Basic Stuff
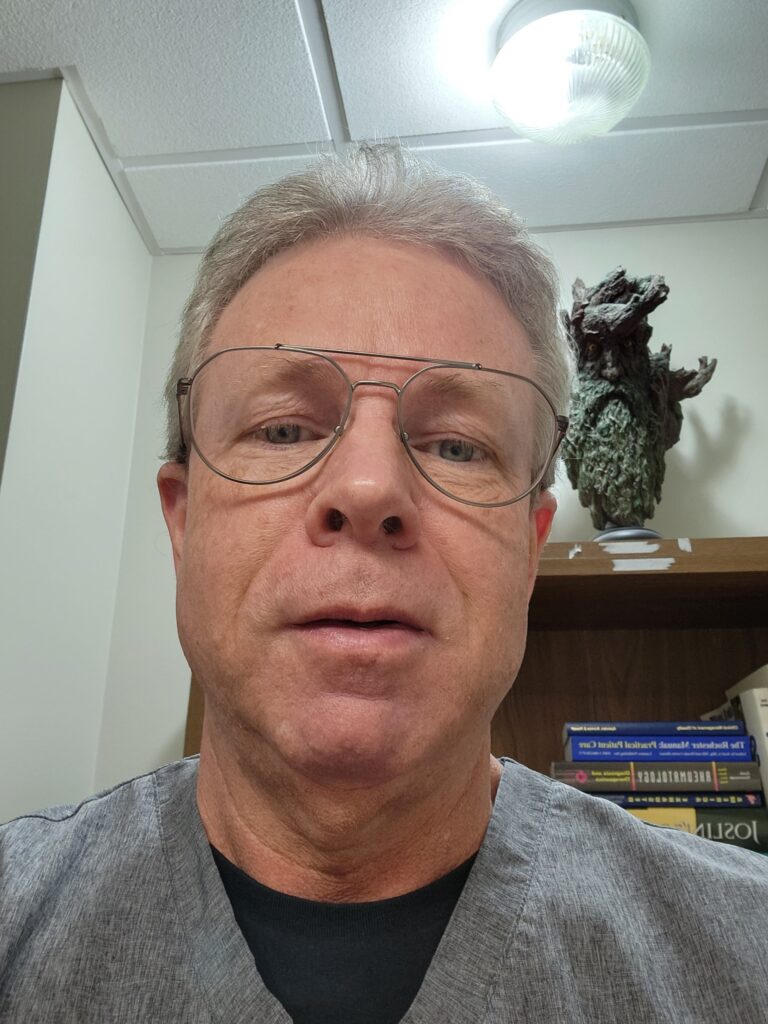
- Name: Bryan
- Country: United States
- State: Alabama
- City: Huntsville
- Gender: Male
- Age: 62
- Education: Ph.D Degree
- Primary Illness: ME/CFS
- Diagnosis:
- Chronic Fatigue Syndrome (ME/CFS)
- Neurally mediated hypotension
- Irritable bowel syndrome
- Migraine
- Year Illness Began: 2001
Functioning Interrupted
Work Interrupted
- Former Occupation: Family Physician
- Job Responsibilities at Former Occupation:
Working in a busy family medicine group, seeing 30-40 patients daily. Working 50-60 hours/week as I was still following my hospitalized patients at that time.
- Years of Work Lost: 10
- Current Work Status: On disability
Income Interrupted
- Yearly Income Before Becoming Ill:
$250,000
- Yearly Income From Disability:
$80,000
-
Minimum Current Annual Income Loss:
$344,877
- Total Projected Economic Losses For Years Not Worked:
$3,660,079
Other Interruptions
- This illness has severely impacted my ability to financially prepare for retirement
- I reduced my work hours
- I took on jobs with less responsibilities than I otherwise would have
- I lost my house or had to move to a smaller dwelling
- I have been unable to or found it very difficult to date
- I believe this illness contributed significantly to a divorce or loss of an important relationship
Most Impactful Loss
The loss of my ability to have the interactive relationships with my children (and now grandchildren) that I had prior to my illness.
The loss of the ability to develop a meaningful relationship with my anticipated soulmate.
My Story
Prior to my illness, I was a very active, very successful member of my community. I was seeing 30-40 patients per day in my busy medical practice, participating actively in my children's daily activities, and playing high-intensity sports for hours at a time. I did happen to be under an enormous amount of stress at the time, both personally and professionally. (I remember noting that I checked the boxes for 9 out of the 10 most common stressful events in life which I had all at once at that time)
During that period, I developed a flu-like illness, which later I discovered must have been EBV (Mono). I had typically recovered from illnesses without difficulty, but this time was different. The fever resolved, but not the extreme fatigue, the body aches, the lymph nodes that popped up everywhere. Within a few weeks, I was struggling to see half the number of patients that I would normally be able to see with energy to spare. My medical knowledge led me to thinking of Hodgkins Lymphoma, and the Oncologist I visited agreed. But after Scans from head to toe, multiple lab tests, and lymph node biopsies, no disease was found. I spent the next few weeks seeing every specialist looking for answers, but finding none. Finally, a Rheumatologist friend, who's wife happened to have recently passed away from complications of CFS, suggested the diagnosis. At that time in 2002, very few physicians, including myself, knew about CFS. In my four years of medical school and three years of Residency training, I never once heard anyone mention Chronic Fatigue Syndrome. But as I looked at the list of symptoms, they matched exactly to what I was experiencing. For better or worse, I had my diagnosis.
