

Health Rising’s Sleep Series
- Pt. I – Dr. Bruck Interview – Bronc kicked the series off with an interview of Dr. Bruck – a retired sleep researcher whose son has ME/CFS.
- Pt. II – Ruhoy and Kaufman on Sleep – an overview of a fascinating talk by two long-term ME/CFS/FM and chronic illness experts: Dr. David Kaufman and Dr. Illene Ruhoy on sleep on their Unraveled Patreon podcast.
- Pt. III – A new sleep drug for fibromyalgia? A look at Tomnya – a sleep/pain drug Tonix Pharmaceuticals is submitting for FDA approval.
- Pt. IV – an interview with Dr. Mullington, a long-time sleep researcher and ME/CFS expert who, courtesy of the Open Medicine Foundation, is using cutting-edge technology to further understand sleep in ME/CFS.
Dr. Bruck on Sleep and Chronic Fatigue Syndrome (ME/CFS)
(Thanks to Bronc for another guest post – this time focusing on the unrefreshing sleep that permeates this disease. In it, Bronc talks with a sleep researcher, Dr. Dorothy Bruck, whose son has ME. This is Pt. 1 of a 4-part series on sleep)
Just before Xmas 2010, I was overcome by a bout of Swine Flu. After the holiday, which was a complete blur due to sickness, I went back to work in January feeling very weak.

I was working over 50 hours a week in a very stressful and physically demanding job which I increasingly struggled to keep onto, partly due to the lack of sleep/unrefreshing sleep. I noticed a considerable decline in my ability to do some of the basics of my job as I struggled to concentrate, and felt increasingly unable to keep up with the very demanding target-driven regime at work.
Trying to teach a class of 30 teenagers can be hard work at the best of times, but when you’re getting 4 hours of unrefreshing sleep, it can be a nightmare. Once I received my diagnosis of ME, one of the first things I asked my GP for was a course of sleeping tablets to help me overcome the worst of the insomnia.
Since my diagnosis, unrefreshing sleep and insomnia have been my constant companions. Sadly, none of the health professionals and scientists I’ve spoken to over the years have been able to offer much insight as to what is causing this and what might help treat it.
As we all know, sleep is the foundation stone of good health for anyone. For those of us who live with dysfunctional sleep all the time, it can be very debilitating and have a considerable knock-on effect on the other symptoms of our illness.
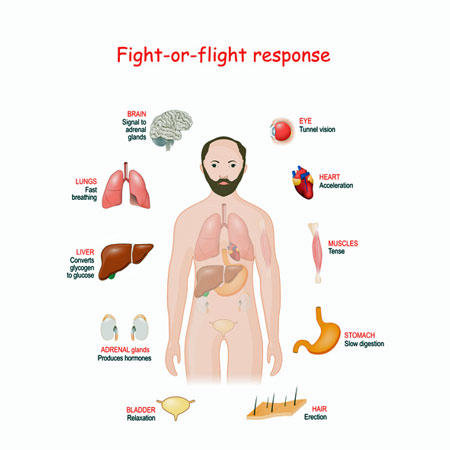
Several studies suggest that an enhanced sympathetic nervous system, or “fight or flight” response, is impacting sleep in people with ME/CFS.
A 2023 review of sleep studies found that ME/CFS patients spend a longer time in bed, take longer to fall asleep, spend more time awake after they’ve fallen asleep, have reduced sleep efficiency, decreased stage 2 sleep, more Stage 3 sleep, and longer rapid eye movement sleep latency. That study suggested that altered sympathetic and parasympathetic nervous system activity was keeping people with ME/CFS from getting good sleep.
That conclusion echoed the results of several studies. Back in 2007, a CDC study found that a similar sympathetic ANS dominance prevailed in ME/CFS patients during sleep. A small 2018 study concluded that people with ME/CFS had lower parasympathetic tone in deep sleep (less “rest and digest” during deep sleep) and higher sympathetic nervous system activity (more “fight or flight) overall while asleep. Finally, in 2020, an Australian sleep study concluded that “Autonomic hypervigilance during the deeper, recuperative stages of sleep is associated with poor quality sleep and self-reported wellbeing.”; i.e. the deep, restorative stages of sleep weren’t as deep or restorative in ME/CFS as they were in healthy controls.
Dr. Dorothy Bruck

Dr. Dorothy Bruck’s son has ME.
I recently spoke with Professor Dorothy Bruck about her insights into some of the sleep issues which affect people with ME.
Emeritus Professor Bruck’s main area of research interest and expertise is sleep and sleep health. She has been thinking about, and working with, many aspects of sleep for about 40 years. Professor Bruck has had a long academic career at Victoria University in Melbourne, with particular expertise in sleep/wake behaviour, mental health, chronic fatigue syndrome, waking thresholds and human behaviour in emergencies.
She has an international research reputation, with over 120 peer-reviewed full-length publications, $2.5 million in competitive grant income, dozens of invited international and national professional speaking engagements, and numerous awards. Professor Bruck’s research has been regularly featured in the media, including Time Magazine and New Scientist. Apart from her academic work, Professor Bruck has worked as a sleep psychologist and, until recently, she was Chair of the Sleep Health Foundation (Australia). She is now semi-retired and lives in the Far South of Tasmania, Australia.
The Gut-Sleep Connection in ME/CFS
Noting that increased levels of faecal gram-positive bacteria have been associated with ME/CFS symptoms (cognitive problems – concentration, excessive irritability, confusion as well as impaired motor coordination), Dr Bruck’s 2015 study used erythromycin to reduce down gram-positive bacteria in individuals with high levels of them. The antibiotic substantially improved sleep times and sleep quality in some individuals, but other symptoms remained.
Dr. Bruck’s larger 2018 follow-up erythromycin/probiotic trial in ME/CFS patients with high gram-negative bacterial counts (Streptococcus) again suggested that the gut may play a role in the poor sleep found in ME. The study found that reduced Streptococcus levels were associated with better sleep (fewer awakenings, greater sleep efficiency and quality) and cognition (attention, processing speed, cognitive flexibility, story memory, and verbal fluency). (Mood and fatigue, however, were not altered.)
