

Geoff’s Narrations
The GIST
The Blog
The GIST is at the bottom right
Small research teams can make a big difference. One wonders where we would be without Leighton Barnden and the National Centre for Neuroimmunology and Emerging Diseases (NCNED) team at Griffith University. The fact that the brainstem has become a major area of interest is largely due to Barnden and the NCNED team.
Barnden has been attracted to the “subcortical” parts of the brain (below the cerebral cortex) which affect basic things like movement, sensory signal processing, alertness, sleep, emotions, breathing, blood pressure, the heart rate, etc. Get these things wrong and you have the potential for widespread problems.

Altered connections means the ME/CFS brain, in some key ways, is not operating efficiently.
While some structural problems (reduced white matter, brainstem volume) have been found, the evidence thus far suggests that altered connections between the different brain regions are the central issue in ME/CFS and fibromyalgia. Something is off in the information highways that make the brain function smoothly. It’s as if you plugged Los Angeles in, and Google Maps kept directing you to San Diego.
Altered connections are the least-worst-case scenario regarding the brain, as repairing structural problems in the brain is very difficult, while altering the connectivity between regions of the brain can, at times, be done.
The strange connections DeLange in 2003 found suggested that the parts of the brain involved in “motor planning” or movement weren’t connecting properly. Miller found something similar when he probed the connections to the basal ganglia. With eleven studies popping up, by far the most impacted area, though, appears to be connections with the default mode and intrinsic networks.
The Study

Everything below the cerebral cortex makes up the subcortical areas of the brain. (Image from US government, Public Domain via Wikimedia Commons)
The Australian researchers used an ultra-high field 7 Tesla MRI to assess the connections (blood oxygen levels) between 27 areas of interest in these regions of the brain as 31 ME/CFS and 15 healthy controls engaged in the Stroop cognitive task, in the “Subcortical and default mode network connectivity is impaired in myalgic encephalomyelitis/chronic fatigue syndrome” study.
With the brainstem and the cerebellum being particularly involved in cognitive impairment, motor dysfunction, and the sleep-wake cycle, the authors probed the connectivity (activity) between: (a) the salience network (SA) and default mode network (DMN); and (b) the cerebellar vermis and brainstem regions.
The Two Regions
The Default Mode Network (DMN) – Because the DMN allows thoughts to bubble up, it can promote creativity. On the other hand, because it excels at introspection, it does not allow you to be present in the here and now. When you think about your past or the future, wonder how you are doing, what’s happening to you, etc., (notice the reference to yourself), the default mode network (DMN) is in play.
Since the DMN is self-referential, if you want to get something done, you need to turn it off, and that’s what the salience network does. When it’s time to buckle down and carry out a task, the salience network turns off the default mode network, stops the distractions, and effectively engages us in the task at hand.
The cerebellar vermis – The cerebellar vermis regulates the autonomic nervous system (heart rate, breathing, arousal) via the brainstem. It is also involved in coordination, gait, and movement, and connects with the emotionally charged limbic system.
Results
Movement problems – Reduced connectivity (read activity) between a part of the cerebellum and the brainstem suggests that the signals that help one move easily, track things with our eyes, stand correctly, and engage in skilled movements are not getting through as they should.
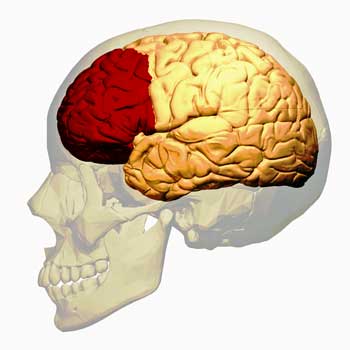
Weakened prefrontal cortex (red area) and anterior cingulate are making it more difficult to carry out tasks – and forcing another part of the brain to step in and help out.
Frontal Brain Problems – Stronger connectivity between the pontine nuclei and clusters of cortical voxels in the frontal pole and superior frontal gyrus suggests that frontal regions of the brain have been damaged.
This is not new. Other ME/CFS and FM studies have found that the frontal cortex (particularly the dorsolateral prefrontal cortex (DLPFC) and anterior cingulate cortex (ACC)) have been impacted. These parts of the brains keep us on task, prevent distractions, integrate sensory signals, regulate movement, and keep the emotionally charged limbic system under control.
This finding suggests that in ME/CFS, the brain has attempted to compensate for the frontal cortex failure by asking the pontine nuclei—a relay center that transmits information between the frontal regions of the brain and the cerebellum—to boost the signal to help people with ME/CFS complete tasks. The authors proposed that a kind of “hyper-stimulation” (hyper-effort?) had occurred.
Problems with Alertness, Sleep, and More – More fun showed up when reduced connectivity to several areas of the cerebellum suggested that the reticular activation system (the RAS), which keeps us alert, regulates sleep-wake cycles and controls attention and the autonomic nervous system—all obvious problem areas in ME/CFS—had been inhibited.

