

Earlier, Klaus Wirth and Carmen Scheibenbogen found a way to explain the brain issues in chronic fatigue syndrome (ME/CFS) without resorting to neuroinflammation. Their multipart series of ME/CFS hypotheses brought the most thorough potential explanation of what’s happening in this complex disease yet.
Now Wirth, working with Mathias Lohn, has found a way to explain the orthostatic intolerance in long COVID and chronic fatigue syndrome (ME/CFS) without resorting to autonomic nervous system dysfunction.
These researchers demonstrate how important it is to have as many eyes on ME/CFS and related diseases as possible. A pharmacological researcher at the University of Frankfurt, Wirth has focused on things like cardiovascular pharmacology, the pharmacology of bradykinin antagonisms, and cerebral blood flows; i.e. he brings a skill set to ME/CFS that we haven’t seen before – and that has brought a new way to look at this disease to the table.
In “Orthostatic Intolerance after COVID-19 Infection: Is Disturbed Microcirculation of the Vasa Vasorum of Capacitance Vessels the Primary Defect?”, Wirth and another cardiovascular specialist, Matthias Lohn, take on orthostatic intolerance – the inability to remain upright without experiencing symptoms.
Most people equate the orthostatic intolerance in ME/CFS, POTS, etc, with autonomic nervous system (ANS) problems and stop there – but not Wirth and Lohn. They agree that the ANS is disturbed but don’t believe it’s necessarily dysfunctional. Instead, it’s doing its best to respond to a deeper problem in the blood vessels. In doing so, they’ve given us, in this hypothesis paper, a deeper cut into the vascular (blood vessel) system in ME/CFS than we’ve seen before.
The Blood Vessels…Again
It seems there’s no getting away from the blood vessels – especially for humans. Because we stand on two feet – leaving our head above our heart – we’ve evolved ways to keep the blood flowing to the all-important brain even as gravity is trying to pull our blood down to our toes. The blood vessels below the heart, for instance, contract when we stand to in order to keep the blood from puddling in our feet. (The blood vessels found above the heart contract in order to squeeze what blood is available up into our brain).
The authors note this vital need – to respond to standing and exercise with a coordinated system of blood vessel contractions – can be impaired in a number of ways:.
- An inability to contract the blood vessels – the smooth muscles that line the blood vessels can fail to contract them – leaving them flaccid and dilated – and allowing blood to flow to settle in the lower part of the body.
- Rigid blood vessels – overly rigid blood vessels that may have shrunken cannot contract and relax properly – and thus don’t provide the room for the blood volume needed to support standing and exercise.
- Hypovolemia (low blood volume) – in what is called the “renin paradox”, the RAAS system in ME/CFS and POTS patients does not produce enough blood to support standing and exercise.
- Problems with autonomic regulation (baroreflex, volume regulation, volume- and barosensors, and vagal and sympathetic activity) – can throw blood flows off as well. For instance, exaggerated sympathetic activity is believed to cause vasoconstriction, or narrowing of the blood vessels in the brain.
- Hyperventilation, which is also reported to occur in ME/CFS and long COVID, may contribute to cerebral vasoconstriction.
Could the Microcirculation be THE Underlying Problem in ME/CFS and Long COVID?
While all these may have a place in ME/CFS, POTS, and long COVID, the authors believe one major factor – in fact, THE major factor is missing – damage to the microcirculation; i.e. the very smallest blood vessels that feed our tissues.
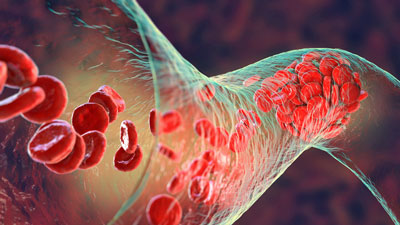
Several factors able to disturb the functioning of the small blood vessels (endothelial cell dysfunction, hypercoagulation, and altered red blood cells) have been found in long COVID (as well as ME/CFS). No one, though, has looked at the blood vessels that feed the blood vessels – the “vasa vasorum”.
The Vasa Vasorum and the Veins

Could the vasa vasorum – the small blood vessels (in dark) that feed the big blood vessels be a problem in ME/CFS and long COVID?
While problems with the microcirculation mainly affect blood flows in small vessels and capillaries, the authors point out that the large and medium-sized blood vessels are dependent on the small blood vessels that feed them to operate properly. Poor microcirculation in the blood vessels – called the vasa vasorum (“the vessels of the vessels”) – which feed the larger blood vessels could therefore impact them.
Of all the larger blood vessels in the body, the veins stand out. The veins are not just passive vessels that deliver blood to the heart; they need to actively contract to push blood back up to the heart. Contraction requires energy – which requires oxygen – which requires that vasa vasorum be feeding the veins lots of oxygen-rich blood.
Because the veins – in their role of delivering “used up and oxygen-poor” blood to the heart – transmit less oxygen-rich blood, anyway, they might be particularly disturbed by an inability of the “vasa vasorum” to supply them with oxygen and nutrients. That could prevent them from filling the heart with sufficient amounts of blood – and cause the preload failure that David Systrom’s invasive exercise tests have repeatedly found in ME/CFS.
Preload failure occurs when the heart receives less than normal amounts of blood from the veins – which, in turn, impairs its ability to send blood to the tissues – particularly during times of increased stress like standing and exercise. Systrom has called preload failure “the elephant in the room” for ME/CFS and has found it in 90% of his patients.
The low “preload” (i.e. the low blood volume presented to the heart) in people with ME/CFS could also be causing the smaller than normal hearts found in ME/CFS.
Flaccid Tubes
Blood vessels – particularly the veins – that have become unable to contract enough to force blood upwards (or towards the muscles) present another possibility. We’re going to hear a lot about the role that connective tissue problems may play in these diseases as time goes on. Suffice it to say, though, that Wirth believes that problems with the connective tissues lining the blood vessels and/or the high histamine release found in conditions like mast cell activation syndrome could be producing “flaccid tubes”; i.e. overly dilated and limp blood vessels that simply cannot move the blood along.
Over-dilated or flaccid blood vessels can’t produce enough pressure to get the blood to the tissues.
Lacking the nice taut tubes needed to squeeze blood out to the tissues, the body compensates by trying to squeeze those tubes down, telling the sympathetic nervous system (norepinephrine) to activate the alpha-adrenergic receptors that tell the smooth muscles lining the blood vessels to contract. That often not-so-successful attempt has consequences of its own.
Receptors that are chronically activated can, at some point, simply stop responding. Given what we know about the problems being upright in ME/CFS and similar diseases, chronic receptor activation could be common in ME/CFS. Being upright does not just refer to standing. Studies indicate that cerebral blood flows can be reduced in some people with ME/CFS even while they’re sitting, and in people with severe ME/CFS if they’re lying at a slight angle.
The authors believe that makes orthostatic stress an almost unavoidable chronic state for many and suggests that desensitized β 2-adrenergic and alpha2-adrenergic receptors could be producing an ongoing case of sympathetic and adrenergic hyperactivity and hypervigilance. (Autoantibodies that target those same receptors, as well as other factors (MAS-receptors, angiotensin-II-type-1 receptor) could produce a similar situation).
