



This three-year old, named Shepherd, has arthritis – juvenile idiopathic arthritis (JIA) – an autoimmune disease that can cause disability, stunted growth, even blindness. Arthritis is hammering both his knees and wrists and his left shoulder and elbow. He’s a stoic three year-old, denying he’s in pain but tearing up when the doctor touches his joints.
He’s put on a NSAID, naproxen, to battle the inflammation in his joints, but his arthritis worsens, the joints in his fingers and thumbs begin ballooning and nodules begin forming on his knuckles. He’s wetting his pants because his fingers hurt too much to pull his pants down when he goes to the bathroom.

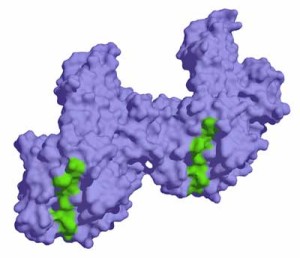
Rheumatoid arthritis can cause disfigurement. Some rheumatologists report,though, that some of their patients are helped by dietary changes
The nodules suggest it’s time to put him on a serious drug called methotrexate, used in larger doses in chemotherapy, and smaller doses for autoimmune disorders. The list of potential side effects (liver damage, increased risk of lymphoma) is terrifying, but the doctor assures them that the drug is perfectly safe at this dosage. Their son may experience nausea, dizziness and drowsiness, but his pain should ease; it’s a good tradeoff, but their doctor expects their son will be on this drug for life.
That gives the mother pause, and one day, out of the blue, she calls the friend of a friend who’s arthritic son went into remission using alternative medicine. Her son had repeatedly woken up screaming and crying a night since he was a month old.
A year and a half later they have a diagnosis. A massage therapist working in an integrative health department, and terrified at the idea of giving her son methotrexate, under the guidance of Dr. Leslie Mendoza Temple in Chicago, she takes an alternative health route. First a naturopath suggests a centuries old antiinflammatory concoction (four marvels). Then gluten, sugar and plants from the nightshade family are cut out. Probiotics (VSL-3), sour Montmorency cherry juice and 2,000 mgs.of omega-3 fish oils are in.
This integrative health worker didn’t believe a mysterious autoimmune process requiring a chemotherapeutic agent was the problem. She believed antibiotics and/or gluten or dairy sensitivity had trashed the integrity of her child’s gut lining, causing his gut to leak proteins and/or bacteria into his blood. The immune response to those proteins and/or bacteria was causing the inflammation that was attacking his joints. She noted that her kid had started crying a week after taking antibiotics. Had his gut lining gotten whacked by antibiotics that most children pass off with no problem? Nobody knew….but the timing was suspicious, and she was going to take the alternative route first.
Six weeks into his treatment her son’s pain started to lift. Three months later it was gone without him ever taking the chemotherapy drug, his doctor suspected he was going to be on for the rest of his life. Two years later he is still in remission.
Meanwhile, Shepherd was not growing normally, was sobbing in the middle of the night, and now had arthritis in his toes. His doctor wanted to increase his methotrexate, was happy for Walker to try the supplements but opposed to cutting gluten and dairy out of his diet.
With her husband backing the doctor, they compromise; Shane will stay on methotrexate and they will go full bore on the alternative regime. Five weeks later, Shepherd is worse, and his parents are a wreck…While Shepherd is spending entire days on his mothers lap, questions over the right course to take cause his parents to bicker and sleep poorly.
They get a second opinion from the director of pediatric rheumatology at Columbia who suggests they double the dose of methotrexate. Dietary changes, she flatly said did not work. Now the father, seeing no progress with his son, pushes hard to double his dose of methotrexate and warns their marriage could be in trouble. The mother holds firm but shaken by everything, manages to have her purse and suitcase stolen, then gets in a car accident. She promptly signs up to see a therapist. Their marriage and their lives are being pummeled by their child’s illness.
