

“Consider that larger clinical trials are often meant to confirm something important to change our practice. The small trials are the ones making conceptual breakthroughs that change our thinking.” Aaron Cypess, M.D., Ph.D., M.M.Sc., National Institute of Diabetes and Digestive and Kidney Diseases NIH.

The early long COVID treatment trials aren’t going to turn the world on its head but do provide some potentially helpful options.
The early treatment trials for long COVID look very much like early trials of anything: they tend to be small, not very rigorous and can be sketchy statistically. Case reports are common. Quite a few came from the alternative health field.
Except for a couple of surprises, many will be familiar to anyone who’s kept a close eye on the chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) fields, which appear to be having quite an impact.
The early trials may provide informed patients and doctors though, with new options and lay the groundwork for bigger, better conceived, and ultimately, more useful clinical trials.
Those trials are coming – and rapidly. Suzanne Vernon Ph.D. – scientific advisor to the Bateman Horne Clinic – reported that a short list of clinical trials the RECOVER Initiative will investigate has been created (she wouldn’t say what they were). These trials will probably be fairly small, but they will undoubtedly be rigorous, and most importantly, if successful, they will undoubtedly receive follow-up. Vernon believes we will likely get new treatment options before we know exactly what’s happening in long COVID. (Interview coming up).
This overview assesses the already published clinical trials for long COVID with an eye to the future – in particular, whether the NIH’s RECOVER Initiative will fund further trials. It’s impossible to tell at this point, of course, how receptive the ultraconservative NIH will be to alternative or unusual attempts to treat long COVID, but one imagines it will have to let its hair down a bit as it plunges ahead with treatment trials without knowing what’s going on in long COVID.
My totally uninformed guess is that it’s going to continue its conservative ways but that some unusual approaches could sneak through. Hopefully, the first treatment on the list will be one of them.
As Expected – Low Dose Naltrexone Makes a Difference
Is the NIH finally ready to fund a trial of a drug that’s a) been shown to help fibromyalgia, b) is commonly used in ME/CFS, and c) won’t get funding from the drug companies – meaning you’re pretty much it NIH!
Study – Safety and efficacy of low dose naltrexone in a long covid cohort; an interventional pre-post study
Drug – Low Dose Naltrexone
Type of study – interventional pre-post study
Size – 36 long term patients (mean – @ 1 year)
Dose – 1 mg once daily for one month; the dose was increased by 1 mg monthly to a maximum of 3 mg
Length – 2 months
Endpoints – questionnaires
Results – 6/7 parameters showed improvement (recovery from COVID-19, limitation in activities of daily living, energy levels, pain levels, levels of concentration and sleep disturbance (p ≤ 0.001); the biggest effect was in pain; low side-effects were found: 36/38 participants finished the trial.
Authors’ conclusion: “LDN is safe in patients with PCS and may improve well-being and reduce symptomatology in this cohort. Randomized control trials are needed to further explore this.”
ME/CFS/FM connection – a commonly used drug in ME/CFS/FM, not surprisingly, does well in long COVID, particularly with pain. The fibromyalgia LDN trials have been successful, but were all quite small.
Bottom Line – Definitely a winner. LDN – a compounded drug that drug companies will not support – desperately needs federal support. The question is will the NIH finally give it? After several failed efforts to get funding, Jarred Younger concluded that the NIH will never fund an LDN trial.
I would be surprised, though, if LDN wasn’t on the short list of early clinical trials of the NIH’s RECOVER Initiative given the ME/CFS experts that have been consulted. Will that be enough for the LDN-averse and ultraconservative NIH to finally launch a trial? Time will tell.
Health Rising has done many blogs on LDN. Learn more about LDN
Getting Etanercept DEEP into the Brain
Injecting etanercept into the cerebral spinal fluid produced excellent results – suggesting that neuroinflammation is a thing in long COVID.
Study – Rapid improvement in severe long COVID following perispinal etanercept
Drug – Etanercept – is a biologic that is capable of ameliorating two components of neuroinflammation: microglial activation and tumor necrosis factor (TNF-a) activity. Perispinal injection of the drug – which involves injecting the drug into the cerebral spinal fluid – has been called “a new therapeutic paradigm in neurology.” The idea is that stopping TNF-A stops a vicious circle from forming.
Type of study – case report
Size – 1
Dose – 25 mg perispinal application
Length – 24 hours and 1 month later
Endpoints – Montreal Cognitive Assessment, Beck Depression Index-II (BDI-II), Fatigue Assessment Scale, Controlled Oral Word Association Test, Trail Making Tests, Timed Finger-to-Nose Test, 20 m Self-Paced Walk Test, 5 Times Sit-to-Stand Test, and Grip Strength.
Results – a dramatic improvement in 24 hours: remarkable reductions in chronic post-COVID-19 fatigue and depression, and significant measurable improvements in cognition, executive function, phonemic verbal fluency, balance, gait, upper limb coordination, and grip strength. Cognition, depression, and fatigue were examined at 29 days; each remained substantially improved.
Authors’ conclusion – “Perispinal etanercept is a promising treatment for the chronic neurologic dysfunction that may persist after resolution of acute COVID-19, including chronic cognitive dysfunction, fatigue, and depression. These results suggest that long COVID brain neuroinflammation is a potentially reversible pathology and viable treatment target. In view of the increasing unmet medical need, clinical trials of perispinal etanercept for long COVID are urgently necessary.”
