Fibromyalgia (FM) is so weird. Exercise studies are just going gangbusters. If researchers devoted as much time and money to attempting to understand what’s going on in FM as they do on exercise studies we might have some real answers.
The outcome has been that exercise is now considered the “foundation” of fibromyalgia treatment. There’s no doubt that moderate exercise can be helpful. On the other hand, studies keep also finding problems with exercise and energy production, some of which echo similar findings in chronic fatigue syndrome (ME/CFS) and long COVID. Energy assessments in ME/CFS tend to use cardiopulmonary exercise tests, while those in FM tend to muscle function.
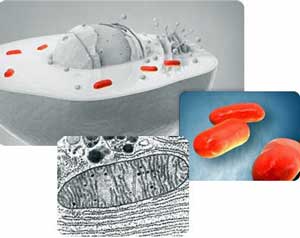
Muscle studies have often found problems with the mitochondria and other factors in FM.
The result is that many more muscle studies have been done in FM than in ME/CFS and the results almost always point to muscle issues. Other studies suggest that something has gone wrong with the mitochondria in fibromyalgia (FM). CoQ10 levels may be low, autophagy may be impaired, a genetic impairment may exist, carnitine deficiencies have been found, peroxisomal problems may exist, AMPK activation is reduced, decreased muscle ATP problems have shown up, and more.
These studies tend to be small, focus on different aspects of the mitochondria, and the results have often not been subject to validation, but the results have consistently pointed to problems in energy production. Still, no consensus exists as to the extent and role of mitochondrial problems in FM. Hopefully, at some point, this subject will be taken seriously and a large, organized effort will be undertaken to understand the role the mitochondria play in FM.
For now, we have another study. The latest one, “The Behavior of Muscle Oxygen Saturation, Oxy and Deoxy Hemoglobin during a Fatigue Test in Fibromyalgia”, comes from a familiar place for fibromyalgia research – Spain.
The study didn’t mess around. Noting that if the mitochondria really are impaired in FM, the authors asserted that that impairment should show up in an exercise test – which, as was noted earlier, has rarely been done in FM. Specifically, since the mitochondria use oxygen for energy, a mitochondrial impairment should show up as reduced oxygen consumption during an exercise test. If the mitochondria aren’t doing well, they simply won’t be able to take up as much oxygen.
If this was chronic fatigue syndrome (ME/CFS), we would probably see a bicycle test, but this being FM, the researchers asked the participants to exercise the biggest muscle in the body – the quadriceps muscle in the thigh – while they monitored energy parameters (oxygen saturation (SmO2), total hemoglobin (THb), deoxygenated hemoglobin (HHb) and oxygenated hemoglobin (O2Hb)) using a portable near-infrared spectroscopy (NIRS) device.
Higher oxygen levels in the muscles of FM patients during exercise meant their mitochondria weren’t taking up as much oxygen (and were producing less energy).
For instance, during exercise, our muscle oxygen saturation should decrease as the oxygen in the muscles is taken up by the mitochondria and converted into energy. Since hemoglobin carries oxygen to the cells, it makes sense that the levels of deoxygenated hemoglobin should increase as the hemoglobin transfer more and more oxygen to the tissues during exercise.
Poorly functioning mitochondria, then, should result in increased oxygen saturation, increased oxygenated hemoglobin, and decreased deoxygenated hemoglobin during exercise. That’s what they found in the FM patients vs the healthy controls – before, during, and after the exercise bout.
The authors concluded “These findings could suggest that people with FM had a significant impairment in the consumption of muscle oxygen.”
The really weird finding, though, was that while these measures changed over time as the exercise progressed in the healthy controls, they remained the same in the FM patients. It was as if their muscles simply didn’t respond to the exercise.
This strange passivity was echoed in an autonomic nervous system exercise study which found that the ANS of FM patients reacted much less than healthy controls did. Since the ANS regulates blood vessel functioning this could result in reduced blood flows (and oxygen) to the muscles.
