

In the April 2021 blog “Could High-Dose Thiamine (B-1) Help with ME/CFS, Fibromyalgia, and the Neurological Complications of Ehlers-Danlos Syndrome?” I reported on the findings of a randomized controlled trial of high-dose thiamine (for people with quiescent inflammatory bowel disease), offered several hypotheses for why high-dose thiamine might have positive effects, and speculated that it might be helpful for people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), fibromyalgia and Ehlers-Danlos Syndrome (EDS).
To gather more evidence on the potential of high-dose thiamine for people in our communities, I asked Health Rising readers who had taken high-dose thiamine in the past to complete a survey. Fifty Health Rising readers responded – thank you! – leading to a total of 55 responses that met the criteria for inclusion in this retrospective study, including a handful gathered earlier from other sources. I report here on the results of the survey.
First a few caveats.
Of the 55 respondents, 49 report having ME/CFS, 20 report having fibromyalgia, and 12 report having EDS. However, the sample is not representative of the overall population of individuals with these conditions, and thus no definitive conclusions can be drawn. Moreover, as we have learned the hard way over the years, some treatments that seem to be effective based on retrospective recollection do not end up being effective when subjected to rigorous evaluation.
The survey results should thus be understood for what they are – an initial indication of the potential of high-dose thiamine that needs to be confirmed through rigorous research. Hopefully, these results will help prompt a large, randomized study that could definitively assess whether high-dose thiamine is effective in relieving fatigue, post-exertional malaise, brain fog, and other symptoms.
Overall Results
As shown there, nearly two-thirds (65.5 percent) of respondents report either that high-dose thiamine has helped them a great deal overall or that one or more symptoms improved “a lot” without any symptom worsening (which I define as a large improvement).
Another 5.5 percent report that high-dose thiamine has improved certain symptoms “a little” (which I define as a small improvement). 14.5 percent report no improvement, 9.1 percent report a mix of improvements and worsening of different symptoms and 5.5 percent of respondents report that high-dose thiamine has made them feel worse.
This interpretation of the data aligns well with respondents’ reported satisfaction with high-dose thiamine on a five-point scale. Two-thirds of respondents give high-dose thiamine the highest marks of 5 (36.4 percent) or 4 (32.7 percent), while 14.5 percent give high-dose thiamine the low marks of 2 (3.6 percent) or 1 (10.9 percent). The remaining 16.4 percent give high-dose thiamine a middle grade of 3 out of 5.
Before exploring the specifics of the survey results, it is helpful to review respondents’ overall comments on high-dose thiamine. Below, I excerpt selected comments on high-dose thiamine from those reporting positive effects and then from those who report experiencing no effect, mixed results or feeling worse from high-dose thiamine. A complete set of comments by survey respondents may be found here.
Excerpts from comments by respondents who report that high-dose thiamine helped them:
- “The thiamine has been a game-changer, it has increased energy, greatly improved cognition and cleared brain fog, increased exercise and muscle endurance and improved some random possibly autonomic symptoms. If I could have only one supplement, it would be thiamine.”
- “It has improved my mental abilities greatly. I would crash from just conversations or thinking about something stimulating otherwise. Much greater mental and mood stability. Focus and memory.”
- “I was bedridden and have regained 75% of normal functioning with thiamine.”
- “One of the most helpful things for CFS/PEM. I could tell it was working the day following the first time I tried a 300 mg dose, then upped the dosage to that based on a study for IBS/Chron’s even though I do not have these or symptoms of these.”
- “After having severe fatigue for 28 years I am getting some help with this.”
- “It has helped my head pressure and daily dull headache… also my weak muscles in my calves feel stronger. The head pressure change is most welcomed!”
- “It helped so much I’m staying on it. My healthy husband (who is normally spectacularly in observant about his own health) volunteered, without even knowing I’d given it to him for a few days, that his memory had improved.”
- “After taking a supplement called Parasym Plus [whose first ingredient is thiamine] my life changed drastically for the better, I felt as if I was in a fog for 6 years and it was very scary, almost immediately after taking it I felt as if the fog had lifted, I could think more clearly, got my sense of direction back and was able to drive again, I had the energy sit up through an entire movie with I couldn’t do for years, it also helped tremendously with chronic edema in my legs!”
- “I used it because I had ME/CFS and had a lot of problems processing alcohol and formaldehyde (which made me really sick), I saw a massive improvement.”
- “My miracle is allithiamine- began 3/2020 and then in the month of August 2020 my high heart rate / POTS went down significantly… I just never gave up searching and wow am I so happy. The fatigue is still constant but the brain/neuroinflammation is improved significantly.”
- “After a decade deteriorating, accelerated by covid mildly 12m ago, I seem to have stabilized and the thiamine coincided with an improvement in brain fog.”
Excerpts from comments by respondents reporting no effects, mixed results or feeling worse from high-dose thiamine
- “I wish B1 would have been a miracle drug but it hasn’t seemed to do anything for me or if it has maybe I would have been worse than I am now.”
- “Seemed to improve carbohydrate tolerance and made me feel relaxed. A feeling that is super rare for me since getting POTS. Effect diminishes after a few days as though my body builds tolerance.”
- “I wish I could get it to work again. Imagine going from housebound to playing a bit of tennis. Unfortunately, after a couple of decades, my body wasn’t really ready for that and I injured myself often. I wish I knew why it stopped working.”
- “Would like to know if there is any alternative to thiamin which will work at normal doses. I am scared of taking high doses of thiamin due to long-term side effects possible.”
Now on to the details of the survey findings.
Survey Sample
Fifty-eight percent of people responded to the survey through May 9, 2021, of which 55 met the criteria for inclusion, which were reporting one or more of three conditions (ME/CFS, Fibromyalgia, or EDS) and taking 200 mg or more daily of thiamine. All but 7 of the survey responses came between April 15 and May 9, 2021, with the balance coming in the prior year. Seventy-six percent of respondents identify as female, while 24 percent identify as male. Respondents report starting high-dose thiamine between ages 20 to 81, with a median age of 50.
Of the 55 respondents, 49 report having ME/CFS, 20 report having Fibromyalgia, and 12 report having EDS. Just over half (28) report Postural Orthostatic Tachycardia Syndrome (POTS) / Dysautonomia, while a bit more than one-quarter (15) report Mast Cell Activation Syndrome (MCAS). Eleven respondents report intracranial hypertension, 9 report cervical or atlantoaxial instability, and 7 report a CSF leak. For purposes of these statistics, I have not distinguished between formal diagnoses and self-reports.
The Gist
- 55 people with ME/CFS, Fibromyalgia or Ehlers-Danlos Syndrome submitted qualifying responses to a Health Rising survey on high-dose thiamine (defined as 200 mg or more daily).
- Nearly two-thirds (65.5%) report a large improvement, and another 5.5% report a small improvement from high-dose thiamine.
- The most commonly reported improvements are reductions in fatigue, post-exertional malaise and brain fog.
- 5% of respondents report no improvement, 9.1% mixed results, and 5.5% report high-dose thiamine made them feel worse.
- Respondents report benefits in each of the dosage ranges examined.
- A more rigorous study is needed to definitively evaluate the potential of high-dose thiamine to help people in our communities.
Type and Amount of Thiamine Taken
I limited the survey to people who report having taken 200 mg or more of thiamine daily to avoid the inclusion of the many people who take thiamine only through B Complex Vitamin supplements, which often include large amounts of thiamine (though generally less than 200 mg). This is not because I have any reason to suspect that 200 mg daily is the minimum amount of thiamine needed to be effective – to the contrary, a newly released study (in preprint) suggests that administration of 100 mg of thiamine daily was associated with a substantial reduction in mortality among critically ill COVID-19 patients. Rather, it was because it would be impossible to disentangle the effects of high doses of thiamine from the high doses of Vitamin B12, biotin, and the many other B vitamins included in B complex vitamins.
Dose
Survey respondents report a range of dosages, with a median of 600 mg and an average of 865 mg of thiamine daily. Just over one-quarter of the sample report taking 200-499 mg daily of thiamine, while another one-quarter take 1,500 mg daily or more, with the balance falling in between. The most common dosages are 600 mg (9 respondents) followed by 500 mg and 1,500 mg daily (7 respondents each).
One survey respondent reports experiencing large benefits from 100 mg daily of thiamine; that response was excluded from the overall statistics to adhere to the study protocol. In comments on my original study, at least one individual also reported benefitting from 100 mg daily of thiamine. Further research is needed to determine what benefits might accrue at different doses of thiamine above the formal FDA recommendation.
Type
Nearly half (49.1 percent) of respondents report using oral thiamine hydrochloride, the thiamine form used in most of the studies of high-dose thiamine to date, while 18.2 percent report using oral benfotiamine, 10.9 percent report using oral thiamine mononitrate, and another 5.5 percent report using generic oral thiamine, which is often thiamine mononitrate. The remaining 18.2 percent report using a wide range of thiamine forms including allithiamine, lipothiamine, sulbutiamine, TPP, thiamine tetrahydrofurfuryl disulfide, coenzymated thiamine, thiamax, and thiamine HCL IM. Several respondents report combining multiple forms of thiamine; those responses have been included in the latter grouping of “other” responses, even when they report using one of the thiamine forms listed separately.
Duration
45.4 percent of respondents report taking high-dose thiamine for 6 months or more, while 12.7 percent report taking high-dose thiamine for 3 to 6 months. Just over one-quarter (27.3 percent) report taking thiamine for three weeks or less, with the balance falling between 3 weeks and 3 months. Thirty respondents (60.8 percent of respondents answering the question) report they are still taking high-dose thiamine. Four additional respondents (7.8 percent) report that they are now taking a daily dose below 200 mg.
