


Systrom has dramatically deepened our understanding of what’s occurring during exercise in ME/CFS.
David Systrom, the Harvard pulmonologist, is digging ever deeper into his ME/CFS patients. In “Insights From Invasive Cardiopulmonary Exercise Testing of Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome” Systrom and company assessed the records of 160 people retrospectively diagnosed with ME/CFS. – and in doing so became the first group to assess small fiber neuropathy (SFN) in this disease.
The first major finding was that mean peak V02 – the highest level of oxygen extraction that occurred during the exercise – was significantly lower in ME/CFS. Since energy is mostly a function of oxygen extraction, this indicated the ME/CFS patients were unable to produce as much energy as the healthy controls. Under that broad brush, though, several subsets were about to pop out.
The Gist
- David Systrom and his invasive cardiopulmonary exercise testing are testing the blood before it gets to the muscles and after it leaves the muscles during exercise.
- The ME/CFS group as a whole had reduced peak oxygen uptake; i.e. they were unable to produce as much energy as expected.
- Approximately 30% of ME/CFS patients had small fiber neuropathy.
- Systrom identified low-flow and a hi-flow groups. The low flow group had low cardiac output, high levels of venous oxygen and reduced preload. This group likely appears to exhibit “venous pooling”; i.e. blood is pooling in the veins – possibly, in some cases, due to a small fiber neuropathy – and then getting lost into the body before it reaches the heart. That reduces blood flows to the heart and the muscles.
- The high flow group has plentiful blood flows but the blood is either not getting to the muscles (possibly because of a small nerve fiber problem), or damaged mitochondria are not taking it up. This group has reduced oxygen extraction.
- The authors declared that deconditioning is “definitively” not causing the problems they’re seeing.
- Ron Tompkins of the OMF funded Harvard ME/CFS Collaborative Center is doing cytokine, metabolomics and proteomics analyses of the blood Systrom is collecting. He reported the cytokine analyses are finding high cytokine levels in the ME/CFS patients.
- The fact that similar low-flow and high-flow findings occur in POTS suggests that POTS and ME/CFS share a similar pathophysiology.
- Low-Flow -Reduced cardiac output is usually caused by problems in the heart (heart failure) or the lungs (pulmonary hypertension), but neither of these were present. Instead, their heart output was reduced because their hearts weren’t getting enough blood in the first place. Studies of this group in POTS indicate they have high vascular resistance; i.e. narrowed down blood vessels that are impeding blood flows.
- High-Flow – Despite their plentiful blood flows, the high-flow group had the lowest oxygen extraction of the group; i.e. less oxygen was being extracted from their blood than the other group. They also had the highest venous oxygen tension (vPO2); i.e. they had higher levels of oxygen in their venous blood. (Oxygenated blood flows from the hearts to the arteries, into the muscles, then out of the muscles into the veins, where it returns to the heart.) In short, this was the impaired oxygen extraction group. The authors proposed that either blood is being shunted away from their muscles and/or a mitochondrial problem is preventing them from taking up the oxygen in their blood. Systrom noted that this kind of shunting has been associated with small fiber neuropathy before.
Small Fiber Neuropathy (SFN) (Finally) Found in Chronic Fatigue Syndrome (ME/CFS)
It was good to see, 8 years after the first fibromyalgia (FM) small fiber neuropathy (SFN) study and dozens of FM SFN studies later, SFN FINALLY getting assessed in ME/CFS. For one thing, it will help people with ME/CFS get their doctors to assess them for this condition if that’s something they want to do.
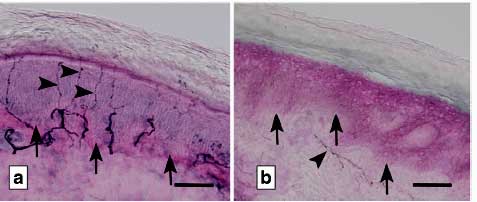
In small fiber neuropathy the small nerve fibers in the skin, cornea’s and probably elsewhere are disappearing. This was the first study to assess SFN in ME/CFS.
About a third of the ME/CFS patients – just a bit below the @ 40% generally seen in FM studies – had small fiber neuropathy (SFN) in their skin. SFN occurs when the very small autonomic/sensory nerve fibers in the skin or elsewhere have become damaged. Studies have also found SFN in the corneas of the eyes of fibromyalgia patients, and in POTS. Both Systrom and Oaklander have proposed that small nerve fibers may be damaged elsewhere such as the blood vessels or the gut.