An even more bizarre finding showed up in a metabolomics ME/CFS study which found an explosion of metabolite changes during and after exercise in the healthy controls – but little evidence of anything happening in the ME/CFS patients (!).
The mitochondrial deficiencies found in FM, thus far, should result in increased fatigue and increased lactate production – both of which have been found in FM (and, of course, ME/CFS). Other FM studies have found more evidence of mitochondrial and muscle problems, including lower levels of phosphocreatine (a high energy reserve in the brain and muscles) and ATP, and dramatic rapid drops in pH in the muscles during exertion – a sign that the aerobic metabolism we rely on for clean energy was quickly getting tapped out.
Some of these studies go way back. Back in 2007, David Katz proposed that the pain in FM is caused by “vasomotor dysregulation (blood vessel problems), and vasoconstriction in muscle, leading to low-level ischemia (hypoperfusion) and its metabolic sequelae”. That study was preceded by a 2004 study which found fewer capillaries, fewer dilated capillaries and reduced peripheral blood flows in FM. That suggested that perhaps the muscles weren’t getting proper blood flows.
Interestingly, Katz proposed that “vasodilatory influences, including physical activity, relieve the pain of FMS by increasing muscle perfusion”. My experience in my case of ME/CFS/FM, which tends more to the FM side of the spectrum, is that that is true – that exercise does temporarily tend to reduce muscle pain – but too much exercise (and it doesn’t take a lot) causes payback.
Add that to recent studies showing problems with the microcirculation and the autonomic nervous system, and you wonder why mitochondrial problems aren’t a bigger thing in FM.
Energy Enhancements Can Help
A rather startling randomized, placebo-controlled trial found that CoQ10 supplementation (300 mg/day) was more effective than Lyrica in reducing pain and anxiety, as well as mitochondrial oxidative stress, and inflammation. Plus, it increased antioxidant levels (glutathione levels superoxide dismutase (SOD)).
Another randomized, double-blind, placebo-controlled trial study found that 300 mg/day CoQ10 produced a reduction in pain, fatigue, and morning tiredness and helped to recover antioxidant enzyme levels as well as mitochondrial productivity and the all-important AMPK activity. Other studies have been done.
The Gist
- Exercise clinical trials now permeate fibromyalgia research and they indicate that moderate exercise is, by and large, helpful. The other side of the coin, though, are muscle and mitochondrial studies that have wracked up a pretty impressive list of problems as well.
- The latest study made a very simple assertion – if mitochondria problems are indeed present in FM, then problems with oxygen delivery should show up as well. The mitochondria – the energy centers of the cells – rely on oxygen to produce energy. If they aren’t working well, then oxygen delivery should drop.
- The Spanish researchers examined the oxygen and hemoglobin levels in FM patients and healthy controls as they exercised their quadriceps muscle. As their mitochondria used up more oxygen, their muscle oxygen levels should drop, and the number of hemoglobin molecules – which carry oxygen to the muscles – should rise, as they pump more and more oxygen into the muscles.
- In a clear sign that their mitochondria weren’t working as well and weren’t taking in as much oxygen as the healthy controls, the FM patients’ levels of muscle tissue oxygen weren’t as depleted, nor did they have as many oxygen-depleted hemoglobin cells as the healthy controls.
- Even more interesting, despite the fact that their muscles had undergone a considerable amount of stress, their oxygen levels, etc. simply didn’t change that much.
- A similar finding regarding the autonomic nervous system showed up in a fibromyalgia exercise study – it simply didn’t respond much. Plus, despite finding that exercise induced massive changes in metabolites in healthy controls, the metabolites in ME/CFS hardly responded at all. It’s as if the proper response to exercise has been shut off.
- Several studies that have found that energy-enhancing supplements such as CoQ10 and acetyl-carnitine may be as helpful as Lyrica and Cymbalta.
- Interestingly, fatty acid problems – which play a key role in energy production – have recently shown up in FM, ME/CFS and long COVID.
