atlassubluxation.wordpress.com
I joined in on the clinical trial from EpicGenetis and was given a score of 92 which is an extreme positive at least for them. Next up is a TB vaccine to hopefully reset my immune system. They are telling me my white blood cells do not produce the correct cytokines and such.
We just need them to start their trial already. I recognize that the pandemic has thrown a big monkey wrench into a lot of plans and EpicGenetics was behind before then. Let’s hope they get that thing started.
Interesting hypothesis Cort. As you know I’m in the EDS, ME/CFS category and now I’m experiencing new symptoms which may be RA or osteoarthritis. I need to get some testing done.
EDS is associated (as Issie often points out) with MCAS which can definitely impact brain functioning and EDS has a very high association with fatigue–and pain–and some studies have shown some correlation with autistic tendencies. EDS, to a lesser degree, is also correlated with other mental conditions like anxiety, obsessive compulsive disorder and ADHD. (Those pesky psychologists always want a piece of the diagnostic pie!)
Mental issues often make it harder to focus. Pain makes it harder to focus. Menopause too. None of these need be connected to ME/CFS or FM. IMO, the most prevalent characteristic of ADHD is distractibility–almost an over active brain which cannot hold steady on thoughts or observations. Perhaps it is in an entirely different category than brain fog or even pain or fatigue.
So I took the ADHD test and I am definitely not that. However, I had an epiphany when I mentally took it for my housemate. I now believe that he does have ADHD and that it accounts for many troubles in this household. So thank you Cort, for that link!! It unexpectedly gave me illumination! Whether or not it will result in getting help, I do not know.
Sorry my comments sound kind of jumbled, but hope you can follow a bit…
🙂
almost an over active brain which cannot hold steady on thoughts or observations
You know what it seems to me like – a brain that’s low on fuel that’s getting continually pushed or a brain which can’t regulate itself properly – it’s spending resources everywhere where it should be spending resources on one thing at a time.
It’s fascinating that stimulants actually can help in this hyperactive type disorder.
@Cort: From the RA paper of younger I read “We hypothesized that RA patients would show higher brain choline (CHO), myo-inositol (MI), and lactate (LAC), and higher brain temperature than healthy controls.”
=> Does that mean Younger has a paper that shows increased *average* brain temperature in ME and FM patients??? If so, could you give me a link to one of those? I thought he only found increased temperature hotspots in certain regions of the brain, not increased average temperature.
If so, that is in line with the idea I have been writting about for quite some time:
Our poor brain blood flow should result in increased brain temperature. Or, if you like to see it otherwise, our increased brain temperature paired with poor brain blood flow should result in a drop in body (all minus brain) temperature. And that drop in body temperature makes many parts of our body function suboptimal as many biochemical processes require that 36 to 37 degree Centigrade (normal body temperature) to operate optimal. Below that, energy production gets more difficult and produces more waste products.
The idea behind it is simple: the brain consumes far more energy for its size compared to the rest of the body. Consumed energy turns finally into heat. That creates some serious buildup of heat in the brain (think of an incandescent lightbulb in a bowl the size of our head). The blood flowing through the brain can take some of that excess heat away. That needs to happen in both healthy and ME/FM patients.
Taking away heat by letting a liquid flowing through it can only work if the liquid that flows into the brain is colder then the brain itself. The cooler the liquid is and the higher the amount of blood flow per second is, the more (excess) heat the blood can take away.
If increased heat is produced, more blood has to flow to the brain to take the extra heat away. That OR the temperature of the blood flowing from the body to the brain needs to be lower.
ME/FM/… patients have *reduced* blood flow to the brain and even less after exertion. So even without extra energy consumption in the brain, this should give rise to increasing brain temperature. That would be probably inflammatory, as increased temperature often is pro-inflammatory.
There is a way out of this with reduced blood flow: drop metabolic rate (energy consumption and heat production) in much of the rest of the body. Then the blood flowing through the body will cool down more. That in turn takes more heat away from the brain for the same amount of blood flow.
(Note: hyperventilating can assist in cooling the body down too; dogs rely heavily on this technique.)
This holds a partial unification of ME/FM too:
In order to try and cope with problems of either poor blood flow or increased brain energy consumption, the brain can try and save the body and keep temperature of the body normal-ish. Then the brain risks some serious overheating and with it chronic inflammation. That would be a more ME type of disease.