SFN was found in both low-flow and high-flow ME/CFS patients. The authors speculated how SFN might be causing problems in either group.
- Low-Flow SFN – The authors proposed that after the blood reached the muscles, small nerve fiber problems were impairing the veins from constricting properly – resulting in blood pooling and blood loss. The reduced blood flows to the heart that resulted caused reduced preload and low heart blood flows.
- High-Flow SFN – The authors proposed that small nerve fiber problems were causing blood to be shunted away from the muscles prior to reaching them. Because less blood was reaching the muscles, less oxygen was being consumed, and less energy was being produced aerobically, – causing the muscles to produce energy anaerobically – and resulting in pain, fatigue, etc. The authors suggested that small nerve fiber losses in the gut be affecting gut motility, and causing discomfort following meals and nausea.
Update! – Ron Tompkins of the Open Medicine Funded Harvard ME/CFS Collaborative Research Center is collaborating with David Systrom to dig deeper into what’s happening during exercise. Tompkins is doing the first-ever “omics’ analysis of ME/CFS patient’s blood before it gets to the muscles (where all sorts of havoc may be happening) and after it’s passed through them during exercise.
Tompkins will be analyzing cytokines and doing metabolomics (metabolism), and proteomic (proteins) in three times points (before, during and after exercise) over 100 patients and healthy controls.
Tompkins recently reported that significantly higher levels of multiple cytokines have been found this far in the ME/CFS patients. That would fit well with Dr. Klimas’s findings suggesting that exercise triggers a burst of inflammation in people with ME/CFS. To cap the Systrom study off Tompkins will also be taking muscle biopsies and creating metabolic models.
Deconditioning Hypothesis Gets Another Body Blow
If the deconditioning angle didn’t get destroyed by Visser’s recent study (not to mention the 2-day exercise studies), it will hopefully be obliterated by this one. It’s not that deconditioning is not present in ME/CFS – it is. The question is whether deconditioning is causing these abnormal exercise results – it isn’t.
It’s a crucial question. If deconditioning is actually causing these abnormal exercise findings, then the answer for ME/CFS is simple: exercise. If, on the other hand, problems with generating energy exist – then too much “exercise” will make the situation worse.
The deconditioning hypothesis takes yet another hit. At least in the research literature it’s sinking fast.
The authors reported that the study “definitively eliminates (the) possibility” that deconditioning is causing the exercise abnormalities “because the hallmark of deconditioning is low peak exercise cardiac output” rather than the increased output they found.
Plus, instead of the high heart filling pressures seen in deconditioning, they found the opposite – low filling pressures. Plus, they noted that deconditioning doesn’t have any effect on oxygen extraction, which was low in the low-flow patients.
The ME/CFS/POTS/Fibromyalgia/Long-Hauler Mega Group
Postural orthostatic tachycardia syndrome (high heart rates, increased symptoms upon standing) and ME/CFS were linked ever closer together with the authors noting that both the low-flow and high-flow subsets found in ME/CFS are also found in POTS.

How many diseases fit into the dysautonomia, orthostatic, metabolically impaired framework?
Visser’s seminal brain blood flow study, which demonstrated that virtually every person with ME/CFS has reduced blood flows to the brain (the very definition of orthostatic intolerance) when standing, more closely links ME/CFS, orthostatic intolerance and POTS.
Given enough study – and quite a bit has already been done – fibromyalgia may fit into this group as well. With POTS and dysautonomia showing up in long COVID patients, they’re joining the club as well.
A suite of factors – dysautonomia, orthostatic intolerance, exertion problems, metabolic and mitochondrial problems – are showing up in different degrees in all these conditions. At some point, this will all hopefully merge together.
Systrom’s invasive tests are so effective and illuminating because he’s able to measure how these factors change before and after the blood feeds the muscles. Assessing ME/CFS from a whole-body perspective, Systrom is finding problems with foundational factors such as oxygen consumption, blood flows, gas levels. Workwell’s two-day exercise test (CPET) and Avindra Nath’s metabolic chambers are other ways of assessing energy production from a more macro perspective.
Muscle studies and cellular energy production studies, on the other hand, examine energy production from a more micro perspective. While the results have varied from study to study, in general, the two approaches seem to be validating each other: both the more macro and the more micro studies are finding evidence of energy production problems. The key will be in linking them together.