Reported Improvements
As shown in Figure 2, most study respondents report substantial benefits from high-dose thiamine. The three most commonly reported benefits are improvements in fatigue, post-exertional malaise, and brain fog. I added brain fog to the survey midway through once respondents began mentioning it spontaneously in the comments; the adjusted levels estimate what the response would have been had brain fog been included in the survey the entire time through straight extrapolation.
More than 40 of the 55 respondents report improvements in fatigue and more than 35 report benefits from post-exertional malaise and brain fog (as adjusted). For all three symptoms, more people report that symptoms improved “a lot” than report that symptoms improved “a little.” At least one person in each category even reports the symptom went away entirely. Other symptoms with more than 10 of the 55 respondents reporting improvements include: other pain, dizziness/lightheadedness, insomnia, neck pain, headaches, and vision issues.
In addition to the symptomatic improvements captured by the survey, two respondents report benefits for dysautonomia / heart rate:
- “Whereas before my BP and HR were all over the place (hyperPOTS – low pressure, high pressure, bradycardia tachycardia), now I’m only ‘stuck with orthostatic hypertension and the tachycardia. I don’t black out anymore and my BP and HR don’t drop too low with B1.”
- “While it helps with PEM, I find that the best way to avoid PEM is to pace. B1 helps me pacing, because it brings down the tachycardia and I’m able to be upright for longer. i.e. – I can cook, with breaks or take a shower, etc. Pacing pacing.”
One respondent reports improvement in light and noise sensitivity, while another reports improvement in edema. Along with improvements in brain fog, one respondent, quoted toward the beginning of this post, reports improvements in mental abilities and mood and mental stability. Two respondents mention improvements in memory. One respondent mentions taking high-dose thiamine for neuropathic pain.
Reported Worsening of Symptoms and Side Effects
Figure 3 shows respondents’ reports of worsening of these same symptoms. Fewer than 5 people report that any particular symptom became worse, with the largest numbers reporting a worsening in headaches (4) and mast cell activation (4). Three of the 4 people who identified MCAS as a problem said the issue became substantially worse, suggesting that caution be exercised by people with severe MCAS or with an MCAS flare-up. (As noted below, however, 73% of the people with MCAS that responded to the survey report large improvements from high-dose thiamine.) One additional individual reports experiencing headaches, but they went away upon splitting the dose during the day.
Figure 4 shows respondents’ reports of the five side effects for which responses were specifically requested. Twelve people report having trouble falling asleep from high-dose thiamine, though the problem went away for 7. A few people report taking the last dose of the supplement before 5 p.m. in order to avoid insomnia, which matches the advice given by Dr. Antonio Costantini, one of the pioneers of this treatment. Nine people report having trouble staying asleep, with most of them reporting it as a moderate problem that persists. 8 to 9 people also report tachycardia and arrhythmia, mostly as a moderate problem that persists. Only one person identifies any of these side effects as serious.
In addition to the responses shown in Figure 4, three individuals report stomach issues, one identifying the issue as severe, one describing it as “stomach irritation,” and a third saying the issue went away after splitting the dose during the day. One individual stopped using high-dose thiamine, despite experiencing large benefits, due to rectal bleeding; the individual notes experiencing this symptom from many different supplements.
One individual reports getting vertigo and being unable to walk straight, but the individual resolved the problem by lowering the dose. One individual reports drying of the skin, another reports jitteriness that went away, one notes diarrhea, and another notes “significant mouth/tongue pain and irritation.”
Several individuals report that high-dose thiamine stopped working for them after a period of time. One individual found they could wait a while and then restart it successfully, while another tried this and found it unsuccessful.
What accounts for the variability in reported effects?
It is impossible to say for sure why some people appear to have benefitted from high-dose thiamine, while others appear to not have benefitted. But the survey did include several dimensions that can be analyzed for potential clues. Given the small sample size, non-representative sample, and my limited statistical skills, I did not do any sophisticated statistical analysis. But I did examine a few cross-tabulations that I report on below.
Type of Condition
As shown in the top panel of Figure 5, more than 70 percent of people who identify as having each of the following conditions report improvements from high-dose thiamine: ME/CFS, fibromyalgia, EDS, and MCAS. While not shown in the table, the same is true for people who identify as having a CSF leak and cervical or atlantoaxial instability. A smaller percentage (57.1 percent) of people who identify as having POTS / dysautonomia report benefiting from high-dose thiamine. All of these categories are overlapping, with individual respondents able to be included in more than one category.
To investigate the POTS results further, I created four exclusive categories (i.e., in which each person can only be listed once) and report on the results in the bottom panel of Figure 5. The four categories are:
- people who identify as having EDS;
- people who identify as having fibromyalgia but not EDS;
- people who identify as having ME/CFS but not EDS, fibromyalgia or POTS; and
- people who identify as having ME/CFS and POTS but not EDS or fibromyalgia.
While the number of respondents within each category is small, and so differences could be due to chance, the results for the last category appear quite different from the results of all the other categories. Among people who identify as having ME/CFS and POTS but not EDS or Fibromyalgia, 40 percent report no improvement whatsoever, a much higher percentage than any other category (see bolded cell in the last row). Perhaps a group of people within this sub-category needs a different treatment approach?
| Figure 5: Reported Effects by Condition | |||||
| Number | Improvement | No Improvement | Mixed Results | Got Worse | |
| Overlapping Categories | |||||
| ME/CFS | 49 | 71.4% | 16.3% | 6.1% | 6.1% |
| Fibromyalgia | 20 | 80.0% | 5.0% | 10.0% | 5.0% |
| Ehlers-Danlos Syndrome (EDS) | 12 | 75.0% | 0.0% | 8.3% | 16.7% |
| MCAS | 15 | 73.3% | 6.7% | 13.3% | 6.7% |
| POTS / Dysautonomia | 28 | 57.1% | 21.4% | 14.3% | 7.1% |
| Exclusive Categories | |||||
| Ehlers-Danlos Syndrome (EDS) | 12 | 75.0% | 0.0% | 8.3% | 16.7% |
| Fibromyalgia without EDS | 15 | 80.0% | 6.7% | 13.3% | 0.0% |
| ME/CFS without EDS or Fibromyalgia | |||||
| Without POTS | 13 | 84.6% | 7.7% | 0.0% | 7.7% |
| With POTS | 15 | 46.7% | 40.0% | 13.3% | 0.0% |
The EDS category has the largest percentage of people who report feeling worse after taking thiamine, but this represents only two individuals and there are potential explanations for both cases. One reports taking 600 mg of intramuscular thiamine, which far exceeds the dosage recommendations from Dr. Costantini for that form. (See discussion below). The second individual reports having a CSF leak, which can lead to alternating periods of intracranial hypo- and hypertension.
In general, I would expect people with intracranial hypertension to benefit from a carbonic anhydrase inhibitor and people with intracranial hypotension to potentially feel worse from the same agent. One respondent addresses this tension specifically: “It’s a balancing act. When I have acute symptoms of spinal CSF leaks and positional headache, I need to avoid large doses of B1. However, large doses might be helpful when the body “overreacts” and overproduces CSF when the leak is healing and not leaking as much.”
Daily Dose
Figure 6 examines how reported effects vary by daily dose among those reporting using oral thiamine. As shown there, large shares of people within each of the four-dose ranges examined report improvements from high-dose thiamine. It is interesting to see strong results reported by people taking 200-499 mg daily as the protocol that has been researched to date focuses on a daily dose between 600 and 1,800 mg, varied by weight and gender. It would be useful for future research to consider if benefits can be achieved for people with ME/CFS, Fibromyalgia, and EDS at doses below those used in prior research.
| Figure 6: Reported Effects by Daily Dose of Oral Thiamine | |||||
|
|
Number | Improvement | No Improvement | Mixed | Got Worse |
| 200-499 mg | 15 | 73.3% | 6.7% | 13.3% | 6.7% |
| 500-600 mg | 15 | 73.3% | 20.0% | 6.7% | 0.0% |
| 601-1499 mg | 10 | 70.0% | 10.0% | 20.0% | 0.0% |
| 1500+mg | 14 | 71.4% | 21.4% | 0.0% | 7.1% |
If results vary by condition, as suggested in the prior section, multivariate analysis would be needed to fully unpack any relationship between dose and different kinds of symptom improvements. A larger sample and better controls for other variations among sample members would also be helpful.
The experience of my daughter – who has EDS, craniocervical instability and Chiari malformation – may be relevant here. In ramping up from 300 mg to 1,800 mg daily over time, she experienced an almost immediate improvement in post-exertional malaise, followed by what felt like dose-dependent improvements in visual and mental acuity as we increased the dose.
In my prior post, I suggested high-dose thiamine might work through several mechanisms, and it seems plausible that one mechanism – such as increased cellular oxygen due to the production of carbon dioxide – might take effect toward the lower end of the dose range and another mechanism – such as reduction in cerebral spinal fluid – might become more impactful at higher doses.
Over time, it has seemed that my daughter needs a smaller dose to derive equivalent benefit; she is now taking 1,125 mg daily. Perhaps there is also a cumulative benefit that allows for maintenance at a lower dose?