If the brain tries to safe itself more, then it has to lower the temperature of the body to (near or even sub) hypoxia threshold. Then energy metabolism of the muscles is very bad and you have cold muscles very prone to damage, just like going to run with very cold muscles is a bad idea. That puts plenty of damage and later inflammation (as that damage needs to be repaired and that requires inflammation) on the muscles. That would be more a FM type of disease.
If the brain decides to go with something in between, then you end up with both ME and FM in this idea. Many do…
Wow, your explanation has been illuminating! Thank you!
As many say, anything trying to explain ME must take into account PEM. This fits in the idea of reduced blood flow to the brain and increased brain temperature too.
When exerting the brain, more energy will be consumed by the brain. That eventually turns to heat and will increase the brain temperature. That has a good chance to cause increased brain inflammation and that will take time to resolve. It also creates a need to remove part of the excess heat from the brain by cooler blood from the body. That cooler blood from the body can be obtained by reducing the metabolic rate of the body. Cooling the body down by producing less energy will take some time to yield a lower temperature, so the cooler body temperature will be delayed.
Cold muscles and other tissues will create their own set of problems once their temperature has dropped enough. Many ME/FM patients have cold body temperature, especially the morning after exertion including exertion of the brain.
When overexerting the muscles on the other hand, they will require a larger part of the already limited blood supply of the body. That will reduce blood flow to the brain. At the same time, the temperature of the muscles will increase due to the exercising and likely later on once more due to the inflammation that is needed to help repair the damaged muscles. Muscle inflammation after exercise is a very natural thing including in healthy people.
The combo of decreased brain blood flow and increased core body temperature will make keeping the brain cool challenging. Increased brain temperature has high chances to increase brain inflammation and that will take some time to resolve. That can paradox in a delayed manner by needing to keep the body very cool the day or so after exercising, conflicting with the need to increase body temperature for repairing the muscles by inflammation.
Note: both Issie and I have good reason to believe that that is but part of a quite bigger set of problems we experience.
Note: just trying to increase blood flow to the brain can easily fire back, for example by reperfusion issues due to too quickly increasing blood flow after it has been too much reduced.
My understanding is that Younger found increased temps in certain parts of the brain but across a fairly wide swath of it.
What an interesting possible explanation for the low body temps often found. That is fascinating! Of course one would need to try save the brain first while trying to keep the body going.
Nice! 🙂
There are so many plausible reasons for the diseases. This one seems brilliant to me. Thank you.
“It turns out that the brain networks (anterior cingulate, prefrontal cortex) that process pain, and those involved in paying attention, partially overlap.”
Together with a study that glutamate injected in the brain of rats can “burn” away pheriphery nerves (Cort had a blog on that one) and widely accepted knowledge that excess glutamate can make neurons “trigger happy” or work very hard and fast (but often yield poor results by hasting too much), producing plenty of heat we come to the spinal cord escalator idea that Issie and I worked on https://www.healthrising.org/blog/2020/12/11/nucynta-opioid-small-fiber-neuropathy-fibromyalgia/.
The idea here is: excessive glutamate and ROS in the brain (possibly produced by inflammation) can travel down the spinal cord and create (or “copy”) the same inflammatory situation that is on the nerve end at the brain side towards the nerve end on the body side.
So, a state of excessive glutamate and ROS on the tip of the spinal cord nerve in the brain can under cicumstances “travel down and leak” towards the tip of the pheriphal nerve (into the body tissues).
But, excessive glutamate and ROS on the tip of the “body part of the nerve” can copy and travel upwards and create the same state on the tip of the spinal nerve that enters the brain.
As such, an inflamed part of the brain can create and inflamed muscle or gut. And that inflamed muscle or gut can once again create or reinforce an inflamed brain. So, we have potential for a vicious circle here.
This “It turns out that the brain networks (anterior cingulate, prefrontal cortex) that process pain, and those involved in paying attention, partially overlap.” adds a new part to the idea: excess (chronic) pain would in this idea *also* be able to trigger a state of increased glutamate / ROS / inflammation at the brain (stem) part where that nerve ends up to.
