

Could a cheap, generic drug used in ADHD help with long COVID, ME/CFS, and FM?
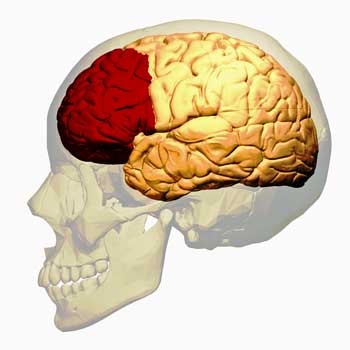
Among other things the prefrontal cortex reigns is in charge of reigning in a sometimes twitchy limbic system.
What an interesting idea! See if a drug that was designed to improve prefrontal cortex and executive functioning could help combat brain fog in long COVID. It makes sense. The bigger question is why this drug was not tried in either chronic fatigue syndrome (ME/CFS) or fibromyalgia (FM) a decade ago.
We’ve known, after all, about poor executive and prefrontal cortex functioning in them for a long time. We know that exercise reduces the flow of oxygenated blood to the prefrontal cortex in ME/CFS, thus impairing executive functioning and cognition. We know that children with ME/CFS have to engage more regions of their prefrontal cortex than normal to carry out tasks. We know that reduced gray matter has been found. Enough interest in the prefrontal cortex (PFC) in ME/CFS has shown up that a repetitive transcranial magnetic resonance (rTMS) trial that seeks to increase PFC functioning is underway.
Literally, dozens of studies have assessed the prefrontal cortex in fibromyalgia. A hyper prefrontal-motor connection has been associated with increased pain. Boosting prefrontal cortex functioning with rTMS has produced good results in several studies. Strange electrical oscillations have been found in the prefrontal cortices of FM patients.
The Guanfacine Gambit
In its short time with us, long COVID has once again produced something that neither fibromyalgia nor ME/CFS was able to do – but made sense to do: publish a treatment study of a prefrontal cortex-enhancing drug called guanfacine. Guanfacine is an anti-inflammatory drug that’s able to turn down the microglia and protect the prefrontal cortex from low oxygen states (which are apparently found after exercise in ME/CFS), and has been shown to enhance cognitive functioning in encephalomyelitis to boot.
Guanfacine (not to be confused with Guaifenesin) is sold under the brand name Tenex. It was created by the senior author of the study, Amy Arnsten, Ph.D, an Albert E. Kent Professor of Neuroscience and professor of psychology at Yale. Guanfacine, or Tenex, was FDA-approved for use in ADHD in 2009 but according to a Yale Magazine piece, has been used “extensively” off-label in PTSD and traumatic brain injury. It’s now available as a generic.
According to Wikipedia, Guanfacine is often used to reduce anxiety and to treat post-traumatic stress disorder. If you’re having nightmares, it may also help with them. It’s also FDA-approved to be used in conjunction with stimulants.
NAC is Back
Guanfacine is being given with 600 mg of N-acetylcysteine or (NAC) daily. NAC has an unusual history in ME/CFS. One of the very rare NIH-funded treatment studies for ME/CFS is assessing the effects of different levels of NAC supplementation. NAC provides a nice complement to guanfacine as it is anti-inflammatory, inhibits an enzyme associated with kynurenine, and protects against calcium overload in the mitochondria.
Results
The Gist
- It made perfect sense. Given the evidence of poor executive and prefrontal cortex functioning in long COVID, why not try a cheap generic drug that was designed to improve cognition and prefrontal cortex functioning in long COVID?
- A bigger question might be – given the similar problems found in ME/CFS and FM why this drug wasn’t trialed in these diseases years ago. That’s long COVID for you, though: it keeps surfacing things that make sense in ME/CFS/FM but never saw the light of day.
- Guanfacine is an alpha-2aa adrenergic receptor agonist that was approved in 2009 to treat ADHD. Its also used off-label extensively in anxiety and PTSD. An anti-inflammatory drug it’s able to turn microglial activity (neuroinflammation), protect the prefrontal cortex and enhance cognitive functioning.