Type of thiamine and combinations with other substances
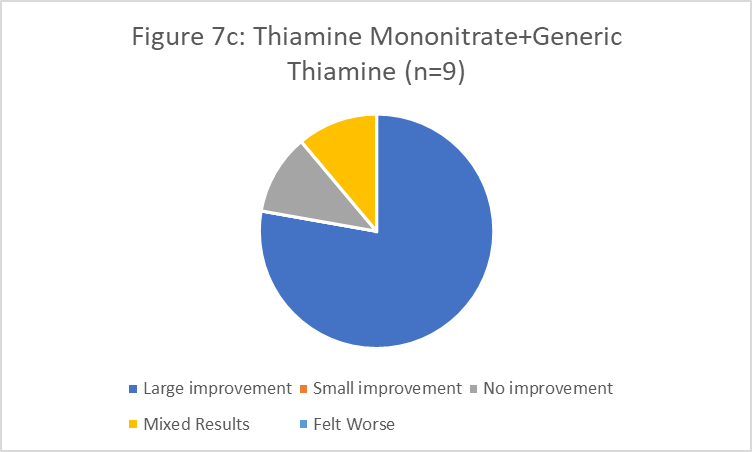
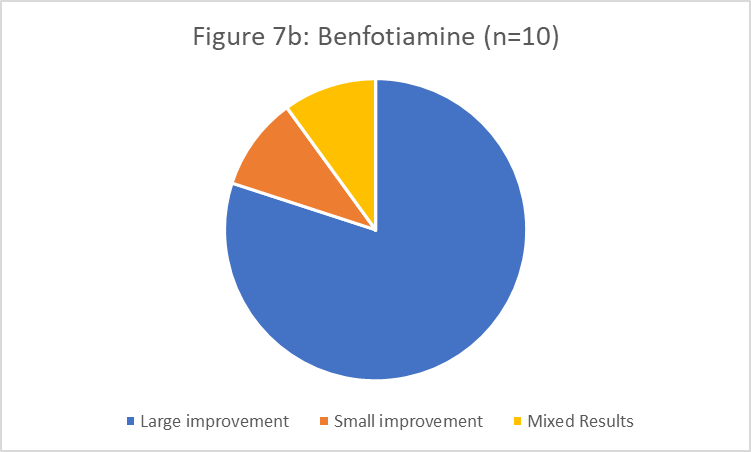
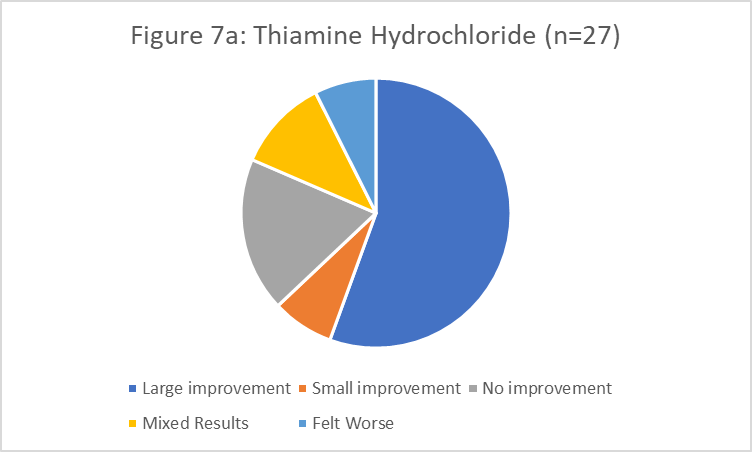
Figures 7a-7c show reported outcomes by thiamine form for the three most commonly reported forms, grouping thiamine mononitrate and generic thiamine together.
Outcomes were most consistently positive for those taking benfotiamine and the combined group of thiamine mononitrate and generic thiamine, but I would not read too much into this since the numbers within each of those groups are small and these results could easily be affected by other variables, such as the medical conditions and diagnoses of those who took different forms of thiamine.
Instead, I would argue the evidence suggests that all three forms of thiamine have at least the potential to be effective. Further research would be needed to determine if one form is more effective than others as a whole or for particular groups.
Several survey respondents comment about their choice of a particular type of thiamine. One individual reports feeling better on thiamine hydrochloride than benfotiamine, while another reports the opposite. One respondent reports feeling worse on thiamine hydrochloride and benfotiamine, but much better on TPP. One indicates that allithiamine is the form that worked best for them. Several respondents report combining two to four different forms of thiamine each day. Several individuals mention finding Dr. Lonsdale’s writing helpful in understanding the potential benefits of different forms of thiamine. Several individuals report feeling their benefits were due to taking one of the more specialized forms of thiamine (see discussion of thiamine type above); however, there were too few results for any one of these forms to analyze and report here.
One individual reports feeling somewhat worse after taking 600 mg of thiamine HCL IM. Presumably this refers to intramuscular thiamine hydrocholoride. A website associated with Dr. Costantini’s team on the use of high-dose thiamine for Parkinson’s disease suggests that one intramuscular injection of 100 mg of thiamine HCL per week is the equivalent of taking 2 grams of oral thiamine HCL daily for a week. If this information on equivalencies is accurate, the amount of thiamine HCL IM reported by this individual far exceeds in potency the amounts taken by other respondents or recommended by Costantini’s team.
Many respondents offer advice about combining thiamine with other supplements to maximize impact. Several respondents express the view that thiamine works best in combination with the other B vitamins, while another notes that thiamine is effective only when taken on its own, without other B vitamins (and without other vitamins). One respondent notes benefitting from niacin, another from B12. One individual combines thiamine with Diamox (acetazolamide) as a way of reducing the amount of Diamox needed to achieve a similar effect. These and the other recommendations provided by survey respondents, along with a copy of the survey instrument, may be accessed here.
What happens next?
I have taken this research as far as I can as a non-expert. I am hoping medical researchers and practitioners can take things from here. I see three important next steps:
1. Assess whether thiamine is a carbonic anhydrase inhibitor in vivo as predicted in vitro. This would help clarify what cautions need to be applied to the use of high-dose thiamine and possibly inform medical treatment of intracranial hypertension and other acetazolamide-responsive conditions
2. Assuming thiamine is a carbonic anhydrase inhibitor, publish guidance on how to use it safely. Many people are already using high-dose thiamine and others will likely start. It will be important for clear guidance to be available from a medical expert on how to reduce adverse drug interactions and side effects, such as hypokalemia and kidney stones. Hopefully, patients’ medical providers can provide guidance on these questions. But some may struggle to find doctors who are open to considering high-dose thiamine as a carbonic anhydrase inhibitor and aware of the possible interactions among supplements commonly used by people with ME/CFS, Fibromyalgia and EDS. It will be useful for the guidance to also address what to do in the event that high-dose thiamine stops working, a problem that several respondents report in this study. As I mentioned in my earlier column, several older studies addressed this issue in the context of acetazolamide, recommending the temporary administration of sodium or potassium bicarbonate.
(While I have no medical training and cannot provide medical advice, I would note that my daughter has found it helpful to accompany high-dose thiamine with increased fluid intake. In addition to addressing the mild diuresis of a carbonic anhydrase inhibitor, this is one of the steps Dr. Frederic Coe, Medical Director of the Kidney Stone Prevention Program at the University of Chicago, suggests to prevent formation of calcium phosphate kidney stones.)
3. Conduct a large, randomized study of high-dose thiamine to definitively assess its effectiveness in relieving different symptoms for people with ME/CFS, Fibromyalgia and EDS. Ideally, the study would include a rich set of information on the baseline characteristics of participants, including the markers of hypermobility and intracranial hypertension collected in this 2020 study. It might be useful to study different doses of high-dose thiamine to see whether there are better or different outcomes at each dose.
Conclusion
In conclusion, a huge thank you to everyone who completed the survey! I hope it will be helpful for prompting future research. I look forward to discussing the findings with anyone who wishes to comment on this post. I would be happy to speak with researchers interested in studying this treatment further.
If high-dose thiamine is a carbonic anhydrase inhibitor as predicted by an in vitro study, it is a serious drug and should be approached cautiously. I would recommend that individuals interested in trying high-dose thiamine discuss with their medical providers if this is a safe treatment option for them given their individual circumstances and other medications and supplements.






A clinical trial would be great but in the meantime this is convincing enough for me to give it a go on myself and my son (both with mecfs, son also with pots)! Thanks for running the poll.
Thanks for your work on this Jeffrey. Like others I appreciate your diligent and restrained approach to what appears to be a promising avenue of exploration.
Personally, I tried ramping from 500mg to 2000mg of B1 (thiamin HCl) over a week and then stopped after noticing no change. (I’m in the FM/CFS camp & EDS adjacent.) Are you aware of anyone that’s experienced improvement after taken high dose B1 for a while, or should any effect be fairly immediate, as your daughter (I take it) experienced?
The survey didn’t ask how long people took high-dose thiamine before noticing an improvement. In my daughter’s case, she felt the effects of a higher dose after 2-3 days, so I would think you might notice the effects within a week. Some people reported that one form didn’t work, while another did. For example, one person said that thiamine hcl worked for them while benfotiamine didn’t (or made them feel worse) while several people said benfotiamine worked when thiamine hcl didn’t. Several people spoke highly of allithiamine. Dr. Lonsdale recommends a type of thiamine called TTFD for people who struggle to absorb standard thiamine. See https://www.hormonesmatter.com/ttfd-thiamine-derivative/ I cannot recommend for or against it, but am passing on that information. Some of the respondents to the survey said this form worked best for them. But one of the commenters on this post said they felt worse after taking that, and preferred one of the more traditional thiamines. At this point, we still don’t know enough about why some people with these conditions respond to high-dose thiamine and others don’t and whether switching to a different form of thiamine might help. Hopefully we can stimulate more research on these questions.
I saw remarkable results on 300mg B1 and B2 in 48 hours after working up gradually over a weeks time. Fatigue and PEM were gone. I now take 200mg but if I stop the fatigue comes back within a few days.
You might find a different type of Thiamine would work better. Some do better on Benfotiamine, or TTFD. Also some find their symptoms not improving or getting worse because the use of one isolated B vitamin may potentially deplete others. Because B vitamins are synergistic, they all support each other in various ways.
Also, in some people it can take a lot longer than one week to really start seeing benefits &some people, possibly due to the presence of certain Thiamine-depleting gut microbes or parasites need to mega-dose before they get benefits. I wouldn’t dismiss Thiamine out of hand without experimenting more with it, personally.
Check out the Hormones Matter website, & Elliot Overton’s website (also as EONutrition on YouTube).