The default mode network excels in self-referential thought.
DMN Problems Affect Basic Baseline Functioning – The authors noted that the DMN’s connections across the brain make it “one of the primary intrinsic networks of the brain essentially responsible for the brain’s baseline functions.”
As noted earlier, the default mode network (DMN) has shown up again and again in functional connectivity studies in ME/CFS. Instead of being inhibited, though, the DMN showed stronger connectivity (activity) in the ME/CFS patients than in the healthy controls.
Overactivity of the DMN can have some real consequences: mind wandering makes it more difficult to engage in tasks (again), increased focus on one’s self can lead to cycles of rumination, increased recall of past events and more difficulty disengaging from negative thoughts has obvious consequences and—given a potential connection with the amygdala in ME/CFS—increased emotional responses to those negative thoughts may be present. Oh yes, high DMN activity is also a recipe for brain or fibro fog.
THE GIST
- The evidence thus far suggests that altered connections between the different brain regions are the main issue in ME/CFS and fibromyalgia – and that’s what Leighton Barnden and the National Centre for Neuroimmunology and Emerging Diseases (NCNED) team focused on in this study.
- Using an ultra-high field 7 Tesla MRI, they assessed the connections between areas in the subcortical, or lower, part of the brain while the participants engaged in a cognitive task.
- Movement Problems – Reduced connectivity (read activity) between a part of the cerebellum and the brainstem suggested that the signals that help one move easily, track things with our eyes, stand correctly, and engage in skilled movements are not getting through as they should.
- Frontal Brain Problems – A “hyperstimulation” in one part of the brain suggested that the frontal areas of the brain that help us carry out tasks and keep the emotionally charged limbic system under control have been damaged.
- RAS – reduced connectivity to several areas of the cerebellum suggested that the RAS, which keeps us alert, regulates sleep-wake cycles, and controls attention, had been inhibited.
- Default Mode Network (DMN) Activity Increased – stronger connectivity (activity) in the DMN indicated yet more problems with alertness were present with mind-wandering, self-referential thinking, and negative thoughts coming to the fore. Increased activity of the DMN has shown up more frequently in connectivity studies than in any other part of the brain.
- Issues with the salience network suggested ME/CFS patients’ attention was being forced to deal with sensory sensations and pain – and might help explain the difficulty being on task, the possibly increased rumination, the negative thoughts, etc.
- The default mode network’s increased connections with the amygdala and hypothalamus in ME/CFS suggest a state of chronic stress has dysregulated both of the stress response axes.
- Getting stuck in “DMN mode” has major implications for energy. Trying to do a task while one’s mind wanders uses more energy. Moving smoothly and efficiently while doing physical tasks becomes impossible.
- Because dopamine – the reward neurotransmitter – suppresses the DMN, low dopamine levels could play a role in DMN activation. Dopamine provides the motivation and, therefore, the energy needed to engage in and carry out tasks. Stimulants can be tricky to use, but they can increase dopamine levels and have been used successfully in some people with ME/CFS/FM.
- Neurostimulation and mitochondrial support might help as well, but most recommendations focus on mind/body techniques (mindfulness and meditation practices, challenging negative thoughts and replacing them, purposely bringing focused attention to bear, loving-kindness meditations, breathing techniques (see blog), brain training apps, and gratitude journaling.
Increased Pain – Positive correlations between several parts of the salience network (anterior cingulate cortex (ACC), insula and vermis VIIIb, and left supramarginal gyrus (SMG) and vermis VIIIb) provided a potential reason for the increased “self-focus” found—increased detection of stimuli and levels of pain—forcing one’s attention onto those. Both the insula and anterior cingulate have been associated with fatigue and pain in ME/CFS and fibromyalgia, and chronic pain has been shown to activate the default mode network.
While not everyone with ME/CFS is in pain, many are – and everyone with fibromyalgia is. If ME/CFS/FM is, as Dr. Clauw has proposed, at least in part a “sensory disease,” one can see all these issues – the difficulty being on task, the possibly increased rumination, the negative thoughts – might naturally emanate from the difficulty of trying clawing through a maze of sensory stimuli. With the body’s alert systems on full blast, a degree of “self-focus” is probably an appropriate, if not helpful in the long run, response.
Rumination has not been assessed much in ME/CFS or fibromyalgia, but the inability to do gainful work (or sometimes almost any work), the hit to finances, the loss of friends, the inability to do the thing that used to bring joy – all provide ample room for rumination.
Implications for Energy Production
The default mode network’s increased connections with the amygdala and hypothalamus in ME/CFS suggest a state of chronic stress has dysregulated both of the stress responses: the hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system activity. The energy-intensive nature of an autonomic nervous system in “fight/flight” mode puts extra strain put on one’s energy resources and the mitochondria – potentially leading to the state of immune cell exhaustion we’ve seen in these diseases.