- This case report study simply followed 12 long-COVID patients given a 1 mg tablet PO (by mouth) at night for the first month, which was increased to 2 mg if patients could tolerate it, as well as 600 mg of NAC daily.
- Four patients quit – two due to low blood pressure and/or dizziness and two for unspecified reasons. The eight who remained all reported benefits with working memory, concentration, and multitasking, and some reported their brain fog went away completely.
- Guanfacine strengthens the ability of the prefrontal cortex to tame the fear center of the brain – the amygdala. One ME/CFS hypothesis proposes that damage to the prefrontal cortex has removed an inhibitory brake on the limbic system in ME/CFS. The resulting hyperarousal and hypervigilance causes their autonomic nervous systems to react to the slightest stimuli, leaving them tired and wired.
- The authors believe that problems with tryptophan and calcium metabolism – which have been highlighted recently in ME/CFS/FM and long COVID – play a key role in brain fog in long COVID.
- Guanfacine also enhances the activity of a receptor that may be associated with orthostatic intolerance in ME/CFS and that exercise decreases in about 30% of people with ME/CFS.
- While the rates of ADHD haven’t been assessed in long COVID yet, they appear to be high in both ME/CFS and fibromyalgia – making Guanfacine, which has been approved for ADHD, an interesting possibility for these diseases.
- The study was small – just 12 patients – but the authors were confident enough in their results to publicly call for doctors to read the paper – and try the combination therapy on their patients stating “You don’t need to wait to be part of a research trial. You can ask your physician – these drugs are affordable and widely available.”
Four patients quit – two due to low blood pressure and/or dizziness and two for unspecified reasons. The eight who remained all reported benefits with working memory, concentration, and multitasking, and some reported their brain fog went away completely.
The authors reported Guanfacine was generally well tolerated. (Typical side effects such as fatigue, irritability, and stomach upset reportedly usually subside within a week or two.)
Mode of Action
It appears that Guanfacine and other drugs of its ilk strengthen the ability of the prefrontal cortex to tame the fear center of the brain – the amygdala. One hypothesis proposes that damage to the prefrontal cortex has removed an inhibitory brake on the limbic system in ME/CFS. The resulting hyperarousal and hypervigilance causes their autonomic nervous systems to react to the slightest stimuli, leaving them tired and wired.
The authors also believe, interestingly enough, that increased kynurenine levels in long COVID block the NMDA receptors from turning the prefrontal cortex on. That’s an intriguing idea given the recent ME/CFS/FM and long-COVID studies that have connected impaired tryptophan metabolism in the gut with the production of toxic metabolites such as kynurenine that affect the brain.
Guanfacine also stimulates the adrenergic α-2A receptor. Because exercise decreased adrenergic α-2A receptor gene expression in about 30% of ME/CFS patients, many of whom also had trouble with orthostatic intolerance (problems standing), perhaps guanfacine is a possibility for them.
At the molecular level, the authors believe it all comes down to calcium signaling – which provides yet another possible ME/CFS connection (blog coming up).
The ADHD Connection in ME/CFS, Fibromyalgia… and Long COVID?
The fact that Guanfacine has been approved for ADHD and for use with stimulants is more than intriguing. Thus far, the ADHD connection appears to have been missed in long COVID, but if the past is prologue regarding this suite of disorders, it should be showing up soon.
According to the National Institute of Mental Health (NIMH), ADHD is characterized by difficulty staying on task and sustaining focus, feeling the need to move constantly, and increased impulsive behaviors. People with ADHD tend to miss details, have problems organizing activities, lose things, and are easily distracted. (That pretty much fits me to a tee…)
- Check out the WHO’s self-test for ADHD in Health Rising’s Cognitive Resource section.
Given common complaints of “racing minds”, difficulty concentrating, difficulty following conversations, reduced information processing speed, and the wired and tired state, ADHD seems like a natural fit for both FM and ME/CFS. In fact, several past studies have suggested that ADHD is increased in FM, and one found that 30% of children with ME/CFS met the criteria for ADHD.
Conclusion

Could an ADHD drug help with the brain fog in long COVID, ME/CFS, and FM?