Suffered for 3 decades, went low carb for years some improvement went carnivor a lot of improvement, did my own research, added nicotine and thiamine a lot of improvement added benfotiamine raw egg yolk have my life back, mechanism. Aceticholine is made from choline by B1, nicotine stimulates the receptors for aceticholine. There is another pathway that uses calcium channels in mast cells try 3 herb formula a Chinese herb mix if the above does not help you
My congratulations Jeffrey for your high quality organization and analysis of this survey in a methodological way.
While you lack resources and formal medical education, to me you beat hands down the quality and methodology of one of the biggest and most expensive studies in ME’s history: the 5 million pound PACE research.
It may seem a very low bar to compare your work with the PACE fiasco, but the point is to compare your level of professionalism compared to these professionals having access to far more patients, equipment and funding.
While your study, as you say, has its limits due to what you had available to work with it speaks highly of your qualities and sincerity as a researcher if you can beat hands down the quality of a multi million pound research project led by medical professors.
Your will and genuine determination to try and get as good as possible to the facts *as they are* and proceed while keeping the value towards the patient key and central is what sets you apart from those that wasted far more resources resulting in more damage then good.
Thank you Jeffrey, we need more people like you!
Thanks for the positive feedback, @dejurgen! I hope the study proves helpful in laying the groundwork for future research.
Ditto for me. Those of us suffering from this hopeless illness rightfully will make someone like you our hero. It gives us hope, and we really need that. Thank you!
I just started taking benfotiamine and it’s unbelievable. After extensive research it appears that beriberi in it’s beginning stages affects autonomic nervous system, dysautonomia ( pots) , panic attacks, central sensitivity, etc, etc. It reduces AGE’s by 40 percent, allows carbs to be converted to energy, basically enabling our body to work as it should. I have been able to eat without passing out for three days, no naps during the day, fibro pain reduced. Excellent article http://www.hormonesmatter.com/beriberi-the-great-imitator/
This is thoughtfully and clearly presented – the more so because the caveats aren’t glossed over. Thank you Jeffrey. Do you – or any others – know how straightforward it is to obtain oral thiamine hydrochloride in the UK? Any advice on the best product to buy? There appear to be both standard-release and slow-release tablets, and I’m not sure if either of these require a doctor’s prescription in the UK. Grateful for any thoughts, and thank you again.
Thanks! In a response to my earlier blog post, Paul noted that G&G sold versions in the UK of 100 or 500 mg, without fillers. Someone else had purchased Solgar in the U.K. My daughter uses standard release format, in 3 divided doses.
Thank you
BTW I have your daughters same conditions. Thank you for the article,
Great, now I have to buy *another* supplement to try. Hopefully this one won’t end up in my supplement graveyard with the others.
yeah, supplement graveyard. it is hard to be hopeful all the time, huh.
Wow. Thanks so much for this study. Very encouraging results
I failed benfotiamine for fibro pain. What is the difference between benfotiamine and thiamine hydrochloride?
Benfotiamine is a human-made derivative of thiamine that is reported to have greater bioavailability than the more common thiamine hydrochloride. Some of the people in the survey suggested they had tried one form before finding success with the other. Other people who did not have success with either one turned to more specialized forms of thiamine that Dr. Lonsdale has recommended. As you can see from the survey, some individuals reported modest reductions in pain from thiamine, but the larger and more common improvements were in fatigue, post-exertional malaise and brain fog. In case it is helpful, my daughter has found Low-dose Naltrexone to be helpful with certain kinds of pain.
Great information and presentation !!
Thank you.
Will be trying this.
?
Benfotiamine does not cross the blood/brain barrier. It is recommended for diabetic nerve pain. I took it for well over a year not seeing any noticeable results but as soon as I learned it didn’t enter the brain I switched to standard thiamine and had remarkable results. It took me a week to ramp up to 300mg but then withing 48 hrs the fatigue and PEM were gone. The fatigue comes back if I stop the 200mg I’m on now. Look up the symptoms of Beri beri (thiamine deficiency) it’s the symptoms I had on Benfo!
I don’t know if anyone will see this now, but as a result of these articles/blogs (thank you Cort), my doctor prescribed 200 mg benfotiamine, and I started taking it the other day. I was hopeful, as day one in the late afternoon, I seemed to be able to do a little more exercise than the very controlled little I do. Yesterday, mid day though, I started feeling really well. So, as per T Allen’s comments here, it sounds like I need to ramp up. Do you have suggestions on how to accomplish that?
Cort, would you be able to put me in touch w T. Allen?
I meant to say below or above, “I started feeling really weird.”
There is a study somewhere that showed fibromyalgia in very many cases to be a prelude to dementia. It’s been shown that excess histamine in the brain leads to neuron death causing dementia over time. It’s also been shown that high dose thiamine lowers histamine in the brain. Benfotiamine on the other hand, despite the way it is marketed, it has been proven in studies that it cannot cross into the brain. I know this from reading a lot trying to figure out why benfotiamine didn’t work for me. I suspect that if it doesn’t work and thiamine hcl does work, then your issue may be due to histamine killing neurons in the brain.
Thanks for info, very interesting. My wholistic M.D. consultant for fibromyalgia, which she thinks it’s a mitochondrial disorder, just prescribed 250 daily benfotiamine for me. I’ll see if she is aware it doesn’t pass the blood brain barrier. I’ve never heard of an FM-histamine-dementia association, though.
Thanks Jeffrey for a great contribution! Hopefully those working on ME/CFS, Long Covid and other chronic disease research will take notice.
Yes! Any trauma or stress wipes out B vitamins (& magnesium) faster than a bullet train! So much money is being spent on post COViD symptom support, yet therapeutic supplementation may well have far more remarkable & rapid effects.
We are made of the elements. We run on the elements. Micronutrients are required for every function & process in the body. Thiamine is the ‘spark’ that fires the engine. Every process also requires energy. Post-viral malaise syndrome is a reduction in the ‘spark’ & consequent down-regulation of less critical functions & processes when Thiamine & other supporting vitamins & minerals have been depleted.
Thanks for doing all this, Jeffrey. Fantastic job well done!
I supposedly became victim of B6 toxicity. It’s not wellknown but vit. B6 can accumulate in your body and lead to B6 toxicity. (for some people) Does anybody know if such a thing can happen with vit. B1 ?
If you get a B-complex vitamin, or a multiple vitamin, formulated for interstitial cystitis, it will not have vitamin B6.
Thanks Betsy didn’t know that
Interesting! Do you happen to know if it has a genetic component? My B6 levels are at the very top of “normal” with no supplementation.
I’ve done well on 750mg-1g of benfotiamine daily. After hearing the Derrick Lonsdale disciples go on and on and on about TTFD, I got some Thiamax and got neuropathy within 10 days of trying 300mg daily of it instead of my usual benfotiamine. It took me a couple of weeks to realize what was causing the neuropathy, and it took about a month for it to go away.
Thiamine is a key part of the transsulfuration pathway, along with molybdenum. This is why if people are taking other B vitamins, NAC, and/or glutathione, the thiamine might be helpful, as toxins liberated by these other things can finally leave the body.
Learner1, I have found that I get neuropathy from all B Vitamins … I have not worked out why this is, but it seems you are saying that taking different forms may avoid the problem?? Is that your experience with taking benfotiamine?? I might have ago with that and see. Thanks for posting your comment!
Maybe I am looking at things the wrong way, but I have always had reservations about trying medications and supplements to alleviate symptoms, without a clear understanding of the underlying disease cause and mechanisms. The recommendations are all over the place, and I used to take so many different things that there was no way to know what might actually be helping or making things worse. I finally quit taking everything except the couple of things that my blood test showed I was actually low on (vit B and D).
Maybe I am needlessly suffering, but I use my symptoms as a guidepost for my pacing. What concerns me about taking meds/supps is this – pacing is hard, very hard. Sure, when I am crashed its pretty easy to do nothing, but as a lifelong ‘go-getter’, any time I start to feel even a little better it is SO hard to still do so little activity (my 2day CPET showed my day 2 anaerobic threshold to be at a mere 81bpm). So my concern is this – if I take something that relieves my symptoms, I will be much more prone to overdoing it, and ultimately making my actual underlying physiological condition worsen. How can we know if the thiamine (or anything else) is actually helping the condition improve, or if its acting as a sort of ‘analgesic’ that allows for expanding activity, but ultimately at an overall cost down the line? Another example is when people suggest stimulants – sure, they might give me energy now, but I know what the ultimate cost will be. As much as it sucks, I am willing to endure suffering that informs me over alleviating it at a longer- term cost.
Maybe this is more of a discussion on general approaches to disease management than one on thiamine supplementation, but I am curious how others see this. I welcome your thoughts, thanks!
You raise some good questions, and perhaps others will want to chime in based on their experience. The questions you raise highlight the importance of better understanding the mechanism though which thiamine works. High-dose thiamine is certainly not a cure. But if thiamine works by increasing the oxygen available for cellular respiration and clearing lactate and increasing blood flow to the brain, as I hypothesize, then it should help improve the underlying physiological condition that is constraining activity. Having said that, I certainly think it would be important to be careful in scaling up physical activity to try to find whatever new thresholds or limits apply, without crossing them and crashing. As with most treatments for these conditions, being careful and taking things slowly seem to be in order.
Thanks Jeffrey
Jeffrey Lubell, I, we, a 1000 Tradesmen were exposed to Pulp Mill Emissions building a New Recovery Boiler and Electrostatic Precipatator, Project duration f 2002-04. I was only exposed 3 weeks. In hindsight after studying the Environment Canada Report for the Mill, it Listed 72 Chemical’s and Solvents if the Daily Tonnage was felt to be high enough. Aldehyde the hangover component of Legal Drinking Alcohol was in the Soup! We were suffering burning feet, and Worker’s were Buying more comfortable Work Boots. Ie; the Red Wing Comfort Force were the last resort to No avail!