Inefficiency is the rule with the DMN, as the brain keeps jerking back and forth between focusing and wandering when trying to do a task.
Getting stuck in “DMN mode” (wandering thoughts, self-focused thoughts, negative thoughts) has major implications for energy. Trying to do a task while one’s mind wanders uses more energy. If it’s a physical task (remember the motor planning issue), moving smoothly and efficiently becomes impossible; with a mental task, one has to keep jerking oneself back to the task—a costly and PEM-inducing enterprise as the brain has to keep shifting resources back and forth.
We recently saw evidence of increased oxygen and glucose consumption in the brains of ME/CFS patients, and two large studies are underway to assess this.
Negative emotions are also associated with increased levels of pro-inflammatory cytokines (e.g., IL-6, TNF-α, CRP), which can potentially slow the immune response, throw the gut microbiome off, accelerate cellular aging, and impact the cardiovascular system and metabolism.
Dopamine Connection
Because dopamine suppresses the DMN, the low dopamine levels that appear to be present in these diseases may play a role in DMN activation. One hypothesis proposes that low dopamine levels play a crucial role in fatiguing neurological diseases such as multiple sclerosis, ME/CFS, and traumatic brain injury.
Dopamine provides the motivation and, therefore, the energy needed to engage in and carry out tasks. Since dopamine is the “reward” neurotransmitter, the “low rewards” associated with tasks in people with low dopamine levels could make it difficult to break out of a DMN chokehold. By assessing our energy state, it helps us choose what tasks to carry out. Low dopamine levels result in tasks being associated with low rewards, translating into difficulty in carrying out tasks.
None of the sources I saw suggested using dopamine-enhancing drugs to reduce DMN activation, and I don’t know why. Stimulants like modafinil, Adderal, and Ritalin can be tricky to use, but they can increase dopamine levels and have been used successfully in some people with ME/CFS/FM. Are they an option?
Treatment Suggestions

All the other recommendations I found involved mind/body techniques. Neuroplasticity practices, including mindfulness and meditation practices, challenging negative thoughts and replacing them, purposely bringing focused attention to bear (one person found focusing on the minutiae around her helped), repeatedly returning oneself to the present moment, loving-kindness meditations, breathing techniques to rebalance the autonomic nervous system (4-7-8 Breathing: Inhale for 4 seconds, hold for 7, and exhale for 8; Box Breathing (4-4-4-4): Inhale, hold, exhale, and pause—each for 4 seconds. Alternate Nostril Breathing), relaxation exercises, brain training apps, good sleep practices, and gratitude journaling (increases dopamine production), were suggested.
Conclusion
Difficulties with movement, cognitive and physical exhaustion, mind wandering, difficulty keeping focus and completing tasks, and increased pain levels seem to be baked into these diseases. It’s good to see brain imaging studies provide a reason why. While we don’t know what’s causing DMN activation, it may be possible for some people to turn the DMN down a bit and get some relief.






Griffiths have been doing some really good work over a few years. And Zak Shan who used to work with them is leading a very interesting study on neurovascular coupling at a different university also in Queensland.
I think transcranial direct current stimulation is very interesting. Has anyone tried it?
Neurovacular coupling – the ability or inability of the brain to speed blood to the areas needed – could just be the cat’s meow…A almost 300 person study is examining it in ME/CFS 🙂
What are there, if any links between adhd and ME ? Is there a higher incidence of ME with adhders if there’s a dopamine deficiency commonality ?
One study found high rates of ADHD in fibromyalgia. I assume that its similar in ME/CFS.
https://www.healthrising.org/blog/2018/01/20/adhd-attention-deficit-hyperactivity-disorder-fibromyalgia/
The same, interestingly, is true for autoimmune diseases…
I’ve been reading a lot about nicotine therapy. Anyone have experience?
It did well in a poll we did.
https://www.healthrising.org/blog/2023/12/07/nicotine-patch-long-covid-chronic-fatigue-fibromyalgia/
Yes I did. It really helped me but only short term and continuing forever was not sustainable because the treatment did exhaustion me to the point that I was missing too many of the few activities and connections I am able to get to. In retrospect, I would have returned earlier for more follow up treatments but only twice a week maybe instead of the 5 times a week which I had done for the course of treatment. Might have been better to hear it off at the pass until waiting until I had started to slide back.
Cort,
This is going to sound contrived, but I literally just came to your site to see if anything had ever been published about default mode networks and ME/CFS and this was the most recent article.
Cutting to the chase, I’ve got a tip based on recent experiences. If you are capable of handling the auditory and mental stimulation, I think audio books are very good at keeping the DMN from gaining momentum during the day. Podcasts (except for very good ones) don’t cut it – your brain needs something of quality to really buy into it. I’ve noticed that using noise cancelling headphones all day (i.e. whenever possible) with a good audio book means my sleep significantly improves. Meditation by contrast (e.g. transcendental) doesn’t seem as effective as the DMN (or whatever it is) gets to build up too much momentum between sessions. I’d propose people could try something free and substantial like War and Peace or David Copperfield to see if it works for them. No shortage of hours of audio in those, with the added bonus that most people haven’t read them.
