


If you’re going to have a conference you might as well have it in a nice place 🙂
It took about three years but the first major international conference on long COVID – the “Keystone Long COVID and Post Acute Sequalae of SARS CoV 2 (PASC): Pathogenesis and Treatment” conference recently took place in Santa Fe, New Mexico at the El Dorado Hotel. Health Rising was there, kind of. (We got the online version).
For people with chronic fatigue syndrome (ME/CFS) many of the faces are new. We know of Avindra Nath and David Systrom but otherwise, the conference featured researchers new to the post-infectious field, some of whom have transitioned heavily into the long-COVID space such as Akiko Iwasaki, Tim Henrich, Michael Peluso, and Stephen Deeks.
We got glimpses at studies examining some ongoing long-COVID cohorts and initiatives such as the Outsmart Cohort, Tulanes ClinSeqSer Cohort, the Mount Sinai Yale Cohort, the ADAPT cohort, the LIINC cohort, and the German COVID-19 OMICS Initiative. We also had several mouse studies – something we rarely see in ME/CFS.
It was good to see Dr. Gary Gibbons, the director of the Heart, Lung, and Blood Institute (NHLBI) at the NIH and a leader of the NIH’s RECOVER Initiative, start things off. Gibbons made sense as COVID-19 affects the cardiovascular system. On the other hand, until now, NHLBI has shown zero interest in ME/CFS or post-viral illnesses. Maybe that will be changing.
Homeless at the NIH
Gibbons noted the many different institutes working together on COVID that never have worked before. That’s not surprising given the complex nature of post-infectious illnesses and it’s the need to do cross-institute work that has led the Solve ME Initiative to begin a long-term effort to create a new post-infectious disease institute. Indeed, ME/CFS is still homeless at the NIH largely because it, like long COVID, doesn’t fit well in any one Institute.

Dr. Stephen Deeks – one of the organizers of the event – called the RECOVER Initiative “a great success”.
The Trans-NIH Working Group that guides ME/CFS research at the NIH is a unique cross-institute effort that has failed to receive much help, in large part, because it’s not associated with any one Institute. Hopefully, long COVID will help force the issue and create an entity that works for these complex, multi-system disorders.
Dr. Stephen Deeks – a respected researcher with a long track record who is a part of the RECOVER effort – underscored how new the long-COVID effort is by noting how many of the speakers had never met each other until now. He called RECOVER “a great success“! Indeed, despite the flack it’s received over the past year or two – the RECOVER Initiative came in for nothing but praise from many of the speakers – suggesting that we need to give it more time.
Yale’s Outsmart Long Cohort
The Outsmart Cohort moved quickly to collect samples from 70 people – most of whom were not hospitalized – within 48 hours of becoming ill and then a month later. Then they followed them for 24 months.
Note the requirement for inclusion – at least 1 symptom remaining for more than 90 days. Another study found that if you had one symptom, you probably had at least a few more, but we don’t know how many of the participants met the criteria for ME/CFS or fibromyalgia, POTS or IBS, for that matter.
People who took longer to clear the virus from the respiratory tract – and were presumably more symptomatic – tended to have brain fog and muscle pain. This makes sense with the Dubbo study finding in ME/CFS that the more symptomatic you were, the more likely you were to come down with a post-infectious fatigue syndrome.
A latent class analysis of long-term symptoms identified 3 groups characterized by:
- Anxiety, headache, weakness
- Body aches, joint pain
- Brain fog, memory problems, insomnia.
Note that fatigue is not mentioned – perhaps because everyone had fatigue. Post-exertional malaise was clearly not on this group’s radar.
They did an extensive immunological evaluation (T-cell panel, myeloid, and B-cell panel) combined with markers of metabolic programming (fatty acid oxidation, glycolysis; TOM-20 – oxidative phosphorylation, mitochondrial mass)
They found increased numbers of myeloid-derived suppressor cells (also found in chronic infection, cancer, and obesity) in the anxiety, headache, and weakness group. On the other hand, they found increased levels of a lectin receptor (LOX-1) – which is also a suppressor (it suppresses T-cell proliferation) but is also associated with the blood vessels (endothelial cells, platelets, macrophages, smooth muscle cells). Either way, the immune system appeared to be trying to tamp down its response.
Granulocytic neutrophilic MDSC cells are similar to monocytes – which have gotten a lot of attention. People with more of these cells experience brain fog, memory problems, and insomnia. Interestingly, people with high CD20+, CD27-memory B-cells – and headache, anxiety weakness – also tend to have high numbers of PMN MDSC cells, as well as eotaxin-3 and IFN (1 and 3).
They don’t know what’s causing these unusual immune configurations to pop up, and are investigating more.