The Breakthrough
“Mommy, my knees don’t hurt anymore”
Six weeks, to the day remarkably, since beginning the no dairy, gluten, etc. regime Shepherd wakes up and says “Mommy, my knees don’t hurt anymore”. Over the next several months, his arthritis pain disappears.

The key to this young childs pain was simply diet. Several years after going on his gluten free diet, he remained well.
He starts to grow again. He runs without pain. He’s has no less than 5 remissions over the period of a year, but each, two after antibiotics and three after eating gluten, can be explained.
It turns out that he’s incredibly sensitive to gluten; just a few bites of a sandwich can leave him in pain for as long as two weeks.
This is not to say that methotrexate doesn’t work; it does work in many kids, but the problem for this child was clearly diet. The Director of Pediatrics at Columbia isn’t buying the that idea at all, but their primary doctor is more open stating “I’m mystified by children on a daily basis”.
The Diet Blog Series
This blog is part of a series of blogs highlighting the effect diet can have on health. Recently we saw a woman with several autoimmune disorders who was able to get back to 80% through diet and supplements. This young boy eluded a lifetime of suffering simply by altering his diet. These blogs are not to suggest that dietary changes will have a dramatic effect in most people with ME/CFS; but to highlight the possibility for some they could. They are a powerful option to check out.
The Six Week Rule
You need to stay on a diet for six weeks to know if it will help – Dr. Nancy Klimas
For myself, I’m a bit haunted by the six-week rule. My jaw dropped when I heard Dr. Klimas say you need to be on a diet for six weeks. A week or two on a new diet has always been enough for me to tick off the dietary approach. My physicians, though, have always treated diet as a sidenote. None has insisted on dietary changes, and I’ve never been tested for gluten sensitivity or celiac disease. My diet knocks most other people’s out of the park but is it good enough for me? I wonder.
Finding that my knee flared up when I started eating a lot of tomatoes from the garden, and then flared back down when I stopped eating them has helped to put diet back on the front burner for me. Right now I can click off at least four things – sweets, brown rice, soy and potatoes that tend to put me sleep…which I continue to keep eating. (I am now off gluten :)).
Inflammation, Diet and Chronic Fatigue Syndrome (ME/CFS)
Lets a bit deeper look at the gut inflammation idea. It turns out that four different kinds of arthritis are associated with inflammatory responses in the gut including a gluten based one. Diagnosing celiac disease, as we re seeing in Niki Gratix’s blogs on Health Rising, can be tricky. The young boy, Shepherd, was as sensitive to celiac as could be, but a blood test was negative.

Gluten foods can trigger ME/CFS-like symptoms in gluten sensitive individuals, yet doctors rarely address gluten sensitivity issues in ME/CFS
The blood isn’t the gut, however, and one study that found antibodies to food in the gut but not the blood, suggests doctors may have to go directly to the gut to get real answers.
The gut-inflammation connection is growing. Researchers are beginning to identify specific gut bacteria that may predispose patients to rheumatoid arthritis. They can turn RA free mice into RA mice simply by inserting bacteria in their guts.
Probably more important than single bacteria, however, are bacterial communities. Like the herpesviruses most healthy people are able to keep under control, ‘bad bacteria’ are already present in our guts. When our bacterial composition shifts, inflammation promoting bacteria can become ascendant creating a ‘fire in the gut’ as Niki Gratix calls it, that feeds inflammation not just in the gut but across the body.
The CFIDS Associations pilot gut microbiome study suggests people with ME/CFS have different bacterial communities than healthy people, and that exercise may exacerbate those differences. It’s becoming clearer and clearer the gut plays at least some role in ME/CFS/FM, and that a multi-pronged treatment approach including the gut makes sense.
The remarkable fact that gut symptoms aren’t necessary for a dysfunctional gut to be present ; that your gut could be whacking you without it being painful, is probably missed by many doctors.