Nice! And it helps with sleep….ramping down the DMN (and the sympathetic nervous system) during the day helps with sleep. That makes so much sense. How can you get into deep sleep with your fight/flight system engaged? A couple of Australian studies concluded that it was the autonomic nervous system that was keeping us from getting good sleep….
I’ve been using audible books to help with sleep for years. I never had issues sleeping until my fibro started. Then my brain wouldn’t switch off. I can now fall asleep within 10 mins as a rule. I still have times when I cant get to sleep. I just wish it helped me sleep all night. Sadly the pain wakes me and I then struggle. If I’m having a particularly bad day I will have my book on to relax and keep my mind from all the things I should be doing and how useless I’m being. I’ve tried relaxing music and meditation cos but they don’t hold my.mind from wandering like a book does.
”The default mode network’s increased connections with the amygdala and hypothalamus in ME/CFS suggest a state of chronic stress has dysregulated both of the stress response axes.”
Well said. This is the main problem in think 🙂 Now we need to know why? Or how can we fix this.
Why is a great question…It’ could be continued immune activation and inflammation. It turns out that the basal ganglia (reward) and the substantial nigra are unusually susceptible to inflammation.
This is the paragraph that jumped out at me. Being a long term patient, I changed the ‘chronic stress’ to ‘chronic Lyme disease’,or ‘Neuroborreliosis’, which is the cause, for many with ME/CFS. This whole article describes perfectly the challenge daily, to get anything done, any simple plan.
So a SGB might help too? Tap down the stress responses?
Right! It does tamp down the stress response – one of the few things that does. Thanks for mentioning it.
What is SGB?
Stellate ganglion block – a new study was apparently recently published about it. Here’s something about it.
https://www.healthrising.org/blog/2021/12/28/stellate-ganglion-long-covid-fibromyalgia/
Stallate Ganglion Block. I had the procedure done, and had high hopes going into it. The hope was it would reset my stress response. The first injection perhaps helped slightly. The second spiked my blood pressure through the roof, and over the next days and weeks my CFS worsened.
It was worth a try, but I likely won’t try it again. It wasn’t cheap.
SGB??
Interesting timing. I woke this morning with by far the least amount of pain since taking a grueling cognitive test at the neuropsychologist 10 days ago.
So what was different? Last night I had what I call a “ketamine dream.” (i.e., a dream that is an echo of the ketamine-for-pain infusions I’ve had in recent years.)
I know ketamine isn’t for everyone, but its impact on DMN is intriguing.
(Hope everyone is feeling okay today.)
Reminds me of when one esteemed blogger said: “there’s a lot of ADHD in ME/CFS” 🙂
About a year ago I attended a ‘mind-body’ focussed webinar on dealing with chronic pain, through the practice of an ME/CFS Dr in BC, Canada (but not by the Dr himself, who I think would not have approved of the content). After previously having learned about the Default Mode Network and it’s role in chronic pain, depression, etc… I was surprised and even dismayed that the presenters were apparently encouraging chronic pain patients to engage in specific practices that activate, rather than minimize, the DMN. I questioned this at the time, suggesting that the goal might instead be to decrease DMN activity, but feel I was offered some disappointing ‘word salad’ explanation by the presenter as to why mind wandering and ‘creativity’ is actually good for chronic pain.
The experience left me wondering what qualifications are required to present to these groups of vulnerable patients, and I felt disappointed. I knew these views did not represent the current medical understanding but there is no mechanism I know of through which patients can leave constructive feedback for the practice.
The Dr himself, featured previously in HR, is very knowledgable. But I think it’s really important, for the sake of patient welfare, that guest presenters are vetted carefully, and have current medical understanding re such topics. As someone who has made progress through learning to limit the DMN’s contribution to ME, FM, and POTS, it was discouraging to hear fellow patients be advised in the opposite direction.
The experience left me wondering if these webinars are relaying evidence-based practices to patients, or instead function as a sort of day care for perceived ‘hopeless’ patients.
I think all of this has a lot to do with the immune system. Some years ago, I needed to write a concept paper based on the proceeds of an international conference on immunotoxicology. There were dozens of scientific papers that I needed to read and digest to put together a paper: Immunotoxins as Teratogens . https://birthdefects.org/wp-content/uploads/2014/04/Immunotoxins_as_Teratogens.pdf I had been putting it off since I just couldn’t concentrate long enough to accomplish the task. Then I got the flu and, as bad as I felt, suddenly I was able to read and digest the science and put together the paper. I have often wondered if my immune system was so busy fighting the flu, it gave me a break from the usual brain fog of ME/CFS.