That glutamate wouldn’t stay exactly there at that position. It is “interstitual” glutamate to start with, meaning it is found outside (in between) the cells. So it can leak and spread from cell to cell. It that happens long enough, glutamate would leak to nearby areas and create a combo of trigger happy neurons consuming plenty of energy, unprecise information processing and increased inflammation, temperature and ROS in that area. And the quoted info from Corts blog says those nearby (or overlapping) areas are key in paying attention…
We should get this in a blog 🙂
Issie and I are working towards putting the core of our ideas in a clear, coherent yet concise series of blogs. To be featured on HR ofcourse.
We seek to make our ideas a lot more accesible and making the links between distinct topics more clear. We see that there is quite a need for that with patients and HR readers. Unfortunately it’s also a monumental task.
The goal is to design this framework of core ideas so that ideas like the one above later can hook fairly well into it, making both our core ideas more clear and the new ideas easier to understand then when they would be written completely separated.
Great idea and very generous of you but a monumental task, I imagine!
dejurgen, would cool packs on the head help take heat away,
or decrease (worsen)blood flow more?
or decrease brain activity (worsen) because of less than optimum temp?
Hi sunie,
I personally find cool packs on the brain a bit too “aggressive” for me. There is a simpler (small) substitue for it:
A Chinese proverb says to chew on food till it’s liquid, and chew on drink till it’s solid.
Rather then drinking warm or even hot drinks in a single go, sipping a bit of room temperature water from time to time and chew it plenty takes away some small amount of (brain) heat through the palate. It is also claimed that saliva helps restore gut lining. Small changes, but easy and cheap ones. Just don’t overexert your jaw muscles.
There is also one thing I like better: to simply not take warm or worse hot baths or showers. No need to have them cold, just a bit less warm so that you can easily tolerate them is already a good start. That works for both me and Issie. Having short cold (or tepid) showers along the spine helps me too, but is bad for Issie. But not having hot baths and showers is doing already half of the job in preventing additional inflammation.
@sunie, timing is everything and knowing what to do and when.
I used to take way to hot showers. Dejurgen asked me to try lowering the temperature and see if I didn’t do better. Before, with the heat being too hot, I would get drained of energy. The shower would wipe me out. I got dizzy and POTSie. With it cooled down now, (not cold, but not steaming hot) I’m not noticing that. I feel better and don’t have those symptoms.
When I’m in pain, which is what Dejurgen is talking about that is different for him and I…..he wants an ice pack and I want a heating pad. We both have back and spine issues and pain.
I find heat helps to vasodilate veins and I seem to need that in my neck. But when this is happening, I have extremely low body temperatures. My normal is about 2 degrees below what is considered normal. (My doctor even wrote that in my medical records. She was afraid a fever would be missed with my normal core being so cold.) So heating me up is good when that happens. I feel better with heat, when my body core is so cold.
Dejurgen doesn’t have low body temperature, but he used to. And now he finds cold to be more preferable.
I also found a study done on differences between men and women. It seems more women preferred heat and more men cold.
So it depends on what is going on as to whether you use hot or cold. And it depends on where you apply it and what is going on at that moment. Our body could be cold and our brains over heated, as Dejurgen talked about.
When I feel faint or nausea, a cool rag on the throat and forehead really helps.
I call myself a fair weather girl. I can’t take extremes in either direction. My body doesn’t regulate temperature correctly. (And it doesn’t appear to be thyroid related.)
One thing to keep in mind with body temperature……pathogens, virus and bacteria appear to lay more dormant in cold. (Could our low body temperature be another compensation? Trying to keep these critters within from being as active? Lyme people use saunas to try to detox from Lyme. It can kill them. But, cold can keep them more dormant. Scientists refrigerate bacteria to keep it alive to be studied later. It doesn’t kill it. But heating it up makes it more alive. Overheating, may kill it. And in Lyme, saunas can cause a nasty herx, with die off.)
We have to know our WHYs and take into consideration whether or not what seems to be a symptom, may in fact, be a compensation.
Hi Dejurgen, I’ve spent time with people with motor neurone disease (research funding is pitiful…) and glutamate is thought to be a factor in over exciting the motor neurones.
@Tracey Anne, we just had a question on the forum about our hypothesis of glutamate being a big part of the picture in all these multi complex illnesses. Here is the link:
https://www.healthrising.org/forums/threads/potential-linking-fm-mast-cells-sleep-deprivation-food-intolerance-exercise-intolerance-and-me.6217/page-3
Also, a reply I made in regard to antibodies to GAD. There can be an autoimmune issue with it. And is highly inflammatory. But there can also be too much norepinephrine released in POTS people. (Its a compensation to help blood flow to the heaet and head.) Both can cause a highly hyped feeling and very intense feelings of anxiety as they both mess with the brain.