- Still, exercise studies have generally been helpful in FM. How to parse those findings, and these, will be the subject of an upcoming blog.
Problems with carnitine metabolism – a key part of energy production involving fatty acids – have also come to the fore in some case reports and studies. Acetyl-carnitine’s analgesic or pain-relieving properties have lead some to suggest it may be helpful in FM. A 2007 study suggested that 1500 mg/day of acetyl-carnitine taken for 10 weeks might be helpful in reducing pain. Similarly, 1500 mg/day acetyl-carnitine was found to be as effective as Cymbalta in reducing pain.
I don’t think anybody believes supplements like these are THE answer to FM or ME/CFS or long COVID. They may help some people but if energy productions play a role in these diseases more refined treatments are clearly needed.
Not Just Fibromyalgia
It’s notable, though, how some of these problems seem to pervade the ME/CFS/FM/long COVID class of illnesses. Fatty acid and carnitine problems have recently come to light in both long COVID and ME/CFS metabolomic studies. A recent long COVID study called for treatments focused on “restoring mitochondrial fat-burning capacity”.
While peroxisomes – the organelles involved in fatty acid metabolism – have recently become a big deal in ME/CFS, it should be noted that peroxisomes were first identified as a possible target in FM three years before they popped up in ME/CFS and that two years ago a peroxisomal enhancer called pioglitazone significantly relieved fatigue, improved muscle performance, reduced inflammatory cytokines and enhanced antioxidant’s activity in an FM mouse model. Clearly more and more study in energy production is needed in these diseases.
A strange yin/yang situation is occurring in FM. On the one hand, studies suggest that energy production is impaired and mitochondrial and muscle problems are present. On the other hand, exercise studies consistently show that exercise can be helpful. Quality of life, physical functioning – even pain levels – have been improved.
An attempt to parse those two findings will be the subject of a future blog.






Thanks Cort for the info you bring us – will start the supplements you mentioned. Never thought my muscle issue was that bad but had muscle pain/spasms after a healed broken femur, knee replacement as it “all works together” manipulation under anesthesia due to muscles not flexing, leg turns black and more stiff from that, and when finally all resolved, have a muscle issue for past couple months that has stopped most rehab. Glad this is now being taken seriously vs 40 years ago when diagnosed and doc simply said nothing can be done as he walked away.
Hi there. Thanks for the information you share on FM/CFS/ME. It’s been really helpful. I was diagnosed with FM in 2005. I’ve had a long love- hate relationship with exercise, believing it to be some kind of key to feeling/being better, whilst being knocked sideways by the consequent flare-ups, crippling muscle pain and other disruptions. But I keep trying to find ways to find a balance. With these findings what are your views on muscle de-conditioning over time in FM? If proper muscle function is disrupted due to poor energy production can it be restored over time with these supplements? Or is it a case of people having to continue managing symptoms as they show up each day against a back drop of gradual physical decline, albeit with some temporary relief? Sounds a bit melodramatic, sorry
Janet you’re not being melodramatic, sarcopenia and osteoporosis are huge concerns for even healthy folks who are aging, but at least they can do something to somewhat counteract it. Just read a short item by Peter Attia about a drug being studied that would be a temporary measure for those who break a hip or such and will be in bed for recovery but it’s still in clinical trials and he’s not holding his breath. He said there is another drug in trials for sarcopenia, but that there’s no substitute for exercise and weight lifting.
Appropriate commentary for me! I was just Dxed with osteoporosis and now my doctor wants to put me on one of those bone altering drugs. Since I have achalasia and cannot take bisphosphonates orally, and my teeth are in a constant state of deterioration–thank you Ehlers-Danlos–the sword of osteonecrosis hangs over my jawbone. What’s a girl going to do?
I was horrified to read the list of side effects for drugs like Reclast, Forteo, Prolia etc. Reclast, what my doctor recommends, has a 43% risk of moderate to severe side effects! There doesn’t seem to be any way to find out if you will be the one to experience them–Russian roulette!