- Dig Deeper: Celiac Disease, Gluten Sensitivity and Chronic Fatigue Syndrome: Pt I Misdiagnosis and Mortality
The gut, nevertheless, is frequently troubled in ME/CFS. IBS has become a more common complaint for me over time, but my lower gut has been sore to the touch since the beginning. I vividly remember Dr. Cheney saying, as I flinched while he probed that area, that lower gut sensitivity is very common in ME/CFS. Gut flora manipulation is in its infancy but we know that diet, probiotics, supplements, antibiotics and things like fecal transplantation can help. We’l b exploring these more in Ken’s and Niki’s blogs as time goes on.






One cannot be stupid and acquire a medical degree.
If the nation cleaned up the gut, (especially the fructose) the monetary impact on the entire medical industry would be catastrophic. I’ve said that many times over the years. RP
Great line Rich – “the monetary impact on the entire medical industry would be catastrophic.” 🙂
My lower right gut has been sore for decades but I’d never heard this was part of CFS. Thanks for all the wonderful information Cort. I saw Shephard’s mom on Dr. Oz but don’t think she laid out everything there such as the type of probiotic or the cherry juice.
Thanks Betty, my lower gut has been sore to the touch since I got ME/CFS. It was sore before I had symptoms of IBS….Dr. Cheney actually highlighted the right lower section of the gut in ME/CFS…..
Hi Cort,
l am trying not taking probiotics or digestive enzymes as l am wondering if they too are messing my gut up. l am giving a trial with Fructoless, a product with prebiotics and probiotics that are already fermented before my meal with almond milk and avocado smoothie to help with digestion. l feel better in my gut and have no bloating also feel better when l eat. l have been on a restricted diet for years and now have dermatitis so that is why l decided to try and get as much nutrition into my body as possible by a green food powder and drinks as well as my meals. l find it also helps to digest vitamin B1 better(100mg) l had to give up the B1 as l found it caused my stomach to stop digesting but now l feel better for the change. l also find it interesting the Cheney says lower right part of the stomach that is exactly the part that felt sore or tight? Could this be the top part of the small intestine that where B1 is supposed to be absorbed?
l am also looking into chewable vitamins to take? l like the idea of chewing them to help with the digestion process.
l have only just started last Friday so it is early days yet.
Cheers and thankyou,
Ros
Good luck on the new approach. No bloating is a great start; I haven’t achieved that regularly in years! I’ve never heard of that so thanks for passing it on.
I do believe the bottom right part of the gut was at a junction of some sort. He said he found it all the time and gave me an explanation but my memory has faded.
That is a sweet story for the little boy, such a happy ending.
When I changed my diet, I had to go off everything (well, it had already come to that point, I could eat nothing), to start a three stage process, led by Dr Cheney. Kill of the bad bacteria thoroughly, transition to a point where I could finally take in good gut bacteria. All the while of that, a time of about six months, I was adding foods one at a time in a fairly systematic way. Easier to do when starting from zero, for me at least. No particular symptoms showed up with any food allowed back in my diet. That was nice, as so many were cut out from the start.
But I still eat gluten, in whole wheat bread. It did not seem to do anything noticeable, good or bad to. I made sure to have more variety of grains, though, with rice in particular. My favorite bread is rice-pecan, made with rice flour and pecan flour. Tasty stuff!
Sugar of any type is the demon for me now. Once I reverted to old ways, and what a punishment to pay! Same for the one day I tried some exquisitely cooked Christmas ham, formerly a huge treat. It took only the one day to make clear that Dr Cheney was right about what I could and could not safely eat.
Hard to do, alter one’s diet, especially cutting whole huge categories of once favorite foods. The hardest test is attending a family event at one of my sister’s homes, where she will have a dessert table, all sweet and delicious. And I eat none of it. I try to get one of my relatives to eat an extra piece for me, since I cannot eat it or even try it. Ah well. Better that hard time than the pain that would follow.
Sarah
Thanks Sarah.
Two questions: how did you kill off the bad bacteria? and now that you can tolerate most foods (but not sugar – I’m with you there), how much of a difference has it made?