In all these cases, though, note that once again, it comes down to blood vessels that have lost the ability to respond properly to the stress of being upright, or to exercise.
Notice what’s missing in this picture? Any need for autonomic nervous system dysregulation. In this paradigm, the ANS is simply trying to compensate for problems caused in the blood vessels.
Rigid Blood Vessels
A different blood vessel could be in play as well. A rigid, and perhaps shrunken, blood vessel system that simply doesn’t have the capacity to store normal amounts of blood could be causing similar problems. Large blood vessels that are chronically squeezed down and unable to carry a normal amount of blood could also result in the presence of small hearts that lack the capacity to pump normal amounts of blood to the muscles and brain.
Either way – it all potentially originates in the blood vessels. (Earlier, Wirth and Scheibenbogen proposed that a similar process is occurring in the brain).
THE GIST
- Klaus Wirth and Mathias Lohn’s new hypothesis demonstrates once again how important it is to have as many eyes as possible on these diseases. These cardiovascular and pulmonary specialists bring a different skill set to these diseases – and it shows!
- They don’t believe that the autonomic nervous system is behaving poorly in ME/CFS and long COVID at all; instead, they believe its simply trying to compensate for problems in the small blood vessels that feed our tissues.
- In particular, they propose that damage to the small blood vessels (called the vasa vasorum) that feed the larger blood vessels (the arteries and veins) may play a critical role in these disorders.
- Each of the blood vessel problems they tick off – narrowed, rigid blood vessels, flaccid blood vessels – could be caused by an inability of the vasa vasorum to feed them the oxygen and nutrients they need.
- Because the veins already receive deoxygenated blood, and because they need to contract – an energy-intensive process – to push blood up to the heart, they may be impacted most of all. That makes sense given David Systrom’s finding of “low preload” – low blood flows to the heart – in many of his ME/CFS patients.
- The chronic stress imposed by standing in ME/CFS and long COVID could also desensitize the receptors responsible for contracting the blood vessels and maintaining blood flows.
- The microcirculatory hypothesis could explain why the current treatment approach – focusing largely on manipulating the autonomic nervous system – has been of limited help. We might get further along, the authors believe, by focusing on the root of the problem – damaged small blood vessels. That would lead, they believe, to “more specific treatment options” and improved outcomes.
- Klaus Wirth believes he’s found a drug (unnamed) that he thinks can help in ME/CFS. He formed a company called Mitodicure which is currently looking for funding.
Long COVID and ME/CFS
Next, the authors ask whether the same factors are causing orthostatic intolerance in ME/CFS and long COVID? The answer is: possibly. Studies indicate the vasa vasorum – the small blood vessels that feed the big vessels – can be damaged by the coronavirus. The inability of those blood vessels to contract could result in a state of chronic sympathetic nervous system activation; i.e. the same autonomic nervous system dysregulation that is seen in ME/CFS.
A More Focused Treatment Approach
The microcirculatory hypothesis could explain why the current treatment approach – focusing largely on manipulating the autonomic nervous system – has been of limited help. We might get further along, the authors believe, by focusing on the root of the problem – damaged small blood vessels. That would lead, they believe, to “more specific treatment options” and improved outcomes.
One way to assess whether their thesis is correct would be to compare the diameter or volume of the large blood vessels in both the supine and upright positions in long COVID and ME/CFS patients versus healthy controls. An inability of the large blood vessels to adjust to an upright position would put a focus on blood vessel functioning.
The Big Picture
Wirth wrote that both precapillary cardiovascular problems (low blood volume, low cardiac filling, vasoconstriction issues) and capillary disturbances (microclots, large monocytes, damaged red blood cells, sticky red blood cells) are present in ME/CFS and allied diseases. Both work together to make it more difficult to maintain good blood flows in ME/CFS and allied diseases. He and Lohn are writing a paper on the “catastrophic interaction” they believe these factors produce in diseases like ME/CFS.
Earlier, Wirth wrote he and his partners have “derived pharmacological mechanisms necessary to address the core of the pathophysiological mechanisms, the vicious circles, that keep the disease process running. Key disturbances are the ionic disturbances in skeletal muscle and disturbed skeletal muscle and cerebral blood flow. To realize this drug project, a company has been recently founded and is looking for seed funding to finance the project.”
That company is called Mitodicure and the drug it’s focused on could help with the blood flows as well as other issues. Right now, Mitodicure is in the phase of gathering financial support in what is currently a difficult market situation (high-interest rates restrict flows into venture capital companies) for a rather controversial disease; in other words, it’s not a piece of cake. Let’s hope they succeed.






Hi Cort, I wish there hypothesis where true and Mitodicure would make finally a treatment. Or is there allready any proof? Mestinon certainly does not help everyone for excample.
i tryd to search Mitodicure but could not immediatelly find a link to the compagny. Do you have a link for me please?
also I thought that Visser and Van Campen found (sorry brain issues) that you could have pots even not shown in a tilt test with there was it echo doppler from a vein from the neck. So even when laying totally flat (or am I wrong). I do not know how this fits in here?
Must I conclude that the bloodwashing from carmen scheibenbogen for the antiboddies is not it? but all from bloodvessels? Or both?
And how about Ron Davis, was it red blood cell deformability?
thanks!!!
Hi there – the Dun and Bradstreet registry for Germany shows a filing for the company, but I think it’s probably too new to have a web site yet. Please bear in mind that it will take them 3 years or so to set up, possibly more if they have trouble with funding, and then it takes an average of 10 years to get a drug to market. While it’s great to see the research, new drugs are a very long term proposition.
Just to add….the research that underpins it might identify existing therapies we can use much more quickly, and in any case will help us understand the disease better, so don’t lose hope! It’s just faster to concentrate now on the information and less on the company.
thank you for both answers verry much!!! yes, identifying therapies (urgently) that we can use much more faster would be ideal. A dream… Or understanding the desease better like you wrote. It all takes so much time…
I’m comforted that there are studies as far back as the 90s, we’re gaining momentum (especially now that Long COVID is around) and learning more all the time….fingers crossed!
thanks, yes fingers crossed like you wrote!!! But i thought that even the long covid is as heterogenous as hell. Just like ME/cfs. And that there is no consensus rigourous proof that the long covid ME/cfs subgroup is 100% the same as ME/cfs. And even if it is, all the heterogenity… If I remember correctly, that was why (with ME/cfs) precicionlife “stopped” there previous research because of the heterogenity and “falls diagnosis”. Think they are still working together with the DecodeME study. And it seems for me (maybe my brain) that every researcher says something else. Am ill since ’94, wish there where at least tests. Money for research we deserve worldwide… Way more biobanks, mousemodels, allready subgroupings, or just allready treatments. The last would be ofcource the best!!! running out of time…
I think you’re right about everything and I hope out of the many treatments currently being tried off-label or as supplements you’re able to find something that helps you NOW 🙂
thank you, you to!!! 🙂 here in my country not found yet (the of label ones) and with supplements no good luck…
Dr Peter Novak discovered a condition in which people have a normal tilt table response in terms of heart rate and blood pressure, but their cerebral blood flow falls. It’s called OCHOS.
https://pubmed.ncbi.nlm.nih.gov/26909037/
In POTS, people have an abnormal tilt table response in heart rate plus a fall in cerebral blood flow.