Being incapacitated by fatigue and consequent low exercise levels is so stressing me out! I worry that if I try any of these medications, the joint pain and bone aches I already have will be exacerbated to the point of agony. Is anybody else dealing with this? What do you recommend?
Nancy B I used to go to a TMJ doc who specialized in treatment of jaws after they had necrosis from those drugs. He had pics on the wall and I thought then no way. I do have a suggestion – I had a Dexa 9.5 years ago and it was -1.8 in 2 places (osteopenia) and -2.5 spine. (Borderline osteoporosis.) Broke femur 2.5 years ago, and had not had a Dexa in those 7 years. Was shocked when it came back as no change. A doc had put me on bioidentical hormones after that Dexa but way too much, had bleeding so halved the dose myself so figured was ok. He never checked levels all that time. A year ago asked myPCP to and she wasn’t going to, said it’s a standard dose(and she was speaking of his original dose I’d halved) but talked her into it and estrogen came back 557, way out of range. I questioned it and she says “well of course it’s high, you’re supplementing!” Got another opinion from NP and she said she’s never seen a level so high in someone my age (69) and could fuel cancer so took me off, said I should be 60-100. I plan to get a 3rd opinion but my point to all this is that I bet that high level is what kept my bones from getting worse. Don’t know your age but if older and not taking hormones might want to look into it with a hormone specialist. I’ve never had menopausal symptoms but put on for bones which I read 25% of women are vs uncomfortable menopausal symptoms. I’ve been off a year now so is a concern if my thinking is correct that it was the hormones. I also take stronium which is supposed to help so could be that’s had an effect.
No melodramatic at all. I think you portray well the conundrum of exercise. We all know its good to do that but finding the right balance is tough – and now exericse is being touted kind of as a solution – something everybody should do. I’ll dig more into that and what kinds of exercise appear to work best in FM when I do the exercise studies blog.
I don’t know if supplements improve functionality in general. In some cases I’m sure they do; in others they probably – that is just par for the course though. I’m really interested in the mitochondria and blood flows and muscle functioning in all these disease – I think there’s something there for us – and am really looking forward to seeing how it turns out.
As to deconditioning – I just don’t know. I couldn’t even find criteria for deconditioning – it seems to be a nebulous term. I’m very interested to see how very short duration weight training does as that might be able to restore some muscle without whacking an already problematic aerobic enery production system.
Cort– In looking at the helpfulness of exercise, please consider interoception and, in particular, proprioception. Is it possible that part of the benefit of exercise is that it refreshes the interoceptive self-reading of the body? Rekindles not only the proprioceptors but also the brain’s processing of proprioceptive information? (I’m a Feldenkrais teacher and this method is (98% about proprioception–and it is very gentle.)
I hadn’t thought about that but I would not be surprised.
Acetyl-l-carnitine with riboflavin keep my muscles from cramping. They are used to treat some fatty acid oxidation disorders. I haven’t notice much of a difference with CoQ10. I have ME/CFS but not fibromyalgia.
Chris how much of each do you take?
Having used high dose oral CoQ10 achieving good blood levels many times above the standard upper limit of normal with such supplementation, I saw no symptomatic benefits in terms of muscle pain, sense of energy or venous blood gases in any of my patients over a period of 6 months.
Well darn, John!
I’ve been using coenzyme q10 for a while, and I haven’t observed any differences, so I stopped.
If ME/CFS is a broad spectrum, I’d think FM is even broader as the criteria is sortof wide – and if possible used even less strict than ME – criteria. May I also add clinical burnout or exhaution syndrome? I know that last one is controversial for the ME/CFS community, but I believe it is essential to compare the different diagnoses to each other.
