

An $8 million clinical trial of a mitochondrial enhancer, no less, in ME/CFS? I thought I was hearing things but it was so, and, in the end, it even makes sense given how rapidly some parts of this field are moving forward. But first, a little backstory.
A Pulmonologist Takes On ME/CFS

Systrom is not your usual pulmonologist.
David Systrom is a pulmonologist – a doctor who specializes in lung conditions – not exactly the kind of doctor you might expect to be interested in chronic fatigue syndrome (ME/CFS). In fact, until Systrom came along, I don’t know if we had any pulmonologists interested in ME/CFS.
Systrom, though, is different. The vast majority of pulmonologists focus entirely on the heart and the lungs – which don’t appear to be damaged in ME/CFS – but ignore the other side of the respiratory system that involves the blood vessels and muscles.
At best, most pulmonologists passed their strange exercise-challenged patients off as mysteries. At worst, they sent them off to their local psychologist. Instead of punting on his patients, though, Systrom dug deeper. He was the first to examine in a really detailed way people with exercise intolerance who lacked the heart or lung problems that most pulmonologists concentrated on.
In a recent call, Systrom related the story of a very well-respected exercise physiologist who asked him – after learning that the exercise tests must be done upright to capture what’s going on – something to the effect of: “Do you mean I’ve been wrong to tell my patients they’re deconditioned and crazy?”.
Over time, Systrom’s invasive exercise tests have provided novel insights into the exertion problems people with ME/CFS, POTS, long COVID, and similar disorders face. From mitochondrial issues, to left to right shunts, to hyperventilation to lo-flow and hi-flow subsets, Systrom has been redefining how we understand these diseases.
A Very Low Oxygen Extraction Group
Really good research takes on a life of its own and so it has here. Systrom had his eye on a particular subset of ME/CFS patients who exhibited more difficulty extracting oxygen from their blood at peak exercise. At the very point that their muscles were screaming out for more oxygen, their mitochondria simply weren’t taking it up.
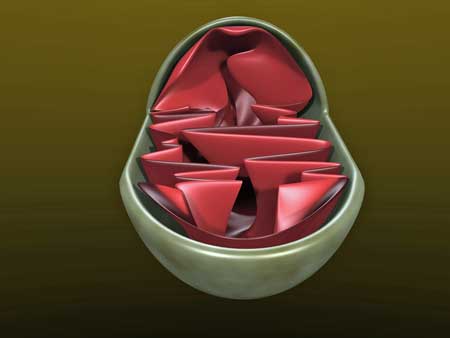
Mitochondrial abnormalities were found in a group of ME/CFS patients with particularly low oxygen extraction levels during exercise.
That suggested a mitochondrial problem might be present. In general, mitochondrial disorders are thought to be genetic but Systrom stated that he’d learned long ago that some mitochondria problems are “acquired”; i.e. that they are simply chronic diseases that show up over time.
Suspecting this was happening in some of his patients, Systrom sent 11 ME/CFS patients to Dallas to get a needle muscle biopsy, which was then sent to Baylor for tests of mitochondrial functioning, electron transport chain activity, and mitochondrial enzyme activity.
If my notes are correct, ten of the eleven patients tested positive for a mitochondrial disorder, with most displaying citrate synthase deficiency – which Systrom stated was thought to be a marker of global mitochondrial dysfunction.
ME/CFS Mitochondrial Study Underway

The Japanese drug company Astellas is funding an $8 million dollar trial of a “mitochondrial stoker” in ME/CFS.
I doubt that even Systrom expected what happened next. Astellas, a multinational pharmaceutical company in Japan, with a branch in the U.S., had apparently been keeping an eye on his work.
Astellas is a large company with dozens of clinical trials underway, many of which are focused on cancer, but it also has a “Mitochondria Biology” section that is funding trials of a PPAR-β/δ receptor modulator called bocidelpar ASP0367/MA-0211. It’s assessing this drug – which is not FDA approved and not available in the U.S. – in a variety of disorders including Duchenne muscular dystrophy, hypoxia, metabolic disorders (aka ME/CFS, renal failure and mitochondrial myopathies.
Bocidelparis is a most intriguing drug for ME/CFS as it appears to be modulating the same peroxisome proliferator-activated receptors pathway (PPAR) that has recently popped up in both chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). This pathway plays a major regulatory role in energy homeostasis and metabolic function, and has anti-inflammatory properties. The PPAR-β/δ receptor Astellas is interested in metabolizes fatty acids so that they can be used to produce energy.
First, Paul Fisher’s novel cell culture study in 2020 identified a flood of mitochondrial problems in ME/CFS – including problems with beta fatty-acid oxidation.
Next, Ian Lipkin’s metabolomic study, “Evidence for Peroxisomal Dysfunction and Dysregulation of the CDP-Choline Pathway in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome“, this year put a spotlight on the peroxisomes’ PPAR pathway in ME/CFS.
Plus, a 2020 fibromyalgia (FM) study found fatty acid metabolism problems in a subset of FM patients. Dietary restrictions, MCT oil, and mitochondria enhancing supplements reportedly were helpful.
The PPAR-β/δ receptor drug Astellas is targeting increases in fat burning capacity during exercise, and enhances the development of type I muscle fibers. It’s not clear if a drug targeting that particular receptor would help a little, a lot, or not at all with the Complex V issues Fisher believes are present in ME/CFS.
Astellas, though, is excited enough to pump $8 million into a clinical trial of a “mitochondrial stoker” in ME/CFS. I almost had to pinch myself when I heard that: a major drug company interested in ME/CFS? Trialing a “mitochondrial stoker” to boot?