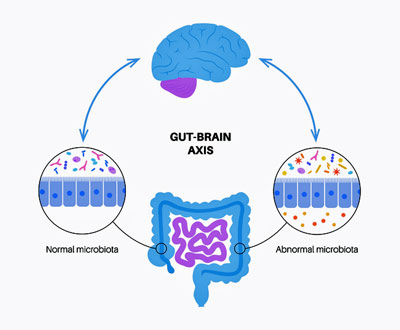
Dr. Bruck’s and other studies suggest that our gut flora may be impacting sleep.
Other studies have shown that people with insomnia typically have dysregulated gut flora – a common finding in ME/CFS. Similarly, reduced levels of short-chain fatty acids such as butyrate have been found in both ME/CFS and insomnia. Studies suggest that alterations in the gut microbiome may even be contributing to the changes in circadian rhythms and sleep patterns that Dr. Bruck outlines below, and some studies suggest that gut flora or microbiome manipulation could help. A study using a probiotic bifidobacterium called Longum 1714 improved sleep quality and increased energy/vitality in healthy controls.
5-Hydroxytryptophan (5-HTP) was able to improve gut health and sleep in older adults who were experiencing poor sleep. Similarly, a recent animal study found that sleep deprivation both altered the gut flora and increased anxiety levels. Melatonin, a common sleep supplement used in ME/CFS, may work, when it does, in part by benefitting the gut flora. On the whole, though, a review of probiotic and prebiotic use to enhance sleep concluded that while some evidence suggests that altering the gut flora may help with sleep, more and better studies are needed.
THE GIST
- Bronc returns to talk with Dr. Donna Bruck, a sleep specialist, about a problem – unrefreshing sleep – that has dogged him and so many others since coming down with ME/CFS.
- Dr. Bruck is an internationally recognized sleep researcher whose son has had ME/CFS for many years.
- Dr. Bruck co-authored two trials, both of which found that using an antibiotic (erythromycin) to change the gut flora in ME/CFS was helpful with some aspects of sleep. Several other studies outside of ME/CFS have been able to connect alterations in the gut flora (the bacteria found in the gut) with sleep issues. The science is still out, but some have found altering the gut flora may be able to help with sleep.
- Dr. Bruck reported that altered sleep patterns (where the person is unable to sleep when they want to) may arise from conditions often found in ME/CFS, such as sleep apnea, insomnia, and circadian rhythm disorders.
- For instance, the fatigue in ME/CFS may lead to irregular sleep patterns where the person sleeps episodically (i.e. naps) across the 24-hour period resulting in their no longer getting their main sleep when their body expects it. This can lead to poor and unrefreshing sleep.
- Delayed sleep disorder – where a person stays up too late and then sleeps into the day – can also result in poor sleep. Causes of this may be too much napping, insufficient exposure to light in the morning, and reduced activity.
- The poor sleep in ME/CFS can also result, however, from biological causes of the illness such as impaired melatonin secretion or other imbalances in the many hormonal metabolic or neurological factors.
- Dr. Bruck reported that ANY ongoing poor-quality sleep, whether it is un-restorative sleep or disturbed sleep, will affect a range of ME/CFS symptoms, possibly all. Pain and brain fog are likely to be particularly affected.
- A researcher recently showed that ‘even modest nightly changes in sleep quality within an individual can result in significant increases in pain and anxiety’. Interestingly, sleep loss also impairs blood vessel functioning in the parts of the brain (insula, anterior cingulate, amygdala) that have been associated with ME/CFS as well.
- Many unanswered questions exist concerning sleep and ME/CFS. Is it sleep fragmentation, sleep disruption, and/or lower EEG delta power, or something else that is causing sleep to be so unrefreshing in ME/CFS?
- The Open Medicine Foundation recently funded the first major sleep study in ME/CFS in year. An interview with Janet Mullington, the lead researcher, is coming up.
The Bruck Interview
Q1. How did you get involved in the field of M.E. research?
I have been a sleep researcher since undertaking my Honours degree in 1978, with a particular interest in disorders of excessive daytime sleepiness such as narcolepsy. In 2010, my teenage son was diagnosed with ME/CFS, which left him bed and recliner-bound for about 10 of the next 15 years. Remarkably, he has now improved sufficiently to hold a job with flexible hours. While he was very sick, I met ME/CFS clinicians and researchers in Melbourne and we managed to obtain funding for a series of studies focusing on sleep and gut microbes. We have since published this research, with Melinda Jackson and Amy Wallis as the first authors.
Q2. In October 2021, the National Institute for Clinical Excellence in the UK issued a new guideline for the treatment and care of people with M.E. This guideline recognized that for a diagnosis of M.E. to be made, people had to suffer from four key symptoms. Unrefreshing sleep or non-restorative sleep is recognized as one of the core symptoms of the illness. The sleep disturbance experienced by pwME can be broken down into two categories: disturbed sleep patterns and unrefreshing sleep.
Despite this, with remarkably little research being conducted into this core symptom of the illness, we still have just a very general idea of what’s involved in it. How would you explain the sleep dysfunction experienced by pwME?
I think the dichotomy between disturbed sleep patterns and unrefreshing sleep is quite useful, keeping in mind however, that a pwME/CFS may have both. Neither are unique to ME/CFS.
Disturbed sleep patterns (where the person is unable to sleep when they want to) may arise from co-morbidities with ME/CFS, such as sleep apnea, insomnia, and circadian rhythm disorders. Sometimes the latter two disorders may begin with, or be perpetuated by, behavioural changes in sleep/wake behaviours that lead to disturbed sleep.
For example, the fatigue associated with ME/CFS may lead to irregular sleep patterns where the person sleeps episodically (i.e. naps) across the 24-hour period and the circadian (24-hour) rhythm becomes confused. The person’s sleep quality suffers because they are no longer getting their main sleep period in a single block at the time the body clock expects it.