And also to incorporate the knowledge between different kinds of fatigue, different kinds of pain etc. Sometimes I think the ambition to define ME/CFS, despite how necessary it is, also make us missing great chunks of knowledge, both in how to manage and cope, as well as find out whats wrong with us. Of course, you can change ME/CFS with FM in this reasoning 😉
Therefore I think studies like the Systrom lab, these comparisons in this blog and for instance studies of fatigue in general are interesting. I also try, for my own benifit, try to find coping strategies and ways to manage my conditions by reading and listening about other diseases/conditions as MS, neuropathies, fatigue from/during infections, other cronically fatiguing diseases.
It also lessens my internal stigmatizations! 😂 and demystfies ME and makes it less scary. And makes me able to explain to others without sounding weirder than I have to, which probably helps the understanding of ME among others. There I explain ME as a sort of cousin to FM and MS, so I’m glad for this text that gives me even more reason to do so! Thank you Cort!
Great idea IMO to keep an eye on other fatiguing diseases. A blog on the similariities and differences would be wonderful…
I have both Fibromyalgia and ME/CFS so I find it a dilemma. Most FM advice is that exercise helps but ME/CFS advice is usually resting as much as possible. I feel that I need to try to keep my body moving to a certain degree. I am bedbound and elderly but can manage a short shuffle around the bedroom but if I do too much then the dreaded payback gets bad. I can’t seem to get a balance. If I don’t move the pain is unbearable. I feel that I am deteriorating fast and can’t work out what is the best path. Coenzyme q10 doesn’t seem to do anything but I’m only taking a small amount as larger doses made me feel bad. I have tried L Carnitine which seemed to help a bit but then I seemed to get a bad reaction to that. I’m going to try again with that to see if it helps. Maybe every other day may work. Would be interested to hear any success stories with these supplements as I can’t take drugs and much prefer to go down the route of supplementation. Interesting to read that the supplements were working as good as the drugs.
I have had FM for many years. I have been taking Acetyl L Carnitine along with NAC (N Acetyl Cysteine) for several months. As a result, I have more energy, better sleep, less pain, less brain fog and neuro-inflammation and less overall stiffness in the morning. I forgot to take it one day, and the following day the pain and stiffness were so bad I could hardly get out of bed. These supplements seem to be helping me have a better quality of life, and I do not have any negative side effects from them.
Good to hear! NAC did well in a small ME/CFS study.
https://www.healthrising.org/blog/2021/09/09/mitochondrial-enhancers-chronic-fatigue-fibromyalgia-nac-n-acetyl-cysteine/
Please let; a know the dosing on these supps….
My muscles have become lumpy, tight and stringy from this disease. If muscles are damaged in that way by the disease, will exercise help them or hurt them more? In general, muscles tear and then are larger and stronger when that year is repaired. But will my tight, stringy muscles tear more easily? And can they repair themselves without sufficient oxygen?
I’ve been taking mitoq which is 10g of mitoquinol mesylate (not sure what that would equate to as dosage of ubiquinol, for a few years. I definitely noticed it helped my energy levels, I trialled going off it to be sure and I won’t do that again! I’ve also found fasting to be helpful for pain and energy and I wonder if it’s because it increases autophagy (amongst other benefits). I’ve had FM with CFS about 7 years. I’ll be interested to try L-carnitate as well. I’ve more recently been able to add exercise in again after years of severe fatigue but finding a balance has been tricky. I definitely find stationary bike to be the worst for “seizing” up my quads and I felt like I needed full extension exercises like walking to get the blood flowing. So interesting to read this article and find some evidence to back up my anecdotal theories of my own personal journey
Thanks so much for this article. I have ME/CFS. I was a fairly high performing athlete in my younger years. Now, my muscles definitely feel like they are oxygen depleted from low level exertion. I have been under the care of a naturopath for a decade. We have tried lots of avenues and the decline still continues. :(.
I do want to report on the most helpful new strategy for me in the last few months has been increasing nitric oxide in my system through breathing exercises. I am following the work of David Deppler at Breathe Your Truth. I incorporate the breathing exercises into my daily regime just to help me get out of bed etc. And, additionally, when I am out in the world interacting and my symptoms flare, I rev up the breathing practices.