MY Reply;
I had my GAD antibodies checked. (I was okay.) It is part of a good workup for POTS that is done. Some people are found with issues here. But not all POTS people have this autoimmune response with it. But as Dejurgen mentioned, it does appear that some of us do have issues with balance of glutamate. It is an excitatory thing and can trigger sympathetic nervous system response, along with other not so good or desired things. Sort of a hyper feel. (But, to note **** HyperPOTS people seem to have way too much norepinephrine when we stand. And that too gives that feeling of being hyped. And also increases heart rate and contributes to the “tachycardia ” part of this syndrome.)
But we do need glutamate. It helps with our brain function and other things necessary for our bodies to function. The key is balance or homeostasis. Some have too much and the balance between glutamate and GABA is thrown off. But GABA is an inhibitory response and too much of it could make one more tired.
Thanks Issie, yes the balance is so important between the glutamate, which excites and the gaba, that calms – as with histamine – we need it but in appropriate amounts. Goldilocks was on to something!
Hi Cort
Having read thru all, considering my metabolic at rest is 19, constant battles of cold and or fever but low grad 36>. I was deemed a hyper kinetic child at 7, brain waves tested….explains much …the exacting toll it takes rounding up help from the gate keepers per se DRS from the survey, tru.
Thank you for being you and sharing
Omg, even typing this is exhausting. ? But trying to comprehend this artical, with my severe brain fog today. Is pointless. ? I wish someone would put the artical in layman.or just summarise it for us PLEASE!!!! ?
Sorry about that! I just added a conclusion and check out The Gist on the side bar – it has a short summary of the key points is there. This stuff is complex but I hope that helps!
With all due respect, I don’t buy it. I just wrote a long, detailed explanation as to why, and then made a typo in my email address and my comment was erased. I don’t think that’s ADHD. I’ve used up my energy for this now, and need to move to the next need (fixing dinner).
I think it’s alluring to think that something that has a therapy in the form of a pill is involved in our cognitive issues, but I don’t buy it. I think it has to do with the amount of energy we have, and how much just standing up demands of that energy. It is for that reason that I walk with a cane: it extends my energy, both physical and cognitive, by (I learned from a balance specialist) providing an additional point of reference to the brain so that the body and brain are not so dependent on using the eyes (which use up a tremendous amount of brain energy) to maintain balance. I said that more articulately in the comment that was erased, but this is what I can do now.
Thanks.
Cameron, ADHD is a syndrome description. It does not imply need for medication nor that medication is the only treatment.
What it does imply is that the attention problem does not occur solely during the course of another DSM syndrome.
So the ideaa of AADHD symptoms being part of fibromyalgia, or of Ehler’s Danlos Syndrome is legitimate and does not undermine the idea that the symptoms may be described as ADHD.
Having made that association one may use stimulants to see if they help- and for about 70% of people with that syndrome they are judged to be helpful.My partner has ADHD and fibromyalgia and ADHD, but she finds the stimulants over activating and will only use a tiny dose,
Your comment about eyes is interesting. When i was working I used to specialise in ADHD and I came to the conclusion that what we doctors call ADHD is identical to the problems called convergence insufficiency by ophthalmologists. Both are improved with stimulants.
Balance and proprioception are also involved and in many cases these are associated with neck injuries- often acquired at birth.
Balance, proprioception and vision work together. The act of reading involves knowing current eye position, estimating the movement needed to read the next phrase, and calculating the vector required to move the eyes- all with regard to the position of the head and neck. This uses enormous amounts of working memory- and that is the result of the behavioural deficiencies in ADHD.
ie- if you have to read something complex- like what i am writing now- so much of your working memory is chewed up by the eye movement task that you cannot process what you are reading.
Calling ADHD a “cognitive” issue illustrates serious deficiencies in the current conceptions of cognition, and a clinging to the neuropsychology of the 50’s or 60’s.
Current conceptions now rate ADHD as a subcortical issue. Its not easy finding doctors who understand this.
Note that my blog listed below discusses some of the issues related to neck injuries that are relevant here- but it is far from complete. Note that the rate of neck injuries is 13 times higher in the FM population than the general population.