Check out Health Rising’s Small Fiber Neuropathy Resource Page






It is my understanding Drs. Alan and Kathleen Light at the University of Utah have been studying post-exertional genomics, metabokutes, and cytokines for some time. With striking results that separate from controls.
Please excuse my METABOLITES typo!
The Light’s produced one of the most stunning graphs I have ever seen – it showed receptors for things like ATP and signs of muscle damage, if I remember correctly, just skyrocketing after exercise. A truly impressive image.
Loved this one Cort.
My having POTS and said to have blood pooling and definite issues with blood flow and low blood volume. In my case, I have higher NE levels with standing that really causes a drastic increase with tachycardia of my heart and a recent flare we got a 160 heart rate with simple standing from a chair. (This response is my heart trying to pump blood to itself and my brain. Uncomfortable, but the lessor of the worst evil and very necessary. I don’t try to stop this.) I have to dilate my veins and not constrict them. And having too thick blood, keep my blood thinner to not be trying to pump sludge. I do have some pretty bad neuropathy. Not all POTS people can be treated the same. I tend to have higher blood pressures and my orthostatic drops bring me more into a normal range. Still with near faints at times. But thankfully, I’m not bad to faint and have enough warning to sit down. I have said for over a decade that I do better to vasodilate (to a certain level or things get worse). Its nice to see that researchers and science are coming to the same conclusions for some of us. With my recent flare (after an infection), neuropathy is definitely worse too. (Partly, seems my immune system went into overdrive to clear the infection and attacked my veins while in overdrive.) I do know that neuropathy caused by attacked nerve fibers, can be damaged by inflammation. And over response of immune system and too much ROS can create havoc. Also having too low O2 and hypoxia is very damaging throughout the body.
Nice write up CORT!
issie, grounding/earthing or placing your feet on the earth outside thins the blood among other beneficial improvements. Rubber soles on shoes should never have been invented!
@Georgia, thanks for the reminder. I love earthing. It does seem to make a difference. Grounding, seems to help sooooo many things.
Cort Johnson, you and other researchers might find this article of interest. The toxins from Cyanobacteria may be linked to these mysterious brain diseases. BMAA is one possibility as a neurotoxin. Dates go back to the 1980’s as did the Lake Tahoe CFS outbreak.
https://www.bbc.com/news/world-us-canada-56910393.amp?fbclid=IwAR2rwBut3Yr7u-ABAI0HaJjTUVbcMbkBMjZdcCnzIXRmRmS_llH_Kspvka0
@Janet, there is testing now that can show this brain “damage”. What the cause is could be varied. With me, I was having testing for CIRS (extended exposure to mold) and Lyme. A NeuroQuant MRI, is done to measure the brain for atrophy. And certain swelling and atrophied areas are assessed to see if it correlates with known patterns with those two exposures. We have been watching my brain for about 5 years now. Some things are better and some worse. I also wonder how much reperfusion with dysautonomia (and all that goes with it, blood flow issues and tachycardia – extreme fast heart rates, just from standing, upright posture), plays into these measurable brain issues. I have had both edema and shrinking of the brain. And it can change. I’m certain inflammation is a key player. And if there is prion disease or retrovirus, or even a type fungus there…….if the immune system is not detecting them and they are in a slow smolder…..that could explain a lot.
“I also wonder how much reperfusion with dysautonomia (and all that goes with it, blood flow issues and tachycardia – extreme fast heart rates, just from standing, upright posture), plays into these measurable brain issues.”
My estimate is that the same sources of damage to Small Fiber Nerves, infection, inflammation and excessive oxidative stress due to physical and mental overexertion, create havoc both at the small nerves (tissue side) AND the other end of the nerves: the brain.
Research has shown that (severe) loss of grey matter is also a clear observed statistic of ME/?FM?. Combine both problems and there is very likely a big overlap between the groups with Small Fiber Nerve depletion / atrophy and grey matter reduction and partial brain atrophy.
Love this Dejurgen:
“My estimate is that the same sources of damage to Small Fiber Nerves, infection, inflammation and excessive oxidative stress due to physical and mental overexertion, create havoc both at the small nerves (tissue side) AND the other end of the nerves: the brain.”
Why wouldn’t the brain suffer damage too: if the nerves suffer (neuropathy with dying nerves and blood flow issues), below the brain and it all being connected to the brain. Loss of signals and blood flow to and in the brain too. Good point!
Thanks. Your example really demonstrates the different ways that these problems can be produced. I imagine there are quite a few variations…
What do you think started all this off? Can you speculate?