A different pattern that we may see in ME/CFS is Delayed Sleep Phase Disorder, where the person is very much an ‘evening’ type, going to bed late and getting up late. People who get insufficient outdoor light during the daytime are particularly susceptible to this. Sometimes their body clock begins to ‘free run’ and each night they may go to bed later than the previous night, so their ‘day’ may be 25 hours instead of 24 hours.
Behavioural changes that may precipitate insomnia include decreased sleep drive (or sleep pressure) arising from reduced activity, significant napping during the day, reduced exposure to daytime light, worry at night about the consequences of having ME/CFS, and/or longer time in bed trying to sleep than the actual sleep duration that person may need.
An example would be, due to boredom and/or feelings of fatigue, turning lights off from 9 pm to 8 am each night (i.e. 11 hours trying to sleep) when the person may only need 8 hours of actual sleep. Best if lights-out time equals the sleep time required. The research shows quite clearly that treatment with Cognitive Behavioural Therapy for Insomnia (CBTi) can provide significant improvements in people whose sleep has been impaired by such behavioural factors, and online programs are available.
On the other hand, disturbed sleep patterns in pwME/CFS may arise, not from behavioural factors, but from factors associated with ME/CFS itself, such as impaired melatonin secretion or other imbalances in the many hormonal or metabolic or neurological factors that we are only now beginning to understand affect sleep patterns. Such imbalances may, in fact, lead to either disturbed sleep patterns or unrefreshing sleep.
Unrefreshing sleep occurs across the population, both in people with a range of clinical conditions and sometimes in people with no diagnosed medical problem. It is usually described by self-report. It is likely to be a very heterogeneous phenomenon.
A study by El-Mekkawy Leqaa et al. (2022) noted a significant change in delta wave power (deep sleep) in the temporal brain region in those with unrefreshing sleep arising from sleep apnea, compared to controls. In our review of sleep patterns in ME/CFS (Jackson and Bruck, 2012), we concluded that technological advances in the assessment/monitoring of sleep may lead to further understanding of how the micro-structure of sleep may differ between those with self-reported unrefreshing sleep compared to quality sleep.
Q3. Anecdotal evidence from some pwME and a few research studies suggest that the sleep disturbance that people experience can have a significant impact on their cognitive abilities. How prevalent is this? What may be causing the sleep disturbance to impact people’s cognitive function?
Any ongoing sleep disturbance will affect a person’s cognitive abilities. Attention, concentration, memory, and reaction time may all be affected in some way depending on: (a) their overall health (physical and/or mental); and (b) individual differences in how poor sleep quality affects an individual. It seems reasonable to think that a pwME/CFS that includes the symptom of brain fog would be affected by the cognitive impairments we associate with poor sleep in an additive way.
Q4. Is there any evidence that non-restorative sleep is impacting other symptoms which pwME experience, such as pain?
I believe that ANY ongoing poor-quality sleep, whether it is unrestorative sleep or disturbed sleep will affect a range of ME/CFS symptoms, possibly all. Pain and brain fog are likely to be particularly affected.

Dr. Bruck noted poor sleep is likely contributing to brain fog and pain in ME/CFS.
With regard to pain, we know that sleep loss increases the experience of pain. Krause et al (2019) showed that acute sleep deprivation amplifies pain reactivity within the human primary somatosensory cortex, lowers pain thresholds and that ‘even modest nightly changes in sleep quality within an individual determine consequential day-to-day changes in experienced pain’.
(In his 2019 publication,”The Pain of Sleep Loss: A Brain Characterization in Humans“, Krause showed that sleep deprivation enhances pain responsivity within the primary sensing regions of the brain’s cortex (somatosensory cortex) but blunts activity in other parts of the brain that reduce pain levels such as the striatum and insula. Abnormalities in both of these brain organs have been found in ME/CFS.
Krause’s 2023 study showed that sleep loss also impairs blood vessel functioning in the parts of the brain (insula, anterior cingulate, amygdala) that have been associated with ME/CFS as well. If you feel anxiousness that you can’t explain, it may simply be due to sleep loss. A 2020 study “Overanxious and Underslept” found that even small reductions in the time asleep “predict consequential day-to-day increases in anxiety.”
Q5. Having a clearer understanding about the pathophysiology of non-restorative sleep in pwME may lead to better treatment options for patients. Are you aware of any clinical trials that are exploring treatment issues for non-restorative sleep in pwME?
Unfortunately not.
Q6. Many people with M.E. report that there is a direct link between the degree of their non-restorative sleep and the depth of the fatigue they experience the next day. What research has been done into this particular issue and what were their findings?
To my knowledge, this issue has not yet been investigated in pwME/CFS. However, cognitive fatigue as measured on a range of working memory tests (Benkirane et al, 2022) found that the main effect of sleep fragmentation was to increase subjectively reported fatigue rather than reduce cognitive test performance. This study, using healthy participants, highlights the difficulties in objectively measuring fatigue, as many people can rally their mental resources for short-term testing in a research setting. This may have little to do with how fatigue is experienced in real-life settings.

Many questions exist regarding sleep in ME/CFS. An Open Medicine Foundation-funded sleep study will answer some of them.
Q7. What further research is required to investigate the causes of non-restorative sleep and the impact this has on cognitive function, fatigue and pain in pwME?
There are so many unanswered questions. The first step for any such research is to have a standard definition of non-restorative sleep. Is it a certain level of sleep fragmentation? Sleep disruption? Lower EEG delta power? Subjective report in the light of an otherwise normal sleep diary? Is reported non-restorative sleep the same for someone with sleep apnea, vivid dreaming or ME/CFS?
*Thanks to the Open Medicine Foundation, the first major sleep study in ME/CFS in years is underway. This study will use cutting-edge technologies to explore the sleep question in ME/CFS in ways that have not been done before. Health Rising’s interview with the lead researcher – Janet Mullington – is coming up. Stay tuned!