I used to breath more slowly and deeply. Now, I incorporate the breathing exercises like 4 – 7 -8, Sa Ta Na Ma exercise (as recommended by Alzheimer’s association for brain health, feather breathing, alternate nostril breathing. It feels counterintuitive to actually reduce air intake. However, I have to say that it really does help with my muscle recovery and also soothing the aroused vagus nerve.
I am just beginning a course of breath training with David. He has a device called a capnotrainer that helps measure CO2 levels and helps you train yourself to breath at the pace and interval that delivers the most oxygen to your muscles. If I could just get SOME exercise without the blowback, I know it would help. Wish me luck!
Good luck! And thanks for sharing. 🙂
I have good success with a mixture of citrulline and norvaline or else a mixture of beet root powder and vitamin C. Both combinations increase nitric oxide production through different pathways
This is so old school. Why is there no mention of the HO-CO pathway? Both FM and CFS are caused by carbon monoxide poisoning hangovers, when levels of CO in tissues are still higher than normal, impairing mitochondria and muscles via binding to Ca3 and myoglobin, respectively.
The symptoms of falling CO are reversed by boosting CO, which is what CoQ10, Resveratrol, Melatonin, Vit C, and Quercetin do. They all boost Heme Oxygenase-1, which is the primary source of endogenous CO in mammals.
The CO hangover is biomarked by chronically high CO in exhaled breath and chronically low body temp.
Note also that studies that report no change in oxygen levels among exercising FM patients are using standard pulse oximeters that can’t distinguish O2Hb from COHb.
If they used Masimo Rad57 or similar devices that can distinguish them, they would see COHb is going up in CFS and FM patients during exercise while their O2Hb is going down.
Interesting post, thank you! My theory is that fibromyalgia is a psychophysiologic disorder, in which the brain’s control of skeletal muscle is dysregulated in the following two ways: (1) higher baseline/involuntary muscle tone, which leads to the pain and stiffness, and increased oxygen consumption, and (2) weakened voluntary muscle action, due to diminished mind-muscle connection. There are multiple research studies demonstrating anormal motor cortex function in fibromyalgia and other chronic pain states. If an exercise regimen is progressed slowly enough over time, one can retrain the brain and nervous system, while also giving the microcirculation and metabolic systems of the muscle tissue time to adapt. In contrast, if too much is done before the mind and body are reconditioned, it can lead to a painful setback. This gradual technique worked for me, and I was able to fully rehabilitate myself from fibromyalgia. I’ve just started using this technique on patients with one good result so far. I would also like to highlight that in my opinion the leading theory on the underlying cause of fibromyalgia is that the nervous system becomes dysregulated due to chronic stressors, whether due to circumstances, personality traits, and/or repressed emotions. This builds off of related work by Dr. John Sarno, and later Howard Schubiner and others, and is also the basis for Pain Reprocessing Therapy, an evidence-based technique for low back pain which in my experience is also applicable to fibromyalgia.
Thanks Theodore Armstrong for your summary. What you write here resonates for me. I have had fatigue/energy production issues since I was young. (I am now 54 years old.). In the early years, I would push through the fatigue for some pretty high spectacular physical feats and then experience huge energy drops. Over the years, the energy highs and lows narrowed to where walking to the car became an energy drain. I have been working with a breath coach/physical therapist, David Deppler, and together we have been able to re-train me to much greater functioning. (from 3,000 steps a day to 10,000- 11,000 average) We utilize the breath through nasal and other restricted breathing, increasing CO2 in the blood, to help retrain the brain and muscle connection. This has combined with counseling and other supportive therapies, to help me limit chronic stressors and gain the space for the retraining to happen. It is a very long road. I am hopeful.
Sounds like you’re on the right track! Feel free to contact me directly if you have additional questions: mindbodywellnessmd@gmail.com