And so long COVID opens up another potential treatment option for ME/CFS, FM, and similar diseases. It was nice to see quite a few potential overlaps between these diseases, including a weakened prefrontal cortex, problems with tryptophan and calcium metabolism and possibly ADHD. The authors noted that a similar type of brain fog was found in ME/CFS and post-treatment Lyme disease syndrome.
The study was small – just 12 patients – and the drug clearly needs a placebo-controlled trial, but the authors were confident enough in their results to publicly call for doctors to read the paper – and try the combination therapy on their patients stating
“You don’t need to wait to be part of a research trial. You can ask your physician – these drugs are affordable and widely available.”
BIG (Little) Donation Drive Update
Thanks to the over 370 people who have supported Health Rising thus far on our end of the year (plus) drive :).

We try to make things clear so that you don’t have to.
Trying to make your way through a medical research paper is enough to trigger a nice case of brain fog in anyone – but that’s why Health Rising is here. We try to be the antidote to medical research-induced brain fog. While the blogs are no walk in the park they try to make things as clear as possible – including studies of drugs that might help brain fog (lol).
If that approach triggers nice things to happen in your brain please support us in our end-of-the-year drive.






I tried guanfacine and clonidine, another a2 agonist, a decade or more ago. They never did much for me but lower my blood pressure, maybe a slight headache. Naphazoline, on the other hand, an alpha-1 agonist in eye drops, had a profound effect on me, giving a euphoric kind of feeling. It was kind of scary it was so intense, so I was afraid to try it again. Oral alpha-1 agonists like adrafinil can help cognition, but they can be really hard on the liver. I don’t even know if adrafinil is available anymore; I tried all this stuff decades ago before concluding that none of it actually affected the root cause of either ME or brain fog. In me, at least.
A study of 8 patients? These are the potential side effects of guanfacine:
Constipation.
dryness of the mouth.
sleepiness or unusual drowsiness.
unusual dullness or feeling of sluggishness.
upper abdominal or stomach pain.
weight gain.
How are any of these better than brain fog? This study did not deserve to be mentioned.
I’ve found most side effects occur because of overdosing. Many people need a much lower dose than the “standard” dose prescribed. I always start any new drug, be it herbal or prescription, at 1/4 dose for a few days and have good success and not many side effects. (Antibiotics are the exception, always take the full dose). If I take the full dose of most meds I’ll have many of the common side effects. All meds and suppplements come with side effects. It’s your decision what to try.
Hi T Allen, You are right about low doses in ME/CFS and that is an important point. However, nobody knows the right dose for them and some side effects can be irreparable. Thousands of children (including our son) were born with partially missing limbs because of a drug that had lethal effects in some pregnancies. (We spent 10 years getting that drug off the worldwide market.) The main point in my comment, however, is that a study of only 8 people is next to worthless. And the fact that 4 dropped out of the study is troublesome.
The study was designed to get some attention – not settle whether the drug was effective – and here we are discussing it – so it’s clearly got some attention. In fact, the media picked up this study pretty well – so it’s making the rounds. I would say it served its purpose.
Because it’s a generic drug we’ll probably never get the big placebo-controlled trial what we want – this may be the best we’ll ever get and honestly, that’s fine. The authors have considerable experience with it, its been found to be helpful in anxiety and PTSD as well and it’s generally well tolerated and it’s cheap and available – so why not, if you can think you can handle it, give it a try?
So true T Allen, side effects are effects. There are effects we might like and want and there are effects we don’t like and we may make the decision that the bad effects are not worth it so we can discontinue, but we don’t know until we try.
Guanfacine unfortunately is $124 for 28 days in Australia. Hoping the generic will be available soon though.
Excellent points! With ME/CFS for 27 years, I nearly always need smaller doses of most meds that can be helpful. It is also useful to remember that a lot of research and subsequent recommendations on dosages are based on subjects who are male and relatively young. Certainly this would seem to be the case for ADHD research
“Potential” side-effects are “potential” and many of those apparently fade after a week or so on the drug.