ME/CFS/FM connection – a fascinating case report given that Dr. Klimas’s modeling efforts suggested etanercept should be used to bring down neuroinflammation first in ME/CFS, followed by mifepristone to reset the HPA axis. That combination is currently being trialed in Gulf War Illness and ME/CFS.
Bottom line – Very small study – big winner, given the in-depth analysis. Much larger studies are obviously needed but what a nice potential linkup with the neuroinflammation idea for both long COVID and ME/CFS. Etanercept seems like a long shot, but if Nancy Klimas – who is apparently on RECOVER panels – has some good data to share with the NIH, we might just see a trial…
Will Vagus Nerve Stimulation Finally Get the Big Trial it Needs? (Probably not)
If any treatment needs large, well-organized trails its VNS. Will the NIH bite? (from Manu5 Wikimedia Commons)
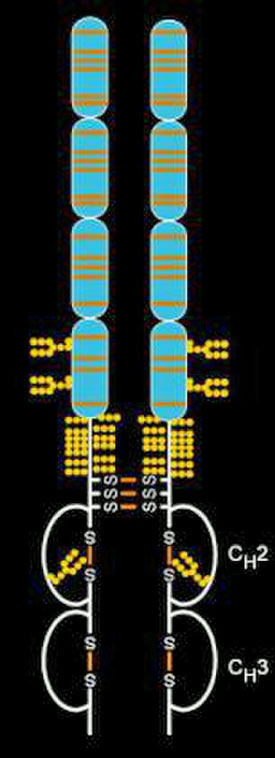
Drug – Vagus nerve stimulation
Type of study – randomized, sham-controlled, trial
Size – 13
Dose – two one-hour sessions/ day delivered at “suprathreshold intensities”
Length – 4 weeks
Endpoints – the study was designed to treat the following symptoms: anxiety, depression, vertigo, anosmia, ageusia, headaches, fatigue, irritability, brain fog
Results – the trends in the data suggest taVNS may have a mild to moderate effect in reducing mental fatigue symptoms in a subset of individuals.
Authors’ conclusion – “This innovative study demonstrates the safety and feasibility of supervised self-administered taVNS under a fully contactless protocol”. (The study was done without anyone stepping into a clinic.)
ME/CFS/FM connection – VNS stimulates the vagus nerve, which is believed to be underactive in ME/CFS. Anything that could tamp down the ferocious sympathetic nervous system response that appears to be present would be helpful, and Lauren Stiles is very hopeful about its chances with postural orthostatic tachycardia syndrome (POTS). It just needs a lot more study.
Bottom Line – In-betweener. The results were not that promising, but the VNS field is like the Wild West – no one knows what doses and durations work best. If anything needs large, placebo-controlled studies, VNS does. Will the NIH step up? It’s taking a deep look at VNS in its SPARC program, but my guess is no.
Is it Too Early for the Best Mitochondrial Enhancer for ME/CFS (and long COVID) to Get Federal Support?
Supplement – Oxaloacetate
Type of study – non-randomized clinical trial
Size – 76
Dose – 500 mg BID (N = 23), 1,000 mg BID (N = 29) and 1000 mg TID (N = 24) AEO for six weeks.
Length – 6 weeks
Endpoints – Chalder fatigue scale
Results – 25% – 33% reduction in fatigue
Authors’ conclusion – “As there has been little progress in providing fatigue relief for the millions of ME/CFS and Long COVID patients, anhydrous enol oxaloacetate may bridge this important medical need.”
ME/CFS/FM connection – trial conceived by an ME/CFS doctor (Kaufman) after he dug into a metabolomic study result.
Bottom Line – A winner with a lot of questions. Will pretty good study size (n=76) and results pave the way for a larger (randomized, placebo-controlled) study? Also – can oxo move the needle on other fatigue scales? And the big question – will the price of oxaloacetate (@$500/month) ever come down? (Dr. Kaufman thinks it might.) My guess is that oxaloacetate may be a bridge too far for the NIH, but time will tell.
Fixing Reddened Throats to Impact the Central Nervous System?
Study – Epipharyngeal Abrasive Therapy (EAT) Has Potential as a Novel Method for Long COVID Treatment
Treatment – Epipharyngeal Abrasive Therapy (EAT) – the application of zinc chloride as an anti-inflammatory agent to the epipharyngeal mucosa.
Chronic epipharyngitis refers to inflammation at the back of the throat which, if memory serves, Dr. Cheney – an astute diagnostician – reported was very common in ME/CFS. This is how a Japanese paper described its possible relevance to ME/CFS:
“However, because of its close link with the nervous system and both the innate and acquired immune systems, it may play an important role as a trigger for the development of neuroendocrine disorders, including chronic fatigue syndrome and other somatic symptoms. Thus, the “epipharynx-brain interaction” is worth consideration in managing patients with chronic fatigue syndrome.”
Type of study – intervention
Size – 58
Dose – A 0.5% ZnCl2 solution was applied to the epipharyngeal mucosa once a week using a sterile straight nasal cotton swab and a pharyngeal swab. To increase the effectiveness of EAT, it is important to thoroughly scrub the epipharyngeal wall with cotton swabs.
Length – 1 month
Endpoints – intensities of fatigue, headache, and attention disorder
Results – EAT significantly improved the intensity of fatigue, headache, and attention disorder.