All the difference in the world! I can eat food and take in the nutrition, and do it without ‘rolling on the floor pain’. I can even use vitamins as supplements, as I can digest them too.
I can eat fish, nuts, whole grains, beans / legumes, soy, whole fresh fruit, vegetables, plain yogurt, some poultry, but essentially no meats, no aspartame (no loss, it tastes awful), and no sugar in any form. No concentrated fruit either, so dried fruits, applesauce, and fruit juices are out. Wheat pasta and white bread are off my list, too, as not being whole grain. My own other food peculiarities, with me before this disease, have stayed with me (I cannot digest cheese very well, e.g., no matter how good it tastes, but milk, whipped cream, yogurt, no problems).
The first step in killing off the bad bacteria was pepto bismol tablets, 4-5/day for 4 days. Bismuth is the relevant ingredient of pepto bismol tablets. A lesser problem might be solved in two days, I think. Concommittant with the killer agents was total avoidance of foods that feed the bad bacteria, which was almost everything. At that stage, no whole grains because the normally healthy fiber (soluble or insoluble) fed the bad bacteria. All the allowable foods seemed white to me — white rice, cauliflower, white bread, white potatoes, were in the starting list.
It took a month or two for that stage (and some other meds and supplements). Then about two months for the stage of regaining homeostasis (the transition stage), when I took a variety of short term OTC supplements, and still kept to a simple diet ( I could add some foods that were not white 🙂 ). Dr Cheney had suggested a powdered protein but I made it with regular food, very limited.
Then I slowly made my way to the last stage with a more varied diet, and I could eat fiber foods again, from oatmeal to whole grain bread and brown rice. I took a different probiotic then to start, Pro Greens Advanced Probiotic made by Nutricology. Now I take MicroPlex made by American Biologics.
Occasionally in the first few years of the new way of eating, I took one pepto bismol tablet when things were getting out of balance, and that was enough.
Once, after 10 or 12 years of perfectly following the new diet, I strayed, and ate too much ice cream for a few months. The whole scene of rolling-on-the-floor gut pain returned, and I needed to use parts of that transition again, which worked. I did it on my own, and more quickly than the first time.
I have been playing with diet for the last 6 months. It does seem like some foods are problematic for me.
Thanks for the great articles Cort!
Thanks Tina. Always good to hear from you. 🙂
Being a fly in the ointment here but every time I’ve gone gluten free I have always gotten worse. Last time I stuck with it for a lengthy period of time as pushed by many on the internet and had a major relapse and developed several new symptoms. Not impressed. Thru trial and error I have found the triggers for my gut symptoms, many are “healthy” foods believe it or not, but yes not gluten! I do avoid heavily refined foods though and practise moderation. Off of my baddies and with other supplements to support my immune system I have improved greatly.
It is important to remember that one cure all doesn’t fit everyone. As more sub-types for fibro/ME/CFS are found and the causes are found I think we’ll understand why different treatments work for some and not others. SO yes worth a try but if you get dramatically worse don’t stick with it, it made me so much worse and I lost over 12 months recovering from that experiment.
:)… That’s amazing Dee. It sounds like you NEED gluten. Hey, we humans are a variable bunch. I guess that’s one of our charms. Glad to hear you’ve improved significantly over time, though 🙂
Anyone out there that has had an ileoanal procedure done? I had one in 1987, so have a W pouch. Now with the J pouch, pouchitis is unheard of. I seem to fall thru the cracks of every treatment as I am the only patient without a colon. I’ve tried lots of diet eliminations, am on antibiotics (half dose) every day. Several antibiotics don’t work for me any longer. A few months ago I started taking the Pearl probiotics so that has helped with yeast problems. I’m also trying acupunture. I feel like I’m on an island by myself with no rescue in sight!
I had a test recently that showed bile in my stomach. I have CFS/FM and I’m wondering if this bacteria that you talk about is related to the bile in my stomach? I would go a long way if I could reduce pain with diet. I might be way off base here. Any thoughts?