I was Driving stupid after work, and a co-worker was in a Collision and Charged with Impaired Driving. I found Dr. Lonsdale story in earth and soil in 2004, and was able to correspond by Email as it was listed in the document. The Thiamine alleviated my snoring and Sleep Apnea, as dozens of us were Booked with a Sleep Disorder Clinic. I couldn’t use the C-Pap Pump because of the Neurotoxin Ethylene oxide is used as a plastic Softener in the Tubing.
When I get exposed to Vehicle Exhaust i suffer Neuropathic pain in the lower limbs and aching in the Tri-geminal area of the Jaw.
Pain Relief would be within 5 minutes after using THORNE, Solvent Renover or MAX GXL, a similar Compound blend.
I was like you and very very careful when my fatigue and PEM went away with thiamine. It took me 8 mths (Fall thru Spring) to get brave enough to start working hard enough to realize I wasn’t going to relapse. After pacing for 18 months it was scary to watch my pulse go over 100bmp but eventually I figured out nothing was going to happen. That doesn’t mean when I work outside in the yard/garden for 4 hours I’m not tired but it’s normal fatigue and the pain is normal muscle strain. My heart rate climbs to between 125 and 140bpm usually when I’m getting tired or have been doing something strenuous but it drops immediately when I rest. This is not an analgesic or stimulate. my genetic testing indicates I may need more Vit B2 so I’m not surprised I need B1 as well. Other supplements are know to deplete B vits so it could be related to that as well. The good news is it will only take you a couple of days to know whether it will help or not. I worked up gradually over a week to 300mg of B1 & B2 and 48 hrs later my PEM pain was gone and the ME/CFS fatigue was gone as well. I now take 200mg/ day and if I stop the fatigue starts coming back within 3-4 days. I’d suggest trying it. It could change your life for the better!
Thank you T. Allen. I went by the weight chart by weight. I started out with 500 mg, then to 1000 and a few days later, 1500. I felt no benefit with the 500 and 1000 mg doses, and when I went to 1500, I felt really bad; it’s hard to describe. Since most are finding benefits at much lower doses, I will start over.
Hi T Allen, I’d be interested to know what genetic testing you did if you don’t mind sharing? I didn’t know there is testing at a genetic that can indicate what you might be pre-disposed at having a deficiency.
Doesn’t your urine goes neon yellow with such high doses of B2?
Mine does with just 30 mg.
Don’t you take a B complex?
I’m building up extremely slowly on TTFD, which I take with Thiamine HCL and also a low dose B vitamin. I must take all B vitamins in the morning and finish by lunch, or I get insomnia. I’m intolerant to methyl B types so I avoid them.
I got worse for the first 5 days on Thiamine, the paradoxical reaction as Prof Lonsdale calls it. I’ve now turned the corner and can feel the benefits. I have Fibro, mild/moderate CFS (way worse after C19 shots), HEDS, POTS, Interstitial Cystitis, IBS, Raynauds, Endometriosis stage 4 and I’m in perimenopause. I work a desk job 30 hours a week mostly from home. Pure suffering for anyone with this level of disability because even that crashes me into PEM. On any given day I also have tremors and many symptoms of early Parkinsons. I truly recommend reading Hormones Matter. Chip away at it slowly because you will PEM just reading too much! Also EO Nutrition (Elliot Overton) on YouTube.
Finally too, go look at Sally K Norton – worth listening to on YouTube – she understands oxalates deplete B1.
Thank you so, so much for this article and survey. It really gives me hope.
yes, “T” , good point. It is so hard to not overdue it regarding our activities…as we pay for it the next day. This is such a challenging condition… thx Cort for this forum, great info and support group.
I have tried thiamine in the past with no noticeable improvements and so now just take a B complex. Perhaps I will have to try a higher dose. I’m not sure about how all the B’s interact, but having a MTHFR mutation, the complex I take is with as many methylated forms as possible–even if they are not folate. This does make me wonder if there is such a thing as a mutation in processing B1 which has yet to be identified.
Thank you for this survey result breakdown Jeffrey!
Now to add to ‘T’s comments about trying to identify which supplements may or may not work (and finally capitulating to pacing), I have noticed a definite improvement in my energy (and haven’t addressed my hypopnea sleep issues yet).
I’m not entirely sure which new addition is helping (and there are about 3 which I need to sort out). Usually I try things one at a time, but I suspect one if these new additions is actually the one which is having an effect.
I have skin breakouts and got a new dermatologist who suggested I drink several cups of spearmint (not peppermint) tea as a therapy. After researching this tea, trying it and peeing way too much, I discovered the main active ingredient was Phenolic Complex which includes Rosmarinic acid.
Since I have been taking this Phenolic Complex for about three weeks now (Swanson), not only is my skin healing very quickly (which is surprising for someone who has Ehlers-Danlos which is known for slow wound resolution), but I am experiencing a very noticeable uptick in energy.
Not sure what to make of this, but I am now doubling my dose and will see what happens.
I wish I was on this trial fibro muscles n fog
This sounds very useful and hopeful. Thanks for all the work in putting this together!
These results are very promising. Please try allithiamine (TTFD), large doses. This is a much better absorbed form see https://www.youtube.com/watch?v=R01PRRF3774
Thanks for your work on this Jeffrey. Like others I appreciate your diligent and restrained approach to what appears to be a promising avenue of exploration.
Personally, I tried ramping from 500mg to 2000mg of B1 (thiamin HCl) over a week and then stopped after noticing no change. (I’m in the FM/CFS camp & EDS adjacent.) Are you aware of anyone that’s experienced improvement after taken high dose B1 for a while, or should any effect be fairly immediate, as your daughter (I take it) experienced?
My effect was quick. I ramped up to 300mg over a week and 48hrs after starting 300mg I was pretty much back to normal. So sorry it didn’t work for you! I recommend everyone get genetic testing , Real Time or Great Plains are often mentions. My test said I needed more B2 so I took B1&B2 at 300mg.
Not sure if this is useful info but… in the Thyroid community Izabella Wentz promotes the use of Thiamine to help reduce symptoms of fatigue and fogginess … perhaps some more data could be gathered there as to its usefulness and dosage etc.???
Thanks!
Jeffrey, As I am sure you know….Ehlers-Danlos syndrome is a group of inherited disorders that affect your connective tissues — primarily your skin, joints and blood vessel walls. Connective tissue is a complex mixture of proteins and other substances that provide strength and elasticity to the underlying structures in your body.
Ehlers-Danlos is not ME/CFS although some symptoms may be similar.
I am concerned about recommending a treatment that appears to be effective in EDS for ME/CFS which clearly has a different cause(s).
That said, thiamine has been used in detoxification of lead poisoning in sheep, but it also depletes zinc.
https://www.researchgate.net/publication/226081291_The_therapeutic_potential_of_thiamine_for_treatment_of_experimentally_induced_subacute_lead_poisoning_in_sheep
It can be dangerous to treat yourself with high doses of anything unless you know the potential consequences.
Thank you Betty – that’s important and helpful information. I rarely reply to you, but wanted to say that I always very much appreciate your comments.
I have/had CFS/Fibro etc but not EDS. 300mg B! & B2 worked for me, I now take 200mg/day. I also supplement zinc. Thanks for your always helpful comments. I agree people need to be under a knowledgeable DRs care (if you can find and afford one) or be really good at doing your own research. It’s a full time job managing these diseases even with a Drs help!
I’d like to second what dejurgen and Jacob Richter have said above. Thank you, Jeffrey, for your careful, and balanced(!), analysis.
I’m starting to feel that knowing what the possible wrinkles or downsides are to any particular treatment is as – or more – valuable to me than knowing what the possible upsides are.
I ended up not completing your survey, as I had such complicated up and downsides that it wasn’t possible to fill it out, except by using ‘other’ in every possible category, which wouldn’t have provided good data. Plus I hadn’t really been on a high dose long enough. I’m very grateful you’ve published your results here; it’s giving me a lot to consider.
I’d also like to strongly support what ‘T’ said above, and Nancy’s comment on more investigation needed re: possible mutations in processing B1. I’ve ended up having to discontinue taking B1, and wonder if that may be an issue for me, and perhaps some of the people who answered your survey? I hope any follow-up to your survey will examine this, because B1 shows so much promise for so many of us.
Unlike Nancy, I had very strong reactions, both positive and negative (T’s points are valid here, I think), and am still having reactions after stopping it for a few days. It’s taken me some time to put it together, but I now recognize many of my negative reactions to thiamine were similar to ones I had years ago when I tried DHEA, and Maca (it was suggested to me as the safest and most gentle adaptogen).
DHEA gave me horrid stomach and intestinal pain, and eventually overall body pain, with pronounced dysmotility. After a few weeks B1 was starting to do the same (similar to people on your survey), after initially having done the opposite.
Maca, in me, which I understand was an uncommon reaction (but not unknown in a subset of women), appeared to convert almost entirely to testosterone, which produced pronounced aggression. Although it didn’t produce the same physical effects as Maca, B1 for me ramped up an alarming level of irritability and at times aggression – which I now suspect may have been testosterone – but at the time my reading suggested increased B1 might be increasing my need for B3, and B3 deficiency can produce aggression. Maca, like DHEA and B1, also produced the same time of ‘clenching’ stomach pain, although to a much lesser extent.
So I’m wondering if B1, like the other supplements, is somehow being diverted to produce too much testosterone in me, and if so, whether that might indicate one of those possible genetic subsets that Nancy was wondering about that respond differently? And whether the people who answered your survey who identified stomach pain might possibly be producing testosterone &/or are in that genetic subset with me? Perhaps some of us need a more comprehensive approach (perhaps more than just B1) in order for B1 to work safely?
I then added a small amount of B3, which produced no results (no flushing, no reduction in aggression). Because I’d read that one shouldn’t take B vitamins in isolation, I then added a very small amount of B-complex (1/8th of a capsule), upon which I had a strong anaphylactic attack – which I hadn’t had in decades. The strongest one I’ve had to date. Apparently something in the B-complex seemed to activate the B3 (which I hadn’t reacted to previously), which seemed to provide rocket fuel for anaphylaxis (with facial swelling, hives, and loss of muscle control, so not just a B3 flush).