I assume that the 8/12 patients who did well on the drug didn’t have problems with them. Trazodone which has a list of possible side effects at least that long and I haven’t had any problem with it
What interested me with this drug is that it was created in order to boost prefrontal cortex functioning and some researchers believe that poor prefrontal cortex functioning could play a big role in ME/CFS.
Since I would say that my limbic system is pretty much roaring away anything that could get that in check seems worth a try.
Why not give it a try? Because any trial takes days and weeks out of my life, every time I have a reaction to a new medicine.
My own history was reinforced with recent surgery and the horrific reaction to having the pain meds I’ve used for a long time but which had potential problems for surgery and anesthesia CHANGED before and after the surgery.
I will not take any of THOSE drugs again – I had everything from brain fog to the kinds of ‘ideations’ I will not mention, and flaming pain for over a month.
THAT is the why not. I can’t afford the cost.
Got it – they are not for you but they may be for other people. For me, I’ve stayed away from prescription drugs for years but recently I’ve found them helpful – I’m not as wary as I used to be.
Ultimately, I think it will be drugs that get most of us out of this. I don’t see any other way for most of us.
I don’t doubt it might be prescription drugs – but I’m ONLY going to try well-vetted ones that have been PROVEN to work – because I KNOW I face side-effect hell. And it better be with an experienced physician, not one I talk into letting me ‘try’ something – I will not be the one experimenting. Other people’s willingness to try MAY some day benefit me – and I am grateful to them for that willingness – but you asked, ‘Why not try?’ and I replied from my experience: I can’t afford to.
I wouldn’t even be able to tell if one might work for me, and would most likely end up abandoning an experiment – the 33% (8) people who left the trial won’t know if it might have worked for them either.
It’s not lack of willingness on MY part so much as bitter prior experience.
These side effects are commonly listed in just about every drug I take. Some I get and some I don’t. But they are all “known” effects a layperson could understand…dry mouth, drowsy etc, and work round. But Brain fog for me…I’m a 25%’er, is off the scale crippling, untreatable and highly abnormal.
Depends on how bad the side effects were don’t you think…
But you are correct they should be mentioned.
Some of these side effects T’s are common in people that have poor management of MCAS.
Hi Leanne,
Yes, I agree that Mast Cell Disorder could be a red flag for those more likely to have adverse effects from drugs.
I am almost sorry I mentioned the side effect issue, because the main point I was making is that the study was only with 12 patients; 4 dropped out and there was no control group for even this small number of patients.
.
Knowing now what I didn’t know before the dreaded 2020, how can I ever trust another medication since medications/pharmaceuticals are probably what put me in this condition in the first place? I believe the key is fixing our immune systems broken by overuse of immunizations and antibiotics and our chemical-laden, bioengineered food. I’m off all pain meds and am working with a functional medicine practitioner (cash only, of course, since our insurance companies are also our corporate medical centers and pharmaceutical companies) on a mast-cell activation syndrome treatment plan. I pray my instincts on this are correct.
Good luck! Definitely worth trying mast cell treatments…:)
Pam, wondering what you are doing with your functional med dr & if anything is helping?
Betty, I am in agreement with you on the “8 patients”. It isn’t much of a study, but the mechanism of the medication is interesting. Reading the long list of side effects is often discouraging.
I actually try to avoid looking at them. I figure if something shows up that’s a problem I’ll know it. Just about every drug has a pretty long list
ADHD or not, you do a wonderful job of presenting so much information to us. Thank you Cort for all your hard work.
Hope you have a lovely Christmas!
Thanks! Definitely got some ADHD going on there – particularly in the mornings for some reason… Just part of the package, I guess.
What are your symptoms of ADHD Cort?
Is that a typo? It says ‘turn microglial activity’ Do you mean ‘turn down microglial activity’?
Definitely don’t want to turn up the microglial activity (lol). Thanks – I will fix.
Great, and thanks so much for this article and others Cort! Merry Christmas, Hanukah, Solstice etc..
I get the same effect with Liposomal Vitamin C 1000, 5ml. Which started taking about 3 weeks ago.
My brainfog disappeared overnight and my energy has increased. I was suddenly able to do complex mathematical calculations AND remembered things from the night before and from the past.