Check out two ME/CFS.FM and long COVID experts talking about sleep in Pt. II of Health Rising’s sleep series.






Oh, do I have sleep problems! I’ve had three sleep studies and they have been no help–except to be able to get Modafinil. I often fall asleep during the day despite “sleeping” for 7 hours. All night I have night sweats and frequently wake up with soaking wet clothes. (Meds don’t work) I’m constantly tossing and turning because of pain and often wake with a headache. Apparently my heart rate is very erratic and I hardly ever get any deep sleep. I also wake to pee several times. I’ve been told I have multiple hypoxias but no apnea (my nose is completely blocked on one side–maybe that’s part of the problem), but I don’t meet the Medicare criteria for a C-Pap. And C-Pap is the only thing the doctors can recommend! So what do I do? It’s so frustrating!
Thank you for bringing this aspect to our attention! Poor sleep might be a factor in brain fog–not to mention everything else.
Thank you, Cort, for this interesting and very relevant information!
I wake up after about four hrs sleep, sometimes, less, with my heart racing.
I’ve taken four sleep courses with individual coaches. And I’ve read maybe 7 books. When I wake up, I’ll calm myself down, but often I’ll lay there peaceful but no sleep . If I get up for a few hours and then back to bed . Sometimes I can get maybe another hour of sleep, often not. It’s now the very worst problem I have after having CFS for over 40 years. One can’t have any quality of life with little sleep.
I use Clonazapam over the years but know it’s habituating do limit how many times I take and try to just take very little. The hyperarousal is terrible and if I know I have to do it go somewhere the next day, well, there goes any good sleep at all.
I’m hoping for the day we can go to a dr and they will understand and know all about the problems we have with CFS and instead of smirking at us, will actually help us…
I’m not being funny but wasn’t Bronc the author of this interview with Professor Bruck not Cort?
Yes Bronc is the author of this blog. I will, however, take credit for posting it! 🙂
Oh yes, good point. Big thanks to Bronc (and Cort for posting it and every thing else)!
I can’t think of anything that impacts me more than poor sleep. The only things that have somewhat consistently helped have been Wyld high THC gummies and a non THC cannabinoid tincture.
I also know not to eat much close to bedtime, to have a regular bedtime and not do much physical exertion in the late afternoon.
Here are some reviews of Cannabis products that have helped with sleep
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/cannabis-fibromyalgia/cannabis-fibromyalgia-chronic-fatigue-reviews/
Poor, fragmented sleep has always been a problem for me. I wasn’t the best sleeper long before I became ill. The only time in my life I’ve ever slept well and had anything close to refreshing sleep was when I was on micronized progesterone as part of my HRT. It would literally knock me out. That’s why I took it only at bedtime.
I’ve found that getting better sleep doesn’t necessarily improve my symptoms but having poor sleep or consecutively skipping my daily naps will make my symptoms worse.
I track my sleep using a Fitbit. I also track my avg resting HR which, for me, is key to preventing a crash. A “good night’s sleep” helps to keep my avg resting HR down.
Resting heart rate is a key indicator for the Oura ring as well – which now has a nice “resilience” feature.
Hi Lori,
question why was on HRT? If you have benefited from progesterone, wouldn’t it be a good idea to find a provider for complete HRT (progesterone, estrogen + DHEA), but ONLY if bioidentical.
There is a lot of benefit for bioidentical hormone replacement your whole life, lesser heart attacks, alzheimer and on it goes…
I am past menopause + very big problems with sleep.
With progesterone at least I fall asleep. I keep a partial dose to take when I wake up during the night, say 3 to 4 a.m. not to late, cause then I feel tired during the day.
It’s no miracle cure but it helps.
I use transdermal creams for bioidentical hormone replacement, with a provider that ships the hormone tests + creams internationally. Take a look at glow natural wellness, on the internet my provider, for info.
I hope that helps? Stephanie from France
Hi Cort, Thank for all you do— with kindness and smarts. Regarding the gummies and tincture: for those of us new to THC and cannabinoid products, could you offer any guidance about where to purchase (and any constraints etc. in doing so?) Much appreciated!
I’ve able to easily purchase Wyld Cannabis infused Elderberry Gummies 2:1 THC:CDN in Nevada. Wyld looks like its a pretty big company and you can probably get it if your state allows. https://wyldcanna.com/
The Rainbow Children CBD-CBG-CBN tincture (no THC) by Angel I picked up in Boise, Idaho is surprisingly powerful and may be more available. (Idaho does not permit the sale of THC products). I like that it doesn’t have THC which can result in increased tolerance. It is very relaxing and it lasts a long time. Use it judiciously – just a couple of drops under the tongue.
https://www.nuggetcbd.com/product/angel-111-tincture-cbd-cbn-cbg-4500mg/
Many thanks for sharing, Cort.
@Cort,
Cannabis gummies work for me too in the less common problem I have of falling asleep. (Staying asleep without all my disturbances is my big issue). Anyway, I want to mention ‘opium lettuce’ as an alternative or additional sleep aid when all else fails.
No, there is no ‘opium’ in this ‘lettuce’, but it really, really aids in sleep. It’s an extract made from a weed and was widely used at the turn of the century. Lactuca Virosa/Lactucarium. I buy the liquid extract from a small supplier in the southern U.S. who grows his own; wildlettuce.com. It only takes less than a tablespoon full.
Thank you for posting this. It’s a very important component of CFS/ME and the exhaustion and fatigue. I have been on Ambien for decades, which has its own set of problems. Sleep eating, foggy memories and brain fog. So far there’s no good answers.
Wow – Nancy that sounds like – to me a laymen – possibly autonomic nervous system issues (heart rate/sweating)- which fits with the research. Have you tried Trazodone – it may help with arousal at night if I remember correctly.
@Cort,
Finally I’m getting back to this thread. Thank you for your suggestion, but I’ve tried Trazadone. Indeed it makes me sleepy at first, but every single time I took it, I woke up–wide awake–at 5:00 a.m.! Not good.