Thinking Bigger: the Immune Hormone Mix
Akiko Iwasaki – “Thinking Beyond the Spike”
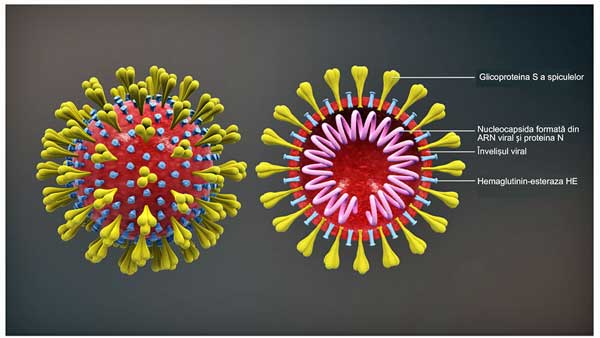
A great deal of focus is being concentrated on the spike protein – the yellow protuberances seen in the image – but Akiko Iwasaki – citing diseases like ME/CFS – feels we need to move beyond the spike.
Akiko Iwasaki did a sort of immunological overview, which didn’t appear to provide anything new but was notable in a sea of long-COVID talks for her emphasis that long COVID is one of many post-acute infection syndromes. She even mentioned a post-infectious disease paper she cowrote with Mady Hornig and an ME/CFS patient.
She said, “We need to think beyond the spike!” and thank god for that. So much attention is focused on the spike protein of the coronavirus – the part of the virus that sticks out and gains entry into the cell. Yes, the spike protein is clearly important, but Akiko reminded everyone that many other post-infectious illnesses exist that are not triggered by the coronavirus – and cannot be explained by the spike.
Health Rising covered her massive, 273-person “Distinguishing features of Long COVID identified through immune profiling” study in preprint form about a year ago. That paper – which set a high standard that, unfortunately, has rarely been met since then – made it to the big time. It was published in one of the most widely read scientific journals in the world – Nature – a couple of days ago.
The study found a number of themes – high levels of monocytes, dendritic cells, activated B-cells, exhausted T-cells, high antibody responses against EBV, and then there was the shocker – the main distinguishing factor – low cortisol. Speaking of hormones, the study also found low testosterone in females and reduced estradiol in males. The study’s rather unique combination of immune and hormonal factors allowed it to differentiate between people with and without long COVID with remarkable accuracy (96 %).
CNN reported that the cortisol finding “was one of the most exciting to the researchers because it makes some biological sense.” Akiko Iwasaki said, “When you have low levels of cortisol, you will get tiredness, nausea, vomiting, weight loss, weakness and pain. So lower levels of cortisol could be contributing to the symptoms.”
At the conference, Iwasaki pointed a finger at the HPA axis, and thyroid and female hormones – all of which have shown up in ME/CFS but which, aside from this paper, have pretty much been ignored in the rush to assess immune functioning in long COVID.
The few times the HPA axis has been assessed in long COVID, problems have shown up. A Japanese study found lower levels of cortisol, and free thyroxin (FT4). Another study found evidence of impaired pituitary functioning, but that’s pretty much it on assessing HPA axis functioning in long COVID. To anyone who’s followed ME/CFS research, the absence of HPA axis and hormonal research is pretty astonishing.
The HPA axis and cortisol have been news in ME/CFS for a long time yet have been virtually ignored in long COVID. Akiko Iwasaki’s study, however, suggested that they may play a critical role.
A review paper, “Protracted stress-induced hypocortisolemia may account for the clinical and immune manifestations of Long COVID“, did, however, pick up on Iwasaki’s findings and expanded on them. It reported – rather astonishingly – that Iwasaki’s study found that “the plasma cortisol levels in patients with Long COVID were almost half of those found in matched controls independently of age, sex, sample collection time, and body mass index”, and noted that machine learning tools found that “cortisol levels alone were the most significant predictor for Long COVID classification“.
The authors believe the HPA axis was first activated by the infection, but then suppressed, and that this suppression results in immune dysregulation and the “expression of sickness syndrome manifestations”; i.e. the “sickness behavior” we have heard so much about. They posited that whether someone comes down with an ME/CFS-like condition in part depends on how impaired their cortisol response becomes.
The review paper also reported that the three major findings of “low cortisol levels, T-cell exhaustion and augmented reactivity to Epstein-Barr virus has been also observed in patients with myalgic encephalomyelitis/chronic fatigue (ME/CFS) syndrome”.
That simply confirms what patients, doctors, and researchers in the ME/CFS know very well – that these are complex diseases that require a multi-systemic approach. We need big, multidimensional studies like the Yale study in order to tease out what’s going on. We’re not getting a lot of them. We also need researchers like Akiko Iwasaki who’ve taken the time to check out ME/CFS findings and apply them. They seem to be in fairly short supply!
David Putrino MD, who is right in the thick of things and was part of the study, stated, “There is no ‘silver bullet’ for treating long COVID, because it is an illness that infiltrates complex systems such as the immune and hormonal regulation. Complex illnesses require complex treatment solutions and we need more rapid research to better understand long COVID and discover new and promising therapies.”…Thank you!
Julio Silva – Yale – Testosterone is a key differentiator of sex-specific immune profiles and symptomology in long COVID
Iwasaki’s group appears to have jumped on the hormone findings as another Yale researcher dug deep into them. Silva reported that testosterone was lower in females and estradiol was lower in males with long COVID. This time, the top predictor of long Covid was lower testosterone.