Only when I started taking this Vit C I realized how extremely brainfogged I had been for an entire year.
I am also on NADH+ Ubiquinol for mitochondrial function and other supplements. Have been for a few months.
This is the second time I heard about liposomal vitamin C 1000mg for fibromyalgia. I’ll look into it. Thanks for sharing!
That’s amazing! And a good reminder b/c I used to take quite a lot of liposomal Vitamin C and had short-lived, but similar eyeopening and brain awakening experiences with high dose IV Vitamin C. May I ask what brand you’re using and where you get it? The one I used to use was very expensive.
Hi Drew. Sure!
Naka Platinum Liposomal Vitamin C 1000mg C1000, Orange Flavour, 750ml
That for sure won’t break the bank at 5ml/day.
If you read what Vit.C does to your cells I find it makes sooo much sense to take it – doesn’t it?
good luck!
Please let us know if you see a difference.
Angelika, can I ask what NADH + Ubiquinol product you take? Is it one product or two? Thank U for Vit C info!
Pure Lab Vitamins NADH + Ubiquinol
Details
Pure Lab Vitamins NADH + Ubiquinol is a dynamic combination of 2 powerful co-enzymes. CoQ10 (ubiquinol) is utilized by every cell in the body to improve energy production and prevent oxidation. NADH (nicotinamide-adenine dinucleotide) is a reduced form of the B vitamin niacin. It is vital to neurotransmitter function and cellular energy production. The highest concentrations of these two important coenzymes are found in the brain and heart.
Pure Lab Vitamins NADH + Ubiquinol Features and Benefits
NADH+Ubiquinol provides an energy boost to every cell in the body, but especially to the heart and brain—where the highest concentrations of these two important coenzymes are found. Individuals within different cohorts have been shown to benefit from the combined energizing effect of these nutrients. Studies performed by Dr. G.D. Birkmayer and team have shown some impressive results with just 20 milligrams of daily NADH supplementation in athletes. Participants found lactic acid-related muscle fatigue after prolonged activity. This means that athletes could perform longer, and the recovery period between training sessions could be shorter, with the same rejuvenating results obtained from a longer rest period. Second, users found 7% more energy, which is likely due to the fact that NADH triggers ATP production—the basic energy source of all cells.
I found another brand that’s less expensive and has more NADH and CoQ10 per serving. It’s from ProHealth. I think I will try that. Side note: I wish there was a supplement that combines NADH, Ubiquinol, and PQQ.
Thank you Cort for your great work for us sufferers. It means a lot to us!
I made a donation to the OMF which I believe supports your work.
Happy Holidays!
In gratitude from Montreal/Canada
Glad to hear it! Hope you’re staying warm in Montreal 🙂
Yes, we are! We hsve a fireplace. 🙂
A friend who is a doctor sent this study to me last week. I do take NAC already, so I spent some time reading about Guanfacine and think I’m not a candidate because of low blood pressure, POTS, other cardiac-presenting form of Dysautonomia. The only real treatments for any of my co-morbid conditions common to ME/CFS is all about raising my blood pressure: weekly IV-saline, drinking 72+ ounces of water a day, increased salt intake, electrolyte tabs, compression socks.
Fortunately we’d need a doctor to prescribe the Guanfacine component, and hopefully that discussion would happen with someone who you’ve been seeing for some time and knows your heart/cardio history. But if you’re new to this illness and have not checked out heart manifestations, please do that before trying this drug. A well-meaning physician may not know how common
It’s interesting because the people in the ME/CFS gene expression study with a2 adrenergic gene expression had more orthostatic intolerance and this is an a2 adrenergic receptor enhancer (agonist). I really don’t know it all would work given that it can lower blood pressure and cause dizziness.
1. Clonidine is helpful in the treatment of orthostatic intolerance. I did not search for guanfacine. I believe it should be similar.
2. Patients express more α2 receptors, doesn’t mean the stimulant will make things worse, because agonists make receptors down, not up.