Thanks, for this blog, Cort.
I and so many other ME/CFS folks don’t have orthostatic intolerance though. I wish that there would be more work on grouping patients more accurately. You can certainly not explain the main disease mechanisms when you focus on symptoms that are not those that everyone experiences.
Those are PEM, the flu-like symptoms and a sore throat.
And an important group experiences “a new type of headache” or, to put it more accurately, simply brain inflammation. Jennifer Brea comes down with this symptom in Unrest. Gez Medinger who is a Long Covid and ME/CFS sufferer-doctor-youtuber has it, and I’ve spoken to and watched so many more tipping their front because they had a fire going on behind in the frontal lope during episodes. Therefore it is correctly called ME.
I am for many things extremely grateful to Prof. Scheibenbogen. She did for example publish a very well overview paper for doctors and the interested public on ME/CFS type of Long Covid and ME/CFS that has served me greatly.
On the other hand I think that it is not her that we should follow theoretically because she doesn’t believe in brain inflammation.
Maybe this is just strategically because the neurologists continue to claim that with their means they cannot detect brain inflammation and that this is prove that there is no brain inflammation.
This is unacceptable: Because, we all who have brain inflammation driven ME/CFS episodes (crashes) feel perfectly that our frontal lobes are inflamed – there is the heat, a feeling of a weird movement that shouldn’t be there and an elevated pressure in the brain. Plus, the tissues get injured when the inflammations become chronic, the episodes are followed by weeks of fatigue which is typical after brain inflammation.
What is very important is, that these simple things of what is really going on are described better in the literature before we try to understand the pathology.
I did art history as a minor and it would be very weird to give an anlysis of a painting without first describing the painting.
But this is what happens in ME/CFS research, unfortunately.
I actually don’t have flu-like symptoms. One study pegged flu-like symptoms at 24% of sufferers. The thing that has bedeviled ME/CFS research for so many years is that the symptoms are not consistent – even all the research suggesting viruses are the cause, the best we’ve been able to do so far, has to admit that only about 70% of patients had a virus first.
The warm, pressured feeling that you get – is it like when you let blood back into your arm after it’s fallen asleep? I’ve seen it mentioned in some case studies but not at a high frequency.
I read the literature on ME/CFS when I can, as a hobby, and the brain inflammation is frequently acknowledged, but as a thing that’s downstream from whatever the cause is. Inflammation is known to happen when there are abrupt changes to blood flow, maybe the cause is draining and sudden restoration of cranial blood?
Hi Kira, thanks for your reply.
That is new to me that you get an ME/CFS diagnosis without the flu-like symptoms that go together with the PEM-style pathological exhaustion. I thought they were required in the CCC.
But your statement is water on my argument that there is a need for a better qualitative description of the subtypes of those who are diagnosed with ME/CFS before there is done more sophisticated research on details of details who lose sight of the problem as a whole.
When you ever had brain inflammation then you would know that the proprioceptive system of the brain can perfectly inform your understanding of you having a brain inflammation. It does not feel different from an inflamed skin after a terrible sun burn, an inflamed parotid gland, inflamed inner ear, inflamed throat, upper lungs. Just to share some other body parts where I have experienced inflammation.
ME/CFS brain inflammation goes together with the typical sensitvity to light and as I mentioned the lingering fatigue for many weeks when you come out of a severe episode.
I think that the reason why it is so difficult for the neurologists to accept that they should investigate brain infammation in ME/CFS is their “brain inflammation law” that states that brain inflammation is rare and always extreme in the symptomatic, going together with typical symptoms like a stiff neck and psychosis and that one can barely survive it without the help of the staff of a hospital ward and tons of antivirals/antibiotics and so on.
That this can’t be true is actually obvious because there are many other known inflammatory processes like MS or Alzheimer’s that do not follow that pattern. But it seems that it is unimaginable to neurolgists that there could be brain inflammation at a middle heat level.
The injured tissues in the frontal lobe heal always more slowly after every episode. With my excellent health management and pacing I revover now well from my mild-moderate disease level. Although my last relapse is nine months away and my overall load limit has improved significantly it is the injured brain tissues that limit my activities. And I have to most strict with not overdoing it with relational and intellectual work because they are jobs where the frontal lobe is heavily involved. Also I experience some mild symptoms of dementia.
It might well be that the brain inflammation damages the endothelial cells (vessels) strongly. I think that there is already proof that ME/CFS damages preferably endothelial cells.
I think it’s a connective tissue disorder at source. We all have EDS…we just don’t know it.
I think the only thing is going to get us out of this is stem cell therapy and regenerative medicine.
Everything else is downstream
I’ve now read three studies including estimates of EDS prevalence in ME/CFS. They variously put that at 20% co-diagnosed, 50% and 70% with symptoms. On those estimates I wouldn’t be willing to bet that we all have EDS (though I personally am hypermobile). There are, however, researchers who are making that argument….
I think whatever’s going on certainly isn’t helped by connective tissue disorders, but I’m still looking for a more complete model – especially since more direct systemic interventions can bypass the processes implicated by connective tissue and still work (pyridostigmine, CoQ10, etc).
The thing is, they’re still finding new eds types. Whether someone gets diagnosed with eds is often a fairly subjective process of crude assessments as for some of the types genetics, just like in m.e. have no discernible genetic cause.
We don’t understand connective tissue but I’m almost convinced it’s the leading cause of the cascade that happens. There will be other issues I’m sure but the overlay between autism, eds, m.e. fibro etc. They all have connective tissue issues.
I think it’s nad that more focus is not placed on this. The sooner there’s a deep dive , the better
They don’t bypass in my opinion. They somewhat improve the tone of the bodies response but they can’t bypass what’s basically a slightly abnormal from. Birth physiology
I look forward to more research 🙂 Rowe, Eccles and Castori are some of the names I’ve seen pursuing this theory, and they’re all busily occupied.
I don’t know that I would turn to neurologists for a complex multisystemic disease, to be honest. Most of them are the engineers of the medical world – stubborn, technocratic and unwilling to see anything not immediately in front of their face. The specialists who’ve done the most in ME/CFS are in Infectious Disease, Exercise Medicine/Physiology, Cardiology, Gastric, Respiratory, Cell Biology Research and Internal Medicine. Most people who aren’t specialists are basically hapless in the face of ME/CFS, because it is so complex and multihued.
There are multiple arguments in the literature about subtypes and after literally three decades of research no one can agree, because there are so many processes that are implicated and no one has yet been able to figure out which ones are at the root and which ones are consequences. Then too, every time someone does some math to try and separate patients into groups, the groups come out different. There’s slowly come around a consensus that there’s probably an immune/post-viral subtype, and that’s as far as we’ve managed to get to date, but no one wants to wait another 30 years for all the tediously exhaustive descriptions to argue about subtypes when researchers could be looking into ways to help people….