That’s pretty interesting given that Hilary White has been using testosterone to treat fibromyalgia in women for quite some time, and estradiol is connected to testosterone and plays a role in pain inhibition.
Differences in immune functioning were found between males and females. Females had significantly higher NK cell levels, produced more cytokines, and displayed higher reactivity to EBV. Males displayed more dysregulated monocytes and dendritic cells. Both had low cortisol.
The Viral Persistence Talks
Viral persistence – the idea that the virus (or, more likely, pieces of the virus) is persisting in the body and triggering an immune reaction – is all the rage. There’s certainly now plenty of evidence that pieces of the coronavirus are persisting in people with long COVID. Whether they are causing long COVID is another question.
Michael Peluso UCSF

People with higher antigen levels; i.e. higher levels of viral proteins – were worse off over time. A correlation appeared to be present between levels of the spike and nucleocapsid proteins and gut and musculoskeletal symptoms. Plus, coronavirus spike RNA (genetic material) was found in gut biopsy up to two years after the infection. Interestingly, given the interest in connective tissues in these diseases, the spike protein was always found in the connective tissue layer but never in the epithelial tissues that line the gut.
However…not everyone with long COVID was found to have coronavirus antigens (proteins) in their blood, and it was possible that some people had simply been re-infected again.
Are they triggering an inflammatory or autoimmune response that’s causing long COVID, or are they just hanging around? Avindra Nath has pointed out that we all carry viruses in our bodies, most of which do no harm.
Answering the viral persistence question is pretty straightforward – remove the virus – and see if the symptoms improve. If the patient recovers, you have your answer, and antiviral studies of Paxlovid are underway. (Time will tell how effective it is in removing the virus and pieces of the virus. The one report I saw did not find Paxlovid effective with long COVID, but larger studies are underway.)
The 30-person Outsmarting Long COVID Monoclonal Antibody Trial
There is another way, though. In yet another Peluso/Deeks/Henrich study from the very active and creative UCSF LIINC group – the 30-person Outsmarting Long COVID study – is using an antiCOVID monoclonal antibody called AER002. Unlike antivirals, which attempt to stop a virus from replicating or infecting other cells – but don’t kill it – monoclonal antibodies can actually clear infected cells from the body. The study is supported by the PolyBio Research Foundation.
Peluso’s group is also doing gut biopsies, and they hope to check out cervical lymph nodes. Peluso said a good biomarker would be completely transformative. It was a good biomarker that jumpstarted HIV research and quickly led to good treatments. Speaking of biomarkers…
Ella Warburg – Harvard – “Uncovering the link between antigen persistence and post-acute sequelae”
Ella Warburg used assays with high sensitivity to three coronavirus antigens in RECOVER and other cohorts in an attempt to find a biomarker. She indeed found high SARS-CoV-2 antigen levels over time, and was able to correlate symptoms with the presence of the antigen.
The implications of the viral persistence hypothesis for ME/CFS are unclear. First, you’d have to identify the source of the immune activation – something that no one has yet been able to do. Of course, there is the Epstein-Barr virus (EBV) connection, but as yet we lack good antivirals for that virus. One would hope, though, that a positive viral persistence result would spur more interest in developing better drugs.
Choutka – Identification of elevated and altered humoral responses to EBV in long COVID
Mount Sinai Yale MY-LC cohort – Iwasaki group again… One study asked whether people with long COVID had been exposed – prior to long COVID – to different pathogens than people who recovered from COVID-19. Something called “original antigenic sin” can occur when our immune systems target a new infection with an old and not very effective immune response against a prior infection.
People with long COVID had similar exposures to common pathogens, as did the healthy controls, but the elevated antibody binding to EBV and varicella zoster virus found in the long-COVID patients suggested that their immune system was reacting more strongly to these herpes viruses than the immune systems of those who recovered.
While they did not find evidence of EBV in the blood, or reactivation of IgM antibodies, they did find that one increased EBV antibody was correlated strongly with specific activated T-cells and increased cytokines (IL-4; IL-6 – gp42) levels. This seemed like a nice package of immune activation and they will surely follow up on that.
Finally! The German COVID-19 OMICS Initiative Targets ME/CFS-like Long COVID
Next came something very different and welcome! While ME/CFS has been mentioned a bit, nobody has actually analyzed an ME/CFS long-COVID subset. Instead, they’ve looked at general long-COVID groups (mostly not hospitalized, to be sure), which may or may not resemble ME/CFS. Even if they do resemble ME/CFS, they might have the full package. This group did.
This study, done in collaboration with Carmen Scheibenbogen’s Charite group, required that the participants meet the Canadian Consensus Criteria for ME/CFS.
The findings from the 60-patient study were interesting indeed. Up popped the innate Immune system – and monocytes! Monocytes have suddenly gotten really interesting in both ME/CFS and long COVID. While the alterations in the gene expression of the major immune cells were found, the most “striking” changes were found in the monocytes. Intrigued by that finding, they really dug in and subsetted the monocytes into their different states and stages of activation.