Authors’ conclusion – “These results suggest that EAT has potential as a novel method for long COVID treatment.”
ME/CFS/FM connection – a possible treatment for a long ignored symptom that the authors believe could impact central nervous system functioning.
Bottom Line – Unusual treatment produces a good result. Not a snowball’s chance in hell that the NIH will pick this up, but doctors might give it a shot. Is it available in the U.S.?
In-depth Case Report Builds Strong Case for Plasmapheresis

Plasmapheresis machine – it was only a case report but it was a good one. (Image from RexxS – Wikimedia Commons)
Study – Case Report: Therapeutic and immunomodulatory effects of plasmapheresis in long-haul COVID
Drug – plasmapheresis
Type of study – case report
Size – 1
Dose – 3 TPEs
Length – 2 months
Results – a formerly healthy 68-year-old man who was very weak, unable to walk, experienced shortness of breath, and had lung issues was able after 2nd transfusion to walk uphill with ease and jog. His brain fog disappeared, and he returned to daily work activities. After the 3rd transfusion two months later, he was back to work, feeling like his normal self, and able to exercise daily without shortness of breath.
The infusions also “increased the markers of T-cells, B-cells, NK cells, and diminished the markers of inflammatory macrophages, suggesting enhanced adaptive immunity and attenuated inflammatory response. Proteomics also revealed a striking reduction in inflammatory markers.
Authors’ conclusion – “this case study suggests that TPE may alleviate post-COVID-19 sequelae via positive shifts toward adaptive immunity and tissue repair that are concurrent with reduction of inflammation.”
ME/CFS/FM connection – no studies have been done in ME/CFS/FM. In his FM study, which found that antibodies from FM patients were able to replicate an FM-like state in mice, Goebel suggested proposed trying plasmapheresis or immunoadsorption in FM. Scheibenbogen has found some success in small studies with immunoadsorption in ME/CFS, and the BC 007 aptamer is a candidate for both ME/CFS and long COVID.
Bottom line – The dramatic results from this very in-depth case report are intriguing given suggestions that a similar approach may work in ME/CFS/FM. Could the NIH spring for a small trial? Perhaps…
English National Opera (ENO) Breathe programme fails to hit the high notes
Treatment – English National Opera (ENO) Breathe programme or usual care
Type of study – parallel-group, single-blind, randomised controlled trial
Size – 150 long COVID patients experiencing breathlessness
Endpoints – Health Related Quality of Life (HRQoL) using mental health composite (MHC) and physical health composite (PHC) scores, as well as the chronic obstructive pulmonary disease assessment test score, visual analog scales (VAS) for breathlessness, and scores on the dyspnoea-12, the generalized anxiety disorder 7-item scale, and the short form-6D.
Results – Mental health but not physical health scores improved, as did the VAS for breathlessness
Author’s conclusion – “Our findings suggest that an online breathing and wellbeing program can improve the mental component of HRQoL and elements of breathlessness in people with persisting symptoms after COVID-19. “
ME/CFS/FM connection – some people with ME/CFS experience breathlessness
Bottom Line – they tried! The most rigorous clinical trial yet, though produced an underwhelming result.
Mast Cell and Microglial Inhibiting Medical Food Makes Its Case
Supplement – Ultramicronized Palmitoylethanolamide and Luteolin Supplement (PEA-LUT 770 mg.) PEA – which has undergone numerous trials in Europe – has been held up as a case study of how the research community can ignore effective treatments it does not understand. It primarily has been used in Europe (the current study was from an Italian group) but has been making its way to the U.S. more recently. Jarred Younger included PEA in his list of potential microglial inhibitors that might be of use in ME/CFS and FM. Studies suggest PEA can reduce mast cell migration and degranulation and can shift them from their activated to their resting states. Hesselink reports that over twenty studies have elucidated PEA’s mast-cell inhibiting effects. A retrospective study found that PEA may be helpful as an add on treatment in FM.
Type of study – Multi-Center Double-Blinded Randomized Placebo-Controlled Clinical Trial
Size – 185 long COVID patients with olfactory impairment
Dose – 770 mg
Length – 90 days
Endpoints – Improvement in the ability to smell
Results – Overall, 92% of patients in the intervention group improved their olfactory scores versus 42% of controls.
Authors’ conclusion – “Among individuals with olfactory dysfunction post-COVID-19, combining PEA-LUT with olfactory training resulted in greater recovery of smell than olfactory training alone.”
ME/CFS/FM connection – PEA has been suggested for both FM and ME/CFS.
Bottom line – PEA’s ability to better improve olfactory scores than with olfactory training alone suggests PEA may be having an impact on neuroinflammation. Two studies have found PEA improved results when used as an adjunct treatment – but why the focus on adjunct treatments? PEA gets a lot of support in Europe, but I would be shocked if the NIH picked this treatment up. Find out more about PEA – what it may do and how to take it.
Perrin Technique Reduces Fatigue in long COVID
Treatment – Lymphatic drainage – Perrin technique
Type of study – Case series – first 20 long COVID patients
Size – 20
Dose – 9-10 sessions
Endpoints – symptom severity using the self-report 54-item profile of fatigue-related states (PFRS) before and after treatment.
Results – 45% and 52% improvements in men and women in fatigue-related scores with the highest reductions for fatigue subscale
Authors’ conclusion – “Our findings suggest that a specific manual lymphatic drainage intervention may help to reduce fatigue symptoms related to Long COVID. “
ME/CFS/FM connection – The Perrin lymphatic drainage technique was developed for ME/CFS.