Thanks for replying, Kira
I didn’t suggest to go to a neurologist when you have a suspicion of suffering from ME/CFS. I know that they don’t want to know anything about it. I think that one of the reasons why they cannot understand that there are brain inflammation processes that they don’t know because they are stuck with their “neurological laws” from the 19th century. One is that they believe that brain inflammation is this extreme event which is immediately life-threatening. Therefore they think that ME/CFS cannot involve brain inflammation. (Another of their bourgeois 19th century laws is that women are insane)
The same is true for the infectiologists. I think they are just as 19th century as the neurologists. They’re model of viral infection makes them believe that viral inflammation is always present as a full cycle of reproduction of the virus. Because they cannot think out of this box they never seriously went into ME/CFS and herpes drugs studies. Which was completely against the fact that many people stopped experiencing ME/CFS symptoms on Aciclovir and Ganciclovir.
I am so glad that virologists have now so much better technological means that the smoldering herpes reactivation theory in ME can finally be researched.
I don’t think that ME/CFS is a complex disease. But I think it’s true that most researchers have a poor understanding of what they’re doing and don’t see the forest for the trees anymore. That’s why they think that it is complicated.
There are others who think it is rather a simple puzzle that can be solved. They are those who are either clinically very experienced. Here is a webinar by a leading Melbourne GP institute on ME/CFS:
https://www.youtube.com/watch?v=EUIdbbwcnAE&t=2553s
Both the doctor and those with lived experience of ME/CFS don’t have a problem to explain it. I think they are really excellent because they are the only one that I know of who can diagnose non-LC ME/CFS in its mild form when one experiences neither many nor severe symptoms.
I think that this is the result of good description. I think we need more of this and not more research of people who have very complex ideas of what ME/CFS is.
Because without a simple understanding of a problem and a simple question what it is that you want to find out you cannot find out anything.
Thanks for the link!
Subconsciously there is active disregard and ignorance to maintain the sick sick. It’s human nature and whoever denies it is lying to themselves. No one is going to help you except yourself. Why would people heal someone that would be competition to them. Of course, like everything it is a spectrum, and there are those who truly want to stop some of our suffering and this is where we get some of the advances.
☝️finally someone that thinks like I do.
They are in the business of making money$$$$$….especially private practice.
Yes, I have a doc that knows about this horrid disease…BUT….when I go to see him he offers nothing and EXPECTS me to do all the research etc.
It’s like a game of cat and mouse.
He isn’t exactly digging in his heals.
His scheduling shows that he’s all about the money….one day I called for an appointment.The reception stated that he’s booked solid for 2 1/2 months.So because I don’t have employment, I decided to go park nearby just to see how busy this guy really is….he’s not busy ….he hadn’t a patient walk through his door for 3 hrs.
If anything, I’ve educated him by finding new research, treatments etc.
One day it dawned on my little swollen pea brain that this guy is just stringing me along and milking me for visits.i get more from this website than I ever will from this guy.
Keep in mind folks…these people have a bottom line and that is to see as many patients as possible in the shortest amount of time for X amount of years till retirement.
It’s the business of sickness…..$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$$
Yes. Thank you. I agree. That is all I can basically type. I am in the midst of another assault and my firebrand and hind brain are in terrible pain. In general, I am person who didn’t experience head pain until third round of covid. I could cry right now. I can feel my brain cells die. I hurts so bad.
I am sorry that you are in so much pain. I remember the acute episodes of brain inflammation vividly. My suffering was also big. I didn’t experience too much pain, but I found it really worrying to have an inflamed brain, and no one to look after me. In hindsight I realised that the inflammation increased feelings of strong anxiety a lot in a physiological brain process. It was hell.
The good news is, with pacing, good rest, and good care the immune system is able to slowly shut the inflammation down again. For me yoga and meditation were key to not totally lose it. But I want to add that I was not a beginner on that path but had over ten years of experience with intensive retreat practice.
When I realised that I was not able anymore to bring stress levels down by myself I went to a shiatsu practitioner. That was very beneficial. I went several times until I was able to mentally calm down again and thus take good care of myself again.
I also can recommend Thai oil massage and acupuncture. But I think for the acute phase shiatsu works best because its the most gentle and soothing practice.
May you be held in boundless compassion in your suffering.
always wondered about the sore throats, wonder if biopsies would show something, some reason for continual sore throats
My understanding from experiencing it was always that the sore throat was a consequence of the lymph nodes overstrained by their job of filtering inflammatory poisons out of the area.
The first thing that I did when I got seriously ill was seeing an Ear Nose Throat doctor. Her findings were negative. This helped me to conclude that my suspicion that I had slight smoldering brain inflammation was correct.
Because the whole thing for me from the beginning felt like herpes virus reactivation I begged her to prescribe me Aciclovir on speck. She did it quite against her will and I was very lucky because the drug immediately stopped all the symptoms, especially also PEM.
That’s why I think that it is Maria Ariza and Bhupesh Prusty with their hypothesis of smoldering HHV6 brain inflammation that are the only researcher for my subgroup of patients (those who point to their front to indicate that there is the center of inflammation) who are the only ones on the right track.
Aciclovir is mainly used against HHV1 and 2 but it is also proved to be efficient against HHV6.
I had no EBV or CMV reactivation when I first fell ill with ME/CFS. It has nothing to do with that.
I didn’t have that either. I think no one has it. I don’t understand why you mention EBV and Cytomegalia.
Maria Ariza from Illinois State University and Bhupesh Prusty from Würzburg in Germany have together with others developed the hypthesis that in ME/CFS an abortive, smoldering type of HHV6 activation plays a central role in the pathology.
The replication of a herpes virus is not a thing of just a few chemical steps in the cells but it is an extended process where a whole battery of molecules that the virus produces play an important part.
Ariza and Prusty hypothesise that in ME/CFS it is the first steps of viral reproduction that start over and over again but don’t lead to the virus repriduced in the end. In the last years they could show that within these first steps there are amongst others enzymes produced that compromise mitochondrial functioning and can thus explain PEM. They can also explain they claim why it is the endothelial cells (vessels) that are among the cells most compromised in the process.
They further hypothesise that people with ME/CFS have a disfunction in the immune system that incapacitates it to stop the virus from activating the first steps of the reproductive process whereas it is still enough competent to prevent the steps further down in the process from unfolding. Thus there is no
From what I know from clinical work around HHV6 is that a full blown reactivation is rare and mainly is common in people who are extremely immunosuppressed during for example a transplantation of organs.
“Thus there is no… viral load to be found in a PCR because the virus doesn’t get reproduced.
Since I was convinced that I had some sort of a new type of herpes reactivation (I am one of those who easily gets a HHV1 reactivation when stressed), long before I heard of ME/CFS as an explanation for my problems and since the ME inflammation process in my body can be stopped with Aciclovir (an herpes antiviral with a good activity also against HHV6) I think that Ariza and Prusty have actually already found the pathomechanism of ME/CFS. Whereas I am not sure whether it is the correct pathomechanism for everyone diagnosed with ME. In that case it would mean that there are different illnesses that look similar.
For early stage Long Covid for example Prusty’s team found out that there is rather a problem with HHV1 early-stage reactivation but not with HHV6 as in “older” ME/CFS patients.
I had a sore throat for about the first 20 years of my illness…
Back to subgroupings here….
I don’t suffer from sore throats at all. Flu-like symptoms and PEM, together with cognitive issues are my plague.
In my experience, it seems that more research is needed to uncover why exercise doesn’t help. If we could exercise, we’d have much better odds of recovering naturally. Especially those of us in mild to moderately severe levels.