They then did the same with natural killer cells (NK), a major emphasis in ME/CFS research, and found evidence of increased inflammatory subtypes (cytotoxicity/ activation).
They also found increased levels of CD16+ T-cells, which can damage the endothelial cells lining the blood vessels, and noted that Carmen Scheibenbogen found markers of endothelial damage in both ME/CFS and long COVID.
All in all, it was good to see quite an immune overlap between ME/CFS and long COVID once they focused on the ME/CFS-like group of long COVID.
Digging Deep…
What came next, though, was even more interesting. While it doesn’t break any new ground in long COVID or ME/CFS, the next study by this group demonstrates how deeply a research team can dig when it has the resources.
We saw this with the recent WASF3 study where an NIH team took a single finding from an ME/CFS patient – kept exploring it – and uncovered a potentially groundbreaking mitochondrial finding which they are already attempting to mount a clinical trial for. That study shows that given enough interest and resources, things can happen very quickly!
The question was why some severely ill COVID-19 patients benefited from dexamethasone – an immune suppressant – while others didn’t. They found that dexamethasone mainly altered the expression of monocytes (there they are again…) as well as B cells and CD4 T-cells.
The researchers were surprised to find that only a specific subset of monocytes responded to dexamethasone. When they did respond, though, they downregulated alarmin genes that raise the alarm in the immune system.
In the people who died, dexamethasone failed to downregulate that specific subset of monocytes and failed to downregulate their alarmins. An epigenetic analysis found the same thing; their monocytes remained in an epigenetic pro-inflammatory state.
This study demonstrates that even a small subset of an immune cell type can have a very powerful impact. This group is involved in 6 large studies, some of which are focusing on long COVID-related ME/CFS; one of them – a national clinical study group led by Charite – contains 1,000 patients…Nice!
Australian ADAPT Cohort Looks for Immune Dysregulation and Finds It Doesn’t Tell the Whole Story
THE GIST
- Day one of the first international conference on Long COVID suggested:
- Pieces of the virus appear to be persisting for several years in long-COVID and perhaps in recovered patients. It’s not clear, though, that they are causing long COVID. We should know more about that in the not-too-distant future as numerous trials are underway that are attempting to wipe out the virus in long COVID.
- Multidimensional studies that include both the immune system and hormones – are exceedingly rare in long COVID – but appear to be more effective than studies that focus entirely on the immune system. The long COVID field might want to take a note from the ME/CFS field and check out the HPA axis and cortisol more.
- Monocytes – a virtually unexplored area of focus in ME/CFS until quite recently – are showing up big time in both ME/CFS and long COVID. The only study to assess long COVID patients who met the criteria (CCC) for ME/CFS found “striking” changes in monocytes.
- The focus on the spike protein that infects cells is understandable in long COVID but given the similarities between long COVID and ME/CFS and other post-infectious diseases which do not feature the coronavirus, researchers need to “go beyond the spike” and look deeper.
- Small parts of the immune system -such as monocyte subsets – that might have been missed in ME/CFS or long COVID could have major implications for the diseases – and if, found, could move the field forward quickly.
- Most immune dysregulations that show up say 8 months later in long COVID disappeared two years later even in people for whom long COVID persisted.
- Instead of smushing them together in one study, the long COVID field needs to differentiate the different types of long COVID present. The RECOVER Initiative could make a big impact here.
- Despite the bad press that the NIH’s RECOVER Long COVID Initiative has received it got excellent reviews from several presenters. Let’s not count RECOVER out just yet.
The study was particularly interesting in what it did not find. While it found altered levels of antibodies to COVID-19, B-cell response, exhausted T-cells, monocytes, and cytokines over the first 8 months or so, all of those issues resolved over two years – yet long COVID remained. (Some cytotoxic T-cell activation was still present.)
An analysis that used machine learning to predict which participants still had long COVID at 8 months plucked out some immune factors (IFN-B, Pentaxin-3, IFN-y, IL-6). Note, though, that the assessment was only 80% accurate at identifying who had long COVID. Compare that to the 96% accuracy in the Iwasaki study which added hormones to the immune mix and it seems pretty clear that immune analyses by themselves are probably not going to do it.
The one really interesting finding, though, again involved, yes, monocytes. CD4 monocytes were still more activated in the long-COVID patients at 24 months.
Takeaways
While the first day of the Keystone long-COVID conference suggested a couple of things, it’s pretty clear that pieces of the virus have persisted for several years in long-COVID and perhaps in recovered patients. It’s not clear, though, that the virus is causing long COVID. We should know more about that in the not-too-distant future as numerous trials are underway that are attempting to wipe out the virus in long COVID.
Multidimensional studies that include both the immune system and hormones appear to be more effective (and long-COVID researchers might want to catch up on their ME/CFS research). Monocytes – a virtually unexplored area of focus in ME/CFS until quite recently – are showing up more and more. Small parts of the immune system that might have been missed in ME/CFS or long COVID could have major implications for the diseases.