Bottom Line – Potential winner. While no placebo controls were included, the results were promising. Hopefully, the emergence of long COVID will spur interest in this novel technique designed to restore lymphatic flows from the brain to the body, thus removing toxins in the brain. RECOVER Initiative funding chances are probably very low, unfortunately. Find out more about the Perrin technique
Not Adaptive Enough
Supplements – Chisan®/ADAPT-232 (a fixed combination of adaptogens Rhodiola, Eleutherococcus, and Schisandra)
Type of study – randomized, quadruple-blind, placebo-controlled trial
Size – 100
Length – 2 weeks
Endpoints – reduction in symptoms
Results – Chisan® decreased the duration of fatigue and pain for one and two days, respectively, in 50% of patients. Plus, significant differences between placebo and Chisan® treatment were observed only with a workout (daily walk time) and in relieving respiratory insufficiency (cough). No significant improvements were made in markers of blood coagulation or inflammation, but blood creatinine was lower.
Authors’ conclusion – “we, for the first time, demonstrate that adaptogens can increase physical performance in Long COVID and reduce the duration of fatigue and chronic pain. It also suggests that Chisan®/ADAPT-232 might be useful for preventing the progression of renal failure associated with increasing creatinine.”
ME/CFS/FM connection – adaptogens have been suggested for ME/CFS.
Bottom line – Loser. This was a serious study, but the results were middling at best. The buck probably stops with this study.
Gut Enhancement
Supplement – a high-fiber formula with investigational new drug (IND) status; this is the type of product that’s typically used to increase butyrate levels and butyrate-producing bacteria.
Type of study – case report
Size – 1
Length – 2 months
Results – Severe “loss of appetite,” palpitation, and anxiety were significantly improved as were serum lipid profile, insulin level, and leptin level.
Authors’ conclusion – “Our study indicates the feasibility of alleviating gastrointestinal symptoms in patients with post-acute COVID-19 syndrome by way of nutritional modulation of their gut microbiota. ”
ME/CFS/FM connection – Low butyrate levels have been found several times in ME/CFS and could be tied to leaky gut and inflammation.
Bottom Line – In betweener. This case report helps to validate what we already know in ME/CFS – that butyrate enhancement could be helpful – but it was hard to understand from the abstract.
Call me naïve, but given the gut problems found in long COVID, and the increasing recognition of the role the gut plays in many diseases, I wouldn’t be surprised if a gut microbiome enhancement trial doesn’t make the cut in the RECOVER Initiative.
Breathing Deep Again…An Inspiratory Muscle Training Trial
Study – Inspiratory Muscle Training Enhances Recovery Post COVID-19: A Randomised Controlled Trial
Treatment – inspiratory muscle training; i.e. breathing training using a device
Type of study – randomized control; inspiratory training vs usual care
Size – 281
Length – 8 weeks
Endpoints – Health-related quality of life and breathlessness questionnaires (King’s Brief Interstitial Lung Disease (KBILD) and Transition Dyspnoea Index (TDI)), respiratory muscle strength and fitness (Chester Step Test).
Results – no difference in KBILD total score but significant and clinically meaningful improvements in breathlessness and significantly improved (but clinically meaningful?) respiratory muscle strength and estimated aerobic fitness.
Authors’ conclusion – “IMT may represent an important home-based rehabilitation strategy for wider implementation as part of COVID-19 rehabilitative strategies.” (Another case report found that 2 months of respiratory muscle training plus cardiopulmonary rehabilitation resulted in improved dyspnea, physical performance, and pulmonary function parameters and that activities of daily living rapidly improved.)
ME/CFS/FM connection – inspiratory muscle training in ME/CFS and long COVID underway now.
Bottom Line – In-betweener – the results were good but not great. (Did not meet its primary goal – total KBLID score). Still, inspiratory muscle training is cheap, readily available, can be done at home, and does not require a prescription. What’s not to try? Given its long history of effectiveness in other diseases and the lung connection in COVID, I could see the RECOVER Initiative funding a trial.
Hyperbaric oxygen treatment increases blood flows to the brain, exercise capacity, and cognition
Two Studies – Hyperbaric oxygen treatment for long coronavirus disease-19: a case report / Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention /
Treatment – hyperbaric oxygen
Type of studies – case report/intervention
Sizes – 1 / 10
Doses – 90 minutes of 100% oxygen at 2-atmosphere absolute pressure with 5-minute air breaks every 20 minutes – 5 days per week
Lengths – 60 sessions / 10 x 105-minute sessions of HBOT to 2.4 atmospheres over 12 days.
Results – Case Report – significant improvements in brain perfusion and microstructure, increased cerebral blood flow, 34% increase in the maximum rate of oxygen consumed during exercise, and a 44% improvement in forced vital capacity. Significant improvement in memory including nonverbal memory, executive functions, attention, information procession speed, cognitive flexibility, and multitasking.
Results – 10 session study – statistically significant improvement in the Chalder fatigue scale (p=0.0059; d=1.75 (very large)), global cognition (p=0.0137; d=-1.07 (large)), executive function (p=0.0039; d=-1.06 (large)), attention (p=0.0020; d=-1.2 (very large)), information processing (p=0.0059; d=-1.25 (very large)) and verbal function (p=0.0098; d=-0.92 (large)).