The next two years were spent in acceptance of my lost life. My ability to see enough patients to produce my salary dwindled. My physical activity level decreased and was eventually lost as my body could no longer perform what my brain expected. I finally accepted that my life as I knew it was over when I experienced my first Crash and the following PEM during a moving day to our new office location. I had collapsed to my floor after pushing beyond my new limits. My brain had reached the now familiar "Brain Fog" level of cognitive dysfunction. My other physician partners rolled their eyes at me as I tried to describe the symptoms of my illness...they didn't believe in CFS. I swallowed my pride and began an application for Disability. Of course, the Psychiatrist assigned to my case reported that I was just depressed. The Internal Medicine "Specialist" assigned to my case told me that he didn't believe in CFS. His flippant attitude actually led to my approval by default, so I thank you Dr Incompetent!
Weeks have turned to months. Months turned to years. And now two Decades later, I've forgotten how my old life felt. I've been able to continue to see a limited number of patients working a few hours a day and taking Wednesdays along with Weekends as my rest days. After a couple of failed attempts at relationships, I've accepted that this illness will most likely prevent me from finding the wife that I had once planned on growing old(er) with. My now grown children understand that I have this disease, but I'm not sure that they realize how much ME/CFS actually affects my daily activity and my inability to interact with them as much as I would prefer.
Medically, my ME/CFS has always been connected to that initial EBV exposure. The virus has reactivated at least twice a year over the course of my illness. Interestingly, my EBV reactivated in the early days of Covid and has yet to return to negative. (Has my EBV stayed active to protect itself (and me) from this other predatory virus?) As far as treatment of my ME/CFS, I have stumbled upon some things that have helped, and more things that have failed, just like most of us. And I keep looking for the next new miracle cure. I've now lost a third of my life to this disease, and I'll never get that time back.
I do offer my apologies for my fellow medical professionals who have, for the most part, failed in their recognition and treatment of these chronic diseases. Most of the problem goes back to just the lack of education and awareness. Obviously Covid has opened a lot of eyes to this field of post-viral/pathogen related diseases. And Myalgic Encephalomyelitis has finally been included in most medical textbooks as a distinct disease as of 2022. Hopefully all of the research money finally being thrown in our general direction will start to pay off with some benefits in the future.





Thanks so much for telling your story, Bryan! It’s particularly valuable for us as a community when doctors – particularly formerly very fit doctors – are willing to tell their stories. Good luck with everything!
Story to be continued. Thanks for the forum to be able to share our stories.
Looking forward to it. Hopefully, it will have a happy turn. 🙂
Bryan, I can relate to your story as I am the same age. Thank you for sharing your story. I hope things improve for you 🙂
Cort, thank you as always for the incredible work you do and also for this series. It’s been interesting to read the stories of others in our community.
Thanks, Elle! If you’re up to it – love to get your story 🙂
Thanks, but my story is pretty typical – girl meets EBV, EBV morphs into CFS+POTS (the latter was unknown at the time), girl quits job (computer programming) and lives a very different life thereafter.
Yes, that does sound familiar. If we get enough stories we hope to publish a statistical analysis of them – so the more the better. Plus, I don’t know if have an EBV story yet or not…hmmm…(We just had our first flu vaccine story!)
Doc, Thanks for sharing your story. It’s a familiar one that all too many of us share, though reading about your own medical colleagues’ attitude was a disheartening twist. Your apology on behalf of people like that was well-intended and thoughtful, but the profession as a whole owes you (and the rest of us) an apology.
It makes me wonder again why it is so many doctors seem to disbelieve their patients and whether it’s due to their training, a lack of critical thinking skills, a lack of empathy, etc. I’ve had CFS/POTS for 30 years and was very lucky to have Dr Lapp as my physician for several years until he retired, but I’ve had some real clunkers too along the way. Still do, except for my great POTS doc.
About EBV reactivation – I’ve reactivated many times. I found Dr Naviaux’ research on CFS regarding HHV-6 Reactivation & Mito Fragmentation and how that may have a strong antiviral effect on viruses interesting. Personally, I don’t remember having a cold or flu in the past 20+ years, so something protective (and tiring) is probably going on.
As for relationships, yes, absolutely, we face huge challenges in finding and keeping them. It’s tough for CFS people our age and it’s also hard for those just starting out in the world, like the young POTS patients I know. There’s no easy answer to this for any of us but I still say don’t give up.
Hi.
I live in Tennessee and can relate to your story. I have ME/CFS but have not been officially diagnosed in TN because Drs haven’t even heard of it here, or they don’t believe in it. I was unoffically diagnosed from a rare disease expert in DC. Unfortunately, they can’t treat me in TN.
I understand your frustration with “dating” with this disease. I came to accept the loss of that dream years ago.
I wish you the best. Thankyou for sharing your story. I pray they find a cure one day.
Bryan, thank you for sharing your story, much of which resonates with me – not least because I’m thinking that getting glandular fever (EBV) at fourteen years old started me on this long and undulating path. I’m still trying to figure this out at 59. I wish you well and hope you manage to claw back some of the life this horrible disease has stolen from you 🌈
Hi Bryan: Your story was so encouraging to me. I am sorry for your many years of lost life due to the illness, but am glad you have been able to recover somewhat, and treat patients again. I am sorry that this disease has come between you and long term relationships. I can relate to that as well, as I have had to accept a separation.
Your description of doctor’s take on the illness sounds so familiar! I am in Canada, but its the same up here.