I also think I have some sort of dysautomonia, but my TTT test supposedly indicated that I don’t. Go figure. I seemed to remember that you mentioned you had a similar result.
EDS literature (POTS common) has said since autonomic functioning is so dynamic, that several readings might be necessary and even then, it might not show up until much later than the 10 minutes (or so) that are used for the testing. Most doctors don’t want to mess around with additional tests so I think that’s one reason it isn’t found.
Even if some sort of disturbance is indicated, many doctor’s don’t want to try to treat because the drugs used to control things like POTS or NMH throw the whole system off. So one might not have the elevated HR but the side effect is that they are dizzy and suffer from pre-syncope–and even more fatigue. It’s a delicate balance–often difficult to achieve.
Hey, Nancy…I don’t know if this will help you or not, but, for me, night sweats is clear indicator that my EBV has reactivated. I discovered this because I used to be a patient of the late Dr. Lerner and he was a frequent tester of EBV. After a year, I was able to match up my symptoms with blood work. The most telling for me is night sweats.
In the nearly 9 years since I made the connection, it never fails…I will have a positive EA (early activation) of EBV via blood work. (And no, I do not always have a positive EA; later testing will show negative).
Anyways, I’m on Valtrex 1000 mg 2x a day, indefinitely. It REALLY helps. It takes a lot of stress (physical, mental, emotional) to make my EBV reactivate, now, whereas before, I would just continuously cycle in and out of reactivations.
@ Jilly,
I appreciate your comment and suggestion! I’ve had only one test to indicate I still carry EBV in my system. I don’t know if this is related, but I recently had Shingrix vaccines (three months apart) and each time I got a bad herpes reactivation–something that is usually uncommon for me.
Here I’m thinking that my night sweats had something to do with menopause, but maybe it’s a ‘something else.’ The problem with trying the Valtrex is that my doctors are very conservative and are probably disinclined to do that. “Show me the study.” Anyway, those night sweats started after I went off HRT in 2017 (had a little problem with early stage breast cancer) and rather then getting better, they have gotten much worse.
I have had long covid 3 years and ever since my sleep has been poor. I recently got a fitbit and found my REM and deep sleep are lower than the normal range for my age on many nights. I started taking maraviroc and it improved (along with my other symptoms of congestion, ETD, tinnitus, and brain fog memory). I went off and it got worse again. It’s and n=1 and anecdotal and I can’t afford the $1800 a month to continue much longer but perhaps someone should look into this in a study. For me the unrefreshing sleep is the worst symptom of long COVID.
Thank you Cort for such an important article. I am plagued by sleep issues as well. Sleep meds get me to sleep. (mostly) But I rarely sleep through the night.
Body pains cause me to be uncomfortable and wake in the night. Ibuprofen tends to help, but I wonder how much I am hurting my liver.
My sleep monitor app says I dream, but I hardly ever remember dreaming. I wake feeling worse than the night before.
You would think sleeping longer would help, but usually I just get a raging headache.
Appreciate your hard work in our behalf.
I think Ibuprofen tends to affect the kidneys more, and acetaminophen affects the liver (if I remember correctly).
I was using zopiclone for insomnia for a couple of years before my doctor insisted that I do CBT-I, saying that it was the “gold standard” of insomnia treatment. It was via zoom, facilitated by a psychologist. It was agony. The sleep deprivation portion of the program left me utterly exhausted and in pain. Very ironically, I was allowed to continue using zopiclone and trazodone, but when the peripheral neuropathy kicked in I was not allowed to use gabapentin because I hadn’t been using it before. The day the program ended I started adding gabapentin to my medication regime.
In spite of the unpleasantness I continue to keep the required sleep diary, and recently the sleep diary software has connected to my Fitbit, so the Fitbit record of my sleep gets transferred to the sleep diary. On average, I am in bed for an average of 9.3 hours and asleep for 8.2 hours.
Same doctor then required me to do an at-home sleep study. The result was that apparently I had severe positional apnea, but only for the first hour that I was ostensibly asleep. I seriously question that result because I don’t believe I was asleep then, and I had already told the sleep study people that I knew that I got choked up sleeping on my back and was already doing my best to avoid that position (sleeping prone). The doctor wanted me to repeat the study but I refused. A CPAP machine costs $$$ here, and I don’t wake up choking since I realized what was causing it.
I note that no matter when I go to bed I always wake up at the same time, so it is better to go to bed early. Most of the awakenings that my Fitbit records I have no memory of, on average 25-30 times a night for seconds at a time, except the on-purpose awakening to pee in the middle (more or less) of the night. My Garmin disagrees with the Fitbit, it only records 2-3 awakenings at most.
Thanks, Cort, for this interesting report. 35 years in, I think my sleep might be the worst element because of the way it never lets me recover. I started using a Garmin watch a few months ago, and it shows my sympathetic nervous system as dominant for almost 24 hours every day (rarely more than 30’/day in parasympathetic), which accords with the level of ‘fatigue’ and other symptoms, often being ‘wired’ and intermittent adrenaline surges through the night. I believe that if only I could get restorative sleep, I might begin to build back out again. As it is, 35 years of never having had restorative sleep (and it looks as though it may be even longer for some here) becomes cumulative and I wonder what impact this has not only on ME but for broadest health/longevity. I think there’s an urgent need to escalate ME research in this area.
I am someone with more than three decades of FM. Your battle to try to get restorative sleep is similar to mine. I can get about four decent hours of sleep. Then, I am up for about two hours, and I might be able to get a couple more less refreshing hours of sleep before I get up. The less sleep I get at night, the next day’s pain increases accordingly.
Commisserations. I’m about to get very diligent with vagal nerve stimulation, just in case, and about to go back on ivabradine which should reduce palpitations. Bit wit’s end these days, but there must be *something* that will break the cycle! Have you found anything that helps at all?