My energy is especially minimal today so all i will say is my brain inflammation is so bad that my head gets hot and my face turns red when i try to think too much ie writing email is too much. My head cools down after i quit thinking so hard
@Jb atl, as Nancy mentioned above about MCAS….the first thing I thought when you said that when you think too much your face turns red and your head gets hot. Emotion and energy can trigger mast cell response. Have you looked into this? There is quite a bit we have written on both these blogs and the forum on it. One of my signs is a red face to start with and a hot flash all over my body and then I lose my color, a flush. One side of my face goes numb too. That is MCAS. You can feel the heat coming from me. And its not hot flashes from lack of hormones of menopause. Its from mast cell over response and my body not turning it down.
A couple things that have really helped is Nettle tea before having this response, not during. And taking a bee product with Propolis, pollen and royal jelly in it. I space it out. One when I get up and one after lunch. Keeps me pretty steady. Few more tricks, but these are the main ones.
Thank you all, especially to both Issie and dejurgen.
also, did not know the flushing connection with mcas, tks again.
An aside—Bhupesh Prusty (cfs/me/hhv6/mitochondrial interests) is soon advertising for talented exceptional PHD student…..hope someone here knows right person to tell about contacting Bhupesh…..
https://mobile.twitter.com/BhupeshPrusty/status/1356617258907410432
My deceased psychiatrist was a dear and highly intelligent guy who studied constantly about all of medicine, not just mental illness. He was convinced that ME/CFS resulted from inflammation in the brain, which amplified pain signals.
He diagnosed me , at age 62 with bipolar disorder. I was diagnosed with ME/CFS at age 65, five years ago. I had been treated for depression for years. Doctors would always ask me if I had any signs of mania and I always said, “no”. My psychiatrist said that my mania exhibited as anxiety, which was acute most of my life.
He believed that bipolar disorder was at least in part, the result of inflammation in the brain. He told me that many ME/CFS patients are bipolar, which would make sense. I told him that I had found that, when I was having a flare, if I took two Benedryl, the extreme flu-like symptoms would improve significantly. He pointed out that allergies also cause inflammation. When I told my rheumatologist about my improvement with taking Benedryl, he said that I probably felt better because of the soporific effects of Benedryl and that I had slept better. I pointed out that it helped me during the day. If I was feeling very ill, the dose of Benedryl would make me feel better within 30 minutes. Of course, Benedryl makes most people very sleepy, but it doesn’t affect me that way much anymore.
In the same vein, if I am feeling very sick, if I take NyQuil before bed, most times I will feel much better in the morning. Of course NyQuil also contains an antihistamine. Neither of the two medications do anything for the pain.
On another topic, I went on a pretty strict KETO diet for a year, not only did I lose 20 pounds more easily than I had on any other diet in my life, my IBS and interstitial cystitis went completely away and they had been constantly troubling for the entire time I had had ME/CFS. Sugar, definitely makes me feel bad, both for pain and flu-like symptoms and it makes sense that if I am not ingesting carbs, which turn into sugar, I would feel better. The KETO diet is also being shown to help autism and purported to almost reverse bipolar disorder.
I would be interested in knowing if others have had similar experiences.
Hi Kat, yes I would have found antihistamines helpful in reducing symptoms but I’m trying to do without them. I also found ibubrofen helped with what I think is brain inflammation but it upsets the rhythm of my heart and not a great medication to be taking long term.
I have extensive food intolerances but have found certain foods that I can eat – and on the whole – yes, it would be a low carb diet. However I find I have great difficulty in getting energy to my brain. Now if I’ve over done things and have depleted my energy stores, then nothing I eat will help much – I just have to sit it out and rest, until I pick up again…
However, now that I have more time feeling fairly normal, I have found chocolate great for boosting my brain energy but that raises histamine too much, I think. So, currently I’m finding ginger biscuits/cookies (no dairy) are working great but I have to limit them!
Your former psychiatrist sounds like he was someone who was open to different ideas. I can get depressed and anxious (unsurprisingly!) but I don’t believe these are the root of my issues. I also feel increasingly uncomfortable trying to distance myself from mental health issues because many people have them and stigmatising people for encountering difficulties with their mental health is unhelpful.