Betty, I can relate to your experience. Although I rarely catch any colds or flu bugs, if I do catch one, I invariably feel noticeably better than my baseline on the day before my symptoms commence. I also felt significantly better than my baseline for several hours after I received my first Covid vaccine. These experiences make me wonder if the new immune challenge distracts my immune system from its usual (CFS) skull-duggery? For this reason (and others) I have a strong suspicion that the immune system is significantly implicated in my (CFS) symptoms.
Dr Howard Schubiner who follows Dr John Sarno’s original mindbody work, would say that these conditions are created by the brain as a solution to distract you from deeply unconscious stresses and thoughts. If you then get a physical illness, the symptoms of that illness provide sufficient distraction from the emotional stress for there to be no need to send ME/CFS/FM/migraine symptoms.
Once the physical illness resolves, the brain needs to start resending the mindbody symptoms.
Many people successfully recover using the suggestions listed by Cort. For evidence see the recovery interviews by Raelan Agle, Dan Neuffer, Rebecca Tolin et al
This reminds me of Dr Ron and bob naviaux noticing autistic symptoms improved during an infection.
Their conclusion was that of the idea of ‘ healing cycles’ interrupted. Not by the infection…the cell danger response stops healing cycles from occurring. This is in response to environmental triggers, vaccines,shouldering infections. But when the immube system is asked to treat a new infection, it let’s go of these long standing cell danger responses and allows healing cycles to be completed, hence the sufferer feeling better. B9b naviaux used suramin as proof of concept. That was nearly ten years ago now. Cheap generic drug…the cynic in me can’t but help think he was shut down from asking this further
I woke from a dream in which I had fully recovered from ME/CFS 4v years ago after drinking something from a well. In the dream, the word “suramin, suramin, suramin” was resounding in my head.
We were in the pandemic at the time and I think I had heard of it once in relation to that (remember all the pine needle tea comments?!). But I had no idea what it was or how it could apply to ME/CFS at the time.
I immediately googled it when I woke up and was shocked to see it could be relevant, and disappointed that I couldn’t get hold of it. I still get chills remembering that dream. If anyone knows how we can try this, please comment! I think my body gave me my answer and to this day I’ve been unable to try it. I wonder if the doctor was silenced too.
Whoa! Let’s hope that your dream was prescient and that drug gets its trial. Bob Naviaux has been trying to get a small trial underway for years. At one time, it seemed like he was quite close.
He did phase two trials as far as I’m aware cort. Improved all patients who received the dosing.
I belueve bayer gave him the recipe to make this abd he crewtee a snall manufacturing plant to make it possible.
Then nothing..seems very odd
Contact naviaux labs would be a good idea. I’d love to know what’s going on
I have actually contacted the labs following those conversation to see what’s happening and all of there’s anything is patients can do to support the efforts and make it happen. I told them about the dream though so they probably think I’m nuts! 🤣🤦
I see it’s supposedly possible to get Suramin from India, but not sure if it’s the same stuff. Also, does pine needle tea or tincture actually contain it? Naviaux says No, but others say Yes.
I agree with you too, Betty (and Dave). Anytime I’ve fallen ill that is when I finally feel “normal” again. Despite being shot down with whatever sickness it is I can function as my “old” self in almost every way. And I too have the same experience as you, Dave. The day before an illness I feel uncharacteristically good.
All I know is if expensive little bandaids, like an NAD IV for example, can alleviate my symptoms and feel almost normal again for about a day, then there must be something out there to bring us to almost normal again.
I have the same experience Betty. For many years I’ve thought it’s probably a big clue as to what’s going on for me but it doesn’t seem to get written about much. I vaguely remember Ron Davis mentioning that Whitney had some temporary respite immediately after recovering from an infection. I think his and Rob Phair’s hypothesis that the Innate Immune System isn’t turning off in certain cells makes sense of the immune dysfunction and other problems downstream of that, like the metabolic dysfunction and muscle weakness. I’d like to see more research that looks at the whole picture and not just one specific dysfunction or symptom.
Thanks for another great article. In terms of treatment though I felt it might be missing one key thing. There has been a lot of good research on the clinical application of psilocybin (a psychoactive compound found in some medicinal mushroom species) in reducing default mode network activity. Here is just a taster:
https://pubmed.ncbi.nlm.nih.gov/32454209/
https://hopkinspsychedelic.org/campaigns/view-campaign/ApqQqn_1cLu3G9LdrJPBUsf-0QVto8VFRn0QbXLsinnng8lz3dMR-5OPt1q65q6WqgBkZRjRqXwkhVKIrI6yRjoZs5W-Ai1T
This is one major reason that it’s been found to be so useful in the treatment of depression and anxiety associated with end of life illness. Johns Hopkins, for example, has done a lot of work focussing on this (see link).