Authors’ conclusion (case report) – “We report the first case of successfully treated long COVID symptoms with hyperbaric oxygen therapy with improvements in cognition and cardiopulmonary function. The beneficial effects of hyperbaric oxygen shed additional light on the pathophysiology of long COVID. “
Authors’ conclusion (10-session study) – “The results presented here suggest potential benefits of HBOT, with statistically significant results following 10 sessions.”
ME/CFS/FM connection – several studies suggest hyperbaric oxygen treatment can help in FM.
Bottom Line – Winner. The case report was notable for its in-depth assessment of brain perfusion, cerebral blood flows, and oxygen consumption during exercise – just the things we’d hoped hyperbaric oxygen treatment would help. The 10-session study found improvements in fatigue and many cognitive assessments including information processing – which studies consistently show is impaired in ME/CFS.
So far so good. The big question is – will the improvements last and what is the optimum number of sessions needed to produce the most efficient results? We need big, well-designed studies to answer those questions. Will the NIH support a kind of new-agey treatment that nevertheless seems to get good results? I would be shocked if it did but hope it will.
Ozone Therapy
Drug – Ozone therapy – According to one site, “ozone therapy is a procedure in which a pint to a quart of blood is drawn into a closed sterile glass device specifically made for this therapy. Medical grade ozone is added directly to the blood before being returned to the body in a 30-minute reinfusion process…(It) delivers potent extracellular and intracellular cleansing and detoxing power of ozone directly into your bloodstream, eradicating on contact all pathogens, bacteria, viruses, mold, fungi and yeast, while oxygenating and feeding your cells for a rapid and drastic improvement of your health and well-being.”
Type of study – ?
Size – 100
Dose – ?
Length – ?
Endpoints – 7-scoring Fatigue Severity Scale (FSS)
Results – reduced fatigue by 67%; 40% reportedly completely recovered
Authors’ conclusion – “Ozone therapy is able to recover normal functionality and to relief pain and discomfort in the form of PASC-associated fatigue in at least 67% of patients suffering from post-COVID sequelae, aside from sex and age distribution.”
ME/CFS/FM connection – Ozone therapy purports to oxygenate cells
Bottom Line – Inbetweener. Rudimentary statistics from an Italian study suggest that ozone therapy may be helpful with fatigue but who really can trust the stats (and an abstract written like that)? Much better studies are needed. Chance of the RECOVER Initiative taking this up? Zero.
Taming the Sympathetic Nervous System with a Shot to the Neck?
Study – Stellate ganglion block reduces symptoms of Long COVID: A case series
Treatment – stellate ganglion block with anesthesia could allow the regional autonomic nervous system to “reboot” , decreasing sympathetic nervous system activity, improving blood flows, etc. – thus fixing or rehabilitating a key system in ME/CFS, FM, and probably long COVID.
Type of study – case series
Size – 2
Dose – 2
Results – two quite severe long-COVID patients return to work after a couple of treatments. (Also another case report found SBG plus injections in other parts of the spine reportedly led to complete recovery of a long-COVID patient.)
Authors conclusion – “The stellate ganglion block has been used for nearly a century to treat a variety of sympathetically mediated medical conditions. Its safety profile is well established. Its application in treating Long COVID/PASC is novel but promising. The lack of effective treatments for Long COVID/PASC makes the SGB an attractive therapeutic modality that deserves further investigation.”
ME/CFS/FM connection – reportedly has worked in a few ME/CFS patients as well – could impact key processes in ME/CFS and FM.
Bottom Line – Winner. Couldn’t have said it better: “The lack of effective treatments for Long COVID/PASC makes the SGB an attractive therapeutic modality that deserves further investigation.” The RECOVER Initiative almost certainly won’t take this up, but others hopefully will.






This is a great article Cort. Thanks for putting it together. There hasn’t been much that has left me feeling truly optimistic over these past few years, but this collection of findings definitely does.
Good to hear, Micheal. Truly the best is yet to come. Suzanne Vernon described the RECOVER Initiative as a “Thing of beauty””. Boy was that good to hear after all the upset over its slow start. Coming up – a blog on the long COVID treatment trials underway now.
Thanks for the diligence Cort
Thank you for compiling this. Is it possible to add to the above list who is doing each of the studies? Listing the research team or linking to a list of the investigators? Thx!
It’s certainly possible but I’m exhausted. However, if you click on the link to the study you can often get email addresses in the affiliations section just below the authors name. Sometimes you need to be able to access the actual study but not always – and many of these studies were open access.
Thanks Cort. Great article.
This year I’ve had a crack at:
1. C4/C6 Sympathetic Nerve Chain block (the one used for PTSD rather than a SGB).
2. PEA
3. Vagus Nerve Stimulator
Something in that mix has helped, but no cure for me. I’m not sure what has worked though. The cause and effect is too complicated. I’m not on anything else.
Plasmapheresis is indeed intriguing. I’m actually a little gob smacked that this has never been tried previously in ME/CFS given Ron Davis’s results with the nanoneedle (i.e. something in the blood plasma is causing grief). Given the potential for spontaneous remission in the single PCS patient over the same timeframe, this obviously needs follow up. Surely this is not that difficult or expensive to do for either PCS or ME/CFS?
And wouldn’t the healthy control group just be able to be selected from folks who already donate blood plasma, or have I completely just missed the point?