However, I find myself becoming defensive because others restrict my health problems to my mental health and then they don’t/won’t look deeper, to where the irregularities, I believe, really exist. I believe the incorrect focus on the psychological cause of ME/CFS, has lead to people not having access to the genuine support of decent, professional, compassionate, mental health workers, which I think is is shame.
Recently I’ve been trying to work out which bit of my symptoms relate to ME/CFS – do I have it at all? I definitely have widespread food intolerances and IBS. I now also have asthma. I can have interstitial cystitis. My hips can hurt and the bones in my feet were painful a few weeks ago. My eyes can be affected – at one point I had difficulty changing focus and I can often have puffiness around my eyes. I believe I have varying levels of inflammation in my brain and I can have ‘information processing and working memory’ issues (the more my brain seems to be inflamed the worse it functions). I can also have symptoms related to my food intolerances in which I feel as though I’m sedated – especially fructose. And there will be other things I’ve forgotten – there always are! (Oh yes, the emotional ups and downs and at times feeling all over the place…) Thankfully I don’t have FM.
So, currently I’m functioning better I can actually think and remember things well enough to be able to evaluate some issues. However, there is still a limit to my available energy. I am wondering – do I actually have more energy, or am I (my mind/body/brain) using less because I’ve calmed down my sympathetic nervous system and inflammatory issues? Being wired 24/7 is very energy intensive and I believe the immune system also uses immense amount of energy. Creating inflammation, in the brain or elsewhere, must (I think) use lots of energy and if that’s limited, reserves will, I would have thought, be used very quickly.
Also if the brain is using parts of itself for jobs, that part is not designed for, I would think that may be cumbersome, take longer and may be less energy efficient. And to be honest, I have also found that life is so much more difficult, and extremely stressful, to be so misunderstood, unsupported, disbelieved etc,. and I having to try and deal with everything (on so many levels) with a brain and memory that isn’t working well (!) and limited energy (absolutely infuriating – I could explode with anger sometimes but that would use a lot of energy – this is a very tricky issue for me). So moving swiftly on, as Cameron points out, if ME/CFS is an illness revolving around available energy, anything happening in the body that uses energy, will be a potential drain on that precious resource.
I was thinking about the Angus Mackay and Warren Tate blog:
‘A Novel Neuroinflammatory Paradigm for Chronic Fatigue Syndrome (ME/CFS)
Neuroinflammation, the hypothalamus and a unifying hypothesis.’
https://www.healthrising.org/blog/2020/05/27/neuroinflammatory-paradigm-chronic-fatigue-me-cfs/
I copied 🙂 this from the gist:
‘Mackay and Tate believe that neuroinflammation is making the PVN twitchy, causing it to over-react to all sorts of stressors. Once the PVN reaches a “stress tolerance level”, it returns the favor, telling the glial cells in the brain to go on the attack – resulting in more neuroinflammation, fatigue, pain, problems with temperature regulation, sleep, cognition, mood swings, etc.
As the stressor abates, the neuroinflammation calms down, the PVN takes its foot off the stress pedal, and the “crash” or “flare” abates. The more inflammation, though, the longer the PVN takes to settle down and the longer it takes to reach “baseline”.’
This makes sense to me and my brain 🙂 It’ll be so interesting to see what future studies reveal.
I know I’m late to the party but I just want to thank you, Cort, for this post. I’ve been telling my wife for years that during my “wired and tired” cycles (which can only be stopped with a doxepin + clonzepam-induced quality sleep), I feel myself slipping into an ADHD-like state. It sometimes even transitions into a quasi-hypomanic stage, where I feel like I’m high on speed and my personality changes (e.g. I go from a fatigued introvert to a stream-of-consciousness extrovert). At that point mindfulness becomes impossible and stimulants just make it worse.
Anyhow, good to know I’m not alone.
Thanks Cort.
I think that this blog is an excellent review of much of the current research in the field. I’m going to see if I can get the printer to work so I can get a copy to my psychiatrist. It provides a neuro-chemical explanation of many of the symptoms about which I have been complaining.
I was an early and frequent subject of the FM/CFS (CFIDS back then)/Gulf War Syndrome/Control studies 25ish years ago. What I learned from the researchers and studies has greatly helped me to manage my symptoms over the last 25 years. I’ve been saying that I control the pain most of the time because I have a tape loop playing in my brain saying “I’m not in pain, I’m not in pain, …”. I originally did this consciously, but it appears to be automatic now. Your discussion of neuroplasticity and the energy requirements of the relocated brain functions seems to provide confirmation of the efficacy of this form of meditation/”diverting attention away from pain. I had not considered the effects of this brain labiality on fatigue and brain-fog though.