But far from being a replacement for meditation, the experience can produce lasting change and also serve as motivation to meditate more regularly. Personally I really turned a corner in my ability to cope with ME and associated DMN dysregulation after receiving psilocybin treatment, which is now legal for this use in Canada (through Health Canada’s Special Access Program)
One more thing I will mention, because Cannabis so often now gets a free pass in the ME community; it’s kind of the opposite of psilocybin. While it may help in the short term with some symptoms, in my experience it revved up DMN activity like nothing else and was not a sustainable treatment option, specifically because of this effect.
So interesting! A couple of fibromyalgia trials are underway.
https://www.healthrising.org/blog/2021/12/02/psychedelics-psilocybin-lsd-fibromyalgia-chronic-pain/
Thank you for this website and your work Cort. All of the scientific information can be overwhelming and confusing. You do a superb job reviewing the material, and pointing out the bits that matter helping the non-medical chronically ill navigate it all. It’s not easy.
Thanks!
Wow ! I recognize myself here.
Difficulties with movement – (problem with gait in the stairs, equilibrium and body awarenees when cycling and skiing, all this directly proportional to my level of fatigue),
cognitive and physical exhaustion – (all the time),
mind wandering – (difficulties to stop thinking),
difficulty keeping focus and completing tasks – (reading, mathematics, logical reasoning)
Pure coincidence ??? I don’T think so…
Michael Pollan’s book “How to Change Your Mind” goes into depth about how psychedelic medicines (ie: psilocybin, LSD, maybe MDMA) help reset or rewire the Default Mode Network. I wonder if they could be helpful with ME/CFS like they are with depression, anxiety, PTSD, and addictions?
Everyone please be aware that we have no objective evidence brain retraining actually fixes this. All the trials of Gupta for example have big issues even meeting their own significance goal despite often doing things like using GET as control. This is Corts opinion, not gospel.
Why do people always go to the “fix it” or cure card when neuroplasticity or mind/body practices are involved. Did I say “fix it”? No, I wrote these practices may be able to help some people – and that’s my experience.
We don’t have strong study evidence with regard to ME/CFS – and we probably never will as no one in those field has the money to put together large studies – so we’re going to have to rely on other ways to assess their effectiveness.
These practices are not in doubt in other illnesses, though. They don’t help everybody and they don’t cure but they can help. This is not an extreme view at all. On the contrary it’s a middle of the road view at least with regard to chronic pain.
Multiple studies have shown that mindfulness meditation can reduce pain – https://pmc.ncbi.nlm.nih.gov/articles/PMC10739252/; so have gratitude practices – https://pmc.ncbi.nlm.nih.gov/articles/PMC10196463/; breathing practices – https://www.va.gov/WHOLEHEALTHLIBRARY/docs/Diaphragmatic-Breathing-Assist-Self-Management-Pain.pdf; loving kindness practices – https://pubmed.ncbi.nlm.nih.gov/16049118/
Oh wow, if it would be okay I would love to screenshot this response Cort? This issue seems to come up a lot in the ME/CFS community and you have so eloquently explained that these practices can help!…
It’s such a waste to shun any mention of them just because they aren’t a “cure”.
Does it suggest brain retraining in the paper? No. So don’t push it on people when there is no definitive evidence.
I stated treatments weren’t indicated in the paper. However, if you look up ways to reduce default mode network activation – those are the things that came up. When I find something wrong I always look for potential treatments and in this case, that’s what came up. I actually tried hard to look for other things – and came up with something none of the sources I consulted mentioned – dopamine enhancers.
Anyway, what I did is not pushing – it’s reporting. While I understand that you and others don’t want to hear about neuroplasticity I make this whole area simple for myself – I’ll just report what shows up!
I don’t think you need to worry about neuroplasticity by the way as I don’t see any way that it will impede biological research. I have something coming up on that.
If you look at Branden’s other work he also showed a lack of myelination of the brainstem which might well be causing this. But if that turns out to be true, brain retraining might not be able to help this at all.
I agree partly. We know that brain retraining can be helpful – but not curative – in people with strokes and neurodegenerative diseases – but it seems you can only go so far once significant structures are damaged. Exhaustion presents another challenge. Still, it’s amazing what some people who have been very ill have been able to accomplish.
I assume inflammation is the culprit. If you lower inflammation can those neurons recover? I have no idea.
Thanks, Cort.
Great! The topic of white matter has finally entered the discussion.
Revisiting my 2008 MRI and having multiple conversations with neurologists about reduced white matter prompted me to write about it in 2023. However, at the time, the question of whether white matter abnormalities are directly related to ME/CFS remained inconclusive. The only certainty was that demyelination of neurons plays a role in many illnesses.