This all reminds me of people with hemochromatosis controlling their condition through exactly the same process as blood donation (they just chuck it in the bin though I guess).
Hello the small brother of plasmapheresis which is called immunadsorption has been testet by mecfs patients in berlin Prof. Scheibenbogen with success some years ago. Now there are smaller studies in some german universties planed for long covid. But its very expensive and invasiv. And its imposiible to get a doplle blind control group.
One of your best articles, Cort. Well done!
Thanks for the great info Cort. I’m especially intrigued by the red throat theory. My son and I both have issues with our throats, including the redness. I wish I could get my hands on some zinc chloride to experiment a little.
Wow. Thanks, Robert!
Can’t you? You can just buy it online. That’s what I’m gonna do. I have constant red throat so I’m also intrigued.
I have been receiving Ayervedic treatment & am feeling much better
Ha! I have an interview coming up with an Auryvedic practitioner with ME/CFS coming up. It’s fascinating stuff! Glad to hear it.
Excellent article, Cort. Thank you.
Have you seen this very recent by Profs Doug Kell and Resia Pretorius on the potential role of ischaemia-reperfusion injury in chronic diseases such as ME/CFS, Long Covid and Rheumatoid Arthritis?
https://portlandpress.com/biochemj/article/479/16/1653/231696/The-potential-role-of-ischaemia-reperfusion-injury
This provides a possible explanation for ME/CFS and Long Covid, and importantly, the authors recognise the long wait for large-scale treatment trials while people are in need of urgent treatments, so they have discussed possible treatments that are more readily available.
Thanks Di! Looking forward to checking it out – particularly the possible available treatment options 🙂
Hello whatsup with BC007 from BerlinCures? The university of Erlangen healt 4 of 4 long covid hauler and 1 of 1 mecfs patient with this heart medication which get on the spike and some auto antibodies. In my opinion tje most hopeful medication for us.
I hope that they do some experiments with ME patients using the plasmapheresis soon. It seems to have such dramatic results. Surely it is worth trying. Were the people in Germany going to try it? Things certainly seem to be moving in a good direction now, at least it gives us a little bit of hope for the future.
The biggest hope on the horizon for me is BC007!
My husband was badly hit by Long Covid (fatigue, post exertional malaise, heart problems….), unable to work and partly bedbound.
After a few months he got Immunadsorption (plasmaapheresis) at a University Clinic in Germany ( we are german).
Within 2 weeks he was symptomfree (!), one can say healed. He even did sports and was fine. Unfortunately after 2 and a half months he got a relapse. Fortunately he’s not as bad as he was before. We think that the autoantibodies might be back. Doctors say for some persons autoantibodies can come back after a while.
BC007 is an aptamers that binds the autoantibodies on a chemical way. So it’s basically the same as plasmaapheresis but it works even more exact. I’m sure my husband would be healed with that drug, even if he would have to take a dose every few months!
There were 4 healing attempts on Long Covid patients. 3 out of 4 were healed and symptomfree within days and weeks and they are stable up to now! The fourth person has some symptoms remained but also impressive improvement.
As far as I know there is NO other drug that could achieve the same.
Unfortunately BC007 is widely underestimated and underfinanced! The company (Berlin Cures) is a small start up, still trying to find investors or funding by the german government for their stage 2 trial (30 Million Euro).
A lot of german Long Haulers try to push BC007 into public, to speed the process.
I know this is the drug my husband needs since he got symptomfree with plasmaapheresis (immunoadsorption).
you know the name at bc007
Merci à toi Cort, tu nous redonnes de l’espoir. C’est un travail remarquable que tu as effectué. Repose toi bien.
Merci beaucoup pour vos aimables paroles, Claudine.
Thanks Cort for a very informative article. Now go and have a good rest!
Indeed! 🙂
Great snapshot Cort. I find it useful to see what they say about individual papers on s4me too, as some members have a very critical eye that can get me thinking (and helps me acknowledge my own ignorance)!
for example, here’s comments on perispinal etanercept
https://www.s4me.info/threads/rapid-improvement-in-severe-long-covid-following-perispinal-etanercept-2022-tobinick-et-al.28460/#post-427431
here’s comments on epipharyngeal abrasive
https://www.s4me.info/threads/epipharyngeal-abrasive-therapy-eat-has-potential-as-a-novel-method-for-long-covid-treatment-2022-imai-et-al.27905/#post-433152
There’s some helpful information there – thanks. I appreciate the digging that has been done. I haven’t been over there for years but I have a bit different orientation than some.
There’s a critical approach that finds shortcomings and therefore ends up being dismissive of a study or trial’s possibilities and there’s a critical approach that recognizes the shortcomings present while acknowledging the possibilities that are present as well.
If a study is flawed that simply means it’s flawed – it doesn’t mean anything about the effectiveness of the treatment or the veracity of a hypothesis. It simply means that it needs better study. The possibility is still present.
As I pointed out – these studies are almost all quite flawed – and are in serious need of validation :). I put in the quote at the top to remind us of how important these small, necessarily, flawed studies are. They are ctually the place where breakthroughs begin – where the message goes out to the scientific community that something might be there.
“Consider that larger clinical trials are often meant to confirm something important to change our practice. The small trials are the ones making conceptual breakthroughs that change our thinking.”