A few observations based on my personal history and experience:
In my late 20s I developed a SEVERE episode of fatigue, short-term memory formation issues, and concentration problems. 6 different doctors/specialists later, nothing cured it, but acupuncture & Chinese herbal therapy helped. Shortly thereafter I talked to a friend who had experienced the same symptoms, and isolated the cause to a soy protein allergy. I did the same type of dietary limited-ingredient-testing that had worked for him and discovered that I had developed a severe allergy (or intolerance) to MSG. (I had been eating Chinese food for lunch every day). Once I eliminated the MSG and several analogs from my diet I was back to normal within a few weeks. I am convinced that the MSG severely affected the glutamate metabolism in my brain. A less likely explanation is the mast cell over-activation caused by the allergy, or possibly a combination of both.
Skipping 10 years ahead, I worked as an operations planning systems analyst for Bell Labs/Lucent Technologies – basically writing requirements for multiple computer systems, call center procedures, testing requirements, management reports, billing, etc. for features in development. Obviously this was a highly technical and detail orientation requiring job. I developed sudden flu-like symptoms, and the company doctor prescribed an anti-viral, and said I’d feel better in a few days. That became a week, 2-3 weeks, 6-8 weeks, … we’d better run some tests. I was flat on my back and sleeping 16 hours a day for 6 months. Luckily an excellent infectious disease specialist referred me to the ongoing CFS/FM/GWS studies.
During the studies I was amazed to observe how quickly I became severely fatigued just from doing a series of memory-requiring simple math addition problems. Basically add two 2-digit numbers, forget the first, add the second and third, forget the second, add the third and fourth, etc. I was yawning and losing the ability to consistently do the additions within 10-15 minutes, and was severely fatigued for the rest of the day. This study measured blood oxygen levels during this exercise, and the researchers were quite excited to see that the oxygen levels plummeted much more quickly than in the control group, without my and other CFS patients hyperventilating (which was the current hypothesis regarding the cause of the fatigue).
At that time I could easily multiply two 3-digit numbers in my head unless I was severely fatigued. Within the next 6 months to a year I could actually observe the loss of intermediate memory registers to store the multiplication products in order to calculate and add the digits from 5 to 4 to 3 to consistently 2. Basically I was too mentally fatigued and had lost the concentration required to remember each step from 3×3 to 3×2 to 2×2 digit mental multiplication. The researchers loved that I could actually explain this in computer analogous terms. In short, I could track the deterioration of working memory and the ability to process complex multi-stage problems over a relatively short period of time.
Another study was the first to quantify exercise tolerance in these 4 groups. The conclusion was exactly what we now know: That CFS/FM/GWS patients did best with regular exercise up to an individual’s tolerance level (which varied greatly from day to day) at least 3 times a week, as measured by an increase in heart-rate over the subjects’ resting rate. For a physically fit patient this was a 60% increase for 20 minutes 3x/week. On a good day I (and other patients in my category) could easily tolerate that level. On a bad day it might only be 2-3 minutes for some of the same patients. This was done on a treadmill, so the resistance could be lowered so as not to exceed the heart rate limit for each patient. Patients exercising at this level did much better both in terms of pain and fatigue than either patients not getting regular exercise and those who exceeded that limit (i.e. walked at the same pace/resistance regardless of heart rate as long as they could.)
Finally, the only medication tested in controlled studies that really provided symptom relief for a large number of non-control subjects was a Parkinson’s medication, which worked for me for a number of years. This leads me to believe that neurological inflammation (without the permanent damage caused by myelitis which leads to Parkinson’s symptoms) is one of the major causes of flare-ups. Once again this is consistent with current research. BTW, I no longer take that medication not because it has lost effectiveness, but because insurance refuses to cover it since it is off schedule for CFS/FM and it costs more than half of my monthly income. It did allow me to return to work for several years after I began taking it.
I hope that my experience provides some additional insight to this group of illnesses to you or some of your readers. I am also hopeful that the surge of new patients with the same or overlapping symptoms due to Covid-19 will lead to increased research funding.