Here are 3 examples:
ME/CFS Is it really elusive evidence? https://swaresearch.blogspot.com/2023/11/mecfs-is-it-really-elusive-evidence.html
Neuron Demyelinating related to many Illnesses https://swaresearch.blogspot.com/2023/10/neuron-demyelinating-related-to-many.html
Brain White Matter https://swaresearch.blogspot.com/2023/09/lost-brain-white-matter.html
Thank you Cort,
I would also want to mention previous work by this group which may open another perspective on the DMN: When ME/CFS patients engage in activity their DMN is not being switched off as it should (and does in healthy people). They remain in the “chill mode”, if you will. This means that the many biological effects that activity brings along (inflammatory signals, adrenergic load, oxidative stress, activation of the immune system) hit the body unprepared – for lack of a switch into the “activity mode” it cannot ward off the untoward effects that activity inevitably brings along. I.e., there is no adaptation to exertional stress – which can now be demonstrated on many levels (summary of studies here: https://tinyurl.com/3b52we79). This could explain why, in ME/CFS, the body gets harmed from exertion. The lack of DMN inactivation could really be the key problem underlying PEM.
Thank you, Renz-Polster, this was extremely informative!
Yours and your fellow researchers’ hypothesis is intriguing in many ways, and is unifying in a lot of aspects.
I am glad i took the time to read it.
To anyone researching comments for all kinds of clues like I do – I highly recommend reading this if you haven’t already. This is not a hypothesis that relies on brain retraining (albeit I recognize that such techniques may help some for some aspects), but a unifying hypothesis regarding medical findings of the brain, brain inflammation, viral reactivation, IBS, traumatic brain injury, Ehler Danlos Syndrome, and so much more.
It really is the most interesting hypothesis I have read so far, and explains many aspects of what might be going on with us.
I think it is important to note that “stress” in this instance does not pertain to solely “mental” or emotional stress. It is not used as a psychological term here, but as anything that puts the the body and/or brain in a state of “arousal” – may that be viral reactivation, inflammation or degradation of brain matter, endothelial dysfunction, mastcelle-activation, mechanical triggers like craniocervical instability, etc. Neither does it claim that brain retraining-techniques can fix all of this.
There is now a vast array of medical research showing that ME/CFS is a biomedical illness. This hypothesis is not underscoring that – I am inclined to say it rather supports this.
Personally I find the dopamine aspect interesting, as I have bipolar disorder 1, although I have been in full remission for many years now. Bipolar disorder has recently been shown to be atleast partly affected by both too much – or too little – dopamine. There is also a dopamine link in fibromyalgia, showing abnormal dopaminergic neurotransmission. But I also believe that dopamine is only a small piece of this big puzzle we’re looking at.
I’m hoping your hypothesis will lead to many interesting findings, and possibly treatments, over time.
There is so much interesting research going on at the moment, from so many different aspects.
I’ll be following your research with great interest!
And thank you too, Cort, for once again bringing us a step closer to figuring out what’s going on and what we can do about it.
Fascinating! My personal experience is that when I’m in DMN mode – when I can’t fully engage in activities – it’s like my body is at war with itself – part of me wants it to move – a big part says no: it’s like it freezes up. Hanson, of course, has shown on several levels how the body is not kicking in during exercise… Looking forward to reading the paper.
I never got into the DMN until I read this paper….
I agree, I also have this same experience as you, Cort. If I for some reason need to force activity beyond means, it becomes harder and harder, a few times up until the part that I literally froze and simply COULDN’T move anymore – or think, even though I tried to get my brain to.
It also explains how we can do much more at times when we feel properly rested – and why PEM hits so hard and can last for a longer or shorter period of time, depending.
(Quality) sleep is one of the processes that takes care of ridding the brain and body of inflammatory processes, and repairing processes. Quality sleep affects resting heart rate and HRV. And normal distribution of neurotransmitters is in part dependent on sleep. And sleep is ofcourse affected by all these other processes – allergies (histamines have a peak around 01.00-04.00 at night), arousal, pain, inflammation, etc etc.
I do believe the lack of quality sleep we are getting is a big part of the picture of why it is so very hard to get better. Sleep is also a big part of fibromyalgia. Dopamine is released in healthy people when they excercise – but not when a person with ME/CFS or fibromyalgia excercises.
At the same time, it might not be as easy to just take dopamine – after all, the body and the brain is wonderful at compensating and tune down whenever we add something.
This has atleast spurred me on to look at a dopamine-enhancing diet (long overdue).
So many connections. Truly fascinating, as you say! 😊
The link provided in the hypothesis about the animal model of central fatigue was also worth a read, showing how central fatigue can be induced by sleep deprivation, and exacerbated by other stressors.
I would have been tempted to introduce some IV saline, real and placebo, between rounds of testing.
The Stroop test and J Ridley Stroop are interesting to read about if you have the energy.
Cort, while we are waiting for the elusive “cure” for ME/CFS and Long Covid, I would love for you to run a blog with suggestions of things that have helped with various symptoms; i.e. bike shorts for compression in higher heat. I would have never thought of this if if hadn’t been for Cydne.