Agreed….The subsetting may happen with long COVID – they are trying.
Toxic-like illness feeling here like cells close to fainting but not flu-like and no sore throat
Easily hoarse though and always need to wear scarves..hm.
my throat always sore, yet norhing the doc can see.
@Cort, does your sore throat show any sign to doc?
It’s funny but I don’t have POTS – I recently did the NASA lean test and it showed no evidence of POTS and my symptoms were stable throughout the test. If I’m up for too long though I really feel the need to lie down – so I’m pretty sure I have it in some form.
With regard to neuroinflammation Jarred Younger is working away on a validation of his earlier finding of widespread neuroinflammation in ME/CFS.
Did you feel any symptoms during the test? Remember you can have a drop in cerebral blood flow on standing with normal BP and HR, such as in OCHOS.
https://www.brighamhealthonamission.org/2019/06/03/expanded-autonomic-testing-helps-to-pinpoint-causes-of-orthostatic-intolerance/
Interesting, thanks!
I think I’ve seen somewhere there’s orthostatic intolerance without classic POTS? For me, might also relate to sceletal muscle ability of holding body upright
you probably don’t have EDS then. ME/CSF is a result of what is described in the article above that when combined with eds’s lax vessels instead of flaccid tubes you get flaccid latex tubes. The excess vasodilation/impaired vasoconstriction along with unlimited expandability of EDS blood vessels result in the catastrophe that is super severe ME/CSF. I’ve only been suffering from this for 8 months and made the connection week one, not sure why all the confusion. It’s pretty simple.
Yeah, this is my pet peeve too. All these new crop of “explanations” since COVID, including blood vessels, micro-clots, gut biome, etc, etc., consistently fail to explain PEM. Unless the explanation explains PEM, the theory is only an explanation of symptoms, not the cause. In this case, orthostatic intolerance and not MECFS.
As for the description of MECFS, the only thing that is truly common across all patients in all spectrums spanning from severe/moderate to mild/recovered is PEM and fatigue stemming from it. I think that’s the description that is both necessary and sufficient.
Hi Lina – I had temporarily forgotten about Jarred Younger and Nancy Klimas till Cort mentioned Younger below, who are each working on the neuroinflammation hypothesis in their own way. I ran across this video today which I thought you would find interesting. He mentions low-dose naltrexone in the video, which – if you believe your disease is neuroinflammatory – is probably worth looking into and talking to a doctor about.
https://www.youtube.com/watch?v=DU0UgWGyi0A
You have to understand that ME/CSF is a syndrome and there are different subgroups. It is lazy to say that PEM is specific to ME/CSF. This syndrome is a basket for various diseases that lead to PEM and a lot of people have OI. Until it is subclassified, OI is a relevant scope.
Intriguing and it could mesh nicely with Pretorius’ interesting (if maybe overstated) recent results on platelet activation.
I am guessing it’s supposed to line up with mitochondrial dysfunction somehow, based on the name of the company – do we know how? Simply assuming that oxygen deprivation explains it wouldn’t mesh well with the work we’ve seen from Phair and Fisher…..
Wirth noted there are two things going on – the problems with the blood and then separate problems with the blood vessels. This was the first time I saw it referred to that way. Somehow those two have to get put together.
Wirth and Scheigenbogen have certainly been productive – I look forward to finding out.
In the paper, I found this: “Skeletal muscle hypoperfusion, as a result of those vascular disturbances, together with mitochondrial dysfunction in skeletal muscle, which we assume is due to an ionic disturbance of sodium and calcium handling, could explain the high fatigability, loss of force and skeletal muscle complaints like myalgia.” I wonder if they’re chasing down a calcium channel inhibitor like verapimil (which is used in POTS).
Interesting. I’ve read the other comments below. My symptoms covered a vast range of things, but I personally have wondered about vascular issues and oxygen delivery. I’ve had issues sitting and standing and even exhausted muscles holding a phone at times. I’ve often thought my cells just weren’t getting what the need to function whether nutrients or oxygen. When I was very sick my ankles bleed internally/bruised when I tried to walk the block. I wondered if my veins were weak… so I watch and wait with anticipation.
I get bruised ankles sometimes, for no apparent reason. I didn’t link it with my ME – silly me.
Could failure of vessels to constrict be why nicotine patches are helpful for some? It’s maybe less about receptors and more about blood vessels?
!!!! I gotta try the patch. My pet theory is the microglial activation causing neuroinflammation. Activated microglial cells happen to be downregulated by dopamine, and nicotine appears to be dopaminergic. Thank you for bringing that up.
“Nicotine acts on nicotinic-acetylcholine receptors on dopamine terminals to release dopamine in the ventral and dorsal striatum encoding reward and habit formation, respectively.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9575980
If that’s of interest to you, you might look in to low-dose naltrexone. One of the two different rationales by which it is offered off-label for POTS is that it controls microglial activation.
https://link.springer.com/article/10.1007/S10067-014-2517-2
Thanks for the link, Kira. LDN for MECFS has been around for a while, but I’ve never heard of nicotine patch for some reason. I figure it would be easy enough to try since it doesn’t require a prescription like LDN. (I now claim to be “fully recovered”, but I’m still vulnerable to PEM at certain times). They seem to work on different receptors though. Wouldn’t it be great if all patients can benefit from one or the other?
TK, maybe someday, if the pace of research keeps up like it’s been recently!!
Re Nicotine Patch (a relatively benign intervention to try)…
https://linktr.ee/thenicotinetest?fbclid=IwAR2BQ6MsNHoqv8yZ3U5KLZwyNrqUbDON40NEx_nnC4S64Kx3icE2mPCiW4Q
https://pubmed.ncbi.nlm.nih.gov/12436426/
https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-023-00104-7
TK, thanks for the info on dopamine. Go to https://linktr.ee/thenicotinetest for all current documentation on the patient-led nicotine patch treatment project for LC & ME/CFS. Originated from a doc in Germany who trialed 4 LC patients, published a paper and had auf poster presentation in this year’s Charite conference, was picked up by patients in Twitter-organized project. I heard about in on Twitter (probably Herbert Renz-Polster’s channel, or @MECFSNews).
Thanks for the link, JR. I’m obviously not keeping up with the news anymore… I can’t participate since I no longer qualify for MECFS, but I’ll try TNT 3.0 when I struggle again.
I do have some reservation about Dr. Leitzke’s hypothesis though. If the virus is antagonizing/damaging the receptor, I’d think the problem should resolve eventually once the virus is gone. There are also nonviral paths to MECFS. But if it works, it works regardless of the explanation. I wish all the luck to Dr. Leitzke and the project!
Could MCAS be the cause of the restriction of the vasa vasorum??
Cort,thank you gor all you do, but I’m pulling my hair out because of these articles…and I don’t have much left.
Yeah, I read it and it’s a nice story designed to give us warm tingly feelings, thinking, oh, this MIGHT be something else that MIGHT help us. But, just as you said, it can take 3, 5, 8 years to get set up, and then there are the studies, trials and tests and everything else the FDA wants…they MIGHT get it approved in 10 years with luck. But what really drives me nuts is the wording of this…and pretty much every write-up like it. You wonder why I capitalized “might” above? It’s because I only see those types of words while reading, eg might, maybe, possibly, could, if, when, occasionally, should, hope, wish, may, potentially, believe, shall I go on? They should all have a precursor paragraph that states something to the effect: We really don’t KNOW anything, it’s just something we thought about so we’re writing this wild assed guess article and HOPE that it MIGHT turn into something in 10 or 20 years.