I saw that info too, it was originally for decreasing blood pressure which is the last thing I need. But it’s inexpensive and might be worth trying at a much lower dose. Not that I want to pay for another compounded medicine but…..
Compared to all the comorbidities I have associated with ME/CFS, those side effects are nothing. I’ll try any prescription that has a remote chance of getting the “brain frogs” out of my head!
I’m with Val!
I have problems standing – so that is a BIG concern – but overall, the dysfunction that is most distressing and crippling, for me, is the brain fog and ADHD. So I’ll give a generic drug a try, starting at a very low dose, and working up.
I happen to have dysregulated blood pressure – it is sometimes low, but sometimes VERY HIGH, so I am on BP meds. Maybe this drug will improve that situation as a positive side effect.
Here’s to better health for all of us in the New Year, and hoping that NAC is not snatched from the shelves by our esteemed “regulators”…..
https://www.nutritionaloutlook.com/view/the-fight-between-the-dietary-supplement-industry-and-fda-over-the-ingredient-nac-will-heat-up-in-2022-2022-ingredient-trends-for-food-drinks-dietary-supplements-and-natural-products
https://www.nutraingredients-usa.com/Article/2022/11/02/npa-withdraws-fda-lawsuit-following-final-nac-guidance-marketplace-stabilization
100% agree. 25% ME is often cited as worse than MS/Cancer and many other chronic/terminal illnesses. and I can well believe it. My friends who have won or lost to cancer had remission, treatment, recovery or they died. And their periods of extreme illness were relatively shortlived. Why would I worry about side effects of drugs, or even addiction. I’ll cross that bridge if they ever cure me. 11 years bedridden.
I definitively want to try it. The difficulty to multi task is really what struck me with this article. Thanks, merci, gracias Cort for your amazing work. Who could guess that you can’t multi-task! You are so prolific!
I will talk to my GP. She is more than willing to try things, she has the humility to say that everything she knows about ME is because I told her. And she is now on a long COVID committee. And she is a fast learner…
I tried guanfacine a couple of years ago, ramping up the dose over some days.
It dropped my blood pressure, so I had to reduce my amlopidine (BP med) dose to accommodate it. (Even so, I ended up in the urgent care clinic one morning with light-headedness and 90/60 BP.)
At a reasonable dose, it perhaps took the edge off my anger – but didn’t increase mental clarity AFAIK.
It did make my ankles swell with edema, and so I eventually stopped taking it.
I tried Guanfacine at the suggestion of Dr. Kaufman. I have hyper-andrenergic POTS, so I have high blood pressure. I had trouble getting the BP under control and also runaway ADD. It’s worked on both counts. The dry mouth lessened and I still feel like a nap after 5 hours or so, but I’m sleeping better at night without drugs, which is great. If you don’t have low blood pressure, it could be worth a try.
So glad it worked for you.
I have POTS/OH and have low blood pressure. But, I’m so tempted to try it anyway.
It will most likely lower your blood pressure, so be careful.
I’m very interested, given my OA, high blood pressure (atypical OA: my bp goes up!), ADHD etc. I take provigil for my fog and to amp up my antidepressant. But it has its downsides.
But I want to note that WEIGHT GAIN as a side effect of tenex worries me. Practically every med I’m on—and I think mine are necessary and helpful, although I’m starting my 11th year in bed—have combined to raise my weight from 155 to 185 —and of course I can’t exercise to temper that. The weight gain in turn worsens my spine snd other pain, brings me closer every day to diabetes, makes breathing deep harder, sleep worse, etc. I think this phenomenon—isn’t given enough attention. I’ve seen many doctors dismiss weight gain as a side effect, let alone think abt the cumulative effect. Including doctors who later do the fat shaming and refuse to believe that I cannot exercise at all.
I’ve lost weight. I was surprised to see a side effect was weight gain. If I had read that was a side effect, I wouldn’t have taken it because I also can’t afford to gain weight. My metabolism is so slow to begin with. But I have found it to be an appetite suppressant.
Barbara, would you share the dosage you have found helpful? And did you need to start at a lower dose and work up? Perhaps Dr Kaufman had you start at a lower dose anyway.