When I was at my worst
(Just like whitney dafoe)
I stared at the ceiling for aprox. 7 years all the while all hell was breaking loose(mcas etc)
ZERO SLEEP!
what got me out of that no sleep phase was a pair of earplugs with headphones on top. Just like Dafoe, the slightest drop of a pin would put me in a downward tailspin.i was one of those people that slept in a tent in my back yard to hold my job down, until winter (no tent)came….then I went down and never ever recovered.
Fast forward to now….I awake at aprox. 3a.m. every day no matter when I go to bed.
A half a puff of weed does a nice job of getting me to sleep if I puff at least 2 or more hours ahead of sleep.
I recently discovered my childhood homes (moved lots) in the city I live in were all in an area that NOW the city warns the water pipes have higher levels of lead than FLINT MICHIGAN!
And advises to NOT drink the tap water until the pipes are removed and installed new pipes.
HIGHER THAN FLINT!!
…and I drank that water in my growing years.those same houses would be painted with lead paint.every car in every city spued lead from their tailpipes until 1980.lead was everywhere back then….kids toys, jewelry.
Lead is responsible for hundreds of deaths for decades and decades. And ,yes, I damn near died! I now have kidney issues.
Thanks, Buckey. I need to give the earplugs and headphones a go; I wake easily at any sound, after having been a single parent for years, so maybe something like this could break the cycle.
Interesting. I recently heard that people born in the 60s and 70s may have a higher lead burden that those from other eras. I thought I was safe, because I had my blood tested, but apparently, only about 10% of your body’s lead can be measured in the blood.
There are charts that show the crime rate steadily dropped in the years after lead was taken out of gasoline. There’s lots of info online about the history of lead and just how seriously a person can get from lead.
Hi Cort, ME sufferer for 27 years almost completely bed bound these days. I almost feel that I could have written this report myself!
I have tried almost every medication on the market Clonazapan works best for me for a couple of days then nothing.
But wife’s home made cannabis infused Pk brownies are the only things that really work. Indica not sativa. A batch contains 6 grams of bud and lasts me a month. One eaten about 10pm kicks in about midnight and I sleep for about 8 hours. I don’t plan much before 11am but thereafter I have relatively normal day, don’t need to nap or take any more pain medication til the evening when I have a 300mg Gabapentin for newly diagnosed polyneuropathy.
Every few months I take a tolerance break for a week or so, but I find it really difficult after the first 3/4 nights the sleep is poor and the pain much much worse.
I’ve tried micro dosing during the day but it makes the night time dose not as effective.
I know we are all different but this regime has given me a quality of life I can live with.
Regards Peter
I’m really surprised at how helpful cannabis can be with sleep and pain….it’s a really nice relaxant. No high involved. There’s a football player who came down with a horrible neurological disease. At one point the choice was to be on a ventilator I think it was for the rest of his life. Without cannabis he would have signed off but he’s apparently still with us.
PEA has been helpful with both sleep and pain, and it doesn’t seem to have any miserable side effects.
Thank you. Not come across the before 🙂
PEA attaches to cannabinoid receptors, but it is perfectly legal. It creates no ‘high’ like THC and can be purchased on Amazon. It is more widely used in Europe than the US. “PEA anti-inflammatory actions allowing for a reduction of peripheral and central sensitization are mediated via both neuronal and nonneuronal cells.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3500919/
Thanks, Karen 🙂
Two years ago I suddenly developed severe insomnia. I went on to the supermarket website and ordered everything with the word sleep in it. They were mostly herbs and some magnesium. It worked like a charm.
After being about 15 years on hormonotherapy for menopause, my GP insisted that I stop. I did. But my insomnia, unrefreshing sleep, etc., became quite worse. I convinced her to put me back on it and it is better. I am back to regular not-so-good-sleep. Benadryl is my best medication. That also my GP wants me to use sparingly. So after a few bad nights, I “treat” myself to a Benadryl.
It’s equally sad and frustrating that the issue of non-restorative sleep doesn’t get the attention it deserves given it’s a core symptom of ME. Do you think that’s due in part to the lack of understanding of the underlying biology of sleep in general?
I’ve been reading everything I get my hands on during the last decade relating to sleep and mecfs and the only sleep researcher I’ve ever been impressed with was Dr. Maiken Nedergaard’s presentation during the Dec 8, 2023 MECFS Research Roadmap Webinar on YouTube. She specifically focuses on the neurobiology of non-restorative sleep.
My muscle aches and stiffness make it hard for me to fall asleep. When I go to bed, I play Buddhist chanting at very low volume. Then I can feel that aches and stiffness are physically reduced. Then I fall asleep.
There are a new class of insomnia medications which have come out in recent years in the US which are no sedating, non addictive and have a high safety profile in clinical trials. I have ME and am shortly going to try one of the new medications as more traditional sleep medications such as zoplicone don’t work for me. Below is a quote from the following article in the Journal of Clinical Medicine Feb 2023
Published online 2023 Feb 17.doi: 10.3390/jcm12041629 PMCID: PMC9959182 PMID: 36836164
Long-Term Use of Insomnia Medications: An Appraisal of the Current Clinical and Scientific Evidence
“The newest class of medications, the dual orexin receptor antagonist (DORA) drug studies have often included data on the efficacy and safety of 3 months or longer medication use.
The DORA drugs are a novel class of insomnia medications that work through a different mechanism of action compared to earlier insomnia medications. They bind to orexin receptors and inhibit the action of the wakefulness-promoting neuropeptide orexin.
Suvorexant was the first DORA drug approved for treating insomnia. Long-term (1 year) suvorexant treatment was evaluated in a multi-site randomized, placebo-controlled, parallel-group clinical trial [39]. Suvorexant at 30–40 mg was determined to be efficacious for subjective measures of sleep onset and maintenance, and safe over 1 year of nightly treatment. In total 69% of the trial participants treated with suvorexant experienced adverse events, as compared 64% of those treated with the placebo. The most commonly reported adverse event was somnolence.