IF frogs had wings they wouldn’t bump their asses on the ground.
🙂 We are still in the world of “might” – the good news is that there are more eyes on this and more plausible “mights” than ever. The bad is that things take so long.
I think with this drug that Mitidocure is looking at it depends if it’s been tested in humans or not. If it hasn’t it has to go through animal and then human testing – a long time! If its already known to be a safe drug then I would think that doctors could get their hands on it and be testing it in their patients pretty quickly once a pilot drug trial was successful.
Cort….I can say with honesty, out of all the people you seem to more hopeful than any person I’ve ever met!
Like, what drives you?
Lots of things but number one is the research. As someone who follows the research I love to see the progress. I am always seeing progress – I am seeing heretofore separate fields coming together and I am seeing more and more superb researchers working on this stuff. I am also really gassed by realy ambitious efforts like the Long COVID Moonshot. Things are moving like I haven’t seen them before.
I think the question should be..what causes mcas.
Connective tissue disorder
Or whether MCAS is causing connective tissue disorder. We are definitely going to get into this on Health Rising.
Mast cells are all over the blood vessels are are certainly possible players in the blood vessel problems seen. (More on this in Wirth and Lohn’s next paper). I don’t know if they are in the vasa vasorum or not. I did find this
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5572344/
“Mast cells are found near the vasa vasorum in the adventitia of coronary arteries of patients with atherosclerosis and play a role in plaque stability (14).
“I read the link and appreciate “the gist” more now. Thanks for all the clues, It is as if several jigsaw puzzles are mixed in the same box, but some of the pieces don’t fit every possible picture,
I achieved a 3 mo remission on high dose luteolin which binds to ACE2 which is a part of the renin angiotensin aldosterone system that they refer to in their argument. The RAAS in the invisible hand. It activates platelets and immune system in the body as well as has a hand in blood pressure control due to body wide baroreceptors. These researchers are into something really big.
I have been so waiting for the ACE connection between ME/CFS, POTS and long COVID to be made….I had no idea that luteolin could help with that. How did you decide to go after something hardly anyone knows about?
Before becoming too ill to work, I was a veterinarian. We learned about the pathophysiology of the Renin-Angiotensin-Aldosterone System in depth because it can cause major illnesses in dogs that affects multiple systems in their bodies. I consider the RAAS and its connections to the baroreceptors in the body to be the *invisible hand*. It has abilities to alter blood pressure and vascular tone, immune system (esp macrophages and lymphocytes), and its ability to induce platelet activation and aggregation, as well as other things. It would be wonderful if someone could interview these researchers and get them more “air-time” on these theories. I truly believe this is a major part of our disease. There is a ton in the literature about it. I only hope that more researchers will begin to see the connection. The RAAS system, baroreceptors, etc are not functioning normally and because of that, can explain ALL of our MECFS symptoms. Now we have to find out what part of the process is broken. https://www.frontiersin.org/articles/10.3389/fphar.2021.640185/full
Oh, and it has a hand in mast cells as well.
Congratulations on your improvements! I’m curious why you chose luteolin over quercetin? What dose did you take?
I cannot tolerate Quercetin due to severe GI pain. My almost remission only lasted for ~3 months with Luteolin. I worked up to ~900-1200mg per day divided into 3-4 parts and most importantly I was cautioned by Dr. Theoharides (the mast cell master) not to use more than 1200mg of TOTAL flavonoids per day (green tea, quercetin, etc. so you have to count total amounts you are ingesting per day and then adjust accordingly). The luteolin became intolerable due to GI side effects, even with reduction in dosage. I have been convinced from the beginning , that all of my symptoms of the disease have to do with blood flow. The amazing thing was, when the remission of most all of my symptoms occurred, my skin became more firm and most all of my *cottage cheese* disappeared, my protruded and tortuous veins on the backs of my hands returned to normal size, the swellings in my fingers resolved and I was able to *feel* things with the tips of my fingers. The heaviness in my arms, legs, weakness all back to normal. I felt so… strong and young. I thought, if MECFS was chronic inflammation and damage, it seemed unlikely that I would be feeling this *normal* and healthy in a matter of days of starting high dose Luteolin. I felt as though I was 25 years old again (I am almost 50). So then I thought, could the heaviness in my legs and arms, which I was always suspicious was *blood pooling*, could that be related to the hypermobility and pain? Generally speaking, my vision of orthostatic intolerance is poor vascular tone, and vessel enlargement likely due to a traffic jam of RBC’s. I have this vision of our blood vessels being more like *water balloons* rather than proper hoses. Could this blood backup could be causing the muscle bellies to swell during contractions, which in my mind would cause overstretching of the tendons that attach your muscle bellies to the joints. During my high dose Luteolin treatment, my joints became completely nonpainful and the hypermobility in my joints were gone. My tendons around my joints felt so strong. If inflammation and chronic damage were a true cause, there is no way in my mind that reversal of such disease could occur in a matter of days. I felt that the ACE2 binder in Luteolin could be affecting vascular tone and blood flow through the Renin Angiotensin Aldosterone System and baroreceptors of the body. This is why I believe these researchers are onto something. The only symptom that I could not resolve fully was the sweating, which to me, shows that I could not shut off the autonomic nervous response fully. When I have gut issues, it is always blood supply issues for me. So when I began experiencing the gut issues while on Luteolin, I did what any MECFS patient would do, I began peeling myself off of my supplements backwards. When I came off of the Luteolin, my stomach improved. Now, each time I try to take even a small dose of Luteolin, 100mg, I return with GI side effects. The RAAS and Baroreceptor system, as well as its interaction with the ANS is VERY complex and outside of my expertise, but as a patient with the disease, with 15 years of being a medical experiment, I am highly suspicious that the RAAS/Baroreceptor System/ANS are together causing our symptoms and that once blood flow is restored, a great majority of the symptoms can be completely reversible.
Thanks for your response. I have been considering trying out PDE5 inhibitors like Viagra / Cialis for this reason. They’re also some interesting but very expensive devices on the market such as Kaatsu bands and D’oxyva that make blood flow improvement claims…
Interesting. I appreciate the recommendation about the blood flow devices. I have had good luck with a Selenite Tower lately. As soon as my GI shows symptoms, I wand it over my abdomen and you can immediately hear my belly begin to move and gurgle.
Amazing what a $20 crystal can do if you are desperate and quirky enough to try. It seems to bring blood flow to the area since most of my blood falls to my arms and legs due to OI.
I’ve been “donating”
My blood due to very high ferritin.
Since “donating”,
My guts have been making a lot of noise and food seems to be moving at a better pace also.
Emily,
I have also had good luck withenzymatically modified iso-quercetin and liposomal luteolin, but I have to take a lot of them to feel better. I also take fisetin. What does Dr. Theo say happens when you get too much? I respect his work so much, as I do with Dr. Afrin’s work.
I have also had very good responses to serrapeptase, 120,000 units per day. Cheap, too!