Issie,
don’t forget worms….(see Klinghardt)
@chrisB, yes, we don’t want to forget worms…..one of the many creatures within that we seem to co-exist with. Yet causes us dysfunction when things are not kept in homeostasis. One of the things we have to detox, to improve health.
This is a very interesting avenue of research and it’s getting attention in the long hauler groups. One side note: there’s still some uncertainty surrounding the lab tests used when analyzing the fibers. I say this b/c my doctors mentioned that for me and one other long hauler, our symptoms have all the hallmarks of SPN, but our biopsies were “normal.” (Yes, this is N=2 anecdata.) So, there are suspicions that the post-Covid nerve fiber damage may be different than what’s been seen to date. Long story short: there’s new work being done on the processes for analyzing the nerve fibers.
Nerves repair / regrow very slowly.
That means: *IF* the process of losing small fiber nerves would be a continuous process (rather then a single shot process thinning out the nerves in days and then lay dormant), then the speed by which nerves are thinned out should be limited too.
Over time, with many ME/FM/POTS/… patients reaching a stable low level, average damage per month should equal average repair of small fiber nerves per month. If not, one would not level out but keep getting worse. As the body’s repair abilities per month for nerves are low, then the average damage per month should be limited too. Still, this “equilibrium” between damage and repair would result in impairing neuropathy over the long term.
In short: there is good reason to believe that losing small fiber nerves would be a slow process spread out over years rather then weeks or months.
That does not mean that Long-Covid neuropathy is not real or imagined. We ME/FM/… patients have years of experience with painfull neuropathy flaring strongly when we overdo it. It seems neuropathy (both pain and dysfunction / dysautonomy) seem to have two factors at work:
One immediate impairement of the functionning of the small fiber nerves due to the effect of the strong inflammation caused by overdoing it and another impairment over time due to the dying of small nerve fibers over time.
Hello… Well your post is thought provoking. First to say I am ill 15 years and only part of my symptoms fit CFS. it was obvious from start I have multiple immune related diseases and CFS is only one of them. After long searching I figured I have POTS and SFN. After 2005 crash I never regained previous level. Next crashes were 2014 2017 and 2020 all from antibiotics wrecking my gut. The attack ie progression of SFN was in a matter of hours… In 2020 I had an attack following too strong oregano oil and severe mold exposure without knowing for weeks…. My neuropathy progressed in 1 single day 10x and I did not fully recover nerves since then. Makes sense usually the progression is slow but all my progressions were provoked w antibiotics or toxins….. Also recently I tested positive for anti fgfr3 antibodies.. Fibrocytes growth factor.. I wonder if it has to do w nerve regrowth being blocked by these antibodies…. P. S. I sti think Sjogrens is not getting enough attention by OMF. I ENDED up proving w lip biopsy I have Sjogrens and after over 20 years of only neuropsychiatric issues I developed sicca too in 2019 after provoking myself w hormone shot…
I ended up diagnosing many friends w Sjogrens who were labelled as “ME”.
. In the end from some ttratments probably high dose vitamin D and few courses of IVIG I absolutely got rid of ME part of disease and don’t have any fatigue anymore…. I work 12 hours a day and don’t have any PEM.. however I have nerve damage, some POTS sicca… My disease morphed and fatigue was easiest to get rid of. I had massive fatigue and couldn’t watch TV or respond to emails or talk to people at some point…
Congratulations Patricia.
I think it is likely that Sjogren’s (which my mother had) is greatly underdiagnosed in the ME/CFS/FM communities. Anyone who’s doctor has told them that antibody tests can diagnose Sjogren’s should check out Lauren Stile’s story – https://www.healthrising.org/blog/2013/08/20/from-chronic-fatigue-syndrome-to-fibromyalgia-to-pots-to-success-one-womans-journey-through-the-medical-profession/
Thanks for mentioning that. The SFN in FM is actually different from the SFN in other diseases in that the fibers are both missing and the ones that are still there are smaller (narrower, I think). They call it SF polyneuropathy.
And now a different kind may be showing up. This is a field which is surprisingly understudied. I find Systrom’s idea that the small fibers are being disturbed in other places than the skin fascinating.
I found it interesting that Nath – who has been studying post-infectious patients early in ME/CFS – appears, If I got it right, to have dropped skin biopsies because they weren’t showing much. Does this mean that SFN comes later?