I’ve since spoken to my allergist who says that allergy to B-complex isn’t unknown, but that B-1 by itself shouldn’t be an allergic trigger and saw no problems in continuing it, despite my anaphylaxis. But he cautioned me to stay away from B-complex.
A student I was seeing at the Naturopathic college a few years ago said that my case had been presented to the students as ‘a textbook case of dauer’. B1 most certainly has seemed to kick me out of a dauer state, which at first was glorious. But, as per T’s point above, I’m now thinking my body went into that state for a valid reason, and I shouldn’t be messing with that lightly. Of course, dejurgen’s point about refeeding syndrome, and Dr. Lonsdales about paradox also seem to be relevant.
I’m reading more lately about an overall deficiency in nutrients thanks to industrial farming practices, and wonder if missing nutrients overall (more than just B1) is a significant factor for some of us.
I very much hope your work will get picked up and carried forward by researchers with funding. The first few days on B1 were so wonderful that I would dearly love to find some way to overcome the negatives. I’m hoping someone will consider following up with an interview &/or more research on re-feeding syndrome / paradox reactions to help those of us with negative reactions (and our healthcare providers) better navigate.
It sounds like you got some very interesting – and promising – results, and some equally important information about cautions. Thank you for doing this.
Thanks! I have issues with Vit B12 even though I’m not MTHFR. Nothing on my genetic testing about B12 but if I take more than 33mcg a day I’ll start getting really tired. The B! & B2 work great as long as I don’t take B12. One of these days maybe someone will do the research and figure out what on earth is going on. 🙂
@Anne, you aren’t alone in anaphylaxis with Niacin. It does me that way too. That flushing action triggers MCAS with me. My throat and nose will swell shut and my face swell. I could take a very small amount of niacinimide in the past. But I just stay away from it.
I do good on B1 and take 100mg. It has helped my ability to walk properly with my muscle strength being improved. I had a tell tell sign with one eye starting to track wrong and that is a sign of needing B1. It straightened that up too. (Both can also be signs of MS. But, I don’t have that DX……) B1 is one of my must haves. It has improved my strength and stamina.
B vitamins are synergistic and all support each other in various ways. I do believe that taking one in isolation could potentially deplete others. I know that if I ramp up Thiamine I also need to increase B12 or I start to get low B12 symptoms.
It seems B1 not only needs other B vitamins, but also enough magnesium, potassium & zinc too. And if taking zinc it may be advisable to take copper occasionally too.
On the histamine issue with the B complex, it’s possible you might have been reacting to a filler rather than the actual vitamins, but interestingly I discovered quite by accident a few years back that drinking plenty of water when I felt a histamine reaction coming on, nipped it in the bud. Every time. I also read more recently on a nutritionist’s website that a histamine reaction can be a sign of cellular dehydration which tied in with my experience.
It made me wonder whether it’s an indication the body needs more water in order either to metabolise the food or substance, or in order to utilise it or something in it for some purpose or function. But whatever the reason, it works & I’m grateful.
So here’s a real novice question: are people in the study taking these forms of thiamine by capsule, by injection, sublingually, by oral suspension? Or is this irrelevant? Does the form of delivery not matter? Esp. do capsules seem to be hunky-dory? Asking because I seem to get really nauseated after any capsule/tablet form of b vitamins — except sublingual B-12, which I take occasionally. Otherwise, I just can’t seem to stand b-vitamin complexes, for sure, or individual B vitamins, though I haven’t tried Thiamine.
One person mentioned taking high-dose thiamine through intramuscular injection. I assume the rest used oral tablets or capsules. There are sub-lingual thiamines available, but I do not have any experience with them. My daughter has problems taking certain other B vitamins in large doses, but not thiamine.
You may be sensitive to the never-ending supply of additives and fillers they put in capsules and even liquids (especially the bleeping food coloring, sweeteners, etc). I recommend taking all B vitamins separately and not complexes because the doses are too high in complexes. I can’t more than 33mcg B12. I Have to get that from drops or I get very tired. I can’t take any Vit B6, my levels are too high without taking any. See my point? but check the ingredients in the capsules and find the “cleanest” (least “stuff”) you can. Stick with well known brands too! NOW, Nature Made, Natures Way. Compare labels on Amazon and track how you feel. Eventually you’ll figure out what is making you feel poorly. Good luck!
@Cort, @Jeffrey
In the past Cort wrote several times about research on how, when the body could not produce enough ATP, it could convert two ADP to one ATP plus one AMP. That AMP then however was irreversibly lost so that is a very expensive emergency operation to produce small emergency amounts of ATP.
In the past I did found one way to recover this AMP back to ATP/ADP but it was fairly elaborate through many steps.
Rereading above comments had me dig in some deeper again. Look what popped up:
Wikipedia(Thiamine_diphosphokinase)
“In enzymology, a thiamine diphosphokinase (EC 2.7.6.2) is an enzyme that catalyzes the chemical reaction
ATP + thiamine ⇌ AMP + thiamine diphosphate
Thus, the two substrates of this enzyme are ATP and thiamine, whereas its two products are AMP and thiamine diphosphate.”
=> It goes BOTH directions, and as such thiamine diphosphate CAN recycle AMP back to ATP.
Wikipedia(Thiamine_pyrophosphate)
“Thiamine pyrophosphate (TPP or ThPP), or thiamine diphosphate (ThDP), or cocarboxylase[1] is a thiamine (vitamin B1) derivative which is produced by the enzyme thiamine diphosphokinase. …
…TPP works as a coenzyme in many enzymatic reactions, such as:
Pyruvate dehydrogenase complex[6]
Pyruvate decarboxylase in ethanol fermentation
Alpha-ketoglutarate dehydrogenase complex
Branched-chain amino acid dehydrogenase complex
2-hydroxyphytanoyl-CoA lyase
Transketolase”
=> So thiamine diphosphate is both common and the enzyme to convert thiamine to thiamine diphosphate is a common human enzyme. Humans can have a disease due to deficiency of this thiamine diphosphokinase enzyme further indicating it is a human enzyme. Looking that up is always necessary as some science is written for other organisms without mentioning that.
=> Humans have all what is needed to convert AMP back to ADP/ATP.
=> This allows this emergency conversion of 2ADP to ATP and AMP to last WAY longer before ATP and ADP (and phosphor) gets depleted.
=> This emergency reaction could take place at high speed at ischemic zones in the body and recycling AMP back to ATP could occur at well oxygenated places in the body like the liver.
=> Another possibility is to convert 2 ADP to ATP + AMP during short bursts of energy consumption at the site of energy burst and then recycle it back after that burst at the same site.
=> The last option would actually act near IDENTICAL as the creatine – phosphocreatine pair in allowing for a quick rechargeable buffer to inter-convert these two substance and get ATP for quick energy use bursts or use ATP to recharge the “battery” after the quick energy use subsides.
=> Given enough thiamine in the body this mechanism has potential to be roughly equivalent to the effect of the creatine – phospocreatine pair buffer (estimate for equivalent potential: see below)!
Wikipedia(Phosphocreatine)
“A 70 kg man contains around 120 g of creatine, with 40% being the unphosphorylated form and 60% as creatine phosphate.”
Estimating the amount of ATP in the human body was a bit more challening. From Wikipedia(Adenosine_triphosphate)
“The energy used by human cells in an adult requires the hydrolysis of 100 to 150 moles of ATP daily, which is around 50 to 75 kg. A human will typically use up their body weight of ATP over the course of the day. Each equivalent of ATP is recycled 1000–1500 times during a single day (100 / 0.2 = 500).”
Combining that info: total ATP usage a day 100 – 150 moles or 50 to 75 kg, total number of recycling operations a day 1000 – 1500 moles. This yields 50 kg / 1000 or 75 kg / 1500 = 50 grams of ATP in the body if I am not mistaken.
Conclusion:
* Several researchers indicated that during very high peak load / shortages of ATP, the body could convert 2 ADP to 1 ATP + 1 AMP but at a very high cost: the irreversible loss of the AMP reducing total amounts of ATP available in the body and leading to phosphor loss in the body (ME patients have been found low on phosphor).
* We provided above a very straightforward way to recycle that “irreversibly lost” AMP back and do so even without the loss of energy: 1 amount of energy used for “recharging this battery” gives us a readily usable amount of the same 1 amount of energy for later use. That is as good as the creatine-phosphocreatine buffer and far better then anaerobic lactate generation from glucose with 3 to 1 loss in energy.
* Sufficient amounts of thiamine plus the needed enzymes to get this reaction going thus can increase the anaerobic buffer AND provide a mechanism to reduce ATP (AMP) and phosphor loss.
* This buffer would also allow for less “spikes” in NADH and NADPH availability in the mitochondria, somewhat reducing oxidative stress as excess NADPH causes bursts in oxidative stress. Excesses and shortages in NADH / NADPH are easily created during varying load as the mitochondria are slow to adapt production under varying loads. Providing more buffer capacity for energy by an extra recharging mechanism can flatten that out.
* The above should reduce lactate, increase breathing and oxygenation ability… …and, predicted based on those ideas, better blood/body phosphor levels.
Do we have a REAL winner here???
Forgot to mention: the above idea also ties in with the observation of Ron Davis that our cells / bodies do a very rare and unique thing: ME cells dump ATP into the blood.
Next to provide ATP to whoever cell that receive this ATP, they also allow the amount of ATP to temporary increase in locations that need it, temporary increasing this hypothetical buffer.
Without any real option to convert AMP back to ATP / ADP, it would be hard to see that our bodies rely extensively and frequently on this option as discarding so much ATP / ADP is a rather costly option.
This thiamine-AMP recycling route offers the option to use this route a lot more frequent and to a higher extend (converting a much larger percentage of 2 ADP to 1 ATP + 1 AMP.