In a 6-month placebo-controlled multicenter trial of another DORA drug, lemborexant [40], significant benefits in objective and subjective measures in sleep efficiency and wake after sleep onset were reported at 5 and 10 mg doses of lemborexant compared to a placebo. The majority of reported adverse events were mild or moderate.
Daridorexant is the most recent orexin receptor antagonist approved to treat insomnia. In investigational trials, daridorexant improved sleep quality measures, as well as daytime functioning in patients with insomnia [41,42]. A randomized, double-blind, placebo-controlled trial showed that the discontinuation of daridorexant (after 3 months) among individuals with insomnia can be completed without withdrawal or rebound symptoms.” [43]
I tried the Dora drugs when they first came out and I was awake all night. Made insomnia for me worse. I wish they had worked.
Did your insurance cover it? I’ve been told they are not covering orexin receptor antagonists yet.
I only got samples from my dr. So I didn’t have to pay anything.
No, I wasn’t using anything else.
This just didn’t work for me at all. Google on reviews for insomnia, Drugs.com. I look up any drug I’m going to try on this site to see the responses from others.
Thanks!
I would definitely get samples from your dr before you outlay any monies.
Were you on anything prior to it? Did it not work because you were dependent on a prior medication and did not titrate off of that first? Or were you trying it fresh, and it just didn’t work? I’m on eszopiclone, and I actually think it helps with brain inflammation because when I don’t take it, I cannot get into a deep sleep state like just after my concussion and early COVID when I had a lot of brain inflammation. I’ve not seen studies citing this, just feel like it affects inflammation from personal experience.
Thank you for this information. I have a PC that is willing to work with me. Anxious to try ANYTHING new to resolve this issue!!!
Interesting read. I’m new to health rising & it’s been invaluable to learn more about me/cfs. I caught covid in 2021 which progressed to me having me/cfs.
I noticed reading some of the comments that it’s mentioned about heart rate being elevated during sleep in the night which I’ve also noticed in myself. I got the samsung watch to record this & I’ve had readings of about 130-150bpm at random times during the night which seems to tally up with what’s being said here. I’ll be really interested to see the latest study on this. Another thing I’ve seen is my drop in oxygen during the night even though I don’t have lung problems. Last night down to 79%. My watch says I’m having not enough deep sleep & other nights I do, however I still wake up not refreshed & feeling terrible. I’m wondering if me is causing the sleep problems or whether it’s exacerbating the me/cfs.
Thanks for providing all this info. As I said its invaluable to us who want to understand what’s happening under the symptoms. I only wish my GPs were as interested.
This tallies with my experience too: sudden HR surges (not sure whether adreneline spike drives HR or other way round), wake up wired and hours to get back to sleep (if at all). Also just had two-night oxygen readings: I’m told I’ve not got sleep apnea and the readings average out to be acceptable, but there are distinct dips during the night and when I wake in the morning, but they don’t see these as significant. I did read that sleep studies in general average out numbers (O2, sleep stages, etc), with the result they miss data that’s relevant to ME and associated conditions, but I don’t think the research is yet there to argue their significance.
I agree, I think it would be helpful to look at these sudden dips in oxygen, especially as they drop so low to be considered a problem, or so I’ve read. Last night my oxygen dropped to 76% (not 79 as I thought) for 27 minutes, and I have no explanation, my watch didn’t even pick up snoring. And as for the heart rate stuff, you would think these sorts of things happen as a result of bad dreaming but I’ve never found this is the case, I just casually wake up for the toilet during the night and my heart is racing. Very bizarre stuff.
Yes, thanks, I think I’ll check them out. I know that Garmin et al oxygen measures are an indiciation rather than a definitive number, but I figure the hospital pulse oximeter should be more accurate. Similar to you, no idea what causes the surges/sudden wakings, but HR, respiration, HRV are all erratic when I’m sleeping; similar to Nancy (above) night sweats, up to the loo multiple times. There has to be significant information in there somewhere, but I don’t know how to interpret or, crucially, do something useful with it!
Oh ok interesting. I’ve actually seen on fb as well that there’s a new device called ‘visable health’ that’s designed for people with ME in order to manage pacing. The device will tell you that you’re overdoing it & to rest, by reading your HR & Oxygen. I think these studies would benefit from looking at the results of these things, plus smart watches as it’s good data they could analyse & find some common occurances. Looks like a great device too but the cost puts me off.
I have the nights sweats too. Not every night but it happens. One Dr suggested I may be perimenopausal so it’s hard to tell now if these symptoms could be ME or hormone related 🤦♀️.
You don’t have to answer as of course it’s sometimes a sensible subject, but do you think it could be hormones causing these symptoms for us? Or definitely ME related? I’ve only had all this since becoming ill.
Kind regards & I hope you’re having a well day.
Hi Donna, There will be people here who know way more about all this stuff than I do! Like you, night sweats but not every night. Mine preceded (peri)menopause, so I attribute them to illness (though I suppose the menopause years could also have added to that). A lot of people seem to be keen on Visible; despite currently using Garmin (and an Apple watch having led me to a dysautonomia diagnosis after decades) , I just can’t stand rating my symptoms all the time as it brings me down – but I think there are also phases where it’s really useful to do this to recognise patterns and triggers and try to work with them. Best wishes to you.
Heart rate spikes during the night could be due to hypoglycaemia. If your blood sugar is dropping too low you’ll have a spike of norepinephrine which would increase heart rate. Blood sugar dysregulation is not uncommon in ME/CFS and FM.
Doing a glucose tolerance test or wearing a continuous glucose monitor for a time could help to indicate any issues.
Another possible cause for heart rate spikes during the night is MCAS – Mast Cell Activation Syndrome. Typical advice is a low histamine diet.
Well Cort, with the plethora of symptoms we experience from this disease, at least you’ll never need worry about running out of topics to cover.
:). No kidding…If its not one thing, its the other – which has made this and diseases like it such a mystery. Look at rheumatoid arthritis – it’s bad enough ,but when people with RA get FM (they are at higher risk for it) things much worse things get because so many more things become haywired.