As DeJurgen aptly noted small nerve fibers can regrow – if we can stop what’s whacking them in the first place.
Re: Nath and NIH, I’m in one of his long Covid studies and had my biopsy done there, but it was done in conjunction with MGH (Oaklander) and sent to MGH for analysis. It was noteworthy to me that NIH didn’t do the analysis itself, given that are as big a lab as any in the world. That might reflect your point about Nath’s perspective in the sense they are not maintaining whatever capability is needed for that kind of analysis. Nonetheless, they seem to have a very strong relationship with Oaklander.
Thanks Michael – glad to hear you are in one of Nath’s long COVID studies 🙂
Oaklander has been a leader in SFN testing methodologies. I wonder if that’s why Nath went there. In any case, very glad he’s collaborating with her. The guy clearly does his homework. I was impressed that he consulted with Workwell regarding the exercise studies 🙂
I feel it will be good when the deconditioning theory can be put to rest…pardon the pun.
Not sure if i have seen any research or references here to stagnated lymph fluid for those who are unable to move much.
Improving lymph flow is certainly not the solution to anyone’s problems but could stagnant lymph fluid could be a contributor to some of the symptoms that continue to appear as people navigate their illness.
Greeeeat Q! I’m particularly curious esp since there are so many ways (even in absence of exercise) to move lymph: massage, “blood moving” herbs like ginger or rosemary or yarrow (I believe…?!!) and “alterativs” and lymph-moving herbs like calendula (or in more extreme cases if you’re a big plant geek like me POKE!) , acupuncture, heat, castor oil packs…. skin brushing I believe is said to love lymph too? There are lots of ways and I feel like WW all should develop an intuition or other ways to assess when we need to move our lymph more (maybe to prevent more immune-mediated flulike flares for some of us?)
Typos!
“MovE lymph…”
We all…”
“when the deconditioning theory can be put to rest…” I love it. Wish I had thought of it. Will probably steal it from you 🙂 🙂
Yes, somebody – I wish I could remember his name – darn it – actually has a protocol to improve lymph flow.
One idea is that the flows of both the lymph and the blood and we might as well throw the gut in there are impaired – perhaps by small fiber problems.
Do you mean Raymond Perrin, UK osteopath? The Perrin Technique involves the movement of lymph.
yes!
Cort, you did an article on Perrin in 2018.
Fort,
This is very illuminating and interesting. I wonder if this bears out what treatment modalities would look like? Any suggestions given in this new research? Would it be IVIG something else?
My most immediate OOH!!!!! here as a pharma copy editor and an herbalist in training is: REPURpOSE EXISTiNg CV DRUGS and HERBS and foods…. explore how the tools we already have for modulating the CV system can help us!!!! J like we’ve retooled drugs (and herbs 🙂 ) we tend to categorize as for the “nervous system” and the “immune system” to help us so too should we not sleep on cardiac/CV drugs!!
Should more severe ME patients be on blood thinners or anticoagulants? Even if there’s no eventual evidence for this in terms of drugs, as an herbalist I not only see no harm but tons of therapeutic/inherent overlap in therapeutic plants that target the “CV” system and that we think of as being “brain”/mind/mind-clearing herbs: centella (gotu kola), ginkgo biloba, hawthorn perhaps, Rosemary (!!! Yes regular Rosemary you read right!).
This list should be a lot longer but I’m nodding off lol…. I would add that by “herbs” here I also mean FOODs: berries, cayenne/chilis, cacao…
“Should more severe ME patients be on blood thinners or anticoagulants?”
That is IMO a tricky question. Blood is a special liquid. Unlike water, blood becomes more thick the slower it flows. A big part of that is because RBC tend to clot more when blood flow is low.
ME patients have been reported multiple times to have unflexible RBC. That makes blood slower to flow, *especially in the smallest capillaries*.
That last part is important:
Part of blood flowing poorly is due to it being too thick, blood thinners can help there. Another part of blood flowing poorly is due to our unflexible RBC. Blood thinners have no (direct) impact on that.
So: if we take blood thinners the RBC will receive no direct benefit, and blood flow in the capillaries will still be dominantly hampered by unflexible RBC. Blood flow in the larger blood vessels however will improve as there the unflexible RBC play less a role then other clothing factors.
What is the risk here? Blood flow will become (even more so) easier in the big blood vessels compared to the smaller capillaries. That risks to further divert blood flow away from the smallest capillaries to the bigger blood vessels (blood flow shunting).