Particularly from the ME/CFS perspective, but also from the long-COVID perspective, we desperately need to differentiate the different types of long COVID found. The fact that several different types of long COVID are probably being smushed together in most of these studies must surely undercut their effectiveness. A general approach was understandable in the beginning, but three years in, one would hope studies would start focusing on subsets. This is where RECOVER – which was praised several times – on the first day – could make a big difference.
Like Reading long Conference Blogs? (Another one is coming up). If so, Please Support Health Rising and Keep the Information Flowing






I think it is important to divide long covid patients into subgroups. LC vaccinated, LC unvaccinated, LC vaccinated who have had the disease and which type of corona, LC unvaccinated who have had this disease which type of corona. The fact that spike protein is still found after a year is in line with studies in vaccinated people. These are much more exposed to the number of spikes than unvaccinated people. The nano particles are found in various organs after vaccination. Which causes an inflammatory response. Unvaccinated people see the entire virus passing by, which provides better protection in the event of reinfection. All this produces a different immune response. I wonder if researchers are also investigating these kinds of complex and different immune responses.
Hi Gijs, would you have a link for “spike protein is still found after a year (…) in (…) studies in vaccinated people”? Thank you!
https://pubmed.ncbi.nlm.nih.gov/34654691/
Here is one study spike protein more than 4 months
Active spike protein produced in adipose tissue
Clustering around capillary endothelium
(Biopsy from living patient, 8 months post vaccine)
http://docs.shortxxvids.com/burkhardt_analysis.html
Thanks for this link, too!
Thank you!
It seems in this study the spike protein was found bound to exosomes and if I understand correctly, this is thought to be a newly discovered mechanism playing a role in the production of Covid antibodies, with the spike-carrying exosomes decreasing over time but still present 4 months in. (…By the way, I don’t think it’s a good idea for the authors to use unexplained abbreviations in a study about this topic).
So maybe it’s even more complicated depending on where the spike is attached – for example, some virus protein binding to receptors where it does not belong (the premise of experimental treatment #TheNicotineTest) would not be good, but I can’t tell if the binding to exosomes might be a much more harmless thing useful for immunization? As spike-carrying exosomes decrease over time, some people might clear it out of the body, but could there be some people where the spike originally carried by exosomes ends up somewhere else in the body?
Questions I hope science will figure out over time. I find this interesting because of some post-Vac on top of pre-existing ME/CFS.
They are looking at vaccination – the problem is that most people – 85% are vaccinated. I imagine we will see more on this.
“Unvaccinated people see the entire virus passing by, which provides better protection in the event of reinfection.”
https://www.cdc.gov/mmwr/volumes/70/wr/mm7032e1.htm
“Among Kentucky residents infected with SARS-CoV-2 in 2020, vaccination status of those reinfected during May–June 2021 was compared with that of residents who were not reinfected. In this case-control study, being unvaccinated was associated with 2.34 times the odds of reinfection compared with being fully vaccinated.”
2023 study
Besides its role in preventing severe acute respiratory syndrome coronavirus infection, vaccination reduces the rate of symptomatic reinfection and increases the reinfection interval; thus, it is necessary to be vaccinated even after a previous infection.
https://pubmed.ncbi.nlm.nih.gov/37766086/
2023 study
In these data, vaccination history was significantly related to reduced COVID-19 reinfection and severe progression, and scheduled vaccinations were important even with a history of infection.
https://pubmed.ncbi.nlm.nih.gov/37644683/
2023 study
The reinfection rate for those who had a booster vaccination was 11.4% (95% CI: 9.2-13.7), which was significantly lower than that for those with an incomplete vaccination series (15.2%, 95% CI: 12.3-18.1) (adjusted odds ratio [aOR]: 0.579; 95% CI: 0.412-0.813).
https://pubmed.ncbi.nlm.nih.gov/37514962/
onker LM, Swank Z, Bartsch YC, Burns MD, Kane A, Boribong BP, Davis JP, Loiselle M, Novak T, Senussi Y, Cheng CA, Burgess E, Edlow AG, Chou J, Dionne A, Balaguru D, Lahoud-Rahme M, Arditi M, Julg B, Randolph AG, Alter G, Fasano A, Walt DR. Circulating Spike Protein Detected in Post-COVID-19 mRNA Vaccine Myocarditis. Circulation. 2023 Jan 4. doi: 10.1161/CIRCULATIONAHA.122.061025. Epub ahead of print. PMID: 36597886.
Ling RR, Ramanathan K, Tan FL, Tai BC, Somani J, Fisher D, MacLaren G. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med. 2022 Jul;10(7):679-688. doi: 10.1016/S2213-2600(22)00059-5. Epub 2022 Apr 11. Erratum in: Lancet Respir Med. 2022 May 10;: PMID: 35421376; PMCID: PMC9000914.
Avolio E, Carrabba M, Milligan R, Kavanagh Williamson M, Beltrami AP, Gupta K, Elvers KT, Gamez M, Foster RR, Gillespie K, Hamilton F, Arnold D, Berger I, Davidson AD, Hill D, Caputo M, Madeddu P. The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: a potential non-infective mechanism of COVID-19 microvascular disease. Clin Sci (Lond). 2021 Dec 22;135(24):2667-2689. doi: 10.1042/CS20210735. PMID: 34807265; PMCID: PMC8674568.