I don’t mean prescription meds which everyone can’t get, but o-t-c products and other treatments that are readily available. For instance, I was having a lot of stomach problems until I started taking a chewable Pepto-bismol before a meal, particularly a meal in a restaurant where you don’t know what they are using. I have extreme reactions to MSG, but you can’t trust restaurants to even know if their cook uses it.
Here is another suggestion from an allergist I saw for food reactions: take 1 tsp. of Vitamin C granules and one aspirin-free alka-seltzer in a small glass of water.
Cream of tarter can also lessen the reaction to MSG.
If you are not sure what you are reacting to, get a copy of Dr. Marshall’s Mandell’s Five-Day Allergy Relief Plan. I saw the late Dr. Mandell many years ago, but his research is still cutting edge in my opinion.
I am sure that other readers also have helpful tips that they could share.
Nice idea 🙂 A Tips paper…
In my experience, increased activity in the DMN is associated with ME/CFS. Given the brain’s inflammatory state, it’s not surprising that it might become dysregulated. However, I’ve also observed that even prolonged periods of reduced DMN activity do little to alleviate ME/CFS symptoms. In other words, while heightened DMN activity does contribute somewhat to the symptom burden, it appears to be a downstream effect of the core ME/CFS pathomechanism.
Anything about dopamine gets my attention because my experience of being able to do more in environments where I feel “alive and awake”.
The wholesale changes in the brain (DMN, RAS…), however, tell me that there must be an upstream event.
I also wonder how overactive DMN relates to PEM, the worsening of symptoms after a delay. One possibility could be brain as whole somehow becoming hypersensitive to inflammatory cytokines, with the brain anomaly getting worse from low-grade inflammation.
Please provide the references. Let us read the paper and not just read your interpretation. Thank you
If you really want to dig into this, Maple, this is not hard. You could plug “default mode network and ME/CFS” into PubMed or even to Google to find the paper and read it or you could go to the first couple of paragraphs and click on the link to the paper.
EMG confirmed demyelination/UCTD, and I’ve concluded from 16 years on with ME that the brain is what controls. From relentless self testing including calendar year diets for most of these years, I’ve arrived at the one that clearly helps, remnant carnivore. It simply provides optimal nutrient density and deletes plants that aggravate so much without any benefit. I’m far less functional in winter, it’s proportionate to the amount of sunlight. Starting about now I slowly start to ramp up energy, clarity, and muscle strength as the days grow longer. I’ve built solariums to enable winter heliotherapy which allows a jumpstart. as soon as I’m able to start working around my home outdoors with my shirt off, it is the single most helpful therapy. As long as I can go at my own pace without pushing or stress, I’ve been able to work up to quite physical hard work. In midwinter I’m barely able to exert more than moving my own body, with much neurological exhaustion. my third leg I’ve found is Buteyko style breath technique, which has now become automatic. It’s the opposite of a Wm Hoff hyperventilation. even living at 5400 feet in Boulder Colorado, I cannot utilize so much oxygen, I now take sips of air with very extended exhalations and everything with my mouth shut. It has become my primary means of pain control and A&S calming. I have adrenergic O/I so adrenaline is a constant battle. When PENE is triggered, my heart becomes erratic and pounds hard, fluctuating between 40 to 90 BPM with skipped beats, and I otherwise have a very good heart with a 0 CAC score at age 60, albeit I was very athletic from a wee kid raised on a clean-air peaceful KS farm in the 1960s and 70s. I became a serious meditator for many years but now feel my life must remain a walking meditation in everything I do. my diet minimizes mental and physical stress, I still have diminished mental resilience, especially with difficult customer service or any stressful events which are unavoidable. I’m looking for someone to interpret my excellent SPECT processed through oasis Sagami software into a amazing 3-D images, would love to overlap this with the referenced MRI studies. Dr Byron Hyde was using my case and his new book which is likely unfinished as he passed a short while ago tragically. I feel his observations around an enterovirus root cause maybe accurate, as my muscle weakness pattern fits a missed-superior-polio scenario. after many years of now finally slowed down enough to recover especially my brain energy, with very careful minute by minute management. it’s been good to catch up a bit especially interacting with people if only online so far, except for restarting Salsa dance classes I used to excel at, I dropped back to beginning level. GET does not help since we must control our exertion by tuning in deeply both body and mind by the second. it’s where I feel the dopamine effect, also staying on two wheels as long as possible, I’ve dropped down from racing motorcycles and mountain bike bikes to scooters and E bikes to control exertion. It allows the greatest extent of joy and a sense of freedom, which for me is the healing portal access. I try to find ways to let enjoyment beat down unwanted thoughts and unavoidable grief; ME = Missing Everything.. I’m glad I found this site even if I can’t fully process all of the technical data. Thank you Cort. Btw where might I find one of these studies to apply for!? i’m very tuned in to my being and would provide solid feedback…