Ann1, that is wonderful that you can get some relief with these flavonoids. I have not heard of Fisetin. Dr. Theo told me that the liver cannot process more than ~1200mg of Flavonoids per days (for ppl with normal liver fxn). I, too, am taking anticoagulants. Having some type of flareup this fall and was having trouble breathing again. Have been on a once daily supplement of Nattokinase (NSK-SD 100mg Pure Encapsulations); but because the diff breathing returned, I added in baby aspirin. Better to breathe after a few days. I have yet to try Serrapeptase. I forgot to mention in my previous threads, that when I had the remission of most of the symptoms, my brain function returned. I began reading books again. It was so wonderful. I was grateful to have those three months. It showed me that there is a functioning person inside of me ready to return. Gave me hope.
Emily,
Thanks for your reply and the information from Dr. Theo. I am just under the 1200mg limit, so I’ll keep doing what I’m doing. Dr. Theo’s own formulation of luteolin is on his company’s website, Algonot. It only has 100mg of luteolin, but it says you can take it four times a day. I take 500mg of liposomal luteolin once a day instead. He says to be careful that your luteolin is not made from peanut shells. His is made from grapefruit seeds and it is very expensive, especially for me here in Canada.
Fisetin is one of the minor flavonoids like rutin. I take it because it is a senolytic, like resveratrol, and I like that idea.
Serrapetase has been very helpful to me. I also read that it is enhanced by taking some nattokinase with it, so that’s what I do. You’re supposed to take them on an empty stomach, but I get a horrible stomach ache and diarrhea when I do that, so I take it on the empty stomach and then eat something like celery to push everything down there. That seems to work.
You had such luck with luteolin, but I understand the GI problems can be bad. Could you get a compounding pharmacy to make up some sublingual tabs for you, to bypass the GI system altogether? Maybe topical? After such success, there must be another option somehow.
I had to do topical with LDN until I got better enough to be able to survive swallowing it. Now I wouldn’t be without it. Ever. Best of luck to you.
Hi Cort,
I have a couple of questions.
Do they really believe that if these small blood vessels are damaged that they can heal with the medication?
Until now I’ve often read that researchers believed they could use an existing drug to treat MEcfs. Is there nothing currently available for this purpose? It sounds like this startup is years away from benefiting current patients.
Thank.
All I know about this drug is that they believe it can get at core issues of ME/CFS. I don’t know if its a repurporsed drug; i.e. it’s already in use elsewhere or is some compound that was produced but never used or what.
Since so many people think it all goes back to inflammation if the source of the inflammation was found I would hope things could heal themselves.
Thanks Cort for your never ending work.
My ME shows mostly in orthostatic intolerance, which increases dramatically when I overdo it and create a PEM, despite all my precautions. I almost never have flu like symptoms.
I like the hypothesis that the ANS is trying to cope for inadequate veins rather than being disfunctionnal. That could explain why relaxing techniques help, indicating the ANs is responding adequately to a different demand.
Right – interesting insight. For me, my OI really shows up when I over do it as well.
and me too – the OI does get worse when I do a lot!
Recently, I had to move and in doing so I encountered quite a bit of sludge/mold/bacteria in the AC system of my “new” apartment. Strangely, my body responded by causing me to have edema where my body retained water. I gained 13 pounds in 3 days all water weight. The interesting thing was that I felt really good. I was able to walk 15000 steps a day while carrying boxes and even in the evening when on a good day I would be wiped out I felt a normal tired. Sadly, the edema started leaving after 3 days and I lost 15 pounds and felt quite sick and wiped out for the next 6 weeks. The same thing happened again when I switched to a ketogenic diet (which is after I had recovered somewhat from my 6 weeks) as I guess your body changes the way it processes electrolytes. Currently, I just started (2 days ago) on a drug Florinef that helps your body retain fluid. I had used it in the past for 10 years with good success in allowing me to function at a higher level. Now, it has been 15 years since I last used it and I have to keep an eye on my blood pressure, but it could be something that people might want to consider trying.
Interesting. I do wish they could provide a little bit more on treatment possibilities now rather than some drug company that will be years in the making. Didn’t the article on low dose propanalol pose a possible solution to the over sympathetic response of the smooth muscles involved in this pathology? Has that been considered?
Just here to support you, friend.
Yeah like I wish they would have given more hints of pharma or supplement intervention that could help address this hypothetical problem. Like they mention ionic possibilities. Calcium influx into cells has come up before. I just wish they would have given more clues as to their thinking as many of us can’t wait years for some special drug when there are things we could be trying now.
Since Klaus has been pharmacological researcher for many years, m guess is that he knows the ins and outs of drug development and keeping quiet right now is the best way for this to move forward as quickly as possible as frustrating as that is for the rest of us.
He has shown remarkable interest in this disease and I dearly hope that his drug idea gets a shot.
Hopefully we will know more before too long.
Propanol is a life saver for me but it hasn’t stopped the m.e.
I honestly think I may be dead without it tho
At this stage it behooves Mitodicure – as it would any company in their position – not to release specifics of the drug. I would guess from the name though – Mito-dicure – that it has something to do with the mitochondria.
He should talk to Frans Visser and his partner Linda van Campen. I think together with Peter Rowe they did. exactly measure changing diameters of the main arteries though I believe to be able to demonstrate the reduced blood flow to the head, when standing or in a tilted position.
Merci pour cet article, Cort. Cela me parle, car depuis 7 mois, je fais des séances de fasciathérapie avec une thérapeute toutes les 3 semaines..
Les tissus conjonctifs (fascias) participent à toutes les fonctions vitales. Ils contribuent à la respiration, aux mouvements, à la digestion, à l’activité nerveuse… Le système fascial joue un rôle essentiel dans les échanges tissulaires et cellulaires, dans la circulation sanguine et lymphatique. Le système fascial est interconnecté avec le système nerveux et la circulation sanguine.
À ce jour, j’ai récupéré environ 50% de mes capacités : moins de fatigue, moins de malaises post effort, plus de concentration, moins d’anxiété, moins de problèmes digestifs, plus de force… Après 20 ans d’EM/SFC, je peux enfin profiter un peu plus de la vie, c’est encourageant, même s’il reste encore du chemin à parcourir
Thanks for this article, Cort. This speaks to me, because for the past 7 months, I have been doing fasciatherapy sessions with a therapist every 3 weeks.
Connective tissues (fascia) participate in all vital functions. They contribute to breathing, movements, digestion, nervous activity… The fascial system plays an essential role in tissue and cellular exchanges, in blood and lymphatic circulation. The fascial system is interconnected with the nervous system and blood circulation.
To date, I have recovered around 50% of my abilities: less fatigue, less discomfort after exercise, more concentration, less anxiety, fewer digestive problems, a little more strength… After 20 years of ME/CFS, I can finally enjoy life a little more, it’s encouraging, even if there is still a way to go…
Really interesting, Claudine! Thanks for sharing that. I think the connective tissue will loom larger and larger in this illness.
Thank you, Cort. I am so glad they’re getting onto the microcirculation issue. Dr Paul Cheney mentioned this and cardiac issues because he was so attentive to our condition. But of course, he was ignored.