You ain’t kidding Cort! Don’t know how many years I’ve followed you, but its been lovely to know you’re there. YesRA, Osteo, FM, ME….Then the heart and gut. We seem to collect them!
Hallo All,
I am suffering from ME/CFS and MCS since 1989.
Sleep used to be a major issue for me.
My problem was resolved: For the past decade I enjoy great sleep and usually fall asleep right away.
Sharing what works for me:
# Not to sleep on my left side, because that desturbs my heart beat.
# A previous blog stated that ME-sufferers seem to have a unique form of type-2 diabetes. Therefore, AGAINST most advice, I eat a complete meal, shortly before I go to bed. (Two cups of fermented brown rice, two meat balls, slice of potatoe and a handfull of frozen green peas – it helps to control my blood sugar through out the night.)
# I massage the adrenal glands for 5-6 minutes, just before I get into bed, because the natural day-night-cycle of my adrenal glands get desturbed.
#Under the tongue: Homeophatic Tissue salts: 2 tablets KaliPhos nr.6 and 3 tablets MagPhos nr.8 just before bed, AND each time I wake up during the night.
# I have to sleep on a very firm mattress.
# I am able to exercise during the day: That also helps me to get a good night’s rest.
Nicolas, thank you . I will definitely try not sleeping on my left side and eat carbohydrates before going to bed. Intuitively I have “known” about these two elements but not enough to systematically do it .
Forgot to mention:
# I sleep with ear plugs, because apparantly ME does not allow our brains to block out sounds during the night. (I put a bit of coconut oil on the earplugs, to make it more comfortable)
Thanks, Nicolaas. It’s great to hear that your sleep’s improved so much. I’ll be giving these things a try 🙂
I’ve had ME for 20 years, now severe. Severe insomnia has made me so ill and frightened. I only achieve usually 2-3 hrs dozing. I cannot sleep in the day. I am never tired always alert.
I now have MCAS/EDS as well, which makes the insomnia worse. I cannot take any sleeping aids as I react badly to all medications, antihistamines,, magnesium etc.
No one understands, the sleep clinics, doctors, specialists. It is my worse symptom as it’s slowly killing me making these diseases worse.
i cannot plan anything due to this. MCAS causes me to react to insomnia as well so the day time is very frightening and difficult to get through…then as night draws close I feel I won’t cope with another night of just lying there in total distress.
I’ve tried everything, all the electronic gadgets, drugs, clinics endocrinologist,CBD/THC.
Try lorazepam or oxazepam ask your doctor if it is possible for you
Hi, I’ve recently persuaded my GP to put me on a new non BZD medication for insomnia called Daridorexant. It works by dampening down the receptors in the brain which promote wakefulness. It is the most recent orexin receptor antagonist approved to treat isomnia. It has really helped keeping me asleep and not waking up every hour which has been so debilitating.
I appreciate the information provided in this article. I’m in the process of developing a sleep course for people with fibromyalgia and this has added some info I wasn’t aware of, especially the relationship to the gut (I am also developing a separate gut health/diet course so love seeing the potential link between the two)
Learning about and optimising sleep and circadian rhythms is a foundation of my fibromyalgia remission. I implement multiple strategies daily to ensure I get good sleep. Early morning sun, low lighting at night, regular bedtime routine, living somewhere quiet and dark, avoiding stimulants, morning exercise, managing stress and body based relaxation techniques when I’m feeling too energised. I spent years re-wring my nervous system out of sympathetic dominance which had a significant impact on my sleep quality.
I always have valium on hand for the occasions when I’m lying in bed for 3 hours and am still awake (though I limit this as I don’t want dependance and know it’s not optimal sleep anyway)
ME/CFS did increase my sleep problems, but
getting off Vyvanse, onto Modafinil, and adding Trazodone seemed to do the trick for a while. Now I have to take an aromatase inhibitor, and my sleep is even worse than it was before. I doubt there are any solutions…
Hi All a very interesting read and I can relate to much of what is being said. I have had ME/CFS for 45 years and sleep disturbance has had quite a role to play.
At Menopause I started having Panic attacks and severe night and day sweating. Because of blood clotting issues HRT was not appropriate. After 10 years of taking a low dose SNRI I decided I would be OK and slowly came off it only to find a rebound within 3 months. Unfortunately I think I am now stuck with this medication!
I have been on Clonazepam for many years and am slowly reducing the dose as I get older. Being treated like a drug addict is no fun especially when a dose is low and never increased!
About 3 years ago my PANIC at 5am became almost unbearable along with the sweating.
I tried medicinal cannabis with some success.
I also believe that Low Dose Naltrexone has been useful.
My rapid heart rate was finally acknowleged and now being treated with medication which has lowered it to a normal resting rate overnight
During the COVID years and having got a smart watch and pulse oximeter and I noted that I was having hypoxic episodes overnight.
I requested Sleep studies and now have a C-Pap machine which has almost completely reduced the early morning panic but not the sweating.
I am sure this is due to HPA axis dysfunction
I see an Osteopath monthly and find my vagus nerve is always malfunctioning
My endocrinologist and I figured out that my early morning awakenings are due to me having almost no butyrate bacteria, which are needed to stabilize your blood sugar levels. Since I have basically no butyrate being produced in my gut, my gut endothelial cells have to siphon glucose from my blood to function. This causes me to get low blood sugar about 4-5 hours after going to sleep (as noted on a CGM). When your blood sugar reaches low levels, it triggers your adrenal glands to flood your system with cortisol, which raises your body temperature and wakes you up. It takes a few hours for the effects of this “wakefulness” hormone to subside so you cannot fall asleep again for a few hours.
Ha! Very interesting. I had not heard of that before – thanks for sharing. What is a CGM?
CGM is a continuous glucose monitor. It helped us figure out that I was awakening when my sugar went low after 4 hours or so.
For me my sleep worsens when I over exert myself. If I am tired and wired and can’t sleep then I know that I need to rest more. This may or may not include napping during the day.