I had covid for the first time last week and its made me feel a bit more tired and stiffness than usual, I spending more time in bed in the middle of the day than prior to infection, which is not unheard of for me but it isn’t something that happens every week or month. I don’t seem to have any new symptoms however. I have a question that I can’t find an answer to on Google search – is it even possible to have ME/CFS and then also later contract ‘long covid’ ?
Another thing that might be important, might be nothing, is that I realized I have never had the ‘hiccups’ since developing ME/CFS symptoms in 2015, I am curious whether this might be something that we all have in common ?
Hiccups are associated with the vagus nerve. Lower vagus nerve “tone” might decrease the frequency of hiccups (?) I’m posting because my husband would get hiccups that lasted for days and we researched a lot about the causes and possible helps. Some people, to stop that kind of hiccups, have a particular nerve cut (not the vagus but in the same vicinity). I know this is vague, but much is unknown about hiccups. Dentist said that he was taught hiccups was a way to try to reset the heart rhythm. My husband also had heart problems as well as esophageal deterioration so any of that that could have been involved. No specialists he accessed were able to help him.
I think it’s related to inflammation in the esophagus maybe bacteria, maybe allergic reaction to certain foods (from what I have experienced and observed in my family) And collagen that gets messed up when DHEA is low (universal in ME/CFS)
DHEA (very low dose, none of these ungodly supraphysiological doses mainstream uses) seems to be helping in my case.
I’m newly me/cfs by way of long covid, but I have seen a few dozen people posting about developing long covid on top of their existing me/cfs. Some people have said it simply lowered their baseline without new symptoms but most posts I’ve seen said they felt a clear difference in new long covid symptoms.
I came down with long covid 1.5 years ago and I have not had a case of the hiccups even once since I got sick, and I usually get them fairly frequently, once a month at least. However, I have been steadily recovering on Maraviroc and after 3 days of TENS vagus nerve stimulation, I got the hiccups again! It really got my attention because its one of those weird things that I’ve noticed. I thought, maybe the hiccups is vagus nerve related. So your comment is very interesting, maybe there is something to it!
Thanks Cort for this overview.
As a (single) infusion, BC 007 is an alternative to immune absorption.
It has been successfully tested on 4 LongCovid and 1 ME/CFS sufferers.
https://www.fau.eu/2022/08/05/news/research/diagnosis-and-therapy-of-me-cfs-what-can-we-learn-from-long-covid/
Unfortunately the license is missing. BC 007 is a non-modified 15mer single-strand DNA oligonucleotide; an aptamer – it is able to neutralize autoantibodies directed against G protein-coupled receptors.
Thanks DJ – from what I’ve heard a bigger long COVID trial is in the works – and hopefully at some point an ME/CFS trial.
We need more international awareness of BC007 as the german government does nothing to help Berlin Cures (small start up)!!! How can we achieve this???
BC007 seems highly potential and there are almost no side effects
Cort, I want to thank you for such a hopeful post! Finally a list of exactly what is being tried–even if they are small efforts! I think many of us live on hope. I know I do.
I try so many things I want to report on my latest; ProDentim. Yes, I fell for those hinky ads on YouTube about a mineral that helps teeth, in my case Ehlers-Danlos fragile and failing teeth. The developer was intrigued by so many ancient skulls with perfect teeth. He concluded ancient man had a healthy mucosal biome and also that many of the ingredients in our modern toothpaste was destroying it.
So I bought ProDentim and was very surprised to find my usually clogged nose suddenly clear! So far I seem to think a bit clearer and my energy is up. It’s too soon to tell but the idea that oral biome can influence other body systems does have some factual support.
On the other hand, Stanford’s idea of ketotifen has not demonstrated much improvement even though Dr. Bonilla wants me to continue to take it at a higher dose.
Again Cort, thank you for the hopeful post!!!
Thank you for the mention (SGB), and for the complement on my writing! I did not apply for RECOVER funding… the application period was very short and I do not have the resources to complete a federal grant application in that time period (same thing for DoD CDMRP… invited to submit full proposal, don’t have the resources to do it). Perhaps a group with better resources and infrastructure will take this up and run with it, but it won’t be us.
Thanks, Duricka. We’re all hoping that the recent visibility regarding SGB translates into more support and most of all funding. You guys have been great at getting the word out.
This is an awesome write-up, Cort! But why do you say “Etanercept seems like a long shot”? Dr Klimas seems pretty confident it may help.
The perispinal application of it – that really seems like a long shot to me but so does etanercept because it hasn’t been tried before in these diseases and my guess is that initial trials will focus on potential treatments that have broad-based support. That said, this is the NIH and they may focus more on drug-based interventions and something like etanercept which has the potential to knock down neuroinflammation might fit their ticket.
Peer reviewed paper from Biochemical Journal, founded 1906, and posted by Di Mohr, I think Comment 12, is amazing. Pulls together so much about commonalities in chronic illness, much about ME CFS and the road to ME from Covid. Many markers and current unusual labs I could relate to personally, and current suggestions regarding treatments for circulatory issues, etc. Hypercoagulation, particularly microclots is figuring big these days. Found in CIRS also.
Amazing article! Thank you!!!
Seems a suitable place to up date on my hyperbaric oxygen therapy. I completed 20 1 hour sessions 2 weeks ago and am now on a maintenance session each week. After about 10 sessions brain fog was reduced but I was feeling very tired after each session. On to 20 sessions and I was thinking much more clearly and fatigue improved but not a massive improvement. I couldnt tolerate a session every day, managing 2 or 3 a week initially and 4 at the end. This was partly due to fatigue but also ear problems, I am treated with other people.