Dr Cheney also discovered that many ME patients have lost their finger prints due to microcirculation problems. Yes, I have. Lately i have also developed red toes, sometimes painful and going purple under some conditions. I also get terrible tingling in the feet and legs and sometimes shooting pains in the veins. Do other people here have these problems?
I had an echocardiograph about 20 years ago which showed narrowing of the diameter of the inferior vena cava, leading to an inference of low blood volume. That should all lead to a strong hypothesis that I have the problems described above. Yet, I hardly ever hear of findings from an echo or of it being done.
Roll on the research and drug development!
I don’t know if you’ve read much about COVID or Long COVID (researchers are still arguing about whether or not that’s the same as ME/CFS). This issue is relatively common in COVID, to the point where treaters have dubbed the problem “COVID toes”. Have you looked into nattokinase, lumbrokinase, serrapeptase or pharmacological anticoagulant therapy?
Thanks Kira. I’m watching LC but I hadn’t heard of COVID toes yet. (I haven’t had COVID.) We certainly have some similarities, even if they’re not exactly the same thing.
I haven’t tried taking any of those things. I’ve only recently become strongly aware that these issues might be affecting me. I haven’t seen a specialist about them and I’m unlikely to. I’m housebound and don’t see myself having the stamina to try and find the correct doctor for a diagnosis, if there is one! I also have trouble taking things, so the opportunity goes wasted!
Check out this! Yet another ME/CFS connection….:)
https://www.aad.org/public/diseases/coronavirus/covid-toes
COVID toes can develop at any age
Doctors around the world have noticed that some patients who test positive for the coronavirus develop discolored and swollen toes.
The condition may develop on your toes, fingers, or both. From what we know, it seems that most people develop this only on their toes, which explains the name “COVID toes.”
The swelling and discoloration can begin on one or several toes or fingers, according to Amy Paller, MD, FAAD, who is a board-certified pediatric dermatologist and Chair of Dermatology at Northwestern Feinberg School of Medicine. At first, you might see a bright red color that gradually turns to purple. COVID toes can also begin with a purplish color.
Never mind “covid toes”….I had covid feet…my entire foot x2
We’re purple,very cold extremities…even my nose is red
Whoa! Have you been able to resolve that using POTS or OI treatments?
I took one single dose of horse ivermectin. Completely changed the coarse of this horrid illness.
Like the iver. Instructions state…”if your horse becomes itchy all over and is rolling itself on the ground,this means you’re horse has filaris”
I’m nowhere near normal buts it’s gained me some ground considering I was like whiteny Dafoe for decades.
I keep thinking, if whitney was all over traveling he may have picked up parasites that can’t be seen by conventional methods.
After decades of low white cells….after the ivermectin, the white cells are up to normal but my reds are still low
My once GERD ,so bad that it was pushing blood out my nose, has receded but still present. I’m pretty sure I was on deaths doorstep
I have heard of all of those things – color changes in the toes – I think David Systrom may have referred to them – and the tingling in the extremities (peripheral neuropathy) – and you have evidence of a narrowing in that big vein that brings blood to the heart.
To my understanding that fits perfectly with the problems with preload (reduced blood flows to the heart) that Systrom has found and with the “rigid tube” hypothesis from Wirth and Lohn – and their ideas that problems with the vasa vasorum affect the veins in particular.
It’s possible that your system – and others – have adapted to the low blood volume by keeping the big blood vessels smaller than usually.
You may just have been really ahead of your time.
Thanks, Cort. Yes, I think I or my then doctor nay have been ahead in some respect. He had the echo done, then ignored the results, apart from saying I’ve got ‘a weak heart’! Then went on encouraging me to exercise which I wasn’t good at. He was very attentive but was treating ‘fatigue’ and there wasn’t much knowledge around in 2001.
Yes- he probably got it backwards. Not many people were thinking of blood flows now. It really took David Systrom and his invasive exercise studies to put the attention back on the blood flowing into the heart.
If exercise made the blood flow problems worse -which I assume it would – then it would just make things worse – ironically causing the heart to get smaller and weaker – not stronger.
If this theory is correct then would you expect to see patients presenting with high blood pressure?
This system is so complex that I really don’t know. Certainly an increased heart rate and increase in blood pressure is one possible compensatory reaction. Klaus Wirth, though, noted that a high histamine response in the blood vessels makes it virtually impossible to close them down again.
For anyone interested in pursuing a micro circulation enhancement option, I have used a Bemer mat for several years. It is an expensive option. I personally feel benefit from it and never skip my daily sessions (8 minutes 2x day).
Re Claudine and Fasciatherapy
See the work of Jill Miller and her books Role model,Body by Breath. Are people here aware of her work?
Yes, “HypoPerfusion of the Brainstem” researched long ago in me/cfs
It is shocking to me how primitive knowledge about the vascular system is considering it’s the most basic and fundamental system. A lot of these things mentioned I could’ve deduced logically with a middle school level education but these scientists struggle to wrap their brains around. But alas, good on them, and I thank them, better late than never.
Interesting. but the nervous system seems hyperactive during a stress too and the response is often strong? Why…
If it’s of any insight I may have found the cause(or a massive contributor) to my ME/CSF. A mutation in MYLK enzyme which activates smooth muscle cell contraction. Defective smooth muscle contraction would lead to exactly what is described by this study. There are people who have a mutation in ACTA 2 gene which leads to severe MSMDS(Multisystemic Smooth Muscle Dysfunction Syndrome). They get excess vasodilation since the smooth muscle cannot contract, they get POTS/Impaired gastric motility/etcc. Basically anything that is composed of smooth muscle cells malfunctions. I have autonomic neuropathy and possibly EDS as my skin is hyperplastic although I was genetically negative. This all combines to make it literally impossible to compensate for being up straight as my vessels(veins) not only do not contract, but they also do not get the nerve signal to contract(neuropathy) and they expand drastically(EDS)
How did you find that mutation?
It is a gene that was part of the connective tissue panel my Dr ordered. It isn’t a connective tissue disorder but included in CT panel because it leads to aortic aneurysms like CT disorders. Following up with Mass General vasculopathy team to investigate if I have some form of MSMDS, it is relatively rare. John Reiter foundation here in Houston research MSMDS but I had no aortic complications so they cannot see me. Basically MSMDS looks a lot like Dysautonomia except it is an end organ dysfunction. The end organ being the smooth muscle cell.
Wonder if Bethanechol could have an impact on this condition?
Dr David Healy’s currently looking into Bethanechol and Benztropine to see if it helps SSRI withdrawal, but only micro dosing for no longer than 6 months.
Although MECFS is different to Ssri withdrawal, he believes they have overlapping symptoms.
Take a look at this link.
https://digitalcommons.wku.edu/ijesab/vol8/iss9/9/
Im useing BEMER therapy for ME/cfs for one year now and ar slowly improving. Get the diagnose in 2008.
I find this flaccid tubes theory interesting. I have mild ME/CFS and hypermobility (possibly mild EDS). I have recently started swimming in a heated pool and found that I can swim for longer than I can do other exercise, I don’t get tired like I do when walking and I feel great afterwards. I’ve thus wondered whether exercising horizontally as in swimming, coupled with the compression effect of the water is helping my exercise tolerance.
Or perhaps the heated pool is doing a sauna like effect?