Lei Y, Zhang J, Schiavon CR, He M, Chen L, Shen H, Zhang Y, Yin Q, Cho Y, Andrade L, Shadel GS, Hepokoski M, Lei T, Wang H, Zhang J, Yuan JX, Malhotra A, Manor U, Wang S, Yuan ZY, Shyy JY. SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2. Circ Res. 2021 Apr 30;128(9):1323-1326. doi: 10.1161/CIRCRESAHA.121.318902. Epub 2021 Mar 31. PMID: 33784827; PMCID: PMC8091897.
obles JP, Zamora M, Adan-Castro E, Siqueiros-Marquez L, Martinez de la Escalera G, Clapp C. The spike protein of SARS-CoV-2 induces endothelial inflammation through integrin α5β1 and NF-κB signaling. J Biol Chem. 2022 Mar;298(3):101695. doi: 10.1016/j.jbc.2022.101695. Epub 2022 Feb 7. PMID: 35143839; PMCID: PMC8820157.
Hi Cort,
you would write a piece about the DecodeME study because of its urgency to find participants. the world biggest ME/cfs study. At least you wrote that 2 blogs past.
why not? do you not want to write a blog anymore on it?
thanks!
I applaud any progress but frustrated why Gut Biome not being more heavily studied since most ME/CFS patients have unbalanced biome. My 26 y/o son (severe fatigue) was asked to take part in a LC study at large research hospital in Chicago headed by a renowned top neuro/scientist who also heads up the LC Clinic. When we had a clinic appointment with him, he had no interest whatsoever in considering any non neuro issues e.g. my son’s Dysbiosis (evidenced Gut Biome results), Constipation, severe Eosiniphilic Esophagitus/Gastritis, Positive Mycoplasma Pneumonia IgM (high IgG) ….I could go on….they said “We are only looking at neurological symptoms”. I understand trials may need to pinpoint a specific subset but how can a “specialty” LC clinic be so silo’d? (rhetorical, we know how frustrating these large hospital systems can be). When we went to the LC study appt. I later asked the nurse, are they even considering the Gut connection? (I believe is the root cause of a LOT), she told me someone had set up a meeting with many disciplines a while ago but not one discipline showed up). She did say they are starting a Gastro LC clinic separately.
Agree!
Right! Day 1 of the conference was heavy immune, some hormones, and very little metabolic or gut stuff (except for the finding of coronavirus RNA in the connective tissues of the gut) or blood vessel stuff. Also nothing on the brain.
Hopefully, we’ll see more of all of that on day 2.
Probably because medicine and science a whole don’t understand the gut microbiome still or how to do anything meaningful to alter and treat it. There is a concept of SIBO that is hotly debated in the medical community, some don’t think it is a real thing, others do and swear they have gotten better by treating it but there is no clear evidence one way or another. Also it doesn’t make sense to focus on the gut in a disease that involves so many systems and organs of the body from a virus that infects so many places (it is very unlikely to all stem from issues in the gut and they have looked to see where COVID virus persists and places beyond gut). I am sure lots of people with GI issues from ME/CFS, LC, and FM , myself included, want answers to address those symptoms but I don’t think focusing on an area where we can’t effectively modulate gut bacteria is going to let us do as much to treat.
I am starting to believe that the Gut is going to be found as the root cause of many illnesses, especially these ones for which there has not been an explanation. It has/is being studied aggressively by many large research organizations. A molecular biologist told me “Ten years from now the gut is going to be the “go to” place for illness diagnosis”. And there is powerful research this is the case.
Microbiome researcher at U of Chicago (Early career award) ZHENRUN J ZHANG
https://www.researchgate.net/publication/361054827_Translating_Microbiome_Research_From_and_To_the_Clinic
ASSOCIATION BETWEEN THE GUT
MICROBIOME AND HUMAN DISEASES
and
challenges in translating microbiome research from and to the bedside.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8761622/
Gut Microbiome in Myalgic Encephalomyelitis Chronic Fatigue Syndrome (ME/CFS)
Showed ME/CFS studies had much worse biome than non CFS studies
October 2023 – Science Direct – https://www.sciencedirect.com/science/article/pii/S014976342300372X#fig0015
Mitochondria of intestinal epithelial cells in depression: Are they at a crossroads of gut-brain communication? “recent studies have shown that gut microbiota is regulated by intestinal epithelial cell (IEC) mitochondria, which has yet to receive much attention”.
https://www.medicalnewstoday.com/articles/parkinsons-may-actually-start-in-the-gut-new-evidence-suggests
Parkinson’s may start in the Gut.
Columbia University Irving Medical Center in New York City
I stay far away from mainstream
Early October and please remind me if I don’t1
Hi Cort, if your message is for me, the decodeME study closes allready half november. now to ill. I copyd a part of what they mailed. The postoffce must be capable to and the people, caregivers to…. I do not understand what the problem is to write the blog sooner? it is the largest study on ME/cfs in the world and they are shortcoming on participants!
my copy of a part of there mail: “We are now in the final stage of participant recruitment and, if you haven’t already done so, you have until the 15th of November 2023 to complete your online questionnaire.