If so, then you risk to have even more blood flowing around without reaching the tissue that need oxygen, nutrients and waste removal. You then IMO become sort of more a “high flow” (versus “low-flow”) person as described above in the blog. That *might* be good if you are in the low flow group, and only up to a certain point. If you are in the high flow group already then it is IMO quite questinable.
With my issues with Factor 8 and Collagen Binding, which causes too thick blood and known issues with a type fungus in my blood that causes biofilm that adheres to blood vessel walls (gotten from mosquitos and similar to malaria in function, but can also cause tumors)…..taking enzymes to help break down biofilm and to eliminate the fungus and thin the blood covers all those areas. If needed I will also use ginger. And Gingko and Bacopa (daily) help with blood flow, thinning the blood and help prevent reperfusion issues that are very possible with POTS people especially with our issues of blood flow, and help brain fog.
I wondered this too and had written Cort to see if researchers noted, but will put it here instead.
“@Cort, Did these researchers find that both could happen in the same person at different times? I can relate to symptoms of both. But Mayo said I had blood pooling and thats indicated with purple feet when standing. But I also relate to symptoms of high flow.”
So maybe as Dejurgen mentioned, at different times, we could possibly swing in either direction depending on what we have done or taken????? That could definitely cause more issues with reperfusion.
With reference to ‘Unflexible RBC…. is this referring to an inflexible membrane of the RBC???
Also, given low blood flow and volume…does this equate to an certain type of anemia? Macrocyclic, microcytic, haemolytic, pernicious, iron deficiency anemia?
Is anemia a common inclusion in ME/CFS diagnoses?
@Linda B:
Yes, RBC are ideally disk shaped cells, but they need to be able to be flexible to “squeeze” themselves best through the smallest capillaries as the smallest capillaries are smaller in diameter then the RBC themselves.
RBC that are flexible can deviate from the fixed disk form and easier adjust to the narrow opening they have to pass through, increasing blood flow a lot.
See for example https://content.iospress.com/articles/clinical-hemorheology-and-microcirculation/ch180469
“We observed from various measures of deformability that the RBCs isolated from ME/CFS patients were significantly stiffer than those from healthy controls. Our observations suggest that RBC transport through microcapillaries may explain, at least in part, the ME/CFS phenotype, and promises to be a novel first-pass diagnostic test.”
It also alligns with https://www.omf.ngo/red-blood-cell-deformability/
“In some very early data generated by this team, there are indications that RBC deformability is reduced in some ME / CFS patients.”
BUT, looking back at it surprisingly different results have been found for FM https://www.healthrising.org/blog/2018/08/15/sticky-blood-antiphospholipid-syndrome-pots-chronic-fatigue-syndrome-and-fibromyalgia/
“Two 2017 studies found evidence of increased red blood cell deformity and rapid platelet aggregation as well as increased platelet distribution width – a marker of coagulation – in fibromyalgia. A small 2018 Gulf War Syndrome study found evidence of red blood cell deformability issues.”
From those paper:
“Conclusion: Our results indicate higher erythrocyte deformability and quicker erythrocyte aggregation in FM patients.”
“Conclusions: In this preliminary study, we observed increased deformability along with increased MCH, MCHC and RDW in veterans with GWI+, which may contribute to the symptomatology of GWI. Further research is required to confirm our findings and the role of RBC microrheology in GWI.”
=> prelimary data suggests decreased RBC flexibility for ME while data suggest increased RBC flexibility for FM/GWS but going hand in hand with more aggregation (clothing).
Could that be where these diseases separate? Could that even separate the low-flow from the high flow groups or are some researchers mixing up reduced and increased deformability but all find reduced blood flow??
My gut feeling says it’s a separator, as reduced flexibility would spell most trouble in the capilaries but not in the larger blood vessels (high flow group) and increased flexibility going hand in hand with more aggregation would spell relatively more trouble in the larger blood vessels versus the capillaries (low flow group).
Thanks for asking that question and having me looking back at info!
As to annemia, it would be closer to poor oxygen provision due to poor blood flow AND poor release of oxygen from the RBC then “pure” annemia.
Wow Dejurgen thanks for the links. I am trying very hard to learn so much so please forgive any rookie questions or suggestions. You seem very informed and i thank you for your effort to consider my comments.
The Anti-phospholipid antibodies is an interesting concept. Seemingly not confirmed or replicated to a definitive point of general acceptance…if i have read the details correctly. Sad the researcher retired before nailing down the theory enough!