Our ME bodies making fairly extensive use of this “newfound” ability to convert *much* of our ADP to ATP + AMP might be in line with some important observations.
After a burst in energy usage, our bodies would have to replenish / recycle both AMP to ATP, creatine to phosphocreatine and thiamine to thiamine diphosphate to be back “up and running” again.
Supposing this extensive conversion of 2 ADP to 1 ATP + 1 AMP happens a lot more frequently in us then in healthy people as we are more often in deep need for emergency ATP, our recovery from a burst of energy usage / activity should be a lot slower then that of healthy people.
When one only has to tap into the creatine – phosphocreatine buffer, one has regular total amounts of ATP / ADP available after exertion. So, both the Krebbs cycle (mitochondria) and glycolysis can proceed at normal speed.
When we / ME patients also have to tap fairly deep into this buffer of converting 2 ADP to 1 ATP + 1 AMP, then we have a significantly reduced pool of ADP (after exertion) that the Krebbs cycle and glycolysis can use to convert to ATP. Hence, ATP (energy) production slows a lot down.
That has a big impact. Suppose, pure hypothetical example, that we dig deep into our buffer and convert 40% of the ATP + ADP pool to AMP (in order to make emergency ATP / energy). This AMP “sits idle” till it is either converted back to ATP by our hypothesized thiamine recovery mechanism or till it is permanently lost and discarded.
So, a quick bit of math could say we can only produce 60% of normal rates of energy. So, recharging our phosphocreatine buffer and recycling AMP back to ATP + ADP should also be slowed to 60% of normal speeds right?
Wrong!!!
Recharging a buffer can ONLY be done with spare energy. Suppose that 50% of the energy our cells (dominantly the mitochondria) produce is normally used for basic cell metabolism (survival, defending against oxidative stress, doing absolutely needed functions like having minimum levels of nerve and brain functioning…), then when we have 100% of our combined ATP / ADP pool we have:
100% production – 50% for basic needs = 50% of energy production left for activities PLUS recharging of our buffers.
When our common ATP / ADP pool is reduced to 60% in this hypothetical example, we have:
60 production – 50% for basic needs = 10% of energy production left for activities PLUS recharging of our buffers.
=> While we had “only” a 40% reduction in available (mainly mitochondrial) energy production, we got an 80% reduction in combined energy available for activities PLUS recharging of our buffers.
=> Our body MUST in this example inhibit our will to do any activity as the smallest activity eats up all of our “free” energy production leaving us no ability to recycle AMP back to ATP before it gets lost. Hitting the wall and being utterly depleted after exertion and feeling like @@@@ sure is something we know…
Keep in mind that we likely not only have a reduced total (mitochondrial) energy production when that happens, but likely the other side of the equation, the needed energy to fight oxidative stress is increased with us too increasing the “reserved” amount of energy needed for basic survival.
=> So, ME patients likely have frequent strong reductions in ATP / ADP pools but also increased base needs for ATP in order to fight oxidative stress. If so, this further hampers recovery to normal-ish ATP levels and increases chances for untimely AMP recycling and phosphor loss.
One “good” way to partially prevent this very slow (to lack of) recovery is to channel a lot more glucose into the anaerobic / glycolysis pathway. Why? Because both the Krebbs cycle (mitochondria) and glycolysis would be hampered by this reduction in combined ATP / ADP pool. Both would be slowed down.
BUT the glycolysis pathway has far larger excess capacity, being far better able to make up the slowing down in conversion speed due to reduced ATP / ADP pools by “just” increasing the enzymes needed to speed up the anaerobic / glycolitic pathway.
This is in line with what research has shown: we / ME patients have far easier lactate production with modest effort and it often lasting (and even starting later after exertion) way longer then what is seen in healthy people. Rather then “plain” lack of oxygen delivered to the cells, it could be nothing less then lack of enough ATP / ADP pool to be able to run the mitochondria at normal speed. That also would be in line with so many observations that there is oxygen in the blood but the cells seem to be unable to use it.
=> Rather then unable to extract the oxygen from the cells, could it be the mitochondria often lacking enough ATP / ADP pools to be able to USE that released oxygen and hence needing more glycolysis in order to try and recover ATP / ADP pools?
Increasing thiamine should offer chances for going less deep into this prolonged state of severely depleted ATP / ADP pools by offering faster speeds to convert AMP back to ATP at any site anywhere in the body who has sufficient energy to spare.
Hence: possibly faster recovery from PEM.
As both brain cells and nerve cells are often firing fast in bursts, having a better buffer mechanism can make energy production, energy availability and amounts of ROS / lactate production better.
Combine the above three: less to no PEM, less brain fog and less neuropathy (for those it works for) are close to the key benefits Jeffrey’s inquiry found. By chance, those likely are the key beneficiaries from a bigger (hypothetical) ADP to ATP and AMP buffer paired with better recycling of “unrecoverable” AMP.
WOW, Dejurgen…..I love it when you get the science to explain the effect and give the WHYs.
I knew B1 was a keeper for me! One of my much needed “purple bandaids”?
Hey Dejurgen, did you finally crack the ME/CFS code around the time of this comment? I’m just curious as to why we don’t see your amazing analysis and hypotheses around here anymore….
Thinking of it, Cort wrote a blog on https://www.healthrising.org/blog/2021/05/06/small-nerve-fiber-snf-energy-chronic-fatigue-syndrome/
Only a subgroup of the patients had poor oxygen extraction with high oxygen levels in their RBC that returned to the heart and lungs. The patients were divided in a high flow and a low flow subgroup. The high flow group was the one with reduced oxygen extraction.
I wonder if there would be a big correlation between the group that is “high flow” and responds fairly well to high dose thiamine… If so, it would provide some additional insight in these ideas but more importantly help predicting who would be more likely to benefit from high dose B1 based on testing.
Note: for those thinking the
ATP + thiamine ⇌ AMP + thiamine diphosphate
reaction can’t be used to recycle (net) AMP back to ATP because thiamine first has to be converted to thiamine diphosphate and that converts ATP to AMP to start with.
Thiamine chemistry seems to have plenty of enzymes for transformations between its different forms. One is Wikipedia(Thiamine-phosphate_kinase) that does:
ATP + thiamine phosphate ⇌ ADP + thiamine diphosphate
So, thiamine diphosphate (needed to recycle AMP back to ATP) can be made without creating AMP.
For those still saying you need somehow AMP to create thiamine phosphate there is Wikipedia(Thiamine_kinase) that does:
ATP + thiamine ⇌ ADP + thiamine phosphate
=> So overal:
Have ATP + thiamine ⇌ gets you ADP + thiamine phosphate (using thiamine kinase enzyme)
Have ATP + thiamine phosphate ⇌ gets you ADP + thiamine diphosphate (using thiamine phosphate kinase enzyme)
=> Overal 2 ATP + thiamine ⇌ gets you 2 ADP + thiamine diphosphate (using thiamine kinase and thiamine phosphate kinase enzymes)
So, you can create thiamine diphosphate without creating AMP. Then, you can use ATP + thiamine ⇌ AMP + thiamine diphosphate to recycle AMP back to ATP by using the reverse reaction (as the reaction goes both ways).
Very misleading, clickbaity title. “Nearly” 2/3 — of 49 people? Out of millions with ME/CFS. And no mention of long-term adverse effects, including downregulation of endogenous thiamine systems, which potentially can have serious consequences.
This is typically the kind of non-scientific “information” that ends up hurting people, in my experience. I thought Health Rising was better than this.
I agree–please revise the title
The titles are usually kept quite short for search engine optimization purposes. Having them longer – and more informative – means less people will be able to access them. We added survey respondents to the title if that helps.
The size of the survey is not a problem, though. Many, if not most studies, actually have FEWER participants than did this survey. No studies include millions of people with FM and few contain hundreds. None are completely representative. All require multiple studies for validation. We have never, by the way, reported the number of participants in a study in the title. We always make sure to include that in the blog itself.
The main thing was that the title was accurate. I was a bit surprised, though, that we didn’t put ME/CFS or FM in there. In retrospect that should have been done not only for accuracy but to draw people with ME/CFS or FM to the blog.
Anyone who decided to check out the blog, however, would quickly realize that it was based on a survey of 55 people with ME/CFS/FM. So long as the survey is accurately identified as such in the blog and that the author notes that further studies need to be done to validate the results – which was done by the second paragraph – I am satisfied.
(Anyone who would take high-dose thiamine based on the title of a blog (I would be shocked if anyone would do that) without checking out the dose or results – would hardly care how the results were produced.)
As to problems of “long-term adverse effects, including downregulation of endogenous thiamine systems” nothing showed up in a web search regarding that or a search of medical journals on PubMed.
Thanks for this great piece. The prospects are exciting.
It’s interesting that some folks with csf leaks got benefits as my understanding is that thiamine can lower intracranial pressure almost as much as Diamox, and the issue is pressure that’s too low. Though many folks with csf leaks have EDS and CFS, etc.