I went to Dr Kaufman when I lived on the West Coast several years ago and liked him a lot.
My cognitive and memory problems have always been an issue and have been getting worse. In the past couple of years I have done trial and error with two other ADD meds and found low doses that do help somewhat, but I am still going downhill, so want to ask my smart, helpful GP if he would consider trying me on guanfacine too.
I definitely don’t have ADHD and I know what it is from a step son and students with the disorder. I had brain fog with Lyme for a few years before progressing to CFS. It went away with anti-parasitic treatments. Brain fog seems to be connected to inflammation in the brain. That’s why low dose Naltrexone helps and I’d be interested in trying this because LDN tends to give me bad dreams and disrupt what little sleep I get. Thanks for another great report Cort! I hope more people decide this info is worth paying for. Merry Christmas!
@TAllen, do you mind sharing what anti-parasitic treatment worked for the brain fog? Thank you.
I used Zahler ParaGuard, Advanced Cleanse and Digestive Supplement. At the time (2015) it was labeled for parasites. Look it up on Amazon and you can see it works for a lot of people even though the “experts” say it doesn’t. For $30 it’s worth a try and even if it doesn’t help the brain fog it won’t hurt to clean out some other parasites. (If you eat food you have parasites). The key is to do the treatment right! First make sure you don’t have any reason to avoid any of the ingredients! Then start slowly to make sure you won’t have a bad reaction. You know how you react to herbs so take a few drops or a half dose and wait 24 hours. If that is ok work your way up to the full recommended dose. You can take it for the 30 days on the bottle or 3 weeks on, 2 weeks off and another 2 weeks on. Make very sure you restart no more than 2 weeks later or otherwise parasites will be reproducing resistant eggs again! You can keep repeating this if necessary. I did one round like this with great results, by brain fog just disappeared one day like a light bulb turned on. About a month later I realized I was getting foggy again and restarted the protocol. 12 hours after starting the fog lifted again but I continued the 3 weeks to make sure I killed everything off and I haven’t needed another treatment since. I still have CFS (in remission) and now MCAS but at least the parasites or whatever was causing the brain fog is gone. I really hope this works for you! If it does please spread the word. 🙂
@TAllen I shall certainly look them up. Thank you for your prompt reply. If it works, rest assured I’ll be screaming from the rooftop 🙂
My first thought was that if this med helps with my brain fog it would be great. My second thought – what kind of mischief will my brain find! 😝 To mess up all the other fatigue in my body!
Well not as serious comment after all, lets wait and se what comes out of this. Alway grateful that you read and makes the science articles readable for me 🥰
Super interesting.
So it could *potentially* help with orthostatic intolerance, as well?
A quick check with 2 German online apothecaries showed that it does not yet seem to be generic in Germany. These apothecaries display only one product costing between a 100 and 140 EUR/28 tablets. (In the public insurance system, it seems to have only one approved indication as second line treatment for childhood/adolescent ADHD). Good thing seems that it does not seem to be subject of Betäubungsmittelverordnung (drug control regulations).
I have low blood pressure AND what feels like sympathetic overdrive. So not sure about this.
Off-label use of drugs is about all we have right now. So imperfect as this study is.
By my logic it makes perfect sense for me to try this drug. Before I was diagnosed with ME/CFS a few months ago, I thought I had ADHD, confirmed by my response to stimulant medications that helped. I still intermittently use Vyvanse or Armodafinil to support executive functioning and motivataion. I hope to leave stimulants behind at some point. I will give this a try with and without stimulants.
Russian translation: https://forums.epstein-barr-virus.ru/threads/1984/ (Hope you don’t mind, Cort)
I have tried it together with NAC and am seeing 50 per cent improvement with brain fog. I have Long Covid (1 1/2 years and fibromyalgia for over 25 years. The brain fog and headaches due to Long Covid were bad, especially the short term memory loss. I take 1/2 the prescribed dose every other day and a full pill on the other days. I don’t know how long I want to be on this medication but for now I’ll take it!
Do we know if it was SR or XR guanfacine?
so cool!
THANK YOU for putting so much time and energy into these posts!