At 5pm on the 15th of November, we will be closing our registration portal to both new participants and to those who have signed up but not completed their questionnaire.
Participants, who sign up and complete their questionnaire by the 15th of November deadline, and who are invited to participate in the DNA stage of the study, will be sent a spit collection kit. Final deadline for posting these back to DecodeME is the 31st of January 2024. As there can be unpredictable delays with the post, especially over the holiday season, please post your kit back to us as soon as possible and before this date, if you can.
This is the last call to sign up and be part of the DecodeME study. Please join those in the ME/CFS community who are doing something extraordinary by taking part.
Almost 25,000 people have already signed up and completed their questionnaire, and almost 20,000 participants have also been invited to provide a DNA sample. This is great news, thank you to everyone who has participated!
However, we still need more people, and this is the last chance to be part of this ground-breaking study. So, if you, or someone you know, are 16 or older, live in the UK and have a diagnosis of ME/CFS, please do take part now to help us decode ME/CFS at http://www.decodeme.org.uk/portal
Finally, we currently have over 4,000 spit kits that have been sent out and not yet returned. If you have received your kit, but have not yet returned it, please send it back to us as soon as possible. If you have questions about returning your sample, then our FAQ page has a number of answers that might prove useful. Each sample returned will strengthen the results of our research, so we appreciate every kit sent back.
If you have been waiting more than three weeks for your kit, since receiving an invite to take part in the DNA stage, please contact the DecodeME team, email info@decodeme.org.uk team or on 0808 196 8664, and we will investigate and order you a replacement kit, if required. The final deadline for requesting replacement kits is the 15th of November 2023.
So, if you are yet to complete your questionnaire or haven’t yet signed up as a participant in the DecodeME study, but would like to do so, please visit http://www.decodeme.org.uk/portal before the 15th of November.
Thank you for supporting the study,
Warmest wishes,
The DecodeME Team”
Hey Cory, have you seen this study yet? Chock full of info. I mention it because they discuss possible treatments toward the end and they had this to say about antivirals and EBV:
“Treatment with antivirals such as valganciclovir or valacyclovir could reduce lytic and abortive reactivation, inflammation, the appearance of transient autoantibodies, disease flares, and insulin resistance.”
Dr. Levine has had me on valacyclovir for three years and she recently increased me to 1g a day as my EBV numbers were crazy high still. I have been unsure it is really doing anything, but then I read things like the above and think I should stay on it.
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04515-7
Sorry – Cort. Damn autocorrect!
Thanks, Amy – always looking forward to EBV stuff!
sorry but were these the wrong way round:
the study also found low testosterone in females and reduced estradiol in males?
Actually that’s correct. It was very interesting. Females who biologically looked more like males; i.e. who had more testosterone and males who had more estradiol – did the best!
Thank you Cort – how counter intuitive for males! If women are generally worse affected more testosterone for them makes sense. But why would more Estradiol help men?????? so much to unpack in this illness!
Appreciate this recap, Cort!
Cort, as someone like yourself has been following this field for a long time, I wanted to put this media note on your radar if you hadn’t seen.
https://www.science.org/content/article/anthony-fauci-becoming-devil-and-warning-his-successor?fbclid=IwAR15DMRB83KW6iVTsyN4zpCsEs4cfwp9_6QEVHimAalY7vEn5_I9Q4nwkhE
This was from 9/25/23: “Anthony Fauci on becoming the ‘devil’ and a warning for his successor”
Q: Let’s say you were starting your research career today. What would you study?
Fauci: ““More than 40 years ago, when I was the physician for the NIH, I was struck by a subset of patients who would come in usually following a viral infection…They would say, “Something is wrong, I just don’t feel right”…People later started talking about myalgic encephalomyelitis/chronic fatigue syndrome. What is it about? I’m fascinated by this.”
Was curious if you had any thoughts, given the history
Wow – you could have knocked me over with a feather. I was told he was always up on the ME/CFS science – but he did kick us out of NIAID – and that killed a lot of funding for us.
At least he’s saying it now. Did you see – our funding at the NIH expected to decline this year by 25% of 2021 levels. Fibromyalgia funding is going down as well.
Sure wish he could do something about it.
Hindsight is 20/20!
Interestingly my Cortisol level tests as low whereas my ACTH (which apparently is the precursor to Cortisol) tests as high. My GP / Doctor notes this and then moves on so I’m not sure how these findings translate into an actual treatment?
Hi Cort,
It’s been a long time since I’ve been active here.
First, great recap, or at least what I could process of it. My brain fog is so thick right now I can only take one subgroup at a time.
When long covid began I was really excited to hear doctors and researchers comment on how their findings would help people who suffer from ME/CFS and Fibromyalgia. Finally some big research $$$$ looking into post viral infections. I’m amazed at all the links between the three.
Hope everyone in this community is well. I’m looking into LDN presently.