I have tried for years to get this researched. It has largely fallen on deaf ears. So what is the mechanism? First, thiamine deficiency (TD) has been known for years to cause beriberi (interpretation, I can’t, I can’t). This emphasizes the knockdown fatigue that is a salient symptom. Beriberi is a polysymptomatic condition that embraces the symptoms of many diseases. None of the symptoms are pathognomonic (indicative of) of the disease, so what indeed is the mechanism? The truth is that thiamine, together with magnesium, has many responsibilities in the production of ATP, the energy currency of every one of the 70-100 trillion cells that make up the body. Even a minor deficiency causes symptoms that are common, many of which are causing sufferers to visit a physician. Because the lab tests do not address the real issue, they may be attributed to other more medically acceptable causes. If normal, the physician may tell the patient that “it is all in your head”. The trouble is that if the true cause of symptoms is not recognized and its cause not defined, the symptoms will gradually worsen and become progressively harder to treat. This might explain why some patients get a dramatic response to thiamine, while others get some or no response. The polysymptomatic nature of beriberi is because every cell in the body cannot function with an inadequate supply of energy, so a tremendous variety of symptoms can develop, depending on the deficiency distribution. However, the brain, heart and nervous system are the major tissues that consume 4+ oxygen to make energy, so they are first to be affected. Please remember that “a thought, an emotion, a single step” all require energy. That is why a high IQ is more at risk from poor diet than someone less endowed. Until this becomes more medically acceptable, these disasters will continue. Please go to Amazon books and read the reviews on Lonsdale D, Marrs C. Thiamine Deficiency, Dysautonomia and High Calorie Malnutrition. 2017, Academic Publishers. For example Ehlers Danlos, Salt Losing syndrome and POTS are all examples of a range of conditions under the broad title of Dysautonomia. All of them are examples of cellular energy deficiency that could be from TD or other causes of energy depletion. To those searching detailed information the book is readable enough. It was written with patients and doctors in mind. Just skip the highly technical issues.
Dr. LONSDALE,
I hope that you will continue with your life work and continue to try to get people to “pay attention” to it.
With me, B1 has made a difference.
When someone has experience with something, yet it is not as well known (or more – not in focus to mainstream) its hard for some to get on board and listen. But, for some of us, it is much appreciated and gives us another WHY. Getting to the core and knowing the WHYs, makes for a much better result when the right combinations come together.
Thank you for your life work and being persistent to get the message heard and it help others.
I know how discouraged one can get when you have spent years to try to get more people to listen and it seems to fall on deaf ears. But know that your life work, has not been in vain. There are some who it has helped and made a difference. I for one, Thank you!
I would love to read your book and the technical parts of it too. That part, I would enjoy!
Issie
If you find any researchers to do further studies and need someone to do statistical analysis, I’d be happy to help. My PhD is in Developmental and Biological Psychology, not anything medicine-related, but I have statistical experience. (I’m an assistant professor and teach Psychological Stats. If you google “Jessica Kraybill executive functions” you can find some of my research articles as well as my dissertation; they have nothing at all to do with this field but demonstrate my statistical experience.) I’ve had long COVID since March 2020, which has morphed into CFS/ME and MCAS, so this is an area that I’m very, very interested in. Thanks muchly for your work – appreciate it!
Thanks for offering to help with statistical analysis. Would welcome a chance to discuss further. You can find my email through my letter to the editor to the journal Alimentary Pharmacology and Therapeutics (on thiamine of course).
Wow. After reading this blog, I bought a jar of B complex vitamins – the store didn’t have B1 alone and I was anxious to try it. I felt marked improvement that same day! I’m only on day two and am taking 300mg thiamine per day, and I’m still feeling much better.
Thank you so much for sharing this information. I’m almost in tears because it’s so hard to find anything that helps. In over 12 years with ME/CFS, I have only found two other things that helped at all. Valcyte was a miracle drug until I was on it for way too long and had very scary side effects, and lexapro, which helps somewhat, but not as much as the Valcyte. So I’m ecstatic to find something else (that’s nontoxic!!!) that helps! It’s certainly not a cure, but so far, it’s added several hours of functioning to my day. Knock wood that it continues to help!
THANK YOU!!!
I am very glad to hear you are finding a benefit! In the survey results, people described being careful in slowly increasing their physical activity so as not to exceed their new aerobic thresholds. This seems like sound advice. Good luck!!
It would be interesting to see a trial of sulbutamine which consists of two thiamin molecules which are absorbed as a whole. It is usually used as a smart drug, but it should have a even better effect than ordinary thiamine.
The thiamine derivatives are very interesting, but I don’t know a lot about them. In case others are interested, there’s a lit review here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7210561/. Another one to look into is TTFD, which Derrick Lonsdale calls the promising promising of the thiamine derivatives.
My partner has had ME/CFS for 7 years. After reading this article she began taking 100mg / day Thiamine Mononitrate. She started that low as she’s often found new supplements cause her issues but are better tolerated after a while.
She’s now been taking 100mg B1 for the last 23 days. Her previous continuous cycle of combinations of gut problems / headaches / gland issues / rash symptoms disappeared almost immediately & there’s been no 23 day period – or anything like – in years that she’s felt so OK & been so symptom-free.
Before B1 she was having to work really hard to get upstairs in the evening. She’d often stop & rest part-way & looked as if she was battling up a mountain, now she’s walking straight up them. Last weekend we were out at a barbecue until 12.30am – without repercussions beyond her feeling ‘a bit tired’ the next day. Yesterday she went for a walk – walking’s always been something she’s able to do a surprising amount of for someone with ME, but she needs to take it slowly. Yesterday she realised she was overtaking people!
We’re not now planning to increase the dose or change the brand or type of B1 she’s taking. Instead she’ll slowly explore the improvement. There are already indications she may now be able to eat a wider variety of foods without triggering gut issues. We’re hoping she’ll be able to do a bit more while still resting each afternoon (she already has been doing more, we’re just beginning to think a bit strategically!)
We’re absolutely delighted with what certainly appear to be B1’s miraculous results. Thank you so much for all the work which went into the survey. This surely merits serious & significant research.
So glad to hear your partner is doing so well! From what I’ve heard from others, it seems prudent to take things slowly as she explores her new capabalities and limits. Hope things continue on an upward trajectory!
Is she still good? Does she takes only Thiamine? Not others B?
Thanks
Translated from French: Hello, the supplementation in thiamine also requires supplementation in magnesium, this may explain the lower effectiveness on some people.On the other hand I do not know what to take in quantity, nor if it is essential to associate it with B6.
I found thiamine hcl incredibly helpful, going into remission for about 3 days at a dose of 1200mg a day (I titrated up over 7 days). Prior to this it felt like thiamine wasn’t quite working, I felt slightly dizzy until I reached the 1200mg dose and then the dizzy lifted and that was when remission started. While it only lasted 3 days I titrated down to 300mg over a week and stayed at that dose.
I noticed this had a huge effect on clearing my mental fog and increasing blood flow to the brain (swelling at the back of my head and neck resolved). It’s quite easy to identify if this is happening, you will feel a warm damp cloth feeling on the skin at the back of the head and this may radiate down into the neck. If this happens you know that blood flow has increased in that area.
I haven’t taken any for quite some time as I found a new protocol that’s resolved most of my ME symptoms. I only relapse when I get a covid vaccine. But as that protocol hasn’t been a cure, just a huge boost to my overall severity and state, I think adding thiamine 300mg a day back in is a good idea. Especailly as it might be great for covid19 infection (the verdict seems to be out however I can find 3 studies on thiamine and covid19)
https://pubmed.ncbi.nlm.nih.gov/33817670/ – this one states that there was a huge impact when thiamine was given by IV to patients in hospital.
Another shows that thiamine hcl at doses of 300mg is sufficient to create a good level of thiamine in the blood serum for 10 hours after oral administration. So bioavailability does not appear to be an issue. Higher doses of 1200mg showed a much much higher saturation of blood serum at 4 hours declining over a further 10 hours.
Did you take other co-factors? Or just Thiamine?
What’s the new protocol that you find that resolved most of your ME symptoms?
Thank you for your efforts, input and information. I think we need all the help like this we can get. The conventional medical field proves to be less than acceptable when it comes to thrying to help. THANK YOU!!
I would be interested to know how long it takes to notice the effects. I took thiamine HCL for a couple days (several hundred mg’s, don’t remember exactly) and stopped taking it since I didn’t notice anything. But sometimes you notice the effects after multiple weeks only.
Do all forms of Thiamine increase the risk of kidney stones, or is it specifically Thiamine HCl that has this effect?
I would greatly appreciate any information anyone has about this.
Many thanks.
All forms of thiamine ought to have the same effect. Just to be clear — I am not aware of studies that have found that high-dose thiamine increases the risk of kidney stones. Instead, I am flagging this as a potential concern based on the evidence that thiamine is a carbonic anhydrase inhibitor. Kidney stones are a well-known risk factors of carbonic anhydrase inhibitors. The advice that I have seen to address this risk is to stay well hydrated through increased water intake.
Thank you very much indeed for getting back to me so quickly, – I’m extremely grateful.
Just one more thing: do you know what kind of kidney stones Thiamine is apt to cause, – assuming, as you say, that it is a carbonic anhydrase inhibitor.
The stones that result from acetazolamide (another carbonic inhibitor) tend to be calcium phosphate stones: https://pubmed.ncbi.nlm.nih.gov/3433023/ . The kidney stone prevention program at the University of Chicago recommends increasing fluid intake and lowering sodium and sugar to prevent these types of stones. https://kidneystones.uchicago.edu/idiopathic-calcium-phosphate-stone-formers/
Hi, I am reading this interesting information just now. Anything new since this was published? Any new research or more experience of people? thanks!
I’ve completed and updated my survey. The responses of 108 individuals with ME/CFS, Fibromyalgia or EDS are summarized here. https://twitter.com/JeffLubell_C19/status/1638097484047163393 . And here: http://www.high-dose-thiamine.org/results-of-high-dose-thiamine-survey/
That’s great, thank you very much
As a medical Optometrist, I’m impressed with how much better I feel on Thiamine 500/d
I take metformin and a multivitamin for years and didn’t expect more mental and physical energy but that is the result!
Hi, This makes me want to try B1; even though the study is ridiculously flawed. Things like this are dangerous when published. You have ask people to respond. Which determines that your sample is not representative of the MECFS community. A large number of people were negatively affected. In a true representative sample B1 is likely to cause harm to a far greater number of people. Please do not publish this unsubstantiated rubbish. Wait until you have some valid evidence.
Our Facebook group, Parkinson’s thiamine hcl, is hoping someday to release Thiamine hcl into a cadre of healing. We have19,000 members