As the flexibility of the RBC unquestionably can be influenced by phospholipids levels (regardless of ones having or not having the antibodies)i imagine there is the possibility that Inflexible RBCs could come down to a genetic factor ..or.. It could also be influenced by poor absorption of fats as in the case of coeliac/gluten sensitive issues. Thus a deficiency of fat soluble vitamins(AED and K).
Also, gut acid levels and bile production, and microbiome play their role.
It is unsurprising there is no easy resolution to most human biological problems!!!
But, one must keep searching and asking.
No need for feeling like being a rookie. If all doctors I encountered had the amount of ME/FM/POTS/… knowledge you have, then I’d be a happy man for sure ;-).
You make a good point with antiphospholipid antibodies being able to attack the RBC cell walls. I hadn’t considered that option yet. So you are no rookie yourself either.
I think innate immune attacks (the untrained immune system), antibody immune attacks and excessive oxidative stress all can weaken the RBC cell integrity. On top of that, RBC need energy or ATP to repair themselves and to be flexible enough to bend to better squeeze through capillaries and restore to their neutral position after bending each time.
Any and all (plus some more) of these factors has the potential to represent in a fairly similar way making up part of what will be ME/FM/POTS/… but the exact mechanism by which the blood flow and oxygen and nutrient delivery and waste removal gets impaired will be different, resulting in a different mix of comorbidities I guess. So yes, better testing for APS has a chance to better find subgroups that require a more adapted treatment for best results.
Some have found APS to be an issue with blood and clotting issues. You have to have two positives for it to be considered a problem and I only got one. But I do have too high Factor 8 and Collagen Binding and that definitely causes too thick blood. So there are things that can be checked with a blood draw. Also looking at platelet stickiness. These thinks can have genetics involved. Its worth checking to see if there are issues. And may avoid some really serious problems in the future it you know about them and try to keep things within range.
Even if IVIG was a reliable treatment option with a decent success rate (it isn’t, and there isn’t enough of it in the world to treat the millions of people who have this SFN), it isn’t practical for most people. We need options OTHER than IVIG. I suggest everyone w/ neuropathy symptoms get a skin punch biopsy (Therapath lab is one that does this); it can help w/ clueless doctors (and proving disability). It may be the only “objective finding” that many patients ever get.
Sorry Cort!! autocorrect I meant Cort,
Thank you as always, Cort. Good stuff, and love ‘the gist.’ I used to have a brain that could read.
Same here Liz- love “The Gist” Cort!!
Usually it’s the only thing I can get through to stay connected to current events in ME & Fibro. Thanks for including it!!
Glad it helps! Hope it’s intelligible – its the last thing I work on…I;m often in not great shape by then (lol)
It looks like altitude sickness. Oxygen deficiency creates thicker blood. If i understand correctly.
Deconditioning does not explain orthostatic intolerance in ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome)
Visser e.a.
4 May 2021
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-02819-0
Love this post @Gijis
Visser e.a.
4 May 2021
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-02819-0
“This study shows that in ME/CFS patients orthostatic intolerance is not caused by deconditioning as defined on cardiopulmonary exercise testing. An abnormal high decline in cerebral blood flow during orthostatic stress was present in all ME/CFS patients regardless of their %peak VO2 results on cardiopulmonary exercise testing.”
Makes me think of our brain fog issues, lack of blood flow to the brain and oxygen (hypoxia)……two big whammy. And then add in perfusion damage when the blood is re-supplied. We got some serious issues going on.
🙂
Deconditioning Denied: Could a Large ME/CFS Study Put an End to the Deconditioning Myth?
https://www.healthrising.org/blog/2018/12/16/deconditioning-denied-chronic-fatigue-syndrome-deconditioning-myth/
@Gijs, Hypoxia sure does seem to be a big issue with us all.
Another great article Cort. I have been drinking the WHO rehydration drink daily for the past two months (since your article on it Cort). Although not a cure, it has helped my orthostatic intolerance immensely. I can now do light activity and standing while keeping my heart rate at a reasonable level. It is kind of a game-changer for me. I hope it keeps working. Unfortunately, I still have the neuropathy.
So glad to hear that Lynn! 🙂
Useful. What is the WHO rehydration drink and where can I find details? Can u buy packets or is it a recipe?
https://www.healthrising.org/blog/2020/09/15/saline-ors-oral-rehydration-pots-chronic-fatigue-syndrome/
There are (2) tests, very important to know.