Can’t agree more about differentiating out subgroups- I think this has stymied ME/CFS and fibromyalgia research for decades besides difficulties in agreeing on diagnostic criteria. I found the HPA axis issues interesting because that is a key issue in fibromyalgia too. Perhaps patients go on to develop the HPA issues after months of altered immune activation and inflammation and other things causing secondary damage, which could be something that happens in fibromyalgia too (just not as clear of a post-infectious illness as ME/CFS is) either in a somewhat autoimmune way or in a prolonged aberrant immune activation sort of way.
Any hunches what might be behind the low cortisol in the morning? My daughter has long covid, and bad fatigue and nausea in the morning are key symptoms.
Autonomic symptoms are often worse in the morning. (Not connected to low cortisol.)
Cort has written several articles on autonomic dysfunction and orthostatic intolerance that might be worth reading.
According to Dr Bruce Patterson, there is a test now for Long Covid and also a treatment for it. He says many people on his protocol have improved or recovered on Youtube.
Dr Patterson is the only one I know that distinguishes classical vs non classical monocytes. Perhaps that the mystery of of those that succeeded vs failed on the dexamethasone..i.e, they did no distinguish?
Nobody spoke about autonomic problems?
Let me give you a first hand account of post-Covid symptoms. My husband and I got Covid on August 12 at a national veterans’ conference here in Orlando. We were treated with Paxlovid. Upper respiratory symptoms and fatigue went on for a month. Finally, when I thought we were out-of-the-woods, we went to a few stores and lunch in the mall. I began to feel fatigued and ran an ECG on my smart watch. It said I had an irregular heart beat and I should contact my doctor. This is a new watch, so I thought it was just a glitch because despite several heart workups (one a year ago), I have never had Afib.
A day later, I was doing a few things around the house and my chest began to feel tight. I ran another ECG and got the same message. This got my attention and so we went to the free-standing ER near our home.
I had irregular heartbeat on two ECGs. This was relieved by nitroglycerin tablets. The staff began a procedure to admit me to the hospital for more testing. They seemed very concerned, but I didn’t want to go to the hospital so I declined.
I have an appointment on Monday with a non-invasive cardiologist at our new medical building nearby. I am worried about myocarditis or pericarditis from the Covid.
I have avoided exertion since the ER visit except for a short walk up and down the aisles of Home Depot. Again my watch registered an irregular heart beat.
I have had ME/CFS since 1984 and was treated for a great part of that time by Dr. Paul Cheney who believed all of his patients had left diastolic dysfunction. He always did an extensive ultrasound at your annual meeting with him.
Dr. Cheney had gotten a mild case of ME/CFS when he was working with the initial outbreak in Incline Village. Unfortunately, it wasn’t as mild as he thought and he developed heart failure and had to have a heart transplant.
I remember him saying that before the transplant, he had gotten to the point where he couldn’t eat much more than pineapple. Afterwards, he was able consume 5000 calories a day.
I am wondering if heart involvement is causing GI problems in both ME/CFS and Long Covid.
Infection, 13 times more infections in vaccinated group,
Symptomatic disease, 27 times more disease in vaccinated group,
Vaccinees not Infection Group, 13.06-fold increased risk for infection
,
Naturally acquired immunity confers stronger protection against infection and symptomatic disease caused by the Delta variant of SARS-CoV-2,
compared to the BNT162b2 2-dose vaccine-indued immunity.
individuals who have had SARS-CoV-2 infection are unlikely to benefit from covid-19 vaccination
Sixteen studies have demonstrated the power of acquired immunity
Clinical Infectious Diseases, Volume 75, Issue 1, 1 July 2022, Pages e545–e551, https://doi.org/10.1093/cid/ciac262
Nabin K. Shrestha, Patrick C. Burke, Amy S. Nowacki, Paul Terpeluk, Steven M. Gordon
doi: https://doi.org/10.1101/2021.06.01.21258176
Now published in Clinical Infectious Diseases doi: 10.1093/cid/ciac022
https://www.washingtonpost.com/outlook/2021/09/15/natural-immunity-vaccine-mandate/
In these studies you can find the information of my reply
The connection with low cortisol is intriguing, and may perhaps explain why I have been as functional as I have been, although I have never fully recovered from a very early EBV infection, and a later, horrifically bad, CMV infection, both of which have caused long term ME/CFS. The thing is – I also have autoimmune Primary Addison’s disease, so I have been on daily cortisone for almost 50 years, and my endocrinologists have been puzzled as to why I seem to need somewhat more than the “normal” dose. Plus, increasing my cortisone dosing when I have flare-ups of my ME/CFS definitely takes the edge off the fatigue and muscle/joint inflammation. It is also notable that one of the symptoms of untreated Addison’s is postural hypotension (in addition to to brain fog, fatigue, and nausea). There is also a recent study that links Primary Addison’s with some sort of impairment of NK cell functioning – not sure how that fits into the picture. And I also remember than I had the EBV infection several years before EBV was “discovered” – and back then it was called infectious mononucleosis, so the connection with monocytes seems logical.