In some ways, though, it makes total sense. Systrom, after all, has three things Pharma has been looking for in ME/CFS for quite a while: (1) he has a way to biologically distinguish a subset, (2) he is able to biologically assess treatment effectiveness, and (3) his tests of effectiveness directly impact the magic word “functionality”.
Except for the fact that the invasive or rather the “advanced” exercise test is expensive and well, invasive, Systrom’s testing regimen would be a slam dunk. (Systrom stated that he’s continually looking for less invasive ways to get his results and has some ideas on how to achieve that.)
The 11-week clinical trial consists of 40 ME/CFS patients with some long-COVID patients being added. An initial invasive exercise test determines which participants are eligible for the trial. (Participants need to have peak exercise ([Ca-VO2])/[Hb]) ≤ 0.85 and VO2max < 85% predicted.) The trial is expected to end about this time next year.
The subset of ME/CFS patients that could potentially be helped, if this trial works out, is not small. Systrom stated that the 1,500 invasive CPETS he’s done over the years suggests that 20-25% of ME/CFS patients have enough problems with oxygen uptake to at least meet the criteria for the study.
Systrom noted that getting a mitochondrial disease diagnosis without evidence of family problems; i.e. that a genetic disease is present, is difficult, as getting insurance to pay for the diagnostic procedures needed is near impossible. That could change if Systrom and this study can show that the mitochondrial problems in ME/CFS are not necessarily genetic in nature.
The Mestinon Clinical Trial
Mestinon has been mentioned with respect to ME/CFS for years. Living with Chronic Fatigue Syndrome reported that Dr. Goldstein considered it one of his favorite drugs for ME/CFS and that Dr. Blair Grubb finds it helpful in some of his POTS patients. With the results of Systrom’s proof of concept, the Mestinon clinical trial should soon be published in the Chest journal, and with his years of data on people with ME/CFS, Mestinon may be on its way to becoming a real thing in ME/CFS.
Systrom believes that by triggering the release of norepinephrine, Mestinon is causing the veins to properly narrow, thus propelling blood back up to the heart and giving the muscles more blood. He notes that retrospective studies – studies done after the fact – suggest that pyridostigmine for ME/CFS can improve oxygen uptake, end-tidal carbon dioxide levels, and ventilatory efficiency. Until now, though, no studies have actually directly measured Mestinon’s effect in ME/CFS.
The Gist
- A Harvard pulmonologist, David Systrom, has found that oxidation extraction problems are common in a substantial subset of people with ME/CFS. The low oxygen extraction rates indicated that their mitochondria were not taking up normal amounts of the fuel they need to produce energy – oxygen – during exercise.
- Suspecting that mitochondrial problems were present, Systrom had muscle biopsies taken of ME/CFS patients who’d displayed very low oxygen extraction rates during peak exercise. Analyses found mitochondria problems, with citrate synthase deficiencies being particularly common.
- Astellas, a multinational Japanese pharmaceutical company, with dozens of clinical trials underway had apparently been keeping an eye on Systrom’s work, and is now funding a (very) rare randomized, placebo-controlled clinical trial in ME/CFS.
- The $8 million trial is assessing the effectiveness of a PPAR-β/δ receptor modulating drug called bocidelpar that is currently being assessed in mitochondrial diseases as well.
- The PPAR receptor modulating capacity of the drug is intriguing as two studies in ME/CFS and one in fibromyalgia have recently turned a spotlight on this particular aspect of mitochondrial function.
- If having a drug company take an interest in ME/CFS is unusual, having a drug company fund a mitochondrial drug trial seems off the charts rare, but Systrom had three things going for him: he’s able to biologically identify a subset, and biologically document progress, and the progress he’s documenting – the ability to exercise in a more normal way – directly impacts functionality.
- The only thing Systrom is missing at this point is an easy way to do this. Invasive exercise tests are expensive and, as their name denotes they’re rather invasive (blood is collected from arteries and veins during the test). Systrom hopes to find a way to gather the data he needs in an easier fashion.
- If ultimately successful the subset of patients this drug – which is not FDA-approved for any diseases – could help could be substantial as approximately a quarter of Systrom’s patients probably meet the criteria to be in this study.
- Systrom is also conducting a proof-of-concept biologically based Mestinon trial that is having patients exercise – take Mestinon – and then exercise again to determine if Mestinon improved their ability to produce energy during exercise.
- Several other studies are digging deeper into the breakdown that occurs when people with ME/CFS exercise. Two are assessing cytokine production and proteomics during exercise, and Systrom is working with Peter Novak to determine if the small fiber neuropathy found in the skin of many people with ME/CFS and/or fibromyalgia and/or long COVID extends deeper and is producing autonomic nervous system problems across the body.
- Finally, the NIH long-COVID RECOVER Initiative has formed a commonalities task force to explore the intersection between long COVID and ME/CFS and other post-infectious diseases. Systrom co-chairs the exercise subcommittee and has reported to the NIH on his findings in ME/CFS and long COVID.
Since we know that Mestinon helps some but certainly not all people with ME/CFS or POTS, it was good to see a Congressionally Directed Medical Research Program grant to Dr. Rosa Maria Pari Ñaña will help her identify patients that are likely to benefit.
A positive Mestinon result could pave the way for a larger clinical trial. That trial wouldn’t likely be funded by a drug company, though, as Mestinon is a generic drug, and drug companies aren’t interested in funding trials on generic drugs.
That would leave the National Institutes of Health (NIH) as one of the sole potential sponsors. This drug, in fact, seems perfect for the NIH. It’s a generic drug with a long safety record. If Systrom’s trial provides solid biological evidence of benefit for a disease like ME/CFS – which has no FDA-approved drugs – one wonders what excuse, if any, the NIH could come up with to explain turning down an opportunity to fund a trial.
Another ME/CFS researcher, Dikomo Shungu has paved the way here. The NIH’s ME/CFS program announcement still will not allow funding for clinical trials (something that has galled Nancy Klimas, in particular, for years), but Shungu took another route and succeeded. It was his biological data that undoubtedly turned the tide.
After Shungu produced preliminary evidence that high-dose NAC could help in ME/CFS, the NIH funded his expanded ME/CFS clinical trial.
Charting the Exercise Breakdown in ME/CFS
Really good studies open more doors and Systrom has been stepping through quite a few lately. Several studies underway are building on his iCPET studies to further uncover the biological effects exercise has on ME/CFS. A hopefully soon-to-be-published paper, for instance, assessed whether exercise triggers a burst of inflammatory cytokines.
Another study the Open Medicine Foundation helped fund is doing proteomic analysis of samples taken during the exercise.
Systrom is also in the midst of a Department of Defense grant that is funding the interaction between blood vessel dysregulation and small fiber neuropathy. Systrom was the first to document damaged small nerve fibers in the skin of about 45% of people with ME/CFS. He believes the real action, though, may be happening deeper. He’s proposed that the small fiber neuropathy found in the skin and eyes of people with ME/CFS and fibromyalgia extends deeper than the skin and is affecting blood flows to the muscles.
He’s working with Peter Novak to do deeper biopsies that capture sweat glands in the thigh in an attempt to get at the autonomic nervous system regulating fibers. The possible implications of a finding that the autonomic nervous system-regulating nerve fibers have been damaged system-wide in ME/CFS are staggering.
RECOVER Initiative IS Getting the Goods on ME/CFS

The RECOVER Initiative is getting the goods on ME/CFS.
Lastly, there was (finally) some very good news from the long-COVID RECOVER Initiative. I’ve been regularly blasting the NIH for its inattention to ME/CFS, but it appears that the NIH is actually quite engaged in the ME/CFS long-COVID connection. (It would be nice for them and for us if they would get out of their ivory tower and communicate this stuff to the patient communities they make such a big deal about engaging with.)
It turns out that the NIH is interested enough in other post-infectious diseases that it established a Commonalities Taskforce to explore the links between ME/CFS and other post-viral illnesses and long COVID. Systrom is co-chair of the Exercise subcommittee of that task force and recently gave a talk to the RECOVER Initiative about his invasive exercise findings in ME/CFS and long COVID.
It was a great relief, at least for me, to learn that the NIH’s RECOVER initiative is actually well-informed about the really exciting invasive and other exercise study results. That’s good for long COVID and it’s certainly good for ME/CFS.






Thankyou so much Cort, I am (a person w ME/cfs since 2001) blown away with some hope that i keep in a little corner of my soul. This is so exciting. There’s always a lot I can’t quite absorb.
I will have to re-read this again several times over the next few days. It brought to mind a documentary about ME/CFS that I recently watched.
It was called “The Mysterious Illness that affects millions of people Worldwide”
There were a few interviews with doctors and scientists working in Europe, Germany in particular. One of them had also narrowed down a mitochondrial connection but needed more support. It would be helpful if these scientists could collaborate or share. I know often that is not the case- because of funding and proprietary information issues.
Today, I am hoping we could be on our way to an exit from this awful illness.
It is worth the watch- if you’ve not seen it. this is all forward momentum.
Thankyou so very much to all that endeavor to finish this puzzle.
https://www.youtube.com/watch?v=YH1wn3D9HNg
Thanks for the link, Bethe. I look forward to checking it out. Lots of exciting stuff going on in Germany 🙂
It’s the documentary that initially aired on ARTE featuring Scheibenbogen, Prusty,…
The Youtube version above seems to have overlay of original German language with English dubbing.
A version with only original language (German or French) plus English subtitles can be selected on the websites of ARTE https://www.arte.tv/de/videos/096283-000-A/die-raetselhafte-krankheit-leben-mit-me-cfs/ or German Society for ME/CFS https://www.mecfs.de/dokumentarfilm/ .
Olli Polo in Finland is a pulmonologist with a specialty in sleep medicine who has been treating ME patients and doing research in ME for the past 15-20 years now. But unfortunately his work is not very known because it was very much hindered by the Finnish National Supervisory Authority for Welfare and Health which received complaints from conservative doctors that he was using unproven treatments like LDN and then proceeded to first restrict and then forbid his working as medical practitioner in Finland. He is now continuing his research into the role of compromised structure of the connective tissue in ME in the Bragée clinic in Stockholm. The general atmosphere is much more allowing towards ME research in Sweden than in Finland, which is really at the back end of developing countries in this.
My god – the audacity of Olli Polo – to use LDN in ME/CFS – a drug which did do well in small clinical trials and is commonly used in the US. (What was he thinking?)
I’m sorry that his commitment to his patients well-being caused him so much trouble and I applaud him for that very same commitment.
It’s good to hear that he’s studying the connective tissue in connection with ME/CFS – a subject that needs much more work.
Thanks for letting us know about a Finnish hero. 🙂
I have the fortune of being treated by Dr Olli Polo at Bragée and his treatment (I’m not in the position to explain all of it due to ongoing research) as been very helpful to me and I have high hopes for the future. His theories are VERY interesting and Cort should interview him to spread the word more. Dr Polo on onto something that I haven’t come across in ME nor fibromyalgia and I read a lot of science.
Griffith University in Australia have almost come out to promote it.
Mestinon has been used by Holtorf and Teitelbaum 20 years ago! Many patients can’t tolerate it unfortunately. They also used heparin and LDN and lots of stuff—but the disease persists.
Unfortunately, we’re not at the point where anyone can expect a cure. Instead, I think we’re at the point where some people can expect improved symptoms and quality of life. We just don’t know who those lucky people are.
It’s totally clear from LDN, for instance, that it really helps quite a few people and it really doesn’t do anything in quite a few people. The same, I’m sure is true with Mestinon.
I wasn’t aware (or had forgotten) that Mestinon was used before (and amended the blog to note that). I see that Goldstein really liked it and you report that Teitelbaum and Holtorf both sue it, and we know that Systrom has tried it in hundreds of his patients and that it works enough that he’s continuing to pursue it.
So it clearly helps some people – and that’s about as good as we can get now. I imagine the same thing will be true with this mitochondrial drug if it works out – it will help some people and it will take those people part of the way.
My guess is that we’ll find the right combinations of treatments for the right people and that will either do the trick or take them a long way towards health.
Research out of Australia identified an acquired ion calcium channelopathy in ppl with ME. It appears LDN can be an effective treatment for some ppl with this channelopathy but not for everyone. It depends on what subunit of the TRPM3 receptor is damaged. Perhaps this is part of the reason why only some, and not all, ppl with ME respond favorably to LDN. The Australian research team is hopeful this channelopathy may become a biomarker for ME. Only time will tell.
Thanks, Lori. That’s the biological data and precision medicine-oriented approach that we need for this heterogeneous disease. 🙂
I was the the Astellas study last fall. Thanks for your great reporting and easily understandable explanations. I am really looking forward to the drug being approved (pretty sure I had a placebo).
Thanks Lori, I’ve just listened to an ABC Australia radio interview featuring Professors Sonya Marshall-Gradisnik and Lara Herrero from Griffith University. (Thanks to Tom Kindlon) They’re talking about both Long Covid and ME/CFS. Professor Sonya Marshall-Gradisnik said, ‘… So, we’ve been focusing on specific receptors, like flags that basically sit on the cells and they respond to virus assault. And what we’ve found is those particular flags, that are located on every cell type in the body, are dysfunctional. So, what do they do? Well, they’re supposed to bring calcium inside a cell and we’ve found that that’s impaired. So, in that instance we’ve identified a unique pathology for ME/CFS. But in saying that the frontier of Long Covid, obviously Long Covid is a viral infection, well preceded by a viral infection. We’re looking to see if those receptors are also dysfunctional in Long Covid patients.
https://www.abc.net.au/radio/programs/nightlife/long-covid/13851840
Thanks for this Cort. Will be watching this & tracking with crossed fingers.
Dr. Leonard Jason is on that same Commonalities Taskforce for RECOVER, correct? Hopefully with Dr. Jason & Dr. Systrom’s presence there a lot of connections for the better can be made.
I hope he is. I looked all over in an attempt to find more on the Commonalities Taskforce. The RECOVER website simply states there are 12 taskforces and other committees but does not list them or state who is on them (sigh). Again, for a effort which states its committed to bringing patients into the process it’s all pretty darn opaque.
What a load of rubbish, the mitochondria is being damaged by inflammation caused by the immune system fighting viral infection and also inflammation is the reason people with CFS have cortisol problems.
🙂 I wish I was as sure! Viral persistence in one form or another – as in the virus itself or an altered form or even a piece of it – is certainly an option particularly with EBV and HHV-6 on the ME/CFS side. I think they’re going to really see if that dog hunts with COVID-19. They’re going to really look into it. .
We keep saying time will tell but I hope it really will and not too much time with long COVID. It’s going to be interesting.
I am so pleased to see research into Me/CFS and FM thank you for all your efforts so far and for your explanation of possible links and causes.Also to trialing a new medication that may help in some way with the pain w3 suffer from.
I find this very interesting cause a few years ago now I suffered pulmonary Embolism
S in both of my lungs.No doctor could tell me why this happened to me and I’m on blood thinners for the rest of my life.I know that now I suffer decreased lung capacity and get breathless quite often just even being active for half an hour which I have found very frustrating and limits my ability to actually improve my fitness level.(Post exercise malaise)
I liv3 in New Zealand where it is very hard almost impossible to find a doctor who has researched ME/CFS and FM and is able to have a decen5 conversation and give up to date help.My Doctor won’t even discuss it with me.Other doctors I have seen prescribe Gabapentin which is addictive and has many side effects.
Your research may be too late for me cause I’m nearly 75 now but it gives me some hope for the future.
What are your thoughts on LDN I see it being used quite widely now and wondered what your thoughts would be?
Thank you for all the work you are doing for this illness.
LDN certainly doesn’t help everyone but it really helps some people. It’s also generally pretty cheap. Be sure to start off slow and give it a couple of months. Check out our LDN resource page – https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/low-dose-naltrexone-ldn-fibromyalgia-chronic-fatigue-syndrom/
Dennis, I’d be interested to know about the inflammation causing cortisol problems if you have any links.
Dennis – I’d also be interested in any links you would share that show the association of inflammation, CFS and cortisol issues.
I totally agree with the comments mentioned above. Inflammation in areas of the brain caused by viruses like EBV and other family of the herpes virus and now Corona virus, which is being investigated, are directly responsible for both me/CFS and fibromyalgia. I have my reason to believe that both these condition can be reversed.
How?
100 percent. Working with my neurologist and infectious disease specialist said the problem is immune system is in overdrive causing high cykotines creating all of the symptoms. Trying mestinon and kidney glandular. Definitely post viral problem.
Cautious optimism …..thanks for posting
Viral Infection- Immune response- inflammation causes damage to mitochondrial cells. Causes lower cortisol levels trying to dampen inflammation levels which in turn lower cortisol levels lowers blood pressure and high levels of inflammation also effects deformability of red blood cells and reduced blood flow in micro capillary circulation. Depending on viral load determines how much fatigue and symptoms of CFS one has.
Hi Dennis, your comment is very interesting. Have you found anything that helps your? On our end, nothing helps! Just misery and agony non stop. Thank you
ps, a huge thanks to our dear Cort for doing all this!
I don’t think cortisol is low in all pwME though.
Interesting to see Mestinon mentioned as I’ve been coming across this class of medication in my own research; I have particularly violent symptoms which extend past the ME/CFS norm that point to Acetylcholine depletion. I’ll be asking my doctor tomorrow for the patch variation of this medication (Exelon) which is supposed to be better tolerated.
If Acetylcholine deficiency is common in ME-CFS then the next question becomes why. Working with a friend with a bioengineering background I’ve learned a cortisol deficiency can be the case(indicating adrenal insufficiency.) There’s a direct line of production regulation from cortisol to acetylcholine through serotonin where you’d expect serotonin to be high & the others low.
I’m highly confident this relates to my case as I had all the symptoms of Cushing’s growing up which vanished around the onset of my ME-CFS perhaps hinting at a drastic adrenal failure of some type. Not sure how useful this would be to others as depression is commonly comorbid & I don’t see the wild crashes(serotonin syndrome) from SSRIs I’d expect from anyone with this specific problem.
Good luck!
Thank you so much Cort. I have had ME for 50+ years.
I have thought for many years that ME will eventually be regarded as an ‘umbrella term’ and that in the end a host of individual conditions will be defined each of which will have its own set of treatments. It’s the only thing that makes sense given the many distinct subset symptom profiles seen within ME. The research that you have collated inso much detail above may well go some way to both identifying the subset conditions and treating them.
I think you must be right Jan. We’re about to do a series of recovery stories – the many different ways people recover boggles the mind really.
@Cort, do you say recover as equivalent to cured?
Recovery? Really? Can,t wait to read the stories!
Viral Infection can be in various parts of the body and organs,hence the difference of symptoms and and affects of inflammation. No I don’t know of anything that helps. The immune system is obviously the best way for the body to attack and rid itself of viruses and pathogens but obviously us with CFS have compromised immune system and unable to effectively mount an effective immune response. The other way of getting relief from the virus replicating is antiviral medication but unfortunately there are none approved or can be used safely. Gangciclovir and Valganciclovir are two that had some effect but highly toxic and causes liver damage. Pharmaceutical companies have done very little in the field of antiviral medication since the eighties when the world demanded treatment for HIV -AIDS. Now they have treatments to stop viral replication. It needs the same commitment to help people with CFS. The other new treatments just hitting the market for asthma and other conditions are monoclonal antibodies which helps the immune system fight viruses and pathogens. This surely must be the way ahead for treatment of M/E CFS and Long COVID. It just needs the pharmaceuticals and medical profession to do the right thing.
I believe that in Spain some doctors have prescribed HIV inhibitors to long covid patients with good results. Also blood thinners can improve oxygen uptake and blood flow in long covid patients. I think this will work for some ME/POTS patients too.
Not being able to control certain viruses is part of the disease, but not the whole story. There’s something else that’s causing that. The common denominator.
My guess as a laymen is that its going to be something like that at least for the near future – one treatment to take care of say, the blood vessels, another to boost the mitochondria etc.
Maybe they will find that it’s all autoimmune and that the immune system is messing up the small nerve fibers that control the blood flows and regulate immune functioning – that might be an easier solution – altho I’m not really up on how effective autoimmune treatments are. I do know they’re a lot more effective than they used to be.
Our immune systems are stuck in the on position. This is creating all of the issues, ie. Inflammation. Leftover viral particles possibly is triggering it. Mitochondria is for sure damaged, high histamine is also an overactive immune response.
Cort:
In regards to:
(Systrom stated that he’s continually looking for less invasive ways to get his results and has some ideas on how to achieve that.)
From this:
https://www.washingtonpost.com/health/2022/04/23/long-covid-return-to-running/
By inserting a small catheter in the wrist artery during exercise, Joseph and a team of researchers assessed how much oxygen the body absorbs throughout exercise.
Is this already a move in the the “less invasive” direction?
Nice catch, Lono! I didn’t put much of that in the blog because I wasn’t sure if my notes were correct but it seemed exactly like that – small blood draws taken at the right time – to get the data he needs. That would be huge improvement – and make this really crucial opportunity to see what’s happening in the body, so much more available. Nice!
I wonder whether boosting the mitochondria would help with brain stamina too? I would have thought it would. My brain’s fairly good now but I still can’t sustain longer periods of concentration, particularly when I’m trying to process a wider range of information and especially if I’m tired.
I wasn’t like that before I was unwell. Back then, ideas I would have, would spark more ideas and they’d be ricocheting around my brain, firing off in all directions. I really loved thinking about all sorts of things. Not any more. However, I’m much more focused now, which is a plus.
I also think that study looking at ‘whether exercise triggers a burst of inflammory cytokines’ sounds very interesting.
That study is going to come out soon and the results are going to be quite illuminating I think. The brain is so interesting. Systrom reported that he only gets the results he gets when the participants are upright – so this whole thing of reduced blood flows to the brain appears to be just crucial! Plus Wirth and Scheibenbogen think that both blood flows to the brain and blood flows within the brain are being disturbed.
https://www.healthrising.org/blog/2022/04/18/neuroinflammation-chronic-fatigue-syndrome-hypothesis-wirth-scheibenbogen/
Whatever is happening if the mitochondria in the brain are either not getting the oxygen they need or can’t use it when they get it – that sure sounds like a recipe for mental fatigue and slow information processing to me.
Just a personal note. Nearly my whole life before CFS I had extremely numerous Herpes simplex infections. I took acyclovir when I felt a outbreak coming on. Plus I utilized the ointment as well. The usual triggers would bring it on.
Now in August 2013, I had a severe respiratory viral infection that was the mother of any previous ones. On September 4th 2013 I received a Flu and Shingles vaccinations. In about 10 days or so I lost my ability to walk with autonomic nervous system dysfunction. This is when my SOB, PEM, muscle weakness and other weird stuff began to occur. Looking in the rear view mirror I think I had a RSV infection with post vaccination GBS. Strangely, after this I have not had a single HSV breakout. Literature says virus is always with you and can not be fully eliminated. It’s now been 9+ years I have been herpes free. Either I had a 6 sigma+ style elimination of the virus from my body or my immune system is keeping it tightly under wraps.
I had both the Modurna Covid vaccinations remotely hoping that my immune response might help my CFS. Didn’t happen but it was worth a shot.
All of this being said, I think CFS and HSV have a connection with the initial suspected RSV playing a possible role in the background. During my teen years I had mononucleosis that also brings EBV into play.
I strongly believe that CFS results from a cell danger response post viral immune response. Robert Naviaux’s papers detail the multiple dimensional aspects of his CDR theory in CFS.
Just a strange detail involved in my presentationn and HSV cure?
All dots are valuable. We must connect ever single one!
Agreed – connect every dot. And what an exciting challenge that is for a research who loves big complex puzzles and taking on big things. Thanks for putting some more dots out there 🙂
Did you ever recover from the flu/shingles vaccine?
Hi Roberta, just a suggestion, it would be helpful if you could spell out the abbreviations you are using (such as SOB, RSV, GBS), I am afraid I don’t know many of them. Thank you!
After I received my second Covid vaccination (Moderna), I noticed that the mental fatigue of CFS had diminished. I felt more normal. I have since had a 3rd full dose and a booster of the Moderna vaccine. My general inability to move around much – PEM? – is still with me. But, my quality of life has improved. I haven’t seen it talked about until you referenced it here. I’ve had stress-induced CFS for 6+ years. I was retired and 68 years old when it started, suddenly. The first year was very bad, I spent my days in a recliner. Now I can get more done. But my ability to predict whether I can plan anything longer than a doctor’s appointment is limited. I take it day by day. I am not on any medication specifically for my condition. I am curious if others have improved following Covid vaccinations. What irony…
Is this Connected to thyroid hormones ft3 and rt3?
Many pasients on t4 only treatment experiences lack of oxygen to cells and lactate building when movement of body, and get diagnoser with cfs.
I have no idea but thanks for curling in a longtime important aspect of ME/CFS – thyroid – an important metabolic regulator.
https://www.healthrising.org/blog/2019/03/04/hypothyroid-chronic-fatigue-syndrome-thyroid-ntis/
https://www.healthrising.org/blog/2016/10/24/thyroid-question-fibromyalgia-chronic-fatigue-syndrome-mecfs/
I’ve had CFS since 2006 and encouraged by research into mitochondrial function. Has anyone tried Mitopure and found any improvement? It’s not available here in the UK… I keep nagging them for a date.
I haven’t tried these or used this brand before but someone posted a link to it in a group I’m in. Not cheap!!
https://www.charava.com/products/urolithin-a-500mg
I started using that approximately three weeks ago I cannot tell you whether it does go to good or what Did it help you at all
It seems strange to me that research has suggested blood flow abnormalities including inadequate microvadcular filtration where small fiber abnormalities trigger excessive microvascular constriction and impair oxygen supply to muscles and organs yet somehow he concludes its a mitochondrial problem.
Why would mitochondrial problems be worse on standing? Lack of venous return is a problem with venous compliance or microvadcular leakage not mitochondria.
So often reasonable CFS sciebce occurs in a silo where assumptions are made.
Midodrine enhances venoys return way better than mestinon via two decades of pots treatment.
You have Mitoguard in the UK, not sure if similar. They did help me, but gave me headaches, you cannot win!
Ich habe alles mit höchstem Interesse gelesen und bin froh das man endlich tiefer ME/CFS erforschen will. Auch das es mit Sauerstoffstörung zu den Muskeln zu tun haben könnte. Soweit andere autonome Störungen und Dsyfunktionen. Ich gebe die Hoffnung nicht auf das meine 19j Tochter nach 8 Jahren schwerer Erkrankung an Me/CFS,Pots, Herpes-Viren, EDS. MCAS und MCS wahrscheinlich durch hochgradigen Schimmelpilz Aspergillus Verticolor noch eine Gesundung erleben darf durch Medis und Therapie durch ihre Studien. Vielen Dank eine Mutter mit 57 J. die Hoffnung in die Studien hat. Danke!
Google Translation:
Please do not give up hope for your daughter. It’s impossible to predict the future but the next couple of years are going to be very interesting. Stay tuned. 🙂
I have always felt that there was an oxygen issue, not enough reaching the brain. When I used to fly, I would get a headache immediately as soon as they started to recirculate cabin air. I would be leery of any medication that targets only one neurotransmitter. My experience with Neurontin was terrible, and it seemed to permanently damage the gaba receptors. It is heartening to see serious research going on. The parallels with long-term Covid have to be of help.
This comment is for you Cort. I will try to make a long story short. In late 2002 l had a very severe viral attack .In may 2003 I was suffering symptoms like glandular fever (stiff neck,sore throat, pain on swallowing and not feeling well).Diagnosis was viral sub acute thyroiditis. Obviously I had not cleared the virus. Unfortunately for me I was prescribed prednisone high dose for a number of weeks and on completion was having shortness of breath on exertion which I didn’t have before. The prednisone affected my immune system. In 2004 after repeatedly complaining about shortness of breath was prescribed Symbicort (corticosteroid). One month after starting Symbicort I had another viral attack the same as 2002. Unaware that Symbicort can affect the immune system I kept taking it. I had repeated viral attacks in 2002-2004-2007-2012-twice in 2013 and 2014 . Each episode lasting 8-10 days. Didn’t know what was happening to me and doctors and hospitals no help. All I knew was after each viral attack I became weaker and weaker and deeper into CFS. I am now on pathology tests EBV serology IgM positive on numerous occasions and PCR DNA test EBV DETECTED. I am diagnosed by Infectious Diseases Specialist having Chronic Active EBV. Whether it’s the only active virus I don’t know but I do know EBV plays a major role. All started after taking corticosteroids.
Thanks Dennis. You seem to have a very clearcut case. It seems crazy to me that doctors treat infectious mono/glandular fever with immune suppressing steroids – all in the service of reducing symptoms. I wonder if the medical profession is going to look back at some point and wonder what the heck we were thinking.
The EBV research into ME/CFS began early and has never stopped. I don’t know if you saw but the authors of large study recently rather definitely stated that EBV is a major contributing factor for MS. https://www.bbc.co.uk/news/health-61042598?at_medium=RSS&at_campaign=KARANGA\
A new drug targeting EBV in MS is apparently showing some promise as well – https://www.medicalnewstoday.com/articles/multiple-sclerosis-ms-drug-targeting-epstein-barr-virus-shows-promise#2
Hi,
I just read the part where Dennis wrote:
“I am diagnosed by Infectious Diseases Specialist having Chronic Active EBV. Whether it’s the only active virus I don’t know but I do know EBV plays a major role. All started after taking corticosteroids.”
My CFS started 35 years ago right after I was hospitalized with ITP (platelet disorder, mine were being made ok but destroyed in error). Treatment was steroids for a few months. I have just this minute made a connection in my history. I never (nor did any of the many doctors I saw) made any connection with steroid therapy. In your opinion does this warrant further research? I will obviously discuss with my primary care dr. I also have very recent bloodwork that’s pointing to Multiple Connective Tissue Disease, and waiting for that to get sorted by the doc. Thank you all for your involvement here. It gets lonely when my regular people don’t have any advice!
As time and research goes on it becomes more an more clear that most of the research that identifies pathology associated with ME (and fibromyalgia) is an effect of the loss of tolerance in the disease. Tolerance in the neuro-immune system needs a LOT of work to identify what we are dealing with. Our knowledge of tolerance and modulus, let alone the immune system, is very poor, this is often why many physicians think that deconditioning or cognitive dysfunction is the cause. I asked a GP this question: How much of the immune tolerance system is understood? Answer “not much”. If that is the case why default to psychological explanation?
I think there is quite a lot more that has been investigated and studied on the science side of things. Doctors and medical system seem to be serving other interests and don’t pay attention to the science. Selye was already at work on the effects of stress on the organism in the 30/40s.
[as in hint, if you are interested in reading about this, there is a… whole new world beyond the MDs. Selye one place to start.]
Thanks for your reply Cort , yes what were they thinking interfering with my immune system and starting this terrible chain of CFS. I am now house bound and all years of seeing doctors since 2009 after the third viral in2007 .Doctors would not listen to my concerns in fact in later years with pathology tests results for EBV serology IgM positive and Cardiac Perfusion stress test results showing abnormalities in heart function in 2008 and another performed in 2014 both similar they actively started to cover up and I could get no help from the multitude of specialist doctors including endocrinologist , rheumatologist and I had the feeling they were not telling me the truth all protecting what doctors had done to me. Especially my lung specialist who gave me high dose prednisone in 2013 three times and I had viral infections twice that year and got worse CFS. Yes Cort I have seen the articles you referred to thanks. I have also seen a article on a antiviral called Tenofovir which is used for HIV and Hepatitis B infection and is going to be trailed in the US for Multiple Sclerosis also says is highly effective in vitro on EBV and has a good safety profile . Would appreciate any input into Tenofovir.
Hi, I am following this dialogue between you & Cort. I just happened upon this page today, having had a resurgence of my symptoms recently. I’ve had CFS for 35 years, not as active as your troubles but still pretty debilitating. Your story about the steroids just floored me because my symptoms started immediately after treatment with steroids (for a few months to save me from ITP (autoimmune bleeding disorder). I knew when it all started but never made a connection with steroids. I will be investigating this now. Thanks for mentioning this. And good luck to all of us!
Mestinon has truly been a lifesaver for me. I was bed bound in the dark for a decade with a disability level below 5%. After four years using Mestinon I’m now about 40% and feel like I have my life back. The clue for me was to increase the dosage continuously, not stop with the «standard» doses used in ME/CFS, they were too low for me. I’m now on dosages in the Myasthenia gravis range – really high dosages. Don’t be afraid to up your dosage if Mestinon is right for you but seems to taper off. Best regards.
Interesting study, fingers crossed. Quite a few indications that the mitochondria are an issue, but I guess the big question is how central are they to the illness, or are they peripheral?
Dennis and Cort, the second article you sent about about MS and EBV had a link to another article about immunotherapy being trialed for the two and had this statement, In this latest study, he and his colleagues tested a new treatment that boosts the ability of CD8 T cells in the immune system to fight against EBV. They believe the approach, called adoptive immunotherapy, could potentially treat MS and other chronic autoimmune diseases.
Cort, where is someone going to be trialing this and the other treatments for us? And here is another article I just found about Herpes virus and EBV could be tackled by heart drug: https://www.medicalnewstoday.com/articles/307852
This was very timely for me to read. I’m going in for one of Systrom’s iCPET tests tomorrow and it is very intimidating. He put me on mestinon (off it for the test right now) and it seemed to help my baseline pain and functionality levels. Unfortunately mestinon comes with its own side effects and I felt strange whenever it was wearing off, heart palpitations etc. And it seemed to make my peripheral neuropathy behave worse and that scares me but that might be a timing coincidence. It only lasts a few hours and then I have to take it again or go to sleep. Life without it hurts a lot more but I wish there was some way to feel better that wasn’t constantly swinging around. Beggars and choosers I guess. Currently depending on mestinon to maybe let me keep my job 😣
Thanks for relaying your experience, Leona. 🙂
My thoughts are … for sure we do have mitochondrial dysfunction. But I believe the dysfunction first starts in a pathway outside the cell, probably caused by a virus or the Sympathetic Nervous System on overdrive. Both can cause cytokines and autoantibodies to be released; but when gone untreated, they act as a trigger in developing mitochondrial dysfunction thus resulting in ME.
That’s why I’m hoping for more research in areas that study the pathways that are outside the cell. If they find those pathways and are able to stop them, I believe we will not have mitochondrial dysfunction occurring.
I am always troubled when I hear of patients being prescribed pyridostigmine (Mestinon).
Our organization has worked with Gulf War families for many years.
This is why pyridostigmine was used in the first Gulf War.
Pyridostigmine bromide (PB)
Anti-nerve agent pill used during the Gulf War as a pretreatment to protect military personnel from death in an attack with the nerve agent soman. Supplied in the Gulf War as 21-tablet blister pack, with prescribed dosage as one 30-mg tablet every 8 hours.
There have been concerns that PB was one of the triggers for Gulf War Illnesses based on genetic differences in the ability to metabolize PB in some exposed veterans.
Gulf War Illness and ME/CFS have many similarities.
True statement!! As a Gulf War Vet, I can say that I am the exception to the rule. I had gulf war syndrome symptoms long before the gulf war. When I got my work up in 2019, at Mass Gen Brigham, the new Neuromuscular Division on Fenwood Drive, they put me on Pyridostigmine after my EMGs and SFN biopsy. I thought the MESTINON, (Pyridostigmine) was not working until I tried to get off it. What a wake-up call. This drug keeps me from being non-ambulatory and walking without mitigating equipment. The Double-Edged sword was that you get leakage from the drug, i.e. as in Olestra Potato chips, (heed every warning to urinate and never trust that you are passing gas). For me, it works. The drug most likely has adverse effects on healthy individuals.
I heard that before, but something does not add up. Pyridostigmine is a FDA approved drug used for decades by Myasthenia Gravis patients without turning them into GWI-like patients. Despite some transitory side effects, it is pretty well tolerated. Even for ME/CFS patients, we’ve had several years of experience with this drug. Besides, recently UTSW confirmed that GWI is actually caused by Sarin (https://www.utsouthwestern.edu/newsroom/articles/year-2022/sarin-nerve-gas-gulf-war-illness.html), and it affected soldiers with a certain defect in gene PON1.
Strange that we never heard about PON1 from Dr. Klimas, who was supposedly being paid to study it for decades. I think she just caused more confusion than helped.
To Gijs I didn’t see your comment on long Covid patients in Spain being treated with HIV antiviral medication with good results. My previous comment on Tenofovir antiviral is also one of the antiviral medications used for HIV. Does anyone know more about treatment with HIV antiviral medication or can you Gijs add any more to what know.
Has anyone taken Cardarine? It’s a potent PPAR delta agonist abused in bodybuilding.
This should have similar effect as the Japanese new drug but higher toxicity
https://en.m.wikipedia.org/wiki/GW501516
Cort – What’s the latest on this study? Did it get shut down?
Yes it did.
Thanks Cort. Bummer.
I just looked into the Astellas trials & from what I see it was terminated? Am I reading this correctly?
Recruitment Status : Terminated (Lack of Pharmacological effect)
First Posted : April 22, 2021
Last Update Posted : January 25, 2023
I’m afraid so. Systrom should get some good data from it, though – which may hold some clues to ME/CFS.
https://www.healthrising.org/blog/2022/12/07/systrom-chronic-fatigue-syndrome-mitochondria-drug/