With the skin punch biopsy, you want to analyze the epidermal AND the sweat gland fibers.
Some labs will only test the epidermal (sensory), and not the sweat gland (autonomic). And I’ve heard of people that were negative for epidermal, and positive w/ the sweat gland.
Clint,
thanks for info
would you know what labs do both?
I have SFN, but it is from B12 malabsorption, not from ME/CFS. B12 injections treat it for me.
I am curious about how many patients have difficulty with blood draws. My blood and our daughter’s clots in the tube while the blood is being draw. A 81 mg. aspirin prior to blood draw helps, but I still had to have 15 tubes of blood taken out of my hand…not fun.
This just appeared in a Florida news report. They are testing Ampligen in Long Covid.
https://www.clickorlando.com/news/local/2021/01/06/ocala-based-company-reveals-new-covid-19-drug-for-virus-long-haulers/
I recently had a sleep study and although I haven’t seen my results yet, one of the things I noticed, when I was semi-awake, was that I alternated a period of relatively shallow breathing with occasional deep breath–to kind of ‘catch-up.’ (It’s different from apnea where one stops breathing for a moment). I later realized that I also have this breathing pattern during the day.
So, little researcher that I am, I ran across something called Cheyne-Stokes Syndrome. Normally doctors think this is associated with things like heart failure, but it has since been found to be related to neurological conditions and some kind of autonomic failure. It is usually detected at night and is associated with fatigue during the day. Humm….
That got me wondering how many other ME/CFS or even fibromyalgia folks have this type of breathing–even mild, like mine. Could this be a cause or contributor to our fatigue?
This is a relatively obscure Dx and is probably not on the researchers radar yet. Anybody else breathe like this?
Nancy, i would say that i am probably in that category. I find my breathing is impaired by very narrow (and oft partially congested) nasal passages. So, its shallow breathing due to effort and eventually a catch up for some oxygen. I do NOT have ME/CFS. I am on the site because my 25 year old daughter has been affected since she was 13. BUT.. i Personally do have very low RBC level and under the radar WCC. Also ..influenced by top of the range MCV .. making the RBCs large and less able to carry oxygen. Your question actually opened my eyes a little…
So, perhaps it may be worth asking the question of how many people have this manifestation broadly in the population, or is it more common in ME/CFS?
I guess we need to keep in mind that not every symptom is part of the ME/CFS. But one cannot be blamed for looking down that particular rabbit hole….it has so many tunnels!!!!!!
LindaB, thank you so much for responding to my query! I often wonder how many people go back to read ‘older’ posts or if they just get overlooked after too much time passes…
I did quite a bit of looking on-line to see if breathing issues like Cheyne-Stokes may be a contributor to ME/CFS, just like you suggested, but alas–nothing much showed up except for the intriguing correlation with things like autonomic dysfunction. Since the topic of this blog is SFN, and it’s also speculated the nerve fibers can affect the autonomic nervous system, plus the suspected lack of proper oxygen distribution in ME/CFS–well, it just seemed to be a great big rabbit hole maybe nobody has investigated!
I agree that not every symptom is part of ME/CFS, and also that not every type of ME/CFS has all the same symptoms. Our bodies are just one big tangle of tunnels!
I feel sure that ME/CFS, which I’ve had for decades, plus perhaps my diagnosed SFN, are contributing to the notable slowness in my recovery of the use of my right arm after a total shoulder replacement nearly a year ago. That surgery was about 5 months after I broke the upper part of the humerus and an original surgery failed owing to avascular necrosis. Range of motion is returning, but restoring the muscles is harder than my surgeon anticipated, despite daily exercises and twice-a-week P.T. with a very patient and understanding therapist. Progress is “glacial” (the latter’s term). Has anyone experiences or studies we can learn from?
It would be great if Systrom could explain how his understanding of ME/CFS has evolved. In an interview with Llewellyn King a few years ago available on YouTube, he said almost all ME patients have cardiac preload failure, as measured by low right atrial filling pressures during the iCPET, and many also have poor oxygen extraction, measured by comparing atrial to venous blood gases. Now, it sounds like he is saying ME patients either have one problem or the other, but not both.
Also, are there any treatment implications for being in the high- vs. low-flow groups (i.e. mestinon for one group, not for the other, etc.).
Do you know how one would go about being tested for small fiber neuropathy?
Do you know which cytokines were found to be elevated after exercise?
What percent of (healthy or general population) people w/out CFS have small fiber neuropathy?