Unfortunately I fear the effect is not permanent. I can still do more than before treatment but I need the weekly top up. Whether this would be necessary if I’d had more sessions initially or could have managed higher frequency of treatment I dont know.
Also dont know if the dives are necessary or if almost the same effect could be achieved by purchasing an oxygen concentrator and using that regularly. If anyone is trying to devise a clinical trial I think they should include that as a treatment option. It would be a much cheaper treatment and might still improve oxygen flows to the brain. I’m thinking of purchasing a Philips machine to use in between hyperbaric oxygen treatments.
Re the vagus nerve , anecdotally my symptoms and energy levels have improved ( with no severe crashes for a while , touch wood , unusual for me as been ill since the 1980s ) whilst listening to classical music , especially early
baroque .
I almost feel like it’s massaging the inside of my head 😊 .
I looked up the science and apparently there is research behind the notion .
Incidentally , I listen to BBC Radio 3 . Before I mostly listened to radio 4 , which is a talk station . It took a while to figure out why I felt a bit better ( by no means cured ! ) as I hadn’t been trying any different medications . That’s when I thought about the radio and looked up the possibility .
Been wondering too if that’s why we often find it difficult to listen to music . Apparently only certain types stimulate the vagus , so perhaps others are harmful at certain stages of M.E. / CFS .
Sometimes , I can’t listen to any music but perhaps that could be herxing with the classical . Even when I’m enjoying it I feel I need a rest after listening for a while .
Anyway , as we’re unlikely to get a trial , it costs nothing to try and , even if I’m kidding myself , there’s no side effects and it relieves stress and calms the breathing and blood pressure .
Thanks again , Cort , for doing so much for us at significant cost to your wellbeing .
Chris .
Mozart for me!!
I was first diagnosed in 1984, but I think I was ill since 1980. I was diagnosed with chronic encephalopathy and immune deficiency (no official name for the illness had been suggested yet) and put on a treatment for each. I always believed my doctor who had been prominent in the Academy of Allergy and Immunology knew a lot more about what I had than he was saying. I asked him if he could cure me and he said “no, but I can give you more good days than bad days”.
Fast forward to 1986, two researchers in the Gallo AIDS lab have discovered a new virus. At first, it is so lethal that they can’t keep it alive long enough to study it. When they finally figure out a way to do this, they discover that the virus is killing B cells so they name it HBLV.
Then they find out it is killing T cells as well so they call it HHV-6 and further subdivide this into HHV6 B (the cause of childhood roseola) and HHV6 A ( a much more devastating virus). At this point, they estimate that 30% of the population is infected with HHV 6, but no one knows the precise breakdown between A and B cases.
By this time, we have formed a support group in our city and I convince my doctor to send blood samples from group members and nonaffected family controls to the lab (at our expense) to look for this new virus. The lab does this, but refuses to give us our test results.
In the interim, I test positive for HHV-6 A through a research lab that Dr. Paul Cheney is working with. I doubt that most ME/CFS patients have been tested for HHV-6 A because they don’t make it easy. The Quest lab tests don’t differentiate between the two versions of HHV-6.
Here is something to think about. What if Covid reactivates HHV-6 A in certain patients? It is estimated that 90% of the population in now infected with HHV6, but no one knows the breakdown between A and B.
HHV6 A is a member of the herpes family of viruses. Once you have it, it lives in your body forever, just like EBV. Anything that lowers your immunity could allow the virus to reactivate. This includes other viruses and toxic exposures.
The problem with all of these treatment studies is if they don’t know the cause, all these treatments are just like throwing darts with a blindfold and some may do more harm than good.
What about the HBOT home chamber ?
Thank you for this compilation. As always, your writings provide great information and inspiration!
Great blog, Cort!
Let’s keep our eye on this trial of suramin for long Covid. Naviaux is quoted:
https://www.prnewswire.com/news-releases/paxmedica-plans-to-initiate-phase-1b-study-for-pax-101-in-patients-with-long-covid-19-syndrome-301456006.html
Also, isn’t Ampligen being tested on long Covid?
Hello Cort,
there is actually a small clinical trial about this in Germany. 1400 patients, ME/CFS subgroup were 928 patients.
It’s at a private day clinic + they call it Cerebropheresis®, at INUS Medical Center, Cham, near Munich, Germany.
It’s on Dr. Klinghardt’s website, below see the link.
https://klinghardtinstitute.com/teachings/slides-from-me-cfs-event-15th-feb-2020/
They use it to treat me/cfs, long covid, chronic virus infections, autoimmune, alzheimers. Cost is from 1400-2400 euros per treatment, depending on the filters used.
Improvements are seen on slide 32 of the presentation.
Research in english published in Nature (p. 4), success for Alzheimer’s + description in english of procedure. Link below:
https://biologicum-baden.de/wp-content/uploads/2021/01/Nature.pdf
I would really love to have your opinion on it, as my son Yannick (21) has ME for 7 years now + worsening + now housebound/bedbound + had to drop university. He has other issues too, partly addressed: Mold, Borrelia + bartonella, gut dysbiosis/sibo, possibly MCAS + candida we can’t get rid off.
We took out a student loan to go to Germany to do this treatment, as everthing else failed, but are unsure if it’s worth it.
PS We are German nationals living in France.
